Introduction
Lung cancer is the main cause of death due to cancer
in men and women in the world (1,2). In
50–60% of the cases, the disease is diagnosed at the dissemination
stage, and a 5-year survival rate is observed in only 6% of the
patients (1). Characteristic for
this group of patients is the presence of other tabacco-related
diseases which are often the cause of numerous problems just like
the cancer is. Frequently, it results in a more aggressive
treatment at the end of life (3).
Several articles have shown that the early palliative care (EPC)
along with chemotherapy has beneficial effects not only on the
quality of life of the patients, reducing the symptoms of
depression, but also it reduces the number of intensive (not always
necessary) medical procedures at the end of life. However, what is
most important, EPC prolongs life (3–6).
Palliative care consisting in the management of the cancer-related
symptoms and psychological support is a key element in the
treatment of patients with metastatic non-small cell lung cancer
(NSCLC). Therefore, the palliative care physician becomes an
important member of the multidisciplinary team deciding on the
therapy management. The guidelines of international scientific
societies emphasize the importance of the implementation of
palliative care immediately after metastatic lung cancer was
diagnosed (7,8).
The systemic treatment of metastatic lung cancer has
changed significantly in the last five years. Presently, apart from
chemotherapy and tyrosine kinase inhibitors, monoclonal antibodies
directed against programmed cell death protein 1 (PD-1), nivolumab,
pembrolizumab or its ligand (programmed cell death protein ligand
1, PDL-1) atezolizumab, which are immune-checkpoint inhibitors, are
used (7,8). The immunotherapy has significantly
improved prognosis of patients with metastatic lung cancer without
epidermal growth factor receptor activating mutations and
anaplastic lymphoma kinase translocation (9–26). The
administration of these drugs in a group of patients in good
general condition (performance status according to the Eastern
Cooperative Oncology Group, ECOG 0–1) in the first- or second-line
palliative systemic care is constantly increasing. It is also the
group of patients that should be provided with EPC.
Studies on maintaining early palliative and
palliative systemic care in parallel were undertaken in the last 10
years when the immunotherapy was not a standard practice. Despite
changes in the guidelines, the recommendations concerning the
implementation of EPC were maintained. However, is there any proof
of evidence based medicine which confirms the justice concurrent
use of the immunotherapy and EPC?
Chemotherapy and early palliative care
The turning point for the integration of EPC with
cancer treatment in patients with metastatic lung cancer has become
the study by Temel et al (3).
The study randomized patients to either standard oncological care
(exclusive cancer treatment) or the standard oncological care
combined with early hospice care implemented eight weeks after the
diagnosis of cancer at the latest. Palliative care included
education of the patient and the family about the disease and
prognosis and treatment of symptoms with a particular emphasis on
pain, pulmonary symptoms (mainly cough and shortness of breath),
fatigue, sleep disorders, mood changes (depression and anxiety),
lack of appetite or nausea and vomiting, as well as patients
participation in decisions concerning oncological treatment
(27). The study showed that in week
12 of observation the patients randomized to EPC had a better
quality of life than patients randomized to exclusive cancer
treatment. The functional assessment of cancer therapy-lung which
has the results from 0 to 136 showed a mean value of 98.0 compared
to 91.5 in favor of EPC, and the difference was significant
(P=0.03). The improvement in the quality of life observed in the
study was similar to that observed in clinical trials which
assessed the benefit of cisplatin-based chemotherapy. In patients
undergoing EPC, the symptoms of depression were observed less
frequently (16 vs. 38%, P=0.01). What is more, aggressive medical
procedures at end of life were also less frequently used in this
group (33 vs. 54%, P=0.05). Despite this, the median overall
survival (OS) rate was significantly higher (11.6 vs. 8.9 months,
P=0.02) (3). After the publication
of that study, the American Society of Clinical Oncology (ASCO)
established EPC as a standard in metastatic lung cancer (28).
Similar observations were obtained by other studies
where the authors pointed to the benefit of implementing integrated
oncological and palliative care (4–6)
(Table I). Also, Temel et al
(6) continued the study on EPC,
extending their observations in other groups of patients. One study
at week 24 of observation demonstrated an improvement in the
quality of life and reduced percentage of depression among patients
and, additionally, noted patients improved ability to cope with
information about the prognosis. Another study also analyzed the
ability of patients to speak with the clinicians about their
end-of-life care (EOL-care) preferences (6). However, after week 12 a similar
proportion of patients in both groups reported that the main goal
of treatment was healing (28.7 vs. 34.5%, P=0.289), but patients in
the early hospice intervention significantly more often declared
that information on their prognosis was ‘very helpful’ or
‘extremely helpful’ in therapy decision-making (96.5 vs. 89.8%,
P=0.043) and in coping with the disease (97.3 vs. 83.6%,
P<0.001). After week 24, significantly more patients discussed
their EOL-care requests with oncologists (30.2 vs. 14.5%, P=0.004).
The results of the studies by Temel indicate that, apart from the
management of cancer-related symptoms, other elements of EPC are
equally important (6).
 | Table I.Benefits of implementing integrated
oncological and palliative care: Summary of the most important
studies. |
Table I.
Benefits of implementing integrated
oncological and palliative care: Summary of the most important
studies.
| First author,
year | Type of study | Aim of study | Patients with lung
cancer, n | Primary outcome
measures | OS for the EPC
group | Type of
questionnaire to assess QoL | EPC group | QoL for the
(Refs.) |
|---|
| Temel, 2010 | Prospective,
non-blinded, randomized, controlled trial | To compare two
groups: Standard oncological treatment with palliative care given
towards the end-of-life and standard oncological care integrated
with EPC which is given soon after diagnosis | 151 | To assess the
impact of early integration with palliative care on QoL in patients
with advanced NSCL | Improved (P=0.02;
HR 0.30) | FACT-L LCS,
TOI | Improved
(statistically significant) | (3) |
| Zimmermann,
2016 | Prospective,
cluster-randomized controlled trial | To determine
whether, compared with conventional cancer care, early involvement
by a specialized symptom control and palliative care team in
patients with advanced cancer will be associated with better
quality of life, greater patient and caregiver satisfaction with
care, better symptom control, improved communication with
healthcare providers and improved caregiver quality of life | 101 | To assess Patient
Heath Related Quality of Life | Improved
(considering only patients with lung cancer) | FACIT-Sp,
QUAL-E | Improved
(statistically not significant) | (4) |
| King, 2016 | Retrospective | To compare outcomes
from the EPC clinic with eligible patients treated by any other
oncologist without the involvement of palliative care as the SC
arm | 207 |
| Improved (P=0.032;
HR 0.72) | Not used | Not measured | (5) |
| Temel, 2017 | Prospective,
non-blinded, randomized trial | EPC integrated with
oncology care compared with usual oncology care | 191 | To assess changes
in QoL | Not measured | FACT-G, PHQ-9,
HADS | Improved
(statistically improved) | (6) |
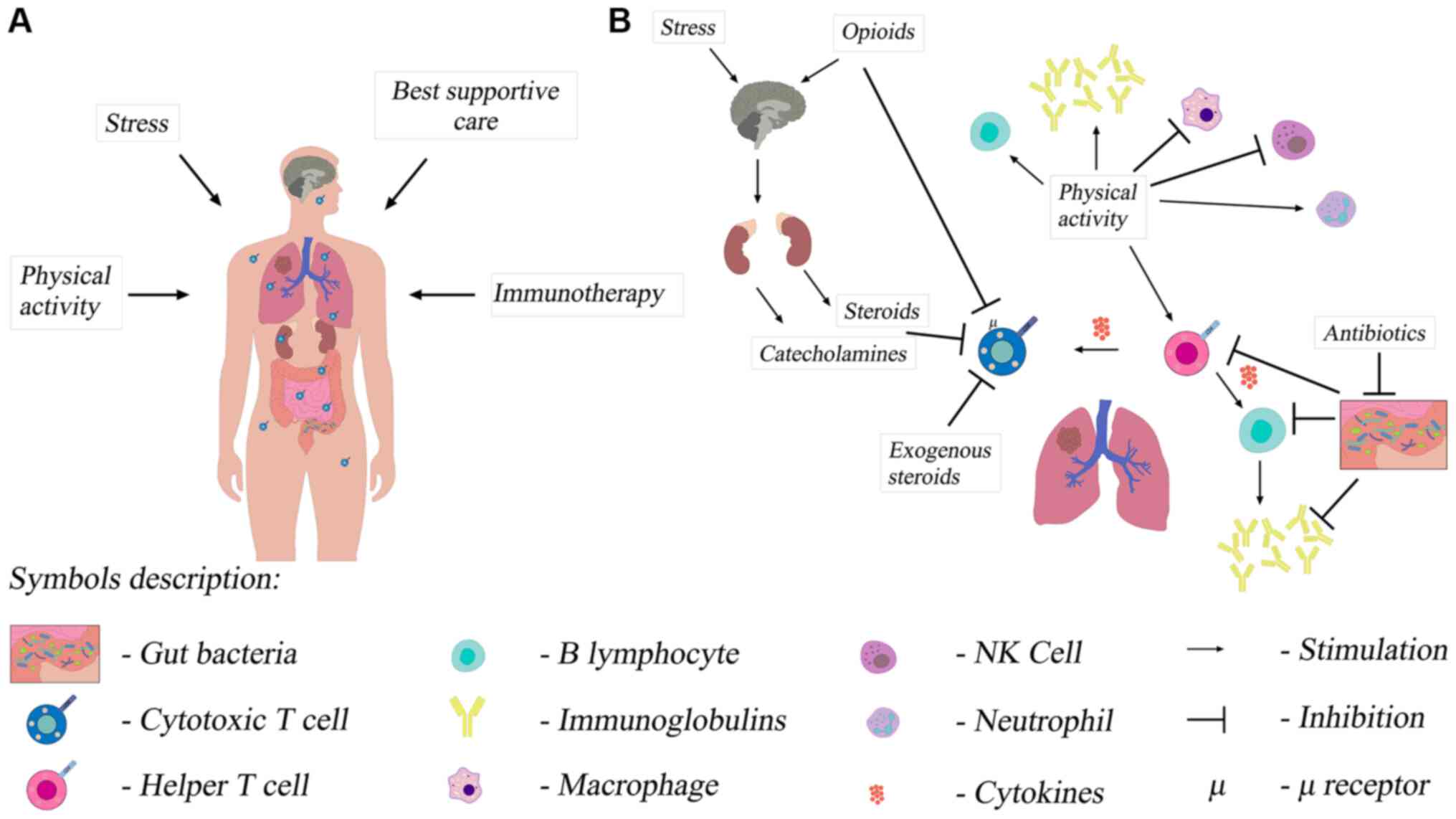
Mechanism of action of early palliative
care
EPC is multidirectional and uses different
mechanisms (29). The first
mechanism is the biological mechanism, i.e. potentially beneficial
anticancer action of the immune system (Fig. 1A and B). The improvement of the
quality of life reduces chronic stress, which may improve the
function of the immune system (Fig. 1A
and B). High levels of chronic stress have been shown to be
associated with higher baseline serum cortisol levels in the
morning and reduced adaptive immune resistance. This results from
the change in the T helper lymphocyte profile. T lymphocytes with
the changed profile reduce the antitumor immunity. Patients with
the improved quality of life showed the reduction of the cortisol
level, which suggests a possible improvement in the function of the
immune system (29).
Another important mechanism of action is the
reduction of the symptoms of depression by early implementation of
multidirectional palliative care. Patients with mild symptoms of
depression are more likely to be physically active, which has a
positive effect on general well-being (Fig. 1B). They also notice, more frequently
and faster, the development of disturbing symptoms, both related to
the disease and to cancer treatment, which may also be the
variables that affect the survival rate. This additional
information helps the clinician understand better the patient and
undertake appropriate treatment (29).
Comprehensive EPC mechanisms may extend the survival
rate through treatment of comorbidities (29). Understanding the prognosis by
patients is also important. The Surveillance, Epidemiology, and End
Results data indicates that chemotherapy undertaken in the last two
weeks of life in patients over 65 years of age does not extend the
survival rate, and the toxic effect of cytostatic agents may
shorten the survival rate (30). If
chemotherapy is stopped at the appropriate time, it may
paradoxically prolong the patients life.
A palliative care practitioner can also implement an
early and adequate treatment of adverse events (AE) of
chemotherapy, which allows conducting chemotherapy in full doses
and in the regular rhythm, and, thus, it can have a favorable
effect on the patients survival rate (29).
It seems that all these elements have an additive
effect, and their total effect is to extend the survival rate.
Immunotherapy in non-small cell lung
cancer
The immunotherapy with the use of the
immune-checkpoint inhibitors mentioned earlier, anti-PD1 and
anti-PDL1 monoclonal antibodies, has become a breakthrough in the
treatment of patients with advanced NSCLC, significantly changing
the prognosis of such patients. It can now be used both in the
first- and second-line therapy, after the failure of chemotherapy.
Everyday clinical practice uses antibodies: pembrolizumab,
nivolumab (anti-PD1 antibodies), atezolizumab (anti-PDL1 antibody)
and ipilimumab [anti-T-lymphocyte-associated antigen 4 (CTLA4)
antibody] (9–26).
In the first line of palliative systemic treatment
of metastatic non-small cell lung cancer the immunotherapy can be
used alone or combined with other drugs. Treatment options include
pembrolizumab monotherapy if PDL-1 expression is strong (≥50%)
(9,10), and regardless of PDL-1 expression,
combination of nivolumab with ipilimumab in patients with high
tumor mutation burden (TMB) (14,15),
combination of chemotherapy with pembrolizumab (12) or combination of chemotherapy with
atezolizumab and bevacizmumab [anti-vascular endothelial growth
factor (VEGF) antibody] (17). All
these schemes have been shown to affect OS and progression-free
survival (PFS) (details in Table
II). The overall response rate (ORR) evaluated by RECIST
criteria were also higher in the group of patients receiving
immunotherapy. The toxicity of the treatment clearly favors
regimens with immunotherapy, in particular when monotherapy with
pembrolizumab is used. The only exception is the combination of
nivolumab and ipilimumab, where the toxicity of the treatment was
slightly higher than in the case of nivolumab monotherapy (details
in Table II). All the above
regimens (except combination of chemotherapy with anti-PDL1 and
anti-VEGF antibodies) also had a positive impact on the quality of
life of patients, which is extremely important as it is one of the
most important goals of palliative treatment (11,13,16,18).
 | Table II.Summary of the crucial clinical
trials which are the basis of the guidelines. |
Table II.
Summary of the crucial clinical
trials which are the basis of the guidelines.
| Name of the
trial | Expression of
PD-L1 | Histology | Stage | Aim of the
study | Median OS (IT vs.
ChT) | Median PFS (IT vs.
ChT) | ORR (IT vs.
ChT) | AE (G3-G4) (IT vs.
ChT) | QoL for IT | (Refs.) |
|---|
| First-line
therapy |
|
|
|
|
|
|
|
|
|
|
| KEYNOTE
024 | ≥50% | SCC and NSCC | IV | To compare
pembrolizumab (at a fixed dose of 200 mg every 3 weeks) vs. the
investigator's choice of platinum-based chemotherapy | 30 (95% CI, 18.3
months to NR) vs. 14.2 (95% CI, 9.8–19.0) months (HR = 0.63; 95% CI
0.47–0.86 months) | 10.3 (95% CI, 6.7
to not reached) vs. 6.0 months (95% CI, 4.2 to 6.2) | 45.5 vs. 29.8
% | G3-G5 31.2 vs.
53.3% | Improved
(statistically significant) | (9–11) |
| KEYNOTE
189 | Benefit regardless
of it | SCC and NSCC | IV | To compare
pemetrexed and a platinum-based drug plus either 200 mg of
pembrolizumab or placebo every 3 weeks for 4 cycles, followed by
pembrolizumab or placebo for up to a total of 35 cycles plus
pemetrexed maintenance therapy | 22.0 (19.5–25.2)
vs. 10.7 (8.7–13.6) months (HR=0.56; 95% CI, 0.45–0.70) | 9.0 (8.1–9.9) vs.
4.9 (8.1–9.9) months (HR, 0.49; 95% CI, 0.40–0.59) | 48.0 vs. 19.4% | G3-G5 71.9 vs.
66.8% | Improved
(statistically significant) | (12,13) |
|
CheckMate 227 IT - ipi
+nivo | Benefit regardless
of it | SCC and NSCC | IV | To compare
nivolumab plus ipilimumab, nivolumab plus chemotherapy, or
chemotherapy alone | 17.1 (15.0–20.1)
vs. 14.9 (12.7–16.7) months (HR=0.79; 97.72% CI, 0.65–0.96,
P=0.007) | 7.2 (patients with
high TMB) (95% CI, 5.5–13.2) vs. 5.5 months (95% CI, 4.4–5.8) (HR
0.58; 97.5% CI, 0.41–0.81; P<0.001) | 35.9 vs. 30.0% | 32.8 vs. 36.0% | Improved
(statistically significant) | (14–16) |
|
ImPower150 | Benefit regardless
of it | NSCC | IV | To compare 3
treatments: atezolizumab+carboplatin+ paclitaxel (ACP),
atezolizumab +carboplatin+paclitaxel +bevacizumab (ABCP) or
carboplatin+paclitaxel +bevacizumab (BCP) | 19.2 for ABCP vs.
14.7 for BCP months (HR=0.78; 95% CI, 0.64–0.96; P=0.02) | 8.3 for ABCP vs.
6.8 for BCP months (HR 0.62; 95% CI, 0.52–0.74; P<0.001) | 63.5 in the ABCP
group vs. 48.0 % in the BCP group | Treatment
tolerability differed between induction and maintenance phases
across treatment arms, more patients had grade 3/4
treatment-related AEs during the induction versus maintenance phase
(ACP, 40.5 vs. 8.2%; ABCP, 48.6 vs. 21.2%; BCP, 44.7 vs. 11.1% | Similar across
study's arms | (17,18) |
| Second-line
therapy |
|
|
|
|
|
|
|
|
|
|
|
CheckMate 017 | Benefit regardless
of it | SCC | IIIB/IV | To compare
nivolumab, at a dose of 3 mg per kilogram of body weight every 2
weeks, and docetaxel, at a dose of 75 mg per square meter of
body-surface area every 3 weeks | 9.2 (95% CI,
7.3–13.3) vs. 6.0 (95% CI, 5.1–7.3) months (HR=0.59; 95% CI,
0.44–0.79; P<0.001) | 3.5 vs. 2.8 months
(HR 0.62; 95% CI, 0.47–0.81; P<0.001) | 20 vs. 9% | 7 vs. 55% | Improved
(statistically significant) | (19,20) |
|
CheckMate 057 | Benefit regardless
of it | NSCC | IIIB/IV | To compare
nivolumab at a dose of 3 mg per kilogram of body weight every 2
weeks to docetaxel at a dose of 75 mg per square meter of
body-surface area every 3 weeks | 12.2 (95% CI, 9.7
to 15.0) vs. 9.4 (95% CI, 8.1–10.7) months (HR=0.73; 96% CI,
0.59–0.89; P=0.002) | No difference | 19 vs. 12% | 10 vs. 54% | Improved
(statistically significant) | (21,22) |
| KEYNOTE
010 | >1% | SCC, NSCC | IV | To compare two
doses of pembrolizumab (2 and 10 mg/kg) vs. docetaxel 75 mg per
square meter of body-surface area every 3 weeks | 10.4 (pembro 2
mg/kg), 12.7 (pembro 10 mg/kg) vs. 8·5 months pembro 2 mg/kg vs
docetaxel (HR=0.71, 95% CI 0.58–0.88; p=0·0008) pembro 10 mg/kg vs.
docetaxel (HR 0.61, 0.49–0·75; P<0·0001) | No significant
difference between groups | 30% (pembro
2mg/kg), 29% pembro 10 mg/kg) vs. 8% | 13% (pembro
2mg/kg), 16% pembro 10 mg/kg vs. 35% | Improved
(statistically significant) | (23,24) |
|
OAK | Benefit regardless
of it | SCC, NSCC | IIIB/IV | To compare
atezolizumab (fixed dose 1,200 mg every 3 weeks) with docetaxel 75
mg per square meter of body-surface every 3 area weeks | 15.7 (95% CI
12.6–18.0) vs. 10.3 (8.8–12.0) months (HR 0.74, 95% CI 0.58–0.93;
P=0.0102) | Similar in both
groups | Similar in both
groups | 37 vs. 54% | Improved
(statistically significant) | (23,24) |
In the second line of treatment, the superiority of
antibodies [nivolumab (19,21), pembrolizumab (23), atezolizumab (25)] over docetaxel chemotherapy was
demonstrated in terms of parameters such as OS, hazard ratio (HR),
ORR and treatment toxicity. All patients benefited from the
treatment, regardless of PD-L1 expression and histology (Table II). Second-line immunotherapy did
not only affect PFS, but is typical of it. The significant
improvement in the quality of life of patients treated with
immunotherapy is also noteworthy (22,24,26).
Based on these study results (Table II), it can be concluded that the
immunotherapy is a therapy that allows patients with metastatic
lung cancer to have longer OS compared with standard chemotherapy
and, in addition, the immunotherapy is a therapy with considerably
lower toxicity. However, the immunotherapy offers benefits to
patients whose immune system is functional, and a simple clinical
exponent of this functionality is the general condition of the
patient. Therefore, the immunotherapy should be used as early as
possible, in the first- or second-line palliative systemic
treatment, when patients are in very good general condition.
So far, no randomized clinical trial has emerged for
immunotherapy and BSC with intent as in the study by Temel et
al (3,6) for chemotherapy and BSC. We do not know
exactly what is the impact (e.g., on OS or QoL) of early hospice
care implementation to immunotherapy compared to the group of
patients treated only with immunotherapy. Based on the observation
of patients treated with chemotherapy and concurrent EPC, it may be
suspected that such patients have a chance of an early initiation
of treatment AE induced by immunotherapy, which may translate into
survival. However, there is no literature data on this subject.
Immunotherapy vs. palliative care
Immunotherapy and opioids
The most common symptoms in patients with advanced
lung cancer are pain, cough and dyspnea. Management of them is the
object of daily practice in EPC, and their treatment consists
primarily in the use of opioids, various steroids and antibiotics
(31). A range of data from
immunotherapy studies indicates that these drugs considerably lower
the efficacy of this method of treatment.
Opioids are drugs with proven immunosuppressive
effects (32). Their influence on
the immune system is multidirectional (Fig. 1B). From the perspective of the
application of the immunotherapy in the treatment of cancers, the
most important seems to be the effect on T cells, which are the
main effectors of action of anti-PD1 and anti-PDL1 antibodies and
their influence on the hypothalamic-pituitary-adrenal axis. Opioids
interact with μ receptors located on T cells, and the effect of
this interaction is impairment of T cell viability and their
proliferation caused by activation factors (32). Immunosuppression induced by opioids
is a result of their effect on the hypothalamic-pituitary-adrenal
axis. Corticotropin-releasing hormone stimulates the anterior
pituitary to produce adrenocorticotropic hormone (ACTH), which in
turn stimulates the adrenal cortex to produce glucocorticoids.
These influence various elements of the innate and adaptive immune
system, suppress cellular immunity and contribute to the tolerance
of different antigens by altering the function of T and B cells
(32). The effect of opioids on this
axis depends on the time of drug administration during the day and
on the duration of their use. Opioids change the concentration of
ACTH as well as of glucocorticoids. Such biological mechanisms of
action translate into worse immunotherapy outcomes in patients on
concomitant opioids. It was demonstrated that patients treated with
opioids from the beginning of the immunotherapy and patients who,
during the immunotherapy, required the increasing of doses, had a
significantly lower survival rate (median OS 4.9 vs. 16.5 months,
P=0.0030) (33,34). It should be noted that the strongest
immunosuppressive properties have morphine and fentanyl, weaker
oxycodone and tramadol and the weakest buprenorphine (33). With respect to the last medication,
no immunosuppressive effect was reported (33).
Immunotherapy and glucocorticoids
Another group of drugs, often recommended by EPC
practitioners and causing suppression of the immune system, are
glucocorticoids. The mechanism of their immunosuppressive effects
is described above. The registration studies for pembrolizumab in
the first-line therapy as well as for nivolumab and atezolizumab in
the second-line therapy excluded patients receiving
corticosteroids. The exclusion criterion was the administration of
prednisone at the dose of 10 mg or more per day or a different
glucocorticoid at an equivalent dose. Over time, the immunotherapy
went from clinical trials to daily practice and became a standard
therapy. Hence the immunotherapy in patients receiving
corticosteroids has began to be used. Indications for use of
glucocorticoids in patients with lung cancer include alleviation of
cancer-related symptoms as well as treatment of comorbidities,
e.g., chronic obstructive pulmonary disease (COPD). They are also
used in the treatment of adverse effects of the immunotherapy. The
study by Arbour et al (35)
assessed the results of the actual population of patients
undergoing the immunotherapy and receiving steroids and undergoing
the immunotherapy and not receiving steroids. In the group of 640
patients, 90 patients (14%) received prednisone at a dose of ≥10
mg/day (or a different steroid at an equivalent dose) at the
beginning of the immunotherapy. The most common indications for
steroid use were dyspnea (33%), fatigue (21%) and cerebral
metastases (19%). In patients receiving steroids, more frequently
there were more than two factors of an unfavorable prognosis, the
performance status ≥2 (according to the ECOG) and the presence of
cerebral metastases (P<0.01 for both factors). In the pooled
analysis, patients receiving steroids had a lower ORR (7 vs. 18%),
significantly lower PFS (P<0.001) and OS (P<0.001) compared
to patients not receiving corticosteroids (35). The very important issue is the time
of corticosteroids treatment initiation. Patients who received and
discontinued corticosteroids days 1 to 30 before to the initiation
of PD-L1 had intermediate PFS and OS compared with those who
received corticosteroids from the beginning of ICI treatment and
those who received no corticosteroids within 30 days of the start
of therapy. The authors of the publication performed a
multifactorial analysis which included the history of tobacco
smoking, performance, history of cerebral metastases and the use of
corticosteroids at the beginning of the immunotherapy. The result
of the analysis showed that the use of corticosteroids was an
independent prognostic factor associated with lower PFS and OS
rates (35). The disadvantage of the
analysis is that it did not take into account the expression of
PDL1 or TMB. In addition, the study included a group of patients
who discontinued corticosteroids 1–30 days prior to the
immunotherapy. They obtained indirect PFS and OS values compared to
patients receiving and not receiving steroids at the beginning of
the therapy (35). An important
aspect of the use of corticosteroids in patients with lung cancer
undergoing the immunotherapy is the treatment of
immunotherapy-related AE. Although biological mechanisms described
above indicate a reduction in the function of the immune system due
to steroid therapy, many studies have demonstrated that patients
undergoing the immunotherapy and steroid therapy achieve higher
survival rates, as opposed to chemotherapy (1,2,6,25). These
observations raise a number of questions. Do glucocorticoids
actually decrease the efficacy of the immunotherapy? Are they used
for a more aggressive disease, in patients with a worse prognosis,
who do not benefit from the immunotherapy, which could indicate
their prognostic significance? One study performed a retrospective
analysis of 424 patients with NSCLC treated with immune-checkpoint
inhibitors, with regard to the use of steroids (36). The highest survival rate was achieved
by patients who did not take steroids and were indirectly treated
with steroids from the beginning of the immunotherapy and the
shortest survival rate by patients who started corticosteroids in
the first eight weeks of the immunotherapy (median OS 13.83 vs. 4.2
vs. 2.2 months respectively, P=0.0001). The analysis of indications
for steroid use showed that patients who received them for
non-neoplastic reasons reached the survival rate comparable to
those who did not receive steroids (median OS of 13.4 vs. 13.8
months, respectively; P<0.0001). In the group of patients
receiving corticosteroids due to cancer-related problems, median OS
was 1.9 months (P<0.0001) (36).
The results of the study support the hypothesis that the use of
steroids can have the prognostic significance and indicate a group
with an unfavorable prognosis. The prudent use of steroids in
immunotherapy patients is recommended in the absence of conclusive
data. The most commonly used steroid is dexamethasone at a dose of
4 to 16 mg, mostly due to pain (including headache), nausea,
weakness and lack of appetite (37–39). The
literature data indicates that glucocorticoids are used in
palliative care in over half of the patients (39–41). The
literature does not include any clear-cut information about whether
EPC contributes to the earlier and more frequent use of steroids in
metastatic lung cancer patients. However, it seems that due to the
nature of the most common symptoms in this population, this may
potentially affect the efficacy of the immunotherapy.
Immunotherapy and antibiotics
The third group of drugs that may affect the
efficacy of the immunotherapy is antibiotics. Based on numerous
studies regarding the correlation between intestinal microflora and
the immune system, it has been found that intestinal homeostasis
prevents systemic inflammation and reduces the ability of
neoplastic cells to escape immune surveillance (40,41). It
has been hypothesized that modulation of intestinal microflora by
antibiotics affects the immune system and may be associated with
the efficacy of action of anti-PD-1 and anti-PDL1 antibodies. Host
intestinal microbiota and immune system create numerous
interactions which modulate the local and systemic immune system
(42). Antibiotics cause dysbiosis,
i.e. reduce the diversity of intestinal microflora, which promotes
chronic inflammatory conditions (43,44). The
study by Derosa et al (44)
assessed the effect of using antibiotics on the efficacy of the
immunotherapy. The administration of antibiotics from 30 to 60 days
prior to the immunotherapy was taken into account. It was noted
that 20% of patients with NSCLC received antibiotics 30 days prior
to the immunotherapy. Compared to the patients not taking
antibiotics, that group had a significantly shorter time from
progression [median PFS 1.9 vs. 3.8 months; HR 1.5, 95% confidence
interval (CI) 1.0–2.2, P=0.03] and shorter OS (median OS 7.9 vs.
24.6 months; HR 4.4; 95% CI 2.6–7.7, P<0,01). In the group of
patients who received antibiotics 60 days prior to the
immunotherapy, no differences in the ORR and PFS were observed, but
shorter OS was noted (median OS 9.8 vs. 21.9 months; HR 2.0, 95% CI
1.3–3.2, P<0.01). A multifactorial analysis showed that the
antibiotic therapy was an independent factor associated with a
lower survival rate (HR 2.5, 95% CI 1.6–3.7; P<0.01) (44). The use of the antibiotic therapy
seems to be an indication of unfavorable prognosis in patients
undergoing the immunotherapy regardless of conventional prognostic
markers. Do antibiotics make the treatment less effective? Do they
indicate a group of patients with a worse prognosis, with a greater
mass of the neoplastic disease, more problems and comorbidities
which are more difficult to manage? There are no clear answers to
these questions. The EPC recommendations list antibiotics for
various problems, including cough or fever (31,45).
However, it is likely that such patients more often require the
antibiotic therapy due to their predisposition to pneumonia and
exacerbation of comorbidities such as COPD (31,45,46). The
doubt may arise whether EPC, through the frequent use of
antibiotics, decreases the efficacy of the immunotherapy.
Literature data indicates that up to 86% of patients who undergo
palliative care receive antibiotics, which are even abused in the
last few weeks of their lives (45–47).
However, there is no data on whether the EPC of lung cancer
patients affects their too early use and, consequently, perhaps the
efficacy of the immunotherapy.
Conclusions
EPC has a well-established role in the treatment of
patients with metastatic NSCLC. However, the studies that have
become the cornerstone of the worldwide guidelines in this respect
did not include patients treated with anti-PD1 and anti-PDL1
antibodies. Drugs that are often used in hospice care probably
worsen the efficacy of the immunotherapy or indicate the worst
prognostic group of patients who would not benefit from the
immunotherapy. Insufficient scientific evidence in this area of
knowledge requires special consideration in everyday clinical
practice and implementation of EPC in lung cancer patients
undergoing the immunotherapy.
Controlled clinical studies involving patients
undergoing the immunotherapy and EPC could help remove these
doubts.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
Not applicable.
Authors contributions
MP was responsible for the concept of the
manuscript, collecting and interpreting data on immunotherapy of
NSCLC, design and production of the figure. PP was responsible for
collecting and interpreting data on palliative care. BR was
supervisor of the manuscript and revised it critically for
important intellectual content. All authors read and approved the
final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
ACTH
|
adrenocorticotropic hormone
|
|
AE
|
adverse events
|
|
ChT
|
chemotherapy
|
|
CI
|
confidence interval
|
|
COPD
|
chronic obstructive pulmonary
disease
|
|
ECOG
|
Eastern Cooperative Oncology Group
|
|
EPC
|
early palliative care
|
|
EOL-care
|
end-of-life care
|
|
FACIT-Sp
|
the functional assessment of chronic
illness therapy-spiritual well-being
|
|
FACT-G
|
the functional assessment of cancer
therapy-general
|
|
FACT-L
|
the functional assessment of cancer
therapy-lung
|
|
HADS
|
Hospital Anxiety and Depression
scale
|
|
G
|
grade
|
|
HR
|
hazard ratio
|
|
IT
|
immunotherapy
|
|
LCS
|
lung-cancer subscale
|
|
NSCLC
|
non-small cell lung cancer
|
|
NSCC
|
non-squamous cell cancer
|
|
ORR
|
overall response rate
|
|
OS
|
overall survival
|
|
PFS
|
progression-free survival
|
|
PHQ-9
|
patient health questionnaire-9
|
|
PD-1
|
programmed cell death protein 1
|
|
PDL-1
|
programmed cell death protein ligand
1
|
|
QoL
|
quality of life
|
|
QUAL-E
|
quality of life at the end of life
|
|
SCC
|
squamous cell cancer
|
|
TOI
|
trial outcome index
|
|
TMB
|
tumor mutation burden
|
|
VEGF
|
vascular endothelial growth factor
|
References
|
1
|
Islami F, Torre LA and Jemal A: Global
trends of lung cancer mortality and smoking prevalence. Transl Lung
Cancer Res. 4:327–338. 2015.PubMed/NCBI
|
|
2
|
Torre LA, Bray F, Siegel RL, Ferlay J,
Lortet-Tieulent J and Jemal A: Global cancer statistics, 2012. CA
Cancer J Clin. 65:87–108. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Temel JS, Greer JA, Muzikansky A,
Gallagher ER, Admane S, Jackson VA, Dahlin CM, Blinderman CD,
Jacobsen J, Pirl WF, et al: Early palliative care for patients with
metastatic non-small cell lung cancer. N Engl J Med. 363:733–742.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Zimmermann C, Swami N, Krzyżanowska M,
Hannon B, Leighl N, Oza A, Moore M, Rydall A, Rodin G, Tannock I,
et al: Early palliative care for patients with advanced cancer: A
cluster-randomised controlled trial. Lancet. 383:1721–1730. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
King JD, Eickhoff J, Traynor A and
Campbell TC: Integrated onco-palliative care associated with
prolonged survival compared to standard care for patients with
advanced lung cancer: A retrospective review. J Pain Symptom
Manage. 51:1027–1032. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Temel JS, Greer JA, El-Jawahri A, Pirl WF,
Park ER, Jackson VA, Back AL, Kamdar M, Jacobsen J, Chittenden EH,
et al: Effects of early palliative care in patients with lung and
GI cancer: A randomized clinical trial. J Clin Oncol. 35:834–841.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
National Comprehensive Cancer Network
(NCCN): NCCN Guidelines-Non-small Cell Lung Cancer, Version 3.2020.
simplehttps://www.nccn.org/globalFebruary 11–2020
|
|
8
|
Planchard D, Popat S, Kerr K, Novello S,
Smit EF, Faivre-Finn C, Mok TS, Reck M, Van Schil PE, Hellmann MD,
et al: Metastatic non-small cell lung cancer: ESMO clinical
practice guidelines for diagnosis, treatment and follow-up. Ann
Oncol. 30:863–870. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Reck M, Rodríguez-Abreu D, Robinson AG,
Hui R, Csőszi T, Fülöp A, Gottfried M, Peled N, Tafreshi A, Cuffe
S, et al KEYNOTE-024 Investigators, : Pembrolizumab versus
chemotherapy for PD-L1-positive non-small cell lung cancer. N Engl
J Med. 375:1823–1833. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Reck M, Rodríguez-Abreu D, Robinson AG,
Hui R, Csőszi T, Fülöp A, Gottfried M, Peled N, Tafreshi A, Cuffe
S, et al: Updated analysis of KEYNOTE-024: Pembrolizumab versus
platinum-based chemotherapy for advanced non-small cell lung cancer
with PD-L1 tumor proportion score of 50% or greater. J Clin Oncol.
37:537–546. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Brahmer JR, Rodríguez-Abreu D, Robinson
AG, Hui R, Csőszi T, Fülöp A, Gottfried M, Peled N, Tafreshi A,
Cuffe S, et al: Health-related quality-of-life results for
pembrolizumab versus chemotherapy in advanced, PD-L1-positive NSCLC
(KEYNOTE-024): A multicentre, international, randomised, open-label
phase 3 trial. Lancet Oncol. 18:1600–1609. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Gadgeel S, Rodríguez-Abreu D, Speranza G,
Esteban E, Felip E, Dómine M, Hui R, Hochmair MJ, Clingan P, Powell
SF, et al: Updated analysis from KEYNOTE-189: Pembrolizumab or
placebo plus pemetrexed and platinum for previously untreated
metastatic nonsquamous non-small cell lung cancer. J Clin Oncol.
38:1505–1517. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Garassino M, Rodriguez-Abreu D, Gadgeel,
Esteban E, Felip E, De Angelis F, Domine M, Hochmair M, Powell SF,
Cheng SY, et al: Health-related quality of life (HRQoL) in the
KEYNOTE-189 study of pembrolizumab (pembro) or placebo (pbo) +
pemetrexed (pem) + platinum (plt) for metastatic NSCLC. J Clin
Oncol. 36:2019.
|
|
14
|
Hellmann MD, Ciuleanu TE, Pluzanski A, Lee
JS, Otterson GA, Audigier-Valette C, Minenza E, Linardou H, Burgers
S, Salman P, et al: Nivolumab plus ipilimumab in lung cancer with a
high tumor mutational burden. N Engl J Med. 378:2093–2104. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Hellmann MD, Paz-Ares L, Bernabe Caro R,
Zurawski B, Kim SW, Carcereny Costa E, Park K, Alexandru A,
Lupinacci L, de la Mora Jimenez E, et al: Nivolumab plus Ipilimumab
in advanced non-small cell lung cancer. N Engl J Med.
381:2020–2031. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Reck M, Schenker M, Lee KH, Provencio M,
Nishio M, Lesniewski-Kmak K, Sangha R, Ahmed S, Raimbourg J, Feeney
K, et al: Nivolumab plus ipilimumab versus chemotherapy as
first-line treatment in advanced non-small cell lung cancer with
high tumour mutational burden: Patient-reported outcomes results
from the randomised, open-label, phase III CheckMate 227 trial. Eur
J Cancer. 116:137–147. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Socinski MA, Jotte RM, Cappuzzo F, Orlandi
F, Stroyakovskiy D, Nogami N, Rodríguez-Abreu D, Moro-Sibilot D,
Thomas CA, Barlesi F, et al IMpower150 study group, : Atezolizumab
for first-line treatment of metastatic nonsquamous NSCLC. N Engl J
Med. 378:2288–2301. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Reck M, Wehler T, Orlandi F, Nogami N,
Barone C, Moro-Sibilot D, Shtivelband M, González Larriba JL,
Rothenstein J, Früh M, et al: Safety and patient-reported outcomes
of atezolizumab plus chemotherapy with or without bevacizumab
versus bevacizumab plus chemotherapy in non-small cell lung Cancer.
J Clin Oncol. 38:2530–2542. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Brahmer J, Reckamp KL, Baas P, Crinò L,
Eberhardt WEE, Poddubskaya E, Antonia S, Pluzanski A, Vokes EE,
Holgado E, et al: Nivolumab versus docetaxel in advanced
squamous-cell non-small cell lung cancer. N Engl J Med.
373:123–135. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Reck M, Taylor F, Penrod JR, DeRosa M,
Morrissey L, Dastani H, Orsini L and Gralla RJ: Impact of nivolumab
versus docetaxel on health-related quality of life and symptoms in
patients with advanced squamous non-small cell lung cancer: Results
from the CheckMate 017 study. J Thorac Oncol. 13:194–204. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Borghaei H, Paz-Ares L, Horn L, Spigel DR,
Steins M, Ready NE, Chow LQ, Vokes EE, Felip E, Holgado E, et al:
Nivolumab versus docetaxel in advanced nonsquamous non-small cell
lung cancer. N Engl J Med. 373:1627–1639. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Reck M, Brahmer J, Bennett B, Taylor F,
Penrod JR, DeRosa M, Dastani H, Spigel DR and Gralla RJ: Evaluation
of health-related quality of life and symptoms in patients with
advanced non-squamous non-small cell lung cancer treated with
nivolumab or docetaxel in CheckMate 057. Eur J Cancer. 102:23–30.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Herbst RS, Baas P, Kim DW, Felip E,
Pérez-Gracia JL, Han JY, Molina J, Kim JH, Arvis CD, Ahn MJ, et al:
Pembrolizumab versus docetaxel for previously treated,
PD-L1-positive, advanced non-small cell lung cancer (KEYNOTE-010):
A randomised controlled trial. Lancet. 387:1540–1550. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Barlesi F, Garon EB, Kim DW, Felip E, Han
JY, Kim JH, Ahn MJ, Fidler MJ, Gubens MA, de Castro G Jr, et al:
Health-related quality of life in KEYNOTE-010: A phase II/III study
of pembrolizumab versus docetaxel in patients with previously
treated advanced, programmed death ligand 1-expressing NSCLC. J
Thorac Oncol. 14:793–801. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Rittmeyer A, Barlesi F, Waterkamp D, Park
K, Ciardiello F, von Pawel J, Gadgeel SM, Hida T, Kowalski DM, Dols
MC, et al OAK study group, : Atezolizumab versus docetaxel in
patients with previously treated non-small cell lung cancer (OAK):
A phase 3, open-label, multicentre randomised controlled trial.
Lancet. 389:255–265. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Bordoni R, Ciardiello F, von Pawel J,
Cortinovis D, Karagiannis T, Ballinger M, Sandler A, Yu W, He P,
Matheny C, et al: Patient-reported outcomes in OAK: A phase III
study of atezolizumab versus docetaxel in advanced non-small cell
lung cancer. Clin Lung Cancer. 19:441–449.e4. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Temel JS, Greer JA, Muzikansky A,
Gallagher ER, Admane S, Jackson VA, Dahlin CM, Blinderman CD,
Jacobsen J, Pirl WF, et al: Early palliative care for patients with
metastatic non-small cell lung cancer. N Engl J Med. 363:733–742.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Smith TJ, Temin S, Alesi ER, Abernethy AP,
Balboni TA, Basch EM, Ferrell BR, Loscalzo M, Meier DE, Paice JA,
et al: American society of clinical oncology provisional clinical
opinion: The integration of palliative care into standard oncology
care. J Clin Oncol. 30:880–887. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Irwin KE, Greer JA, Khatib J, Temel JS and
Pirl WF: Early palliative care and metastatic non-small cell lung
cancer: Potential mechanisms of prolonged survival. Chron Respir
Dis. 10:35–47. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Saito AM, Landrum MB, Neville BA, Ayanian
JZ and Earle CC: The effect on survival of continuing chemotherapy
to near death. BMC Palliat Care. 10:142011. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Watsob MS, Lucas CF, Hoy AM and Back IN:
Oxford Handbook of Palliative Care. 1st edition. Oxford University
Press; Oxford: 2005
|
|
32
|
Zajączkowska R, Leppert W, Mika J,
Kocot-Kępska M, Woroń J, Wrzosek A and Wordliczek J: Perioperative
immunosuppression and risk of cancer progression: The impact of
opioids on pain management. Pain Res Manag. 2018:92937042018.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Rinaldi S, Marcantognini G, Fiordoliva I,
di Pietro Paolo M, Morgese F, Toriniai M, Burattini L and Berardi
R: The negative prognostic role of opioids in patients with NSCLC
treated with immunotherapy. Presented at MASCC/ISOO Annual Meeting
on Supportive Care in Cancer San Francisco, CA: 2019
|
|
34
|
Bironzo P, Pignataro D, Audisio M,
Tagliamento M, Paratore C, Tabbò F, Bungaro M, Zichi C, Filippis M,
Rapetti S, et al: Association between opioids and outcome of 1st
line immunotherapy in advanced NSCLC patients: A retrospective
evaluation. JTO. 14:s7132019.
|
|
35
|
Arbour KC, Mezquita L, Long N, Rizvi H,
Auclin E, Ni A, Martínez-Bernal G, Ferrara R, Lai WV, Hendriks LEL,
et al: Impact of baseline steroids on efficacy of programmed cell
death-1 and programmed death-ligand 1 blockade in patients with
non–small cell lung cancer. J Clin Oncol. 36:2872–2878. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
De Giglio A, Mezquita L, Auclin E,
Blanc-Durand F, El-Amarti L, Caramella C, Martinez Bernal G,
Hendriks L, Ferrara R, Naltet C, et al: Impact of early
introduction of steroid on immune-checkpoint inhibitors (ICI) in
patients with advanced non- small cell lung cancer treated. Ann
Oncol. 30((s11)): xi162019. View Article : Google Scholar
|
|
37
|
Shih A and Jackson KC II: Role of
corticosteroids in palliative care. J Pain Palliat Care
Pharmacother. 21:69–76. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Barghi K, Edmonds KP, Ajayi TA and Atayee
RB: Prescribing trends of palliative care teams use of
dexamethasone for cancer-related pain. J Pain Palliat Care
Pharmacother. 32:37–43. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
North West Clinical Senates: Guidelines
for the use of corticosteroids in palliative care. simplehttp://www.nwcscnsenate.nhs.uk/files/2814/3394/6186/Corticosterioids.pdfMay
18–2020
|
|
40
|
Lozupone CA, Stombaugh JI, Gordon JI,
Jansson JK and Knight R: Diversity, stability and resilience of the
human gut microbiota. Nature. 489:220–230. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Zitvogel L, Ayyoub M, Routy B and Kroemer
G: Microbiome and anticancer immunosurveillance. Cell. 165:276–287.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Ubeda C and Pamer EG: Antibiotics,
microbiota, and immune defense. Trends Immunol. 33:459–466. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Lange K, Buerger M, Stallmach A and Bruns
T: Effects of antibiotics on gut microbiota. Dig Dis. 34:260–268.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Derosa L, Hellmann MD, Spaziano M,
Halpenny D, Fidelle M, Rizvi H, Long N, Plodkowski AJ, Arbour KC,
Chaft JE, et al: Negative association of antibiotics on clinical
activity of immune checkpoint inhibitors in patients with advanced
renal cell and non-small cell lung cancer. Ann Oncol. 29:1437–1444.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Rosenberg JH, Albrecht JS, Fromme EK,
Noble BN, McGregor JC, Comer AC and Furuno JP: Antimicrobial use
for symptom management in patients receiving hospice and palliative
care: A systematic review. J Palliat Med. 16:1568–1574. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Helde-Frankling M, Bergqvist J, Bergman P
and Björkhem-Bergman L: Antibiotic treatment in end-of-life cancer
patients-A retrospective observational study at a palliative care
center in Sweden. Cancers (Basel). 8:842016. View Article : Google Scholar
|
|
47
|
Juthani-Mehta M, Malani PN and Mitchell
SL: Antimicrobials at the end of life: An opportunity to improve
palliative care and infection management. JAMA. 314:2017–2018.
2015. View Article : Google Scholar : PubMed/NCBI
|