Introduction
Thyroid cancer is a common malignant endocrine tumor
that has a good prognosis, while 15-20% of patients with
differentiated thyroid cancer (DTC) and most patients with
anaplastic thyroid cancer (ATC) still have drug resistance to
standard regimens, such as radioactive iodine (RAI) treatment
(1). The incidence rate of the
disease has increased over the past few decades and nearly tripled
in the United States between 1975 and 2009. Despite the increasing
incidence rate, the mortality rate of the disease remains stable
(2). According to a study, thyroid
cancer was the fifth most common cancer threatening women after
breast cancer, lung cancer, colon cancer and uterine cancer in
Canada in 2016 (3). Thyroid cancer
consists of papillary, follicular, medullary and anaplastic thyroid
cancers, among which papillary thyroid cancer is the most common
one. Tumor is currently treated by chemotherapy, and the patients
are treated with liquid medicine during hospitalization for a long
time. Permanent needle of deep venipuncture reduces the stimulation
to the vein and skin and better injects liquid medicine, which is
commonly used in intensive care and conducive to carrying out
central venous pressure monitoring, blood transfusion, hemodialysis
and total parenteral nutrition (4).
Both peripherally inserted central catheters (PICC)
and totally implantable venous-access ports (TIVAP) are currently
commonly used techniques for central venous catheterization, while
their effects on chemotherapy are different. Studies have shown
that PICC based on the patient's condition is usually safe and
convenient (5), and may be
significantly superior in patients with advanced cancer compared
with subcutaneous and peripheral venous catheters. For example,
PICC has a strong analgesic effect, causes less surgery-related
pain and provides fluid therapy. Additionally, more drugs whose
dosages are adjustable are available. It has also been shown that
PICC has a high success rate without severe surgery-related
complication. According to a study, the success rate of PICC is
~85-95% in patients without related complications (6). TIVAP, a totally implantable vascular
access system, provides long-term venous vascular access and plays
a vital role in the treatment of patients with tumors (7). In PICC a thin and long catheter made
from a biocompatible material (silicone or polyurethane) is
percutaneously inserted into the basal vein or cephalic vein of the
forearm or anterior cubital fossa under the guidance of ultrasound
or fluoroscopy, and then advanced to the central vein. The tip of
the catheter is usually placed at the superior vena cava or the
junction between cava and atrium. Compared with other central
venous accesses, PICC has fewer complications, such as hemothorax
and pneumothorax (8). Therefore, the
application values and safety of PICC and TIVAP in chemotherapy for
patients with thyroid cancer were compared in this study to provide
references for clinical practice.
Patients and methods
General information
A retrospective analysis was performed on the
clinical data of 188 patients with thyroid cancer who were treated
with PICC or TIVAP for chemotherapy in Qingdao Municipal Hospital
(Qingdao, China) from January 2013 to March 2018. The patients were
divided into the PICC group and the TIVAP group according to deep
venous catheterization. The PICC group consisted of 44 males and 52
females, aged 20-64 years with an average age of 32.35±8.54 years.
According to the pathological type (9), 23 cases were undifferentiated, 33 cases
were papillary adenocarcinoma, 24 cases were follicular
adenocarcinoma, and 16 cases were medullary carcinoma. The TIVAP
group consisted of 40 males and 52 females, aged 21-62 years with
an average age of 31.37±8.91 years, and 19 cases were
undifferentiated, 36 cases were papillary adenocarcinoma, 23 cases
were follicular adenocarcinoma, and 14 cases were medullary
carcinoma. Inclusion criteria: Patients diagnosed by imaging system
and clinicopathology; patients who were aged >18 years (5) and had no history of mental illness;
patients who were able to communicate normally; patients with
complete clinical data; patients who or whose immediate family
members signed an informed consent form before the clinical data
were collected. Exclusion criteria: Patients with severe cardiac
and hepatic dysfunctions; patients who dropped out; patients with
malignancies other than thyroid cancer; patients who used to take
antiangiogenic drugs; patients with hypertension.
Methods
Patients in the TIVAP group were treated with TIVAP
for postoperative intravenous chemotherapy. A Groshong catheter and
3M transparent glue were used. The patient was placed in a
horizontal position with the arm extending 190 degrees and the head
deviating to the one side in order to determine the puncture site.
The biceps circumference, and the distance from the puncture point
to the right sternoclavicular joint and from the puncture point
down to the third intercostal space were measured and recorded
before puncture. After disinfection, draping and local anesthesia
were carried out within a radius of 50 cm of the puncture point,
the catheter was inserted into the vein ~20.0 cm. After the
puncture reached the axillary vein, the lower jaw of the patient
approached the shoulder on the side where the catheter was inserted
to determine the puncture site, so as to prevent the catheter from
entering the internal jugular vein. After puncture, the catheter
was fixed with sterile dressings and 3M glue. After that, chest
X-ray was carried out to determine the position of the catheter
end. Finally, the patient was instructed to undergo regular review
and pay attention to the puncture site for pain and redness.
Patients in the PICC group were treated with PICC
for postoperative intravenous chemotherapy. Under the guidance of
X-ray fluoroscopy, the catheter was percutaneously inserted into
the right subclavian vein. The patient was placed in a horizontal
position with the arm extending 190 degrees and the head deviating
to the one side in order to determine the puncture site. The biceps
circumference, and the distance from the puncture point to the
right sternoclavicular joint, and then down to the third
intercostal space were measured and recorded before puncture.
Disinfection 3 times and local anesthesia were carried out within a
radius of 50 cm of the puncture point. After the right subclavian
vein was punctured with a minimally invasive puncture needle, the
intravenous indwelling catheter was introduced through the guide
wire. After the pillow was removed and the catheter was washed, the
catheter was appropriately cut short and the puncture area was
bandaged for 24 h. After heparin saline was injected without
leakage, the skin incision was sutured and the drainage strip was
retained. For both groups of patients, indoor disinfection was
carried out before operations that were aseptic during the
operation.
Observational indexes
The success rate, indwelling time, complications,
quality of life and nursing satisfaction were compared between the
two groups. The nursing satisfaction with a total score of 10
points consisted of treatment information, complaint management,
physical environment, follow-up, hospitalization and overall
service. The higher the score was, the higher the satisfaction was.
The quality of life with a total score of 10 points consisted of
psychological function, physical function, social function and
self-evaluation. The higher the score was, the higher the
satisfaction was. The total incidence rate of complications =
(cases with local infection + cases with catheter obstruction +
cases with catheter leakage + cases with catheter
displacement)/total cases.
Statistical methods
SPSS 18.0 (IBM Corp.) was used for statistical
analysis, GraphPad Prism 7 for plotting figures. Count data were
expressed as number of cases/percentage (n/%), and Chi-square test
was used for comparison of count data between groups. Measurement
data were expressed as mean ± standard deviation (mean ± SD).
Student's t-test was used for the comparison of measurement data.
P<0.05 indicates a statistically significant difference.
Results
General information
There was no statistically significant difference
between the two groups in terms of sex, age, body weight, clinical
staging, pathological types, lymph node metastasis and lesion
characteristics (P>0.05) (Table
I).
 | Table I.General information [n(%)] (mean ±
SD). |
Table I.
General information [n(%)] (mean ±
SD).
| Groups | PICC group
(n=96) | TIVAP group
(n=92) | χ2/t
value | P-value |
|---|
| Sex |
|
| 0.105 | 0.745 |
| Male | 44 (45.83) | 40 (43.48) |
|
|
|
Female | 52 (54.17) | 52 (54.52) |
|
|
| Age (years) | 32.35±8.54 | 31.37±8.91 | 0.770 | 0.442 |
| Body weight (kg) | 61.98±5.24 | 63.45±6.78 | 0.097 | 0.097 |
| Clinical staging |
|
| 1.355 | 0.244 |
| Stages
I–II | 43 (44.79) | 38 (41.30) |
|
|
| Stages
III–IV | 53 (55.21) | 54 (58.70) |
|
|
| Pathological
types |
|
| 1.241 | 0.743 |
|
Undifferentiated | 23 (23.95) | 19 (20.65) |
|
|
| Polypoid
adenocarcinoma | 33 (34.38) | 38 (41.30) |
|
|
|
Follicular carcinoma | 24 (25.00) | 23 (25.00) |
|
|
| Medullary
carcinoma | 16 (16.67) | 12 (13.05) |
|
|
| Lymph node
metastasis |
|
| 0.637 | 0.425 |
| Yes | 29 (30.21) | 23 (25.00) |
|
|
| No | 67 (69.79) | 69 (75.00) |
|
|
| Lesion
characteristic |
|
| 0.528 | 0.468 |
|
Uninodular | 34 (35.42) | 28 (30.43) |
|
|
|
Multinodular | 62 (64.58) | 64 (69.57) |
|
|
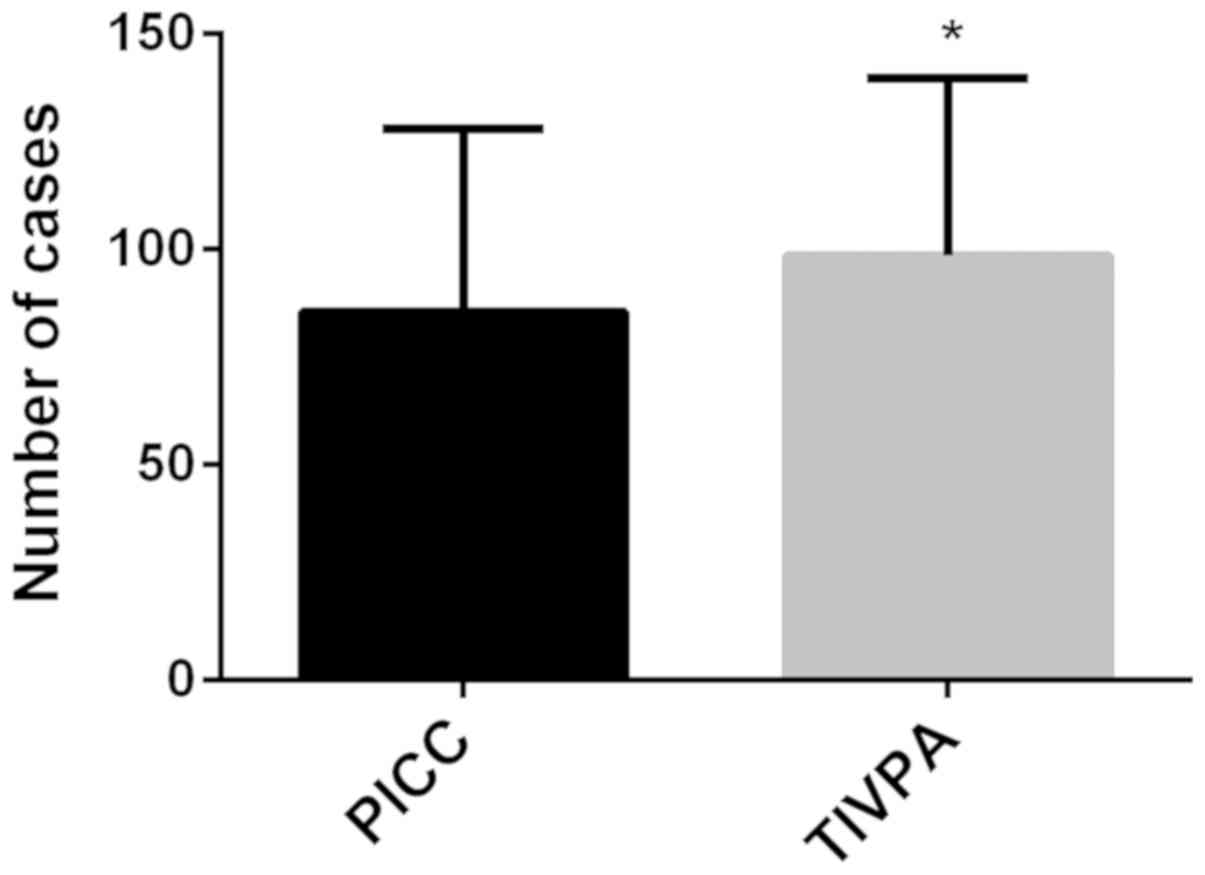
Comparison of success rate
A total of 95 cases succeeded and 1 case failed in
the PICC group, with a success rate of 98.96%. A total of 91 cases
succeeded and 1 case failed in the TIVAP group, with a success rate
of 98.91%. There was no statistically significant difference
between the two groups (χ2=0.001, P=0.982). More details
are shown in Fig. 1.
Comparison of indwelling time
The indwelling time was 98.38±41.36 days in the
TIVAP group, significantly longer than 85.37±42.48 days in the PICC
group (P<0.05) (Fig. 2).
Comparison of complications
In the PICC group, there were 3 cases with local
infection, 1 with catheter obstruction, 4 with catheter leakage and
6 with catheter displacement, with a total incidence rate of
14.58%. In the TIVAP group, there was no complication mentioned
above, with a total incidence rate of 0%. The incidence rate of
complications in the TIVAP group (0%) was significantly lower than
that in the PICC group (14.58%) (P<0.05) (Table II).
 | Table II.Comparison of complications
[n(%)]. |
Table II.
Comparison of complications
[n(%)].
| Groups | Local
infection | Catheter
obstruction | Catheter
leakage | Catheter
displacement | Total incidence
rate |
|---|
| PICC group
(n=96) | 3 (3.13) | 1 (1.04) | 4 (4.16) | 6 (6.25) | 14 (14.58%) |
| TIVAP group
(n=92) | 0 | 0 | 0 | 0 | 0 |
| χ2
value | – | – | – | – | 14.50 |
| P-value | – | – | – | – | 0.001 |
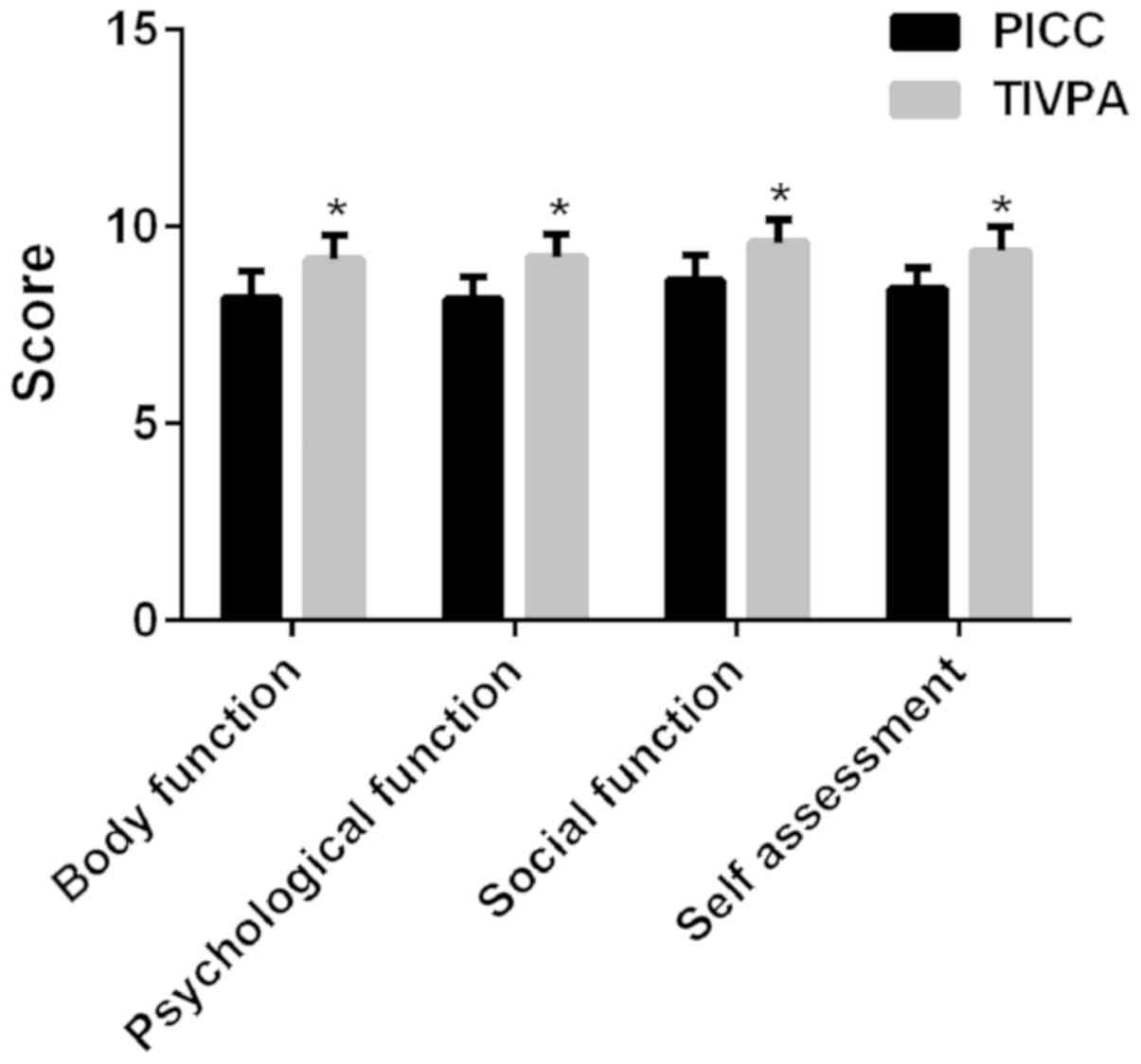
Comparison of quality of life
score
In the PICC group, the physical function was
8.21±0.66 points, the psychological function was 8.17±0.55 points,
the social function was 8.65±0.63 points and the self-evaluation
was 8.42±0.54 points. In the TIVAP group, those were respectively
9.17±0.61, 9.22±0.58, 9.59±0.58 and 9.38±0.61 points. The quality
of life scores in the PICC group were significantly lower than
those in the TIVAP group (P<0.05) (Fig. 3).
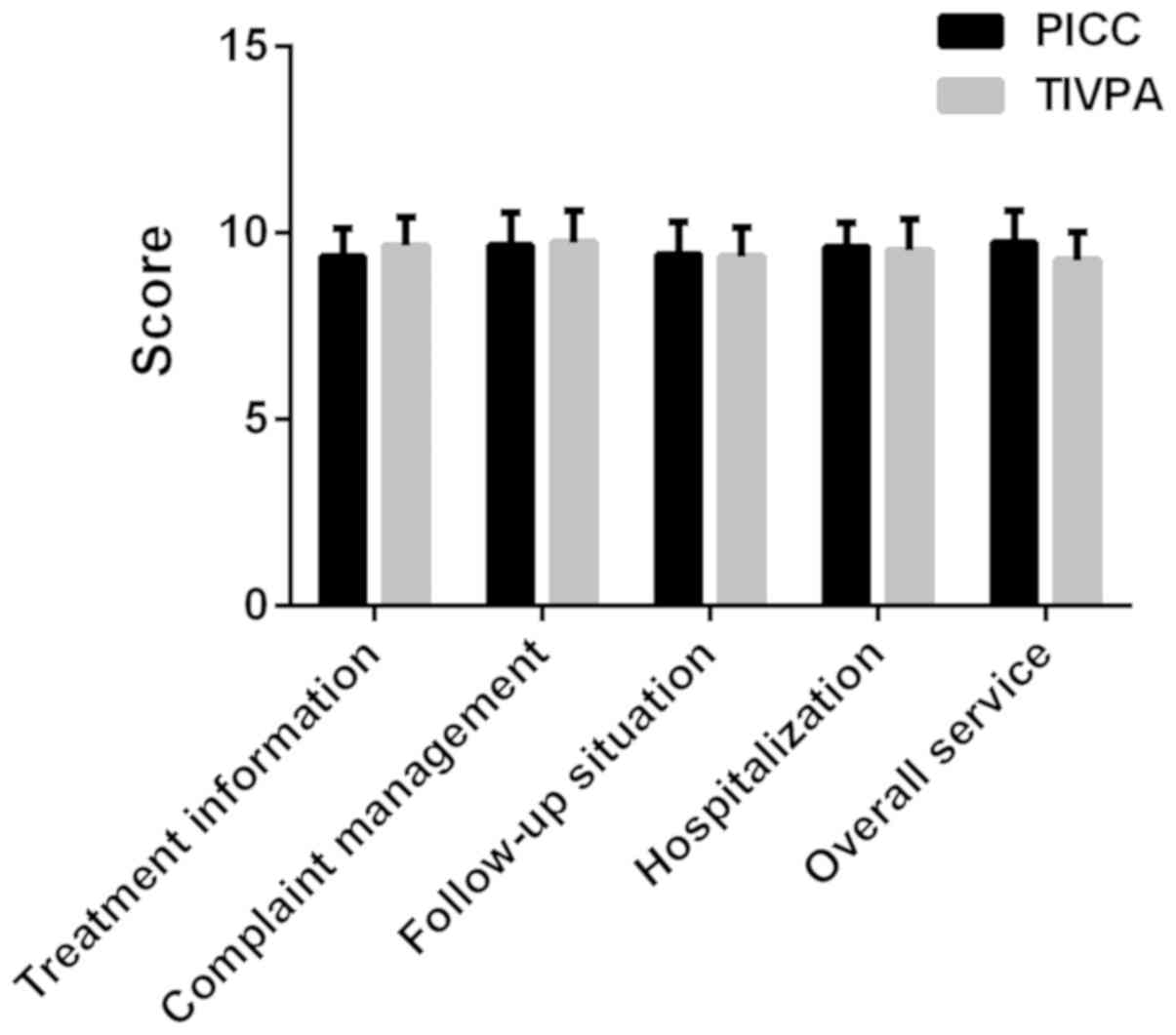
Comparison of nursing satisfaction
score
In the PICC group, the treatment information was
9.36±0.76 points, the complaint management was 9.67±0.73 points,
the follow-up was 9.42±0.86 points, the hospitalization was
9.62±0.65 points and the overall service was 9.73±0.86 points. In
the TIVAP group, those were, respectively, 9.65±0.77, 9.73±0.86,
9.73±0.86, 9.52±0.83 and 9.26±0.75 points. There was no
statistically significant difference in the nursing satisfaction
scores between the two groups (P>0.05) (Fig. 4).
Discussion
As a common malignant endocrine tumor that has an
increasing incidence rate, a high recurrence rate or high
persistence but a low mortality rate, thyroid cancer has different
histological types and subtypes, as well as cell sources,
characteristics and prognoses (10).
Central venous access devices (CVADs) provide an access to the
larger vascular system for peripheral treatment, contraindication
treatment, long-term treatment, venous monitoring and blood
sampling. Patients who require CVADs are heterogeneous, and they
have different ages and acute and chronic diseases, as well as
hospital and community care. CVADs such as long- or short-term
treatment and continuous or intermittent treatment are alternative
and patients can choose types based on their conditions (11–14).
While CVADs are clinically popular, their complications such as
blood infection are still common and considered to cause damage to
patients, negatively affecting the healthcare cost of the patients.
At present, the prevention of CVADs-related injuries is taken into
consideration of healthcare researchers, clinicians and patients
(15). PICC is commonly used medical
equipment for saving life (16).
Usually inserted into peripheral deep veins (bonethirst, brachium,
head and armpit), the catheters are used for blood sampling, drug,
liquid and nutrient delivery through the superior vena cava
(17). PICC is suitable for
long-term or frequent treatment, chemotherapy and infusion of
irritant drugs, especially for patients who cannot be treated with
PICC through the vein (18).
However, the failure of PICC leads to poor experience, including
stabbing pain and increase in hospital stay, equipment cost and
work (19). TIVAP is a widely used
intermittent central venous access, especially suitable for
patients with cancers, and its ports have higher safety margin
compared with other long-term venous access devices (20). It is generally used for patients who
require long-term or repeated treatment, such as antitumor
chemotherapy, parenteral nutrition and blood transfusion. TIVAP
causes infection and even endangers lives even though the risk of
infection is low. Pocket or subcutaneous tunnel infection is
probably caused by TIVAP that should be removed immediately
(21). PICC (22,23) and
TIVAP (24,25) provide effective deep venous accesses
for patients with tumors, but they have their own advantages and
disadvantages. Therefore, the application values and safety of PICC
and TIVAP in chemotherapy for patients with thyroid cancer were
compared in this study to provide references for clinical
practice.
In this study, the success rate in the PICC group
was 98.96% (95/96) and that in the TIVAP group was 98.91% (91/92),
without statistically significant difference; the indwelling time
in the TIVPA group was significantly longer than that in the PICC
group; the incidence rate of complications in the TIVPA group was
significantly lower than that in the PICC group. A retrospective
study of 1,254 patients with TIVAP implantation showed that the
success rate was 99.9% and the incidence of complications was 5%
(26). Another study observed 1,183
patients implanted with TIVAP for 30 days and found that only 0.6%
of patients had catheter-related infections (27). A recent study showed that PICC had a
higher risk of catheter-related deep vein thrombosis and other
adverse events than TIVAP (28). Our
results are similar to the above findings, which further suggests
that TIVAP is more secure and effective than PICC. In this study,
the physical function, psychological function, social function and
self-evaluation scores in the TIVAP group were significantly higher
than those in the PICC group, whereas there was no statistically
significant difference in the nursing satisfaction score between
the two groups. Biacchi et al (29) found that compared with PICC, TIVAP
management was simpler, provided better quality of life for
patients and reduced complications. In a study by Patel et
al (30), TIVAP was superior to
PICC in the quality of life but inferior in medical expenses. PICC
has a high incidence rate of infection due to the indwelling
catheter in vitro, so the patients should go to the hospital
regularly for local skin management in order to prevent
infection.
In conclusion, both PICC and TIVAP provide a deep
venous access, but TIVAP has a low incidence rate of complications,
higher safety and better improvement in quality of life. Therefore,
TIVAP is better for chemotherapy in patients with thyroid cancer,
worthy of clinical promotion.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
FQ compared the complications and the quality of
life and wrote the manuscript. HC analyzed and interpreted the
patient data. XY performed the experiment and designed the study.
LZ was responsible for the analysis and discussion of the data. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Qingdao Municipal Hospital (Qingdao, China). Patients who
participated in this research, signed an informed consent and had
complete clinical data.
Patients consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Asna N, Livoff A, Batash R, Debbi R,
Schaffer P, Rivkind T and Schaffer M: Radiation therapy and
immunotherapy-a potential combination in cancer treatment. Curr
Oncol. 25:e454–e460. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Pajamäki N, Metso S, Hakala T, Ebeling T,
Huhtala H, Ryödi E, Sand J, Jukkola-Vuorinen A, Kellokumpu-Lehtinen
PL and Jaatinen P: Long-term cardiovascular morbidity and mortality
in patients treated for differentiated thyroid cancer. Clin
Endocrinol (Oxf). 88:303–310. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Topstad D and Dickinson JA: Thyroid cancer
incidence in Canada: A national cancer registry analysis. CMAJ
Open. 5:E612–E616. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hazama S, Tamada K, Yamaguchi Y, Kawakami
Y and Nagano H: Current status of immunotherapy against
gastrointestinal cancers and its biomarkers: Perspective for
precision immunotherapy. Ann Gastroenterol Surg. 2:289–303. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Gao Y, Liu Y, Ma X, Wei L, Chen W and Song
L: The incidence and risk factors of peripherally inserted central
catheter-related infection among cancer patients. Ther Clin Risk
Manag. 11:863–871. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Osmani L, Askin F, Gabrielson E and Li QK:
Current WHO guidelines and the critical role of immunohistochemical
markers in the subclassification of non-small cell lung carcinoma
(NSCLC): Moving from targeted therapy to immunotherapy. Semin
Cancer Biol. 52:103–109. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Cheng F, Liang H, Butte AJ, Eng C and
Nussinov R: Personal mutanomes meet modern oncology drug discovery
and precision health. Pharmacol Rev. 71:1–19. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Johansson E, Hammarskjöld F, Lundberg D
and Arnlind MH: Advantages and disadvantages of peripherally
inserted central venous catheters (PICC) compared to other central
venous lines: A systematic review of the literature. Acta Oncol.
52:886–892. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Cooper DS, Doherty GM, Haugen BR, Kloos
RT, Lee SL, Mandel SJ, Mazzaferri EL, McIver B, Pacini F,
Schlumberger M, et al American Thyroid Association (ATA) Guidelines
Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer, :
Revised American Thyroid Association management guidelines for
patients with thyroid nodules and differentiated thyroid cancer:
The American Thyroid Association (ATA) guidelines taskforce on
thyroid nodules and differentiated thyroid cancer. Thyroid.
19:1167–1214. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Xing M: Molecular pathogenesis and
mechanisms of thyroid cancer. Nat Rev Cancer. 13:184–199. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Loveday HP, Wilson JA, Pratt RJ, Golsorkhi
M, Tingle A, Bak A, Browne J, Prieto J and Wilcox M; UK Department
of Health, : epic3: National evidence-based guidelines for
preventing healthcare-associated infections in NHS hospitals in
England. J Hosp Infect. 86 (Suppl 1):S1–S70. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Taylor JE, McDonald SJ and Tan K:
Prevention of central venous catheter-related infection in the
neonatal unit: A literature review. J Matern Fetal Neonatal Med.
28:1224–1230. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Davis MH: Pediatric central venous
catheter management: A review of current practice. JAVA. 18:93–98.
2013. View Article : Google Scholar
|
|
14
|
McMullan C, Propper G, Schuhmacher C,
Sokoloff L, Harris D, Murphy P and Greene WH: A multidisciplinary
approach to reduce central line-associated bloodstream infections.
Jt Comm J Qual Patient Saf. 39:61–69. 2013.PubMed/NCBI
|
|
15
|
Broadhurst D, Moureau N and Ullman AJ;
World Congress of Vascular Access (WoCoVA) Skin Impairment
Management Advisory Panel, : Management of central venous access
device-associated skin impairment: An evidence-based algorithm. J
Wound Ostomy Continence Nurs. 44:211–220. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Schiffer CA, Mangu PB, Wade JC,
Camp-Sorrell D, Cope DG, El-Rayes BF, Gorman M, Ligibel J,
Mansfield P and Levine M: Central venous catheter care for the
patient with cancer: American Society of Clinical Oncology clinical
practice guideline. J Clin Oncol. 31:1357–1370. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Cotogni P and Pittiruti M: Focus on
peripherally inserted central catheters in critically ill patients.
World J Crit Care Med. 3:80–94. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Chopra V, Flanders SA, Saint S, Woller SC,
O'Grady NP, Safdar N, Trerotola SO, Saran R, Moureau N, Wiseman S,
et al Michigan Appropriateness Guide for Intravenouse Catheters
(MAGIC) Panel, : The Michigan Appropriateness Guide for Intravenous
Catheters (MAGIC): Results from a multispecialty panel using the
RAND/UCLA appropriateness method. Ann Intern Med. 163 (Suppl
6):S1–S40. 2015. View
Article : Google Scholar : PubMed/NCBI
|
|
19
|
Walz JM, Memtsoudis SG and Heard SO:
Prevention of central venous catheter bloodstream infections. J
Intensive Care Med. 25:131–138. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Pinelli F, Cecero E, Degl'Innocenti D,
Selmi V, Giua R, Villa G, Chelazzi C, Romagnoli S and Pittiruti M:
Infection of totally implantable venous access devices: A review of
the literature. J Vasc Access. 19:230–242. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Shang M, Chang C, Pei Y, Guan Y, Chang J
and Li H: Potential management of circulating tumor DNA as a
biomarker in triple-negative breast cancer. J Cancer. 9:4627–4634.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Hatakeyama N, Hori T, Yamamoto M, Mizue N,
Inazawa N, Igarashi K, Tsutsumi H and Suzuki N: An evaluation of
peripherally inserted central venous catheters for children with
cancer requiring long-term venous access. Int J Hematol.
94:372–377. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Macmillan T, Pennington M, Summers JA,
Goddard K, Zala D, Herz N, Peacock JL, Keevil S and Chalkidou A:
SecurAcath for securing peripherally inserted central catheters: A
NICE medical technology guidance. Appl Health Econ Health Policy.
16:779–791. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ignatov A, Hoffman O, Smith B, Fahlke J,
Peters B, Bischoff J and Costa SD: An 11-year retrospective study
of totally implanted central venous access ports: Complications and
patient satisfaction. Eur J Surg Oncol. 35:241–246. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Subramaniam A, Kim KH, Bryant SA, Kimball
KJ, Huh WK, Straughn JM, Estes JM and Alvarez RD: Incidence of
mechanical malfunction in low-profile subcutaneous implantable
venous access devices in patients receiving chemotherapy for
gynecologic malignancies. Gynecol Oncol. 123:54–57. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Ahn SJ, Kim HC, Chung JW, An SB, Yin YH,
Jae HJ and Park JH: Ultrasound and fluoroscopy-guided placement of
central venous ports via internal jugular vein: Retrospective
analysis of 1254 port implantations at a single center. Korean J
Radiol. 13:314–323. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Covey AM, Toro-Pape FW, Thornton RH, Son
C, Erinjeri J, Sofocleous CT, Brody LA, Brown KT, Sepkowitz KA and
Getrajdman GI: Totally implantable venous access device placement
by interventional radiologists: Are prophylactic antibiotics
necessary? J Vasc Interv Radiol. 23:358–362. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Taxbro K, Hammarskjöld F, Thelin B, Lewin
F, Hagman H, Hanberger H and Berg S: Clinical impact of
peripherally inserted central catheters vs implanted port catheters
in patients with cancer: An open-label, randomised, two-centre
trial. Br J Anaesth. 122:734–741. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Biacchi D, Sammartino P, Sibio S, Accarpio
F, Cardi M, Sapienza P, De Cesare A, Atta JM, Impagnatiello A and
Di Giorgio A: Does the implantation technique for totally
implantable venous access ports (TIVAPs) influence long-term
outcome? World J Surg. 40:284–290. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Patel GS, Jain K, Kumar R, Strickland AH,
Pellegrini L, Slavotinek J, Eaton M, McLeay W, Price T, Ly M, et
al: Comparison of peripherally inserted central venous catheters
(PICC) versus subcutaneously implanted port-chamber catheters by
complication and cost for patients receiving chemotherapy for
non-haematological malignancies. Support Care Cancer. 22:121–128.
2014. View Article : Google Scholar : PubMed/NCBIPubMed/NCBIPubMed/NCBI
|