Introduction
Nasopharyngeal carcinoma (NPC) is endemic in North
Africa, Southeast Asia and, most notably, South China (1). According to the current World Health
Organization (WHO) classification of pathological subtypes, NPCs
are grouped into i) non-keratinizing squamous cell carcinoma, ii)
keratinizing squamous cell carcinoma and iii) basaloid squamous
cell carcinoma (2). The first
group is further subdivided into non-keratinizing differentiated
carcinoma and non-keratinizing undifferentiated carcinoma, which is
dominant in endemic areas (2,3).
Neuroendocrine carcinoma (NEC) is a poorly differentiated
neuroendocrine neoplasm that is classified as small-cell NEC and
large-cell NEC and may occur in the nasopharyngeal area (4). However, the recent WHO classification
of nasopharyngeal malignant epithelial tumors does not include NEC
(2). According to the 5th edition
of the WHO Classification of Head and Neck Tumors, the literature
so far indicates that the larynx is the most common site of
occurrence of NECs of the head and neck and accounts for 60% of all
head and neck NECs (4). The
sinonasal tract is a distant second and accounts for 35%; however,
unpublished observations and day-to-day clinical experience may
significantly contradict these statistics and indicate that the
sinonasal tract is the single most common site of occurrence of
head and neck NECs (4). However,
to the best of our knowledge, only sporadic cases of nasopharyngeal
NECs have been reported (5–22).
The present study contributed to the literature and statistics on
nasopharyngeal NEC by describing a rare case of high-grade
nasopharyngeal NEC that exhibited features of large-cell NEC and
small-cell NEC and compared the present case with previously
reported cases. In addition, an updated review of nasopharyngeal
NECs reported in the literature up to May 2022 was provided.
Case report
A 34-year-old female visited the ear, nose and
throat clinic of Panyu Central Hospital (Guangzhou, China) in
September 2021, due to paroxysmal pain in the cheek for nearly half
a year. Nasopharyngeal examination revealed a lump with an
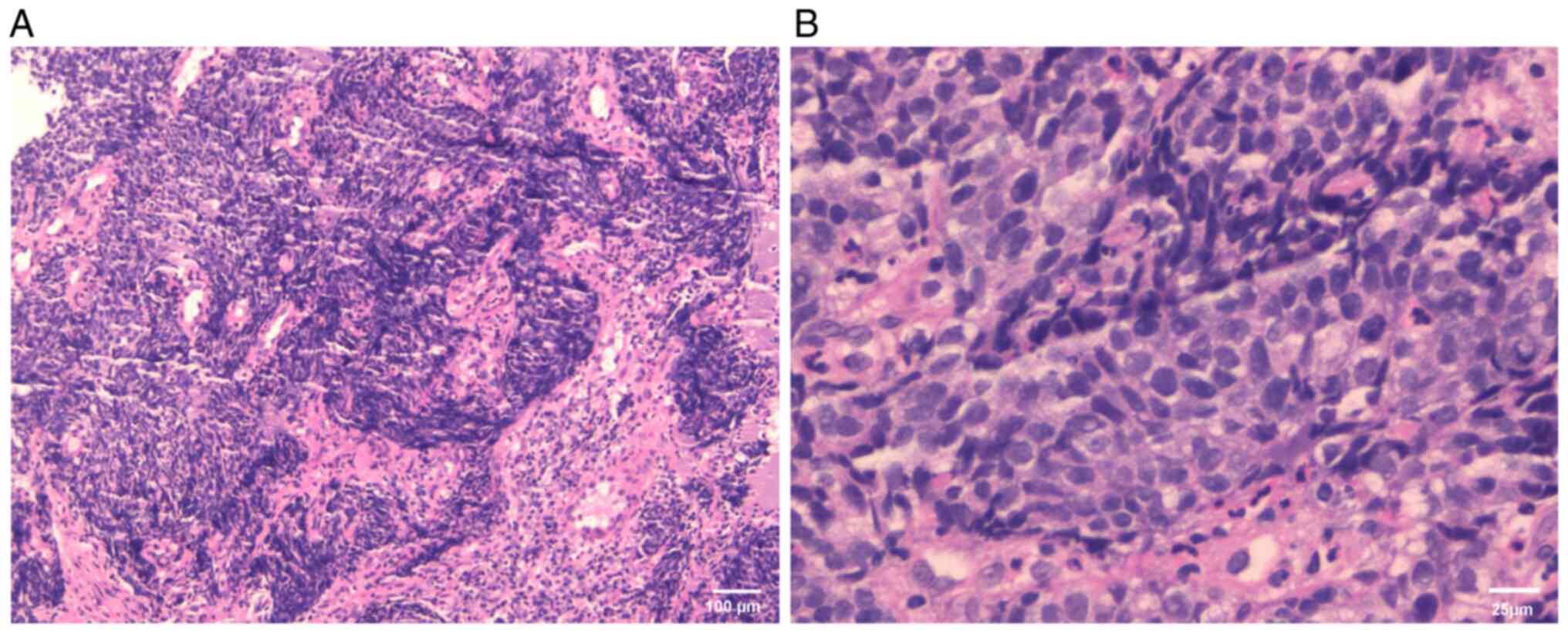
irregular surface. Biopsy of the nasopharyngeal mass and
examination of the sample indicated that the mass contained
invasive cancerous cells arranged in clumps with eosinophilic
cytoplasm. Tumor tissue specimens were fixed, sectioned and stained
according to standard procedures. Hematoxylin and eosin staining
was performed on the tissue samples. This was followed by
immunohistochemical staining in an automated Roche BenchMark1
instrument (Roche Diagnostics) according to the manufacturer's
instructions with standard positive and negative controls using the
following mouse monoclonal antibodies: CD56 (cat. no. MAB-0743),
synaptophysin (cat. no. MAB-0742), cytokeratin (CK; cat. no.
MAB-0671), Ki-67 (cat. no. MAB-0672), neuron-specific enolase (NSE;
cat. no. MAB-0791; all from Fuzhou Maixin Biotech Co., Ltd.) and
thyroid transcription factor-1 (TTF-1; cat. no. ZM-0270; OriGene
Technologies, Inc.). The expression of epidermal growth factor
receptor (EGFR) was tested by using rabbit monoclonal antibody
(RMA-0804, Fuzhou Maixin Biotech Co., Ltd.). All the antibodies
were ready-to-use and optiview diaminobenzidine (DAB)
Immunohistochemistry (IHC) Detection kit (Roche) was used, which
was conducted according to the manufacturer's instructions. The
nuclei of the tumor cells were large, hyperchromatic or vacuolar,
with partially visible nucleoli and obvious heterogeneity (Fig. 1). The Ki-67 index was high at 80%.
The cells were immunopositive for CD56, synaptophysin and CK, and
negative for NSE and TTF-1 (Fig.
2). Based on these features, the nasopharyngeal lump was
identified as a high-grade neuroendocrine carcinoma that exhibits
the features of large-cell NEC and small-cell NEC. In situ
hybridization for Epstein-Barr virus (EBV)-encoded RNA (EBER)
(23), which was performed with an
EBER detection kit (ISH-7001; OriGene Technologies, Inc.) according
to the manufacturer's instructions, indicated that the sample was
positive for EBER (Fig. 2).
The patient was admitted for clinical staging of the
carcinoma. Magnetic resonance imaging of the nasopharynx and neck
confirmed the presence of a massive lump (42×49×31 mm) in the
nasopharynx that had invaded the bone of the skull base and
cavernous sinus, and also involved the right retropharyngeal lymph
node and right cervical lymph node (Fig. 3). Computed tomography (CT) imaging
of the chest and abdomen did not reveal anything remarkable and no
tumors were found at any other sites. Based on these findings, the
tumor was staged as T4N1M0 and the patient received three cycles of
induction chemotherapy (with docetaxel-cisplatin) that was followed
by concurrent chemoradiotherapy with triweekly cisplatin and a
total dose of 70 Gy delivered in 33 fractions. The treatment was
well tolerated and the patient completed the scheduled treatment.
The patient was followed up every three months in the first two
years after treatment. Remission of the tumor was achieved and no
recurrence or metastasis was detected 6 months after the treatment
(Fig. 4).
Literature review
The PubMed database was searched for articles
published up to May 2022 in any language, as well as their
references, using the following search terms: ‘Neuroendocrine
carcinoma’, ‘small cell cancer’, ‘small cell neuroendocrine
carcinoma’, ‘large cell cancer’, ‘large cell neuroendocrine
carcinoma’, ‘nasopharynx’ and ‘nasopharyngeal cancer’. The
epidemiologic features, therapeutic strategies and survival status
of the reported cases, including the present case, were collected
and summarized.
Discussion
The present study described a rare case of
EBV-positive large-cell and small-cell NEC of the nasopharynx. To
the best of our knowledge, this is the first reported case of
nasopharyngeal NEC that exhibits the features of large-cell and
small-cell carcinomas.
The literature review revealed that in a
population-based study, only 60 cases of nasopharyngeal small-cell
carcinoma were identified among 13,993 cases of nasopharyngeal
cancer that were extracted from the Surveillance, Epidemiology, and
End Results database, and there are only 16 literature reviews on
nasopharyngeal small-cell carcinoma (9). Furthermore, another five cases were
reported, including one case of non-small cell neuroendocrine
carcinoma and four cases of EBV-positive large-cell neuroendocrine
carcinoma (6,10,13,15,19).
In addition, one case of human papillomavirus-associated small-cell
carcinoma was reported (22). The
present case was confirmed based on positive immunostaining for
CD56, synaptophysin and CK. TTF-1 has been found to be positive in
cases of extrapulmonary small-cell carcinoma, but the tumor in the
present case was negative for TTF-1. The patient of the present
study was finally diagnosed as having high-grade NEC with the
features of large-cell and small-cell NEC after a number of
consultations with pathologists, and it was thus distinguished from
previously reported cases of NEC (5–22).
In the present case, the tumor was in a locally advanced stage and
had a high Ki-67 index, which is regarded as a marker of cell
proliferation, aggressive biological behavior and poor prognosis
(24,25). The median overall survival of
patients with small-cell carcinoma of the nasopharynx is 18 months,
which is much shorter than that of patients with nasopharyngeal
carcinoma (9). In the present
case, the patient responded well to the treatment and no tumor
recurrence was noted at the 6-month follow-up. However, given its
poor prognosis, consistent and careful follow-up is warranted in
this case.
EBV infection is common worldwide and is associated
with infectious mononucleosis, Burkitt's lymphoma, classical
Hodgkin's lymphoma, gastric cancers and NPC (26). Almost 98% of NPC cases are closely
related to EBV infection (27),
which may promote the progression of NPC (28). A large number of studies have
indicated that the level of free EBV DNA in the plasma of patients
with NPC is highly correlated with its prognosis and is widely used
as a clinical marker in the clinical diagnosis and monitoring of
NPC (1,29). In the present case, the carcinoma
was positive for EBER. This indicates that it may be related to EBV
infection. However, the carcinoma was consistently negative for
plasma EBV DNA during the diagnosis and treatment process, probably
due to the sensitivity, specificity and accuracy of plasma EBV DNA
detection at our hospital. There is no internationally recognized
EBV DNA standardized testing process and comparatively large
interlaboratory variability, even for the same assay using
identical procedures without harmonization (1,30,31).
Furthermore, in previous studies, small-cell cancers were not
associated with EBV infection (5,9,11,22),
while non-small cell cancers, including large-cell cancers, were
associated with EBV infection (6,10,13,15,19).
Therefore, it was still confirmed that NEC was associated with EBV
infection in the present case.
In the present case, the tumor was negative for
EGFR. In contrast to the present findings, it has been reported
that EGFR overexpression is a potential prognostic biomarker for
advanced-stage patients with a poor outcome and is relatively
common in NPC (32). Furthermore,
EGFR is highly expressed in EBV-infected cells and may promote the
neoplastic transformation of EBV-positive cells; importantly, EGFR
may be necessary for the internalization and fusion of EBV in NPC
cells (28). However, only a small
amount of information regarding EGFR expression is available
(5–22), despite non-small cell cancers,
including large-cell cancers, being associated with EBV infection
(6,10,13,15,19).
These results indicate that the biological behaviors of NECs of the
nasopharynx may be different from those of common nasopharyngeal
carcinomas. Therefore, their diagnosis requires further
investigation into the biological behaviors through the study of
additional cases in the future.
Due to its rarity, the treatment of NEC of the
nasopharynx is challenging. The current strategies include
chemotherapy and radiotherapy, and surgery is also considered in
patients with early-stage NEC (9,14).
Based on the findings of a population-based study, patients who
received radiotherapy had prolonged overall survival and the
radiotherapy dose was >60 Gy in most cases (9). Furthermore, most of the reported
cases were treated with radiotherapy (with a dose 70 Gy in the
majority of the cases) and chemotherapy (with cisplatin-etoposide
treatment in most cases) (10,12,15,16,22).
However, most of the chemotherapy regimens have been described for
small-cell cancer of the lung, for which the classic and
conventional chemotherapy regimens include cisplatin-etoposide and
cisplatin-irinotecan, which are regarded as first-line chemotherapy
regimens. Paclitaxel, docetaxel and other regimens are also
effective for lung small-cell cancer (33,34).
By contrast, there is no consensus regarding treatment strategies
for large-cell NEC. Typically, patients with lung large-cell NEC
receive the same treatment as patients with non-small cell
carcinoma, with the cisplatin-etoposide regimen being one of the
most common choices (35,36). The docetaxel-cisplatin regimen is
recommended by the guidelines for nasopharyngeal carcinomas
according to the National Comprehensive Cancer Network and the
Chinese Society of Clinical Oncology (37). Accordingly, in the present case,
the patient received three cycles of induction chemotherapy with
docetaxel-cisplatin and then concurrent chemoradiotherapy (70 Gy
delivered in 33 fractions). After the treatment was completed,
complete remission of the tumor was observed. However, further
follow-up is required to determine the long-term survival outcomes
and these results may contribute to pooled statistics regarding the
survival outcomes in combination with other studies.
In conclusion, the present study was the first, to
the best of our knowledge, to report on a patient with EBV-positive
large-cell and small-cell NEC of the nasopharynx.
Immunohistochemical staining is the gold standard for diagnosis and
the immunohistochemical findings in this case clearly indicated
large-cell and small-cell carcinoma features and the presence of
EBER. There is no standard treatment, but the patient achieved good
complete remission with the standard chemoradiotherapy protocol for
nasopharyngeal carcinomas. Reports on more such cases in the future
will shed light on the clinical behaviors of this rare group of
nasopharyngeal malignant tumors and aid its diagnosis and
treatment. In addition, multidisciplinary consultation may be a
good strategy to determine the appropriate treatment and achieve
optimal treatment effects.
Acknowledgements
The authors would like to thank Dr Yanhua Li
(Radiology Department Central Hospital, Guangzhou, China) and Dr
Qian Yu (Pathology Department, Panyu Central Hospital, Guangzhou,
China) for providing imaging and pathological data.
Funding
The present study was supported by the Panyu Science and
Technology Medical Project, Guangzhou, China (grant no.
2019-Z04-29).
Availability of data and materials
The data are available from the corresponding author
upon reasonable request.
Authors' contributions
GRZ conceived and designed the study. ZS and HWY
acquired the data and acquired and provided the radiology images.
ZS and HWY contributed to the study design and analyzed and
interpreted the data. GRZ supervised the study. ZS and HWY confirm
the authenticity of all the raw data. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
This case report was reviewed and approved by the
Institutional Ethics Committee of Panyu Central Hospital
(Guangzhou, China).
Patient consent for publication
Written informed consent for publication of
anonymous case information was provided by the patient.
Competing interests
The authors have no competing interests to
declare.
Glossary
Abbreviations
Abbreviations:
|
NPC
|
nasopharyngeal carcinoma
|
|
WHO
|
World Health Organization
|
|
NEC
|
neuroendocrine carcinoma
|
|
CK
|
cytokeratin
|
|
NSE
|
neuron-specific enolase
|
|
TTF-1
|
thyroid transcription factor-1
|
|
EBV
|
Epstein-Barr virus
|
|
EBER
|
EBV-encoded RNA
|
|
MRI
|
magnetic resonance imaging
|
|
EGFR
|
epidermal growth factor receptor
|
References
|
1
|
Chen YP, Chan ATC, Le QT, Blanchard P, Sun
Y and Ma J: Nasopharyngeal carcinoma. Lancet. 394:64–80. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Badoual C: Update from the 5th edition of
the World Health Organization classification of head and neck
tumors: Oropharynx and nasopharynx. Head Neck Pathol. 16:19–30.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wang HY, Chang YL, To KF, Hwang JS, Mai
HQ, Feng YF, Chang ET, Wang CP, Kam MK, Cheah SL, et al: A new
prognostic histopathologic classification of nasopharyngeal
carcinoma. Chin J Cancer. 35:412016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Mete O and Wenig BM: Update from the 5th
edition of the World Health Organization classification of head and
neck tumors: Overview of the 2022 WHO classification of head and
neck neuroendocrine neoplasms. Head Neck Pathol. 16:123–142. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lee LY, Chang KP, Hsu CL, Chen TC and Kuo
TT: Small-cell neuroendocrine carcinoma of the nasopharynx: Report
of a rare case lacking association with Epstein-Barr virus. Int J
Surg Pathol. 19:199–202. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Weinreb I and Perez-Ordonez B: Non-small
cell neuroendocrine carcinoma of the sinonasal tract and
nasopharynx. Report of 2 cases and review of the literature. Head
Neck Pathol. 1:21–26. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Lin IH, Hwang CF, Huang HY and Chien CY:
Small cell carcinoma of the nasopharynx. Acta Otolaryngol.
127:206–208. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Galera-Ruiz H, Villar-Rodriguez JL,
Sanchez-Calzado JA, Martin-Mora J and Ruiz-Carmona E: Sinonasal
neuroendocrine carcinoma presenting as a nasopharyngeal mass.
Otolaryngol Head Neck Surg. 124:475–476. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Zhou YL, Peng YP, Liu QD, Chen XZ, He J,
Wei W, Zhong GH, Zhang YQ, Liu Y, Pan JY, et al: Clinical
characteristics and prognosis of small cell carcinoma in the
nasopharynx: A population-based study. Cancer Control.
29:107327482210870752022. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Du YR, Guo CY, Yuan P, Zhang J and Ying
JM: Epstein-Barr virus-positive large cell neuroendocrine carcinoma
of the nasopharynx: Report of a case. Zhonghua Bing Li Xue Za Zhi.
50:530–532. 2021.(In Chinese). PubMed/NCBI
|
|
11
|
Teinor J, Groshek L and He J: Rare case of
metastatic small cell carcinoma of the nasopharynx to the pancreas.
BMJ Case Rep. 13:e2350542020. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Mesolella M, Allosso S, Varricchio S,
Russo D, Pignatiello S, Buono S and Motta G: Small-cell carcinoma
of nasopharynx: A case report of unusual localization. Ear Nose
Throat J. 1455613209737802020.(Epub ahead of print). PubMed/NCBI
|
|
13
|
Cai Z, Lin M, Blanco AI, Liu J and Zhu H:
Epstein-Barr virus-positive large cell neuroendocrine carcinoma of
the nasopharynx: Report of one case and review of the literature.
Head Neck Pathol. 13:313–317. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Bhardwaj N, Kakkar A and Irugu DVK: Small
cell neuroendocrine carcinoma: A rare nasopharyngeal malignancy
with aggressive clinical course. Indian J Otolaryngol Head Neck
Surg. 70:454–458. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Wasserman JK, Papp S, Hope AJ and
Perez-Ordóñez B: Epstein-Barr virus-positive large cell
neuroendocrine carcinoma of the nasopharynx: Report of a case with
complete clinical and radiological response after combined
chemoradiotherapy. Head Neck Pathol. 12:587–591. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Azevedo D, Rios E, Vendeira L and Sarmento
C: Small cell neuroendocrine carcinoma of the nasopharynx: A rare
case report. Autops Case Rep. 7:31–35. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Bellahammou K, Lakhdissi A, Akkar O,
Kouhen F, Rais F, Dahraoui S, M'rabti H and Errihani H: Small-cell
neuroendocrine carcinoma of nasopharynx: A case report. Int J Surg
Med. 3:132–135. 2017. View Article : Google Scholar
|
|
18
|
Takahashi S, Miyashita T, Hoshikawa H,
Haba R, Togami T and Shibata T: Accelerated hyperfractionated
radiotherapy for small cell carcinoma of the nasopharynx. Head
Neck. 37:E63–E65. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Sturgis CD, Burkey BB, Momin S and Hoschar
AP: High grade (large cell) neuroendocrine carcinoma of the
nasopharynx: Novel case report with touch preparation cytology and
positive EBV encoded early RNA. Case Rep Pathol.
2015:2310702015.PubMed/NCBI
|
|
20
|
Lin CH, Chiang TP, Shum WY, Hsu CH, Tsai
YC, Tsao TY and Su CC: Primary small cell neuroendocrine carcinoma
of the nasal cavity after successful curative therapy of
nasopharyngeal carcinoma: A case report. Kaohsiung J Med Sci.
25:145–150. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Deviprasad S, Rajeshwari A, Tahir M,
Adarsha TV and Gangadhara S: Small-cell neuroendocrine carcinoma
originating from the lateral nasopharyngeal wall. Ear Nose Throat
J. 87:E1–E3. 2008.PubMed/NCBI
|
|
22
|
Ma W, Betts G, Dykes M, St Leger D,
Sargent A, Shelton D, Holbrook M and Rana D: Human
papillomavirus-associated small cell carcinoma with synchronous
squamous cell carcinoma in the nasopharynx: Report of a rare case.
Cytopathology. 32:385–388. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Weiss LM and Chen YY: EBER in situ
hybridization for Epstein-Barr virus. Methods Mol Biol.
999:223–230. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Menon SS, Guruvayoorappan C, Sakthivel KM
and Rasmi RR: Ki-67 protein as a tumour proliferation marker. Clin
Chim Acta. 491:39–45. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Shi Z, Jiang W, Chen X, Xu M, Wang X and
Zha D: Prognostic and clinicopathological value of Ki-67 expression
in patients with nasopharyngeal carcinoma: A meta-analysis. Ther
Adv Med Oncol. 12:17588359209513462020. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Yin H, Qu J, Peng Q and Gan R: Molecular
mechanisms of EBV-driven cell cycle progression and oncogenesis.
Med Microbiol Immunol. 208:573–583. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Tsao SW, Tsang CM and Lo KW: Epstein-Barr
virus infection and nasopharyngeal carcinoma. Philos Trans R Soc
Lond B Biol Sci. 372:201602702017. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Peng X, Zhou Y, Tao Y and Liu S:
Nasopharyngeal carcinoma: The role of the EGFR in Epstein-Barr
virus infection. Pathogens. 10:11132021. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Tang LL, Chen YP, Chen CB, Chen MY, Chen
NY, Chen XZ, Du XJ, Fang WF, Feng M, Gao J, et al: The Chinese
society of clinical oncology (CSCO) clinical guidelines for the
diagnosis and treatment of nasopharyngeal carcinoma. Cancer Commun
(Lond). 41:1195–1227. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Kim KY, Le QT, Yom SS, Pinsky BA, Bratman
SV, Ng RH, El Mubarak HS, Chan KC, Sander M and Conley BA: Current
state of PCR-based Epstein-Barr virus DNA testing for
nasopharyngeal cancer. J Natl Cancer Inst. 109:djx0072017.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Le QT, Zhang Q, Cao H, Cheng AJ, Pinsky
BA, Hong RL, Chang JT, Wang CW, Tsao KC, Lo YD, et al: An
international collaboration to harmonize the quantitative plasma
Epstein-Barr virus DNA assay for future biomarker-guided trials in
nasopharyngeal carcinoma. Clin Cancer Res. 19:2208–2215. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Liang R, Yang L and Zhu X: Nimotuzumab, an
anti-EGFR monoclonal antibody, in the treatment of nasopharyngeal
carcinoma. Cancer Control. 28:10732748219893012021. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Smyth JF, Smith IE, Sessa C, Schoffski P,
Wanders J, Franklin H and Kaye SB: Activity of docetaxel (Taxotere)
in small cell lung cancer. The early clinical trials group of the
EORTC. Eur J Cancer. 30A:1058–1060. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Smit EF, Fokkema E, Biesma B, Groen HJ,
Snoek W and Postmus PE: A phase II study of paclitaxel in heavily
pretreated patients with small-cell lung cancer. Br J Cancer.
77:347–351. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Masters GA, Temin S, Azzoli CG, Giaccone
G, Baker SJ Jr, Brahmer JR, Ellis PM, Gajra A, Rackear N, Schiller
JH, et al: Systemic therapy for stage IV non-small-cell lung
cancer: American society of clinical oncology clinical practice
guideline update. J Clin Oncol. 33:3488–3515. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Chinese Medical Association Oncology
Branch, . Lung Cancer Clinical Guidelines for Diagnosis and
Treatment (2021 Edition). Chinese Journal of Oncology. 43:591–621.
2021.PubMed/NCBI
|
|
37
|
Pfister DG, Spencer S, Adelstein D, Adkins
D, Anzai Y, Brizel DM, Bruce JY, Busse PM, Caudell JJ, Cmelak AJ,
et al: Head and neck cancers, version 2.2020, NCCN clinical
practice guidelines in oncology. J Natl Compr Canc Netw.
18:873–898. 2020. View Article : Google Scholar : PubMed/NCBI
|