Introduction
The incidence of ovarian cancer (OC) is third
highest among female genital malignancies, and has the highest
fatality rate; for example, ~14,080 women died from OC in the
United States in 2017 (1). Moreover,
the mortality rate of OC ranks first among all types of
gynecological tumors, and these malignant tumors seriously threaten
the lives of women (2). In recent
decades, there have been three major advances in the diagnosis and
treatment of OC, namely, scientific surgical pathology staging,
maximum tumor reduction surgery, and combination chemotherapy with
platinum and paclitaxel, which have increased the 5-year survival
rate of patients from ~35 to 50% (1). However, there are no effective
biomarkers for the early diagnosis of OC; thus, 70–80% of patients
are at the late stage of the disease upon hospital admission and
miss the optimal time window for radical surgery, chemotherapy and
radiotherapy (3). Therefore, it is
crucial to identify suitable prognostic biomarkers of OC to improve
outcomes in patients.
CD8+ cytotoxic T lymphocytes (CTLs)
specifically kill tumor cells and play an important role in
antitumor immunity. However, numerous factors in the tumor
microenvironment (TME) can induce CD8+ T cells to
upregulate the expression of the inhibitory receptor programmed
cell death-1 (PD-1) (4). The binding
of PD-1 to programmed cell death-ligand 1 (PD-L1) significantly
decreases the ability of CD8+ CTLs to kill tumor cells
(5). Although several basic studies
and clinical trials have shown that anti-PD-1 or anti-PD-L1
antibodies can elicit significant antitumor immunity, ~80% of
patients fail to respond to treatment with antibodies against PD-1
or PD-L1 (6). Based on the available
clinical data, PD-1 blockade is effective in only a small number of
patients with certain types of tumors. Furthermore, the molecular
mechanisms that underlie this phenomenon remain to be
clarified.
Recently, Schietinger et al (7) reported that tumor-infiltrating
lymphocytes (TILs) in mice strongly express PD-1 and that their
differentiation involved two separate chromatin states, i.e., a
therapeutically reversible state (state 1) and a fixed state (state
2) (7). These authors further
demonstrated that the CD8+ T cells in state 1 exhibit a
low level of CD38 and CD101 coexpression, and can recover the
ability to secrete interferon-γ (IFN-γ) and tumor necrosis factor-α
(TNF-α) following in vitro stimulation, thus restoring the
ability of the CD8+ T cells to kill tumor cells. By
contrast, state 2 is an irreversible dysfunctional state in which
the CD8+ T cells strongly coexpress CD38 and CD101, and
cannot recover IFN-γ or TNF-α secretion despite several rounds of
stimulation (8). Therefore, the
coexpression of CD38 and CD101 on PD-1+CD8+ T
cells can predict the therapeutic effect of anti-PD-1/PD-L1
blockade (8). Nonetheless, whether
the coexpression of CD38 and CD101 in
PD-1+CD8+ T cells can predict the clinical
prognosis of OC remains unclear.
In the present study, the expression and
distribution of CD38/CD101 in PD-1+CD8+ T
cells was examined in peripheral blood and cancer tissues of
patients with OC. Furthermore, the association of
PD-1+CD8+ T cell subsets with patient
clinical parameters, postoperative chemotherapy outcome indexes,
serum cancer antigen 125 (CA125) and human epididymis protein 4
(HE4) values was analyzed to explore the predictive value of
CD38/CD101 coexpression in PD-1+CD8+ T cells
on the prognosis of patients with OC.
Materials and methods
Patients
A total of 96 women with epithelial OC aged 37–68
years (mean age, 55.21±9.91 years) were enrolled in the present
study, as well as 26 age-matched healthy volunteers. All patients
were admitted to the Department of Obstetrics and Gynecology at
Southwest Hospital of the Third Military Medical University
(Chongqing, China) between March 2017 and February 2018. On the
basis of histological stage, 45 cases had high and moderate
differentiation, and 51 cases had low differentiation. Tumour
staging was performed by the International Federation of Gynecology
and Obstetrics classification (https://www.figo.org). Inclusive criteria were as
follows: Ovarian cancer as the first tumor; no radiotherapy or
chemotherapy treatment before admission; and all specimens
histologically confirmed with complete clinical data. Exclusive
criteria were as follows: Borderline OC or OC in combination with
other malignant tumors or abnormal liver and kidney; severe blood
coagulation disorders; and primary cardiovascular and
cerebrovascular diseases. The detailed clinical characteristics of
these patients and the healthy controls are shown in Table I. Written, informed consent was
obtained from all subjects prior to participation, and the study
was approved by the ethics committee of the Third Military Medical
University in Chongqing, China.
 | Table I.Patient clinicopathological
parameters. |
Table I.
Patient clinicopathological
parameters.
| Clinicopathological
parameters | Peripheral blood
samples, n=96 | Tissue samples,
n=15 |
|---|
| Age (years) | 37-68 | 37-68 |
| Pathological grade,
well + moderately differentiated/poorly differentiated | 45/51 | 4/11 |
| Tumor grade,
T1-T2/T3-T4 | 25/71 | 3/12 |
| Lymph node
metastasis, N0/N1 | 26/70 | 3/12 |
| Distant metastasis,
M0/M1 | 93/3 | 15/0 |
| Serum CA125 (U/ml),
≤35/>35 | 25/71 | 4/11 |
| Serum HE4
(pmol/ml), ≤76.2/>76.2 | 31/65 | 4/11 |
Cell separation
Fresh peripheral blood mononuclear cells (PBMCs)
were obtained from the peripheral blood of healthy adult volunteers
and patients with OC by Ficoll-Hypaque gradient centrifugation
(Axis-Shield), according to the manufacturer's instructions. TILs
were separated from the fresh tumor tissue of 15 patients with
epithelial OC by a combination of mechanical, chemical and
enzymatic digestion. Briefly, tissues were cut into small pieces
with a surgical scissor, and were digested with type IV collagenase
and pancreatin (Gibco; Thermo Fisher Scientific, Inc.). The TILs
were then obtained by Ficoll-Hypaque gradient centrifugation.
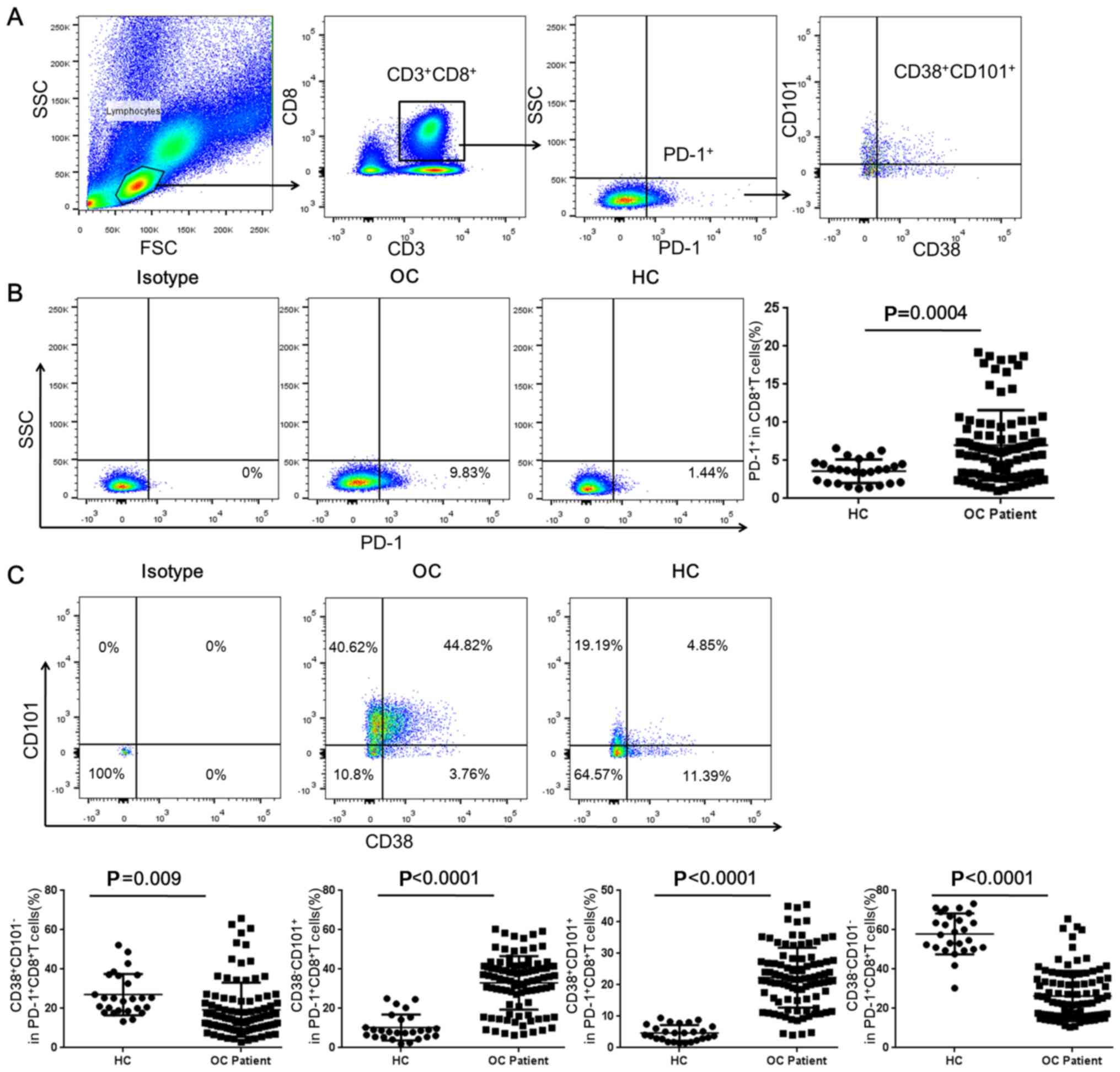
Flow cytometric analysis
The PBMCs or TILs were stained with the following
fluorochrome-labeled monoclonal antibodies (mAbs) at 4°C for 30 min
in the dark: Anti-CD3-PerCP (1:100; cat. no. 300428; BioLegend,
Inc.), anti-CD8-FITC (1:100; cat. no. 11-0086.42; eBioscience;
Thermo Fisher Scientific, Inc.), anti-PD-1-PE/Cy7 (1:100; cat. no.
329918; BioLegend, Inc.), anti-CD38-PE (1:100; cat. no. 4322550;
Invitrogen; Thermo Fisher Scientific, Inc.) and anti-CD101-APC
(1:100; cat. no. 331007; BioLegend, Inc.). Isotype control
antibodies were used to ensure accurate compensation and to set
gates. The stained cells were analyzed using a FACSCalibur flow
cytometer (BD Biosciences), and the data were analyzed with FlowJo
10 software (FlowJo LLC).
Immunofluorescence (IF) analysis
The colocalization of CD38 and CD101 was assessed by
IF staining of fresh tumor tissues and adjacent non-tumor tissues
from five patients with epithelial OC representative of the whole
cohort. For double-staining with anti-CD38 (cat. no. ZM-0422;
OriGene Technologies, Inc.) and anti-CD101 (cat. no. AG09158376;
BIOSS) antibodies, anti-CD38 (50 µl) and anti-CD101 (1:100) were
mixed and applied to slides, and subsequently incubated for 12 h at
4°C in a humidified chamber. Next, DyLight 488-labeled anti-rabbit
(1:500; cat. no. A-11008; Invitrogen, Thermo Fisher Scientific,
Inc.) and DyLight 555-labeled anti-mouse antibodies (1:500; cat.
no. A-31570; Invitrogen; Thermo Fisher Scientific, Inc.) were
applied for 60 min at 37°C. Nuclear counterstaining was performed
by incubating the slides in DAPI (1:100 in PBS; Invitrogen; Thermo
Fisher Scientific, Inc.) for 5 min at room temperature. Normal
mouse, goat or rabbit IgG (1:100; cat. no. bs-0296P; BIOSS) was
used as an isotype control. Images were obtained using an upright
fluorescence microscope at ×200 magnification (Olympus
Corporation).
Statistical analysis
All data were analyzed using SPSS statistics
software (v24.0; IBM Corp.) and GraphPad Prism software (v6.0;
GraphPad Software, Inc.). All experiments were repeated three times
and all data are presented as the mean ± SD. P<0.05 was
considered to indicate a statistically significant difference. The
patients were divided into high- and low-expression groups
according to the median value. Student's t-test was used to analyze
comparisons between two groups, and the χ2 test was
applied to analyze the associations between each cell subset and
the clinicopathological parameters of patients. The associations
between CD38/CD101 coexpression on PD-1+CD8+
T cells in PBMCs or TILs and serum CA125 or HE4 levels following
surgery and first chemotherapy in OC patients were analyzed using
nonparametric Kruskal-Wallis test.
Results
CD38/CD101 were markedly upregulated
on peripheral PD-1+CD8+ T cells of patients
with OC
PD-1 is a key checkpoint factor in immunosuppressive
pathways and an acceptable marker of immune failure. The
overexpression of PD-1 has been reported in patients with OC
compared with healthy donors (9).
Therefore, the expression of PD-1 on peripheral CD8+ T
lymphocytes was investigated in patients with OC by flow cytometry,
using the indicated gating strategies (Fig. 1A). Statistical analysis revealed that
the frequency of PD-1+CD8+ T cells in the
peripheral blood of patients with OC was significantly higher than
that in the peripheral blood of healthy controls (Fig. 1B). Further analysis of CD38 and CD101
expression on PD-1+CD8+ T cells demonstrated
that the frequencies of CD38−CD101+ and
CD38+CD101+PD-1+ CD8+ T
cells were higher in samples from patients with OC than in samples
from healthy controls. In contrast, the frequency of
CD38−CD101−PD-1+CD8+T
and
CD38+CD101−PD-1+CD8+T
cells was dramatically decreased in samples from patients with OC
compared with those from healthy controls (Fig. 1C).
Clinical significance of PD-1 and
CD38/CD101 expression on peripheral CD8+ T cells in
patients with OC
In order to explore the clinical significance of
CD38 and CD101 expression on PD-1+CD8+ T cell
subpopulations in OC patients, the associations between the
expression frequency of total peripheral
PD-1+CD8+ T or CD38/CD101-expressing
peripheral PD-1+CD8+ T cells and clinical
parameters or postoperative chemotherapy outcomes were analyzed.
According to the results, total PD-1+CD8+ T
cells and all PD-1+CD8+ T cell subsets showed
no association with age or histopathological grade of patients
(Table II and Table SI). Moreover, the frequency of total
PD-1+CD8+ T cells and positive expression of
CD38 or CD101 on PD-1+CD8+ T cell subsets
were not associated with the clinicopathological parameters of
patients (Table SI). However, the
double-positive or double-negative expression of CD38/CD101 on
PD-1+CD8+ T cell subsets was significantly
associated with tumor grade and lymph node metastasis (Table II).
 | Table II.Association between CD38/CD101
coexpression in PD-1+CD8+ T cells and
clinical parameters of patients with ovarian cancer. |
Table II.
Association between CD38/CD101
coexpression in PD-1+CD8+ T cells and
clinical parameters of patients with ovarian cancer.
|
|
|
PD-1+CD38+
CD101+ |
|
PD-1+CD38−
CD101− |
|
|---|
|
|
|
|
|
|
|
|---|
| Clinicopathological
parameters | n | Low | High | P-value | Low | High | P-value |
|---|
| Age (years) |
|
|
| 0.537 |
|
| 0.537 |
|
<55 | 54 | 29 | 25 |
| 25 | 29 |
|
|
≥55 | 42 | 19 | 23 |
| 23 | 19 |
|
| Pathological
grade |
|
|
| 0.101 |
|
| 0.220 |
|
Well/moderately differentiated
(G1-G2) | 45 | 27 | 18 |
| 19 | 26 |
|
| Poorly
differentiated (G3) | 51 | 21 | 30 |
| 29 | 22 |
|
| Tumor grade |
|
|
| 0.019 |
|
| 0.019 |
|
T1-T2 | 25 | 18 | 7 |
| 7 | 18 |
|
|
T3-T4 | 71 | 30 | 41 |
| 41 | 30 |
|
| Lymph node
metastasis |
|
|
| 0.002 |
|
| 0.038 |
| N0 | 26 | 20 | 6 |
| 8 | 18 |
|
| N1 | 70 | 28 | 42 |
| 40 | 30 |
|
Similarly, the frequency of total
PD-1+CD8+ T cells and positive expression of
CD38 or CD101 on PD-1+CD8+ T cell subsets was
not associated with the therapeutic effect of chemotherapy
following surgical resection (Fig.
S1), whereas double-positive or double-negative expression of
CD38/CD101 on PD-1+CD8+ T cell subsets were
significantly associated with the therapeutic effect (Fig. 2).
Expression of CD38/CD101 on
CD8+ T cells among TILs from patients with OC and
clinical significance
TILs were isolated from OC tissues, and expression
frequencies of PD-1, CD38 and CD101 on CD8+ T cells from
OC TILs were determined separately by flow cytometry. Similar to
the observations in peripheral blood, the frequency of total
PD-1+CD8+ T cells and positive expression of
CD38 or CD101 on PD-1+CD8+ T cell subsets
were not associated with the clinicopathological parameters of
patients except that CD38 expression on
PD-1+CD8+ T cells was associated with the
pathological grade (P=0.037; Figs.
3A and S2A). In contrast,
double positive or double negative expression of CD38/CD101 on
PD-1+CD8+ T cell subsets was significantly
associated with lymph node metastasis (Fig. 3A).
Additionally, the frequency of total
PD-1+CD8+ T cells and positive expression of
CD38 or CD101 on PD-1+CD8+ T cell subsets was
not associated with the therapeutic effect of chemotherapy
following surgical resection (Fig.
S2B). However, both double-positive and double-negative
expression of CD38/CD101 on PD-1+CD8+ T cell
subsets demonstrated significant association with the therapeutic
effect (Fig. 3B).
Colocalization of CD38 and CD101 on
TILs from OC tissues
The flow cytometry results indicated that the levels
of CD38+CD101+ T cells were significantly
increased in OC tissues. Thus, double-IF staining was conducted in
order to assess whether CD38 and CD101 are able to colocalize on
TILs from OC tissues. The results showed that both CD38 and CD101
were highly expressed in OC tissues, and some staining revealed
colocalization of the two markers on TILs. In contrast, almost no
CD38 and CD101 expression was observed in adjacent tissues
(Fig. 4).
Discussion
The immune system plays a crucial role in the
antitumor process. On one hand, the immune system can monitor and
eliminate tumor cells and prevent the development of tumors. On the
other hand, in a complex TME, tumor cells exert an inhibitory
effect on the immune system, allowing tumor cells to evade immune
surveillance, and rapidly multiply and metastasize in vivo
(10). T cells differentiate from
lymphatic stem cells in the thymus, and are the most complex type
of lymphocytes (11). Among T cells,
killer T cells, which are also called cytotoxic T cells, release
perforin/granzyme, and cytokines such as IFN-γ and TNF-α to kill
target cells, including cells infected by pathogens and cells
expressing tumor-specific antigens (12). To ensure that T cells are not
overstimulated, activated T cells also express coinhibitory
molecules, mainly cytotoxic T-lymphocyte-associated protein 4-B7
and PD-1/PD-L1, which regulate their activity (13–15).
However, the TME usually induces CD8+ T
cells to overexpress immunosuppressive molecules such as PD-1;
binding of PD-1 with PD-L1, a ligand on the surface of tumor cells,
significantly inhibits the ability of CD8+ CTLs to
eliminate tumor cells (5). It is
widely known that the binding of PD-1 with PD-L1 activates a
critical immune checkpoint, leading to T cell dysfunction,
exhaustion and tolerance (16–18).
Moreover, high-affinity anti-PD-1 or anti-PD-L1 mAbs, which block
the PD-1-PD-L1 interaction, can reverse the immune checkpoint,
releasing the repression of T cell responses (19). However, previous studies have also
shown that certain CD8+ T cells can enter an
irreversible dysfunctional state that cannot be rescued by
PD-1/PD-L1 blockade. In the majority of advanced tumors, with the
exception of Hodgkin's lymphoma and melanoma, the objective
response rate with anti-PD-1/PD-L1 monotherapy is only ~20%
(20), which strongly suggests that
PD-1+CD8+ T cells may comprise a highly
heterogeneous population, of which a certain subpopulation may
determine the effects of PD-1 blockade immunotherapy.
Recently, Schietinger et al (7) demonstrated that tumor-transformed
tissues express tumor-specific antigens during tumorigenesis. In
the noninflammatory TME, a small number of inhibitory receptors
expressed in original tumor-specific CD8+ T cells
disrupt CD8+ T cell function; this dysfunction is
reversible during the early stages of malignancy (state 1).
However, during persistent antigen stimulation, CD8+ T
cells continuously upregulate the expression of inhibitory
receptors such as PD-1, thus causing irreversible dysfunction of
CD8+ T cells and loss of the killing effect of
CD8+ T cells against tumors, which contributes to tumor
immune escape and unregulated growth (state 2) (7,21).
Notably, Schietinger et al (7) further reported that CD8+ T
cells in state 1 exhibit low levels of CD38 and CD101 coexpression,
and can recover the ability to secrete IFN-γ and TNF-α following
in vitro stimulation to kill tumors, and that
CD8+ T cells in state 2 strongly coexpress CD38 and
CD101, and lose their ability to secrete IFN-γ and TNF-α despite
several rounds of stimulation (8).
These results indicate that PD-1+CD8+ T cells
can be subgrouped into several subpopulations according to their
CD38 and CD101 expression. This hypothesis may explain the
observation that, although PD-1/PD-L1 blockade with neutralizing
antibodies has achieved great clinical success in combating certain
cancer types, and long-lasting responses can be achieved in
patients (22,23), clinical trials have demonstrated that
the majority of patients with PD-L1+/PD-1+
expression do not respond to PD-1/PD-L1 blockade (20).
The aforementioned studies also suggest that the
frequency of PD-1+CD8+ T cell subsets with
different CD38/CD101 expression patterns may be a key indicator of
tumor prognosis. To verify this hypothesis, the association of
CD38/CD101 expression in PD-1+CD8+ T cells
with clinical parameters and postoperative chemotherapy outcomes in
patients OC was analyzed in the present study. The results
demonstrated that the proportion of CD38/CD101-coexpressing
PD-1+CD8+ T cells significantly increased and
the proportion of CD38/CD101 double-negative
PD-1+CD8+ T cells was markedly decreased in
peripheral blood and tumor tissues of patients with OC compared
with the proportions in paracancerous tissues. The frequency of
PD-1+CD38+CD101+CD8+ T
cells was associated with clinical stage, lymph node metastasis and
postoperative chemotherapy outcomes in patients with OC but not
with age or histological grade. A higher level of CD38 and CD101
expression was associated with a higher degree of malignancy in OC
and worse postoperative chemotherapy outcomes. Therefore, the
coexpression of CD38 and CD101 in PD-1+CD8+ T
cells may be used as an indicator of adjuvant diagnosis and
prognosis in patients with OC, and may serve as an effective
adjuvant biological index for determining the applicability of
anti-PD-1 immunotherapy in patients with OC.
CD38 is a 45-kDa single-chain transmembrane
glycoprotein that localizes to the cell membrane. The expression of
CD38 in human peripheral blood lymphocytes varies with age
(24). The first indicator that CD38
may be involved in signal transduction was due to the fact that the
interaction between CD38 and ligands on PBMCs and T cell lines can
induce activation and proliferation signals (24). Furthermore, studies on hepatitis B
virus and human immunodeficiency virus have shown that, since CD38
induces T cell activation via external signals, CD38+
can be used as a T cell activation marker (25,26).
CD101 is a 240-kDa disulfide-linked homodimeric type I glycoprotein
(27) that was considered to play a
costimulatory role in T cell receptor/CD3-mediated T cell
activation. A mAb against CD101 inhibits allogeneic T cell
responses (28). Therefore, CD38 and
CD101 are viewed as markers of T cell activation (24,29);
however, the overexpression of these factors may also be considered
an exhaustion marker due to overactivation of T cells, particularly
when these factors are highly expressed in
PD-1+CD8+ T cells. The expression of PD-1 was
significantly increased following T cell activation to limit T cell
overactivation; thus, sustained high expression of PD-1 in T cells
has been viewed as a marker of T cell exhaustion. It is reasonable
to propose that high CD38, CD101 and PD-1 expression in
CD8+ T cells represents the irreversible state 2 of
CD8+ T cells. Hence, a significant increase in
CD38+CD101+PD-1+CD8+T
cells would predict poor clinical status and treatment outcomes for
patients with OC, which is supported by the data in the present
study, i.e., CD38/CD101 coexpression levels in PBMCs and TILs in
patients with terminal-stage OC were much higher than those in
patients with early-stage OC.
CA125 is currently the most commonly used biomarker
for OC (30,31); it is employed as a diagnostic tool to
assess the effect of OC treatment and to monitor recurrence
(32,33). HE4 is considered a potential
biomarker for OC because it is expressed in 32% of patients with OC
without CA125 expression, and the Food and Drug Administration has
approved HE4 for monitoring disease recurrence in patients with OC
(34). Thus, the combination of
serum CA125 and HE4 measurements may improve evaluations of
malignancy prognosis in ovarian tumors (35,36). The
present study demonstrated that patients with OC and a higher
frequency of
CD38+CD101+PD-1+CD8+ T
cells exhibited higher CA125 and HE4 levels upon chemotherapy
following surgical resection compared with those of patients with a
lower frequency of
CD38+CD101+PD-1+CD8+ T
cells. Thus, the hypothesis that coexpression of CD38/CD101 on
PD-1+CD8+ T cells is an indicator of worse
prognosis in patients with OC is further supported.
In conclusion, the present study is the first to
demonstrate an association between the coexpression of CD38/CD101
in PD-1+CD8+ T cells and the clinical stage,
lymph node metastasis of patients with OC; by contrast, total
PD-1+CD8+ T cells alone among TILs or PBMCs
do not reflect disease status or prognosis. These observations are
in line with a previous study, in which CD38/CD101 protein
coexpression was suggested to represent a more useful predictor of
diagnosis and prognosis for patients with pancreatic cancer
compared with PD-1 alone (37).
However, the present study further suggested that the coexpression
of CD38/CD101 by peripheral PD-1+CD8+ T cells
and TILs may serve as a new indicator for the treatment efficacy of
patients with OC and as an indicator for the selection of patient
populations for further immunotherapy by immune checkpoint
blockade. However, the detection of CD38/CD101 coexpression in
PD-1+CD8+T cells in the present study relied
on flow cytometry analysis, and therefore this method would be more
expensive than routine ELISA detection of levels of CA125, HE4 and
other serum biomarkers. Accordingly, cost is one of the limitations
of the strategy for OC diagnosis described in this study.
Although the coexpression of CD38/CD101 in
PD-1+CD8+ T cells is a potential novel
biomarker for the diagnosis and treatment of OC, which is strongly
associated with serum levels of CA125 and HE4, other helpful
biomarkers of OC diagnosis and treatment exist (38). For instance, osteopontin (OPN) has
been used as a biomarker for the diagnosis and treatment of several
cancer types, such as ovarian cancer, breast cancer, colorectal
cancer and osteosarcoma (39–41). OPN
is a secreted extracellular matrix glycoprotein that is involved in
a number of cellular processes, including wound healing,
inflammation, immune response and tumorigenesis (40). As OPN is usually overexpressed in
several cancer types, including OC, an increase in serum OPN is
often used to assess the diagnosis and prognosis of various human
cancer types, including breast, lung, gastric and ovarian cancer,
as well as melanoma (39–41). Therefore, in the future, the combined
application of several biomarkers, such as CA125 and OPN, as well
as the expression of CD38/CD101 in PD-1+CD8+
T cells, may provide more accurate and sensitive diagnoses and/or
treatment indicators for patients with OC.
Supplementary Material
Supporting Data
Acknowledgements
Not applicable.
Funding
This study was supported by the National Key
Research and Development Project (grant no. 2016YFA0502203).
Availability of data and materials
The datasets used and/or analyzed during the
present study are available from the corresponding author upon
reasonable request
Authors' contributions
JZ and WW performed the main experiments in this
study. WH and DW performed the clinical data collection and
statistical analysis. ZL provided the clinical samples and
interpreted the clinical data of patients. BN, WH and DW designed
the study and drafted the manuscript. All authors read and approved
the final manuscript.
Ethics approval and consent to
participate
The study was approved by the ethics committee of
the Third Military Medical University (Chongqing, China). Written,
informed consent was obtained from all subjects prior to
participation.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2017. CA Cancer J Clin. 67:7–30. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Miller EM, Tymon-Rosario J, Strickler HD,
Xie X, Xue X, Kuo DYS, Makhija SK and Nevadunsky NS: Racial
differences in survival from epithelial ovarian cancer are
associated with stage at diagnosis and use of neoadjuvant therapy:
A 10-year single-institution experience with a racially diverse
urban population. Int J Gynecol Cancer. 28:749–756. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Dong X, Men X, Zhang W and Lei P: Advances
in tumor markers of ovarian cancer for early diagnosis. Indian J
Cancer. 51 (Suppl 3):e72–e76. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Santoiemma PP and Powell DJ Jr: Tumor
infiltrating lymphocytes in ovarian cancer. Cancer Biol Ther.
16:807–820. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Prosser ME, Brown CE, Shami AF, Forman SJ
and Jensen MC: Tumor PD-L1 co-stimulates primary human CD8(+)
cytotoxic T cells modified to express a PD1:CD28 chimeric receptor.
Mol Immunol. 51:263–272. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Festino L, Botti G, Lorigan P, Masucci GV,
Hipp JD, Horak CE, Melero I and Ascierto PA: Cancer treatment with
anti-PD-1/PD-L1 agents: Is PD-L1 expression a biomarker for patient
selection? Drugs. 76:925–945. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Schietinger A, Philip M, Krisnawan VE,
Chiu EY, Delrow JJ, Basom RS, Lauer P, Brockstedt DG, Knoblaugh SE,
Hämmerling GJ, et al: Tumor-specific T cell dysfunction is a
dynamic antigen-driven differentiation program initiated early
during tumorigenesis. Immunity. 45:389–401. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Philip M, Fairchild L, Sun L, Horste EL,
Camara S, Shakiba M, Scott AC, Viale A, Lauer P, Merghoub T, et al:
Chromatin states define tumour-specific T cell dysfunction and
reprogramming. Nature. 545:452–456. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Rådestad E, Klynning C, Stikvoort A,
Mogensen O, Nava S, Magalhaes I and Uhlin M: Immune profiling and
identification of prognostic immune-related risk factors in human
ovarian cancer. Oncoimmunology. 8:e15357302018. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ochsenbein AF, Klenerman P, Karrer U,
Ludewig B, Pericin M, Hengartner H and Zinkernagel RM: Immune
surveillance against a solid tumor fails because of immunological
ignorance. Proc Natl Acad Sci USA. 96:2233–2238. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ada G: The enunciation and impact of
Macfarlane Burnet's clonal selection theory of acquired immunity.
Immunol Cell Biol. 86:116–118. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Reimann J, Böhm W and Schirmbeck R:
Alternative processing pathways for MHC class I-restricted epitope
presentation to CD8+ cytotoxic T lymphocytes. Biol Chem Hoppe
Seyler. 375:731–736. 1994.PubMed/NCBI
|
|
13
|
Wei F, Zhong S, Ma Z, Kong H, Medvec A,
Ahmed R, Freeman GJ, Krogsgaard M and Riley JL: Strength of PD-1
signaling differentially affects T-cell effector functions. Proc
Natl Acad Sci USA. 110:E2480–E2489. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Arasanz H, Gato-Cañas M, Zuazo M,
Ibañez-Vea M, Breckpot K, Kochan G and Escors D: PD1 signal
transduction pathways in T cells. Oncotarget. 8:51936–51945. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Srinivasan P, Wu X, Basu M, Rossi C and
Sandler AD: PD-L1 checkpoint inhibition and anti-CTLA-4 whole tumor
cell vaccination counter adaptive immune resistance: A mouse
neuroblastoma model that mimics human disease. PLoS Med.
15:e10024972018. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ishida Y, Agata Y, Shibahara K and Honjo
T: Induced expression of PD-1, a novel member of the immunoglobulin
gene superfamily, upon programmed cell death. EMBO J. 11:3887–3895.
1992. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Freeman GJ, Long AJ, Iwai Y, Bourque K,
Chernova T, Nishimura H, Fitz LJ, Malenkovich N, Okazaki T, Byrne
MC, et al: Engagement of the PD-1 immunoinhibitory receptor by a
novel B7 family member leads to negative regulation of lymphocyte
activation. J Exp Med. 192:1027–1034. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Dong H, Zhu G, Tamada K and Chen L: B7-H1,
a third member of the B7 family, co-stimulates T-cell proliferation
and interleukin-10 secretion. Nat Med. 5:1365–1369. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Wang C, Thudium KB, Han M, Wang XT, Huang
H, Feingersh D, Garcia C, Wu Y, Kuhne M, Srinivasan M, et al: In
vitro characterization of the anti-PD-1 antibody nivolumab,
BMS-936558, and in vivo toxicology in non-human primates. Cancer
Immunol Res. 2:846–856. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Xu-Monette ZY, Zhang M, Li J and Young KH:
PD-1/PD-L1 blockade: Have we found the key to unleash the antitumor
immune response? Front Immunol. 8:15972017. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hellström I, Hellström KE, Pierce GE and
Yang JP: Cellular and humoral immunity to different types of human
neoplasms. Nature. 220:1352–1354. 1968. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Brahmer J, Reckamp KL, Baas P, Crinò L,
Eberhardt WE, Poddubskaya E, Antonia S, Pluzanski A, Vokes EE,
Holgado E, et al: Nivolumab versus docetaxel in advanced
squamous-cell non-small-cell lung cancer. N Engl J Med.
373:123–135. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Robert C, Long GV, Brady B, Dutriaux C,
Maio M, Mortier L, Hassel JC, Rutkowski P, McNeil C,
Kalinka-Warzocha E, et al: Nivolumab in previously untreated
melanoma without BRAF mutation. N Engl J Med. 372:320–330. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Quarona V, Zaccarello G, Chillemi A,
Brunetti E, Singh VK, Ferrero E, Funaro A, Horenstein AL and
Malavasi F: CD38 and CD157: A long journey from activation markers
to multifunctional molecules. Cytometry B Clin Cytom. 84:207–217.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
d'Ettorre G, Ceccarelli G, Serafino S,
Giustini N, Cavallari EN, Bianchi L, Pavone P, Bellelli V,
Turriziani O, Antonelli G, et al: Dominant enrichment of
phenotypically activated CD38(+) HLA-DR(+) CD8(+) T cells, rather
than CD38(+) HLA-DR(+) CD4(+) T cells, in HIV/HCV coinfected
patients on antiretroviral therapy. J Med Virol. 88:1347–1356.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Mao X, Peng L, Liu X, Yang Y, Wang Q, Wang
D, Xiao J and Leng J: TLR9 expression is positively correlated with
the levels of CD38, HLA-DR and CD95 on peripheral blood mononuclear
cells in chronic HBV infected patients. Xi Bao Yu Fen Zi Mian Yi
Xue Za Zhi. 32:660–665. 2016.(In Chinese). PubMed/NCBI
|
|
27
|
Rivas A, Ruegg CL, Zeitung J, Laus R,
Warnke R, Benike C and Engleman EG: V7, a novel leukocyte surface
protein that participates in T cell activation. I. Tissue
distribution and functional studies. J Immunol. 154:4423–4433.
1995.PubMed/NCBI
|
|
28
|
Soares LR, Tsavaler L, Rivas A and
Engleman EG: V7 (CD101) ligation inhibits TCR/CD3-induced IL-2
production by blocking Ca2+ flux and nuclear factor of
activated T cell nuclear translocation. J Immunol. 161:209–217.
1998.PubMed/NCBI
|
|
29
|
Gouttefangeas C, Jacquot S, Meffre E,
Schmid M, Boumsell L and Bensussan A: Differential proliferative
responses in subsets of human CD28+ cells delineated by BB27 mAb.
Int Immunol. 6:423–430. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Urban N, Mcintosh MW, Andersen M and
Karlan BY: Ovarian cancer screening. Hematol Oncol Clin North Am.
17989–1005. (ix)2003. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Urban N and Drescher C: Current and future
developments in screening for ovarian cancer. Womens Health (Lond).
2:733–742. 2006.PubMed/NCBI
|
|
32
|
Kafali H, Artunc H and Erdem M: Evaluation
of factors that may be responsible for cyclic change of CA125
levels during menstrual cycle. Arch Gynecol Obstet. 275:175–177.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Bast RC Jr, Badgwell D, Lu Z, Marquez R,
Rosen D, Liu J, Baggerly KA, Atkinson EN, Skates S, Zhang Z, et al:
New tumor markers: CA125 and beyond. Int J Gynecol Cancer. 15
(Suppl 3):S274–S281. 2005. View Article : Google Scholar
|
|
34
|
Rosen DG, Wang L, Atkinson JN, Yu Y, Lu
KH, Diamandis EP, Hellstrom I, Mok SC, Liu J and Bast RC Jr:
Potential markers that complement expression of CA125 in epithelial
ovarian cancer. Gynecol Oncol. 99:267–277. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Zhao T and Hu W: CA125 and HE4:
Measurement tools for ovarian cancer. Gynecol Obstet Invest.
81:430–435. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Xi QP, Pu DH and Lu WN: Research on
application value of combined detection of serum CA125, HE4 and TK1
in the diagnosis of ovarian cancer. Eur Rev Med Pharmacol Sci.
21:4536–4541. 2017.PubMed/NCBI
|
|
37
|
Zhang M, Yang J, Zhou J, Gao W, Zhang Y,
Lin Y, Wang H, Ruan Z and Ni B: Prognostic values of
CD38+CD101+PD1+CD8+ T
cells in pancreatic cancer. Immunol Invest. 48:466–479. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Kumari S: Serum biomarker based algorithms
in diagnosis of ovarian cancer: A review. Indian J Clin Biochem.
33:382–386. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Hu ZD, Wei TT, Yang M, Ma N, Tang QQ, Qin
BD, Fu HT and Zhong RQ: Diagnostic value of osteopontin in ovarian
cancer: A meta-analysis and systematic review. PLoS One.
10:e01264442015. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Wei R, Wong JPC and Kwok HF: Osteopontin-a
promising biomarker for cancer therapy. J Cancer. 8:2173–2183.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Han X, Wang W, He J, Jiang L and Li X:
Osteopontin as a biomarker for osteosarcoma therapy and prognosis.
Oncol Lett. 17:2592–2598. 2019.PubMed/NCBI
|