Introduction
Interdigitating dendritic cell sarcoma (IDCS) is an
extremely rare neoplasm arising from dendritic cells, which can be
subclassified as interdigitating dendritic, follicular dendritic,
Langerhans, or fibroblastic cells (1,2). The
median age at diagnosis is 58 years old with a wide range of 2–88
years old, and the male to female ratio of patients is 1.65:1
(1). Despite its aggressive
clinical features, with a disease-specific mortality rate of 36.4%
as well as the median overall and progression-free survival times
being 12 and 6 months, respectively, no definitive treatment exists
for IDCS due to its low incidence rate (1). Most IDCS tumours arise in the cervical
or axillary lymph nodes, and reports of IDCS in the extranodal
region are scarce (1,3,4).
Cervical lymphadenopathy is typically observed and is rarely
accompanied by systemic symptoms, such as fatigue, fever, or weight
loss. Either surgical resection or radiotherapy are recommended for
the treatment of localised IDCS, whereas chemotherapy is the
preferred option in disseminated IDCS. In some cases, patients are
treated with surgery with or without chemotherapy and/or
radiotherapy. ABVD (doxorubicin, bleomycin vinblastine, and
dacarbazine), CHOP (cyclophosphamide, doxorubicin, cisplatin, and
etoposide), ICE (ifosfamide, cisplatin, and etoposide) or DHAP
(dexamethasone, cisplatin, and high dose cytarabine) are usually
administered as chemotherapy regimens (5). In the present study, the case report
of a patient diagnosed with IDCS located in the parotid gland who
reached a 40-month disease-free survival time following surgical
resection is reported.
Case report
Patient background
A 29-year-old woman presented to Nara Medical
University Hospital (Kashihara, Nara) in April, 2019, with a
2-month history of painful right subaural swelling that was
refractory to antibiotics. A hard mass was palpated at the same
location. The patient had no facial nerve palsy, trismus, or
noteworthy medical history of any disease except type 2 diabetes.
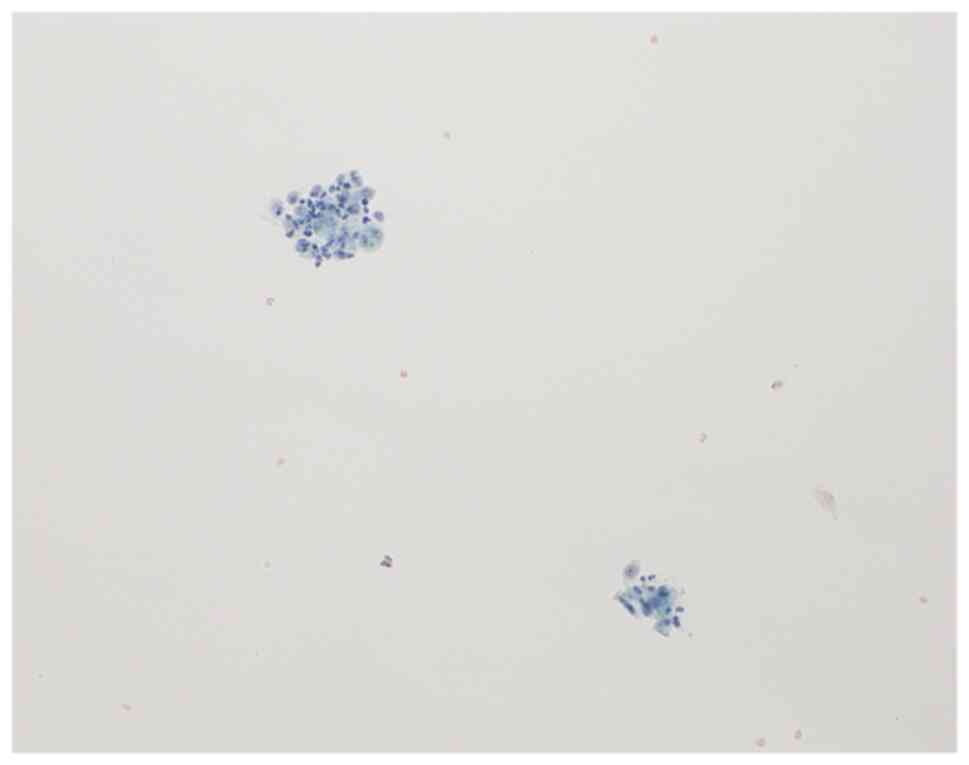
MRI showed a right parotid gland tumour (Fig. 1), which was suspected to be a
malignant neoplasia, as determined using fine needle aspiration
cytology. Cytology indicated the presence of polygonal, oval, and
spindle cells with enlarged nuclei, whereas mucous and squamous
cells were not detected; thus, cytology alone was insufficient to
make a definitive diagnosis (Fig.
2). Subsequently, a biopsy of the tumour was performed and the
histological findings, following immunohistochemical staining,
revealed histiocytic lesions positive for CD68 and S100 and
negative for CD1a and Langerin. By contrast, no epithelial cells
were detected. These results suggested sarcoma, histiocytosis, or
malignant lymphoma (not carcinoma) as differential diagnoses.
18F-fludeoxyglucose (FDG) positron emission
tomography/computed tomography (PET/CT) revealed a parotid gland
tumour with a high uptake of FDG, as well as an ipsilateral lower
cervical lymph node, and no evidence of distant metastasis
(Fig. 3). Furthermore, while the
patient waited for a final pathological diagnosis, the parotid
gland tumour grew rapidly (~10 mm over 4 weeks, as determined by
CT), accompanied with pain. Since a final diagnosis had not been
achieved, an appropriate chemotherapy regimen could not be
selected, and chemotherapy could therefore not be performed.
Similarly, radiotherapy was not performed as its effectiveness
could not be confirmed owing to a lack of final diagnosis. The
patient consented to undergo a right partial parotidectomy and
lymphadenectomy to treat and alleviate the symptoms and to assist
in a more accurate diagnosis after consultation with
haematologists.
Surgery
Firstly, a lymphadenectomy of the right lower
cervical region was performed. The lymph node was resected with
peripheral tissue owing to the partial invasion of the peripheral
fascia and strap muscles. Secondly, a right partial parotidectomy
was performed. Separate incisions were made during the two
surgeries. After the main branch of the facial nerve was
identified, it was traced back to the periphery. It was then
determined that the parotid gland tumour had invaded the peripheral
tissue. Intraoperative frozen diagnosis was performed to identify
the surgical margin. The right parotid tumour was removed en
bloc with the peripheral tissue. The great auricular,
accessory, and hypoglossal nerves were preserved.
Pathology
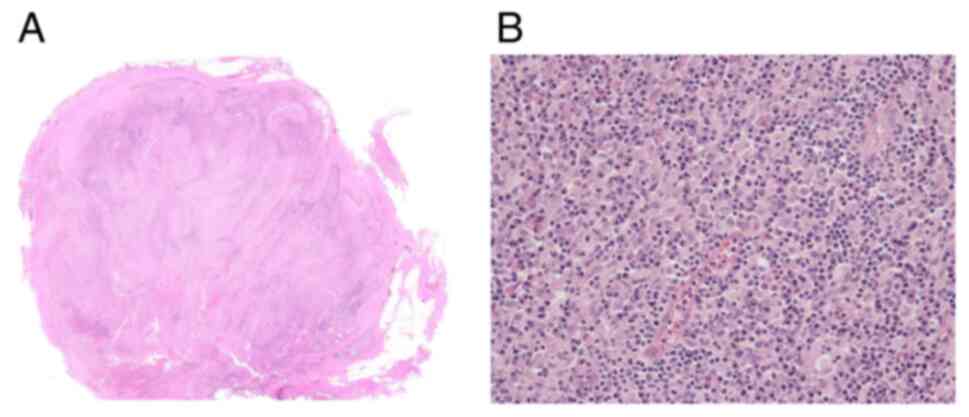
Histological examination of the surgically resected
specimen from the right parotid gland (45×42×35 mm) revealed a
histiocytic tumour with proliferating atypical spindle cells. These
spindle cells had an abundant and slightly eosinophilic cytoplasm
and moderately to highly atypical nuclei that were interspersed
among small lymphocytes and plasma cells (Fig. 4). The tumour cells were irregularly
invasive to the peripheral fat and muscular tissues. Multinucleated
and tumour cells with emperipolesis were also observed but no
necrosis was detected. Immunohistochemical analysis showed that the
tumour was positive for S100 (diffuse and strong), CD68, CD163,
CD209, and fascin, whereas it was negative for CD1a, Langerin,
HMB45, epithelial membrane antigen, EBER1 in situ
hybridization, CD21, CD23, CD43, CD56, CD123, myeloperoxidase, BRAF
V600E, CAM5.2, and AE1/AE3 (Fig.
5). The histology of the right lower cervical lymph node was
similar to that of the parotid gland tumour. Based on these
results, the patient was diagnosed with IDCS.
Outcome and follow-up
Facial nerve palsy was not observed after the
surgery, and there were no notable adverse events. During the
follow-up period, the patient did not receive additional therapy;
however, the patient was evaluated using investigations such as CT,
ultrasound scan, or PET/CT. The health condition of the patient
remained stable without evidence of recurrence for 40 months after
surgery.
Discussion
IDCS is an extremely rare and aggressive neoplasm
that mainly affects the cervical lymph nodes, with IDCS in
extranodal lesions rarely being reported (1,3,4). To
the best of our knowledge, the present study is only the fifth
report of an IDCS located in the parotid gland, and it represents
the longest follow-up period among IDCS cases (6–9).
Although surgery, chemotherapy, radiotherapy, or a combination
thereof has been used to treat IDCS, there is currently no
established treatment strategy for these cases (1,3,4,10).
Moreover, the lack of specific disease markers makes diagnosing
IDCS challenging and thus, the median time to a final diagnosis is
12.5 weeks (1). In the present case
report, the final diagnosis was reached after 16 weeks.
Unfortunately, the patient needed to start treatment while waiting
for a final diagnosis owing to rapid tumour growth accompanied with
painful symptoms. Due to the lack of a final diagnosis, the
effectiveness of chemotherapy and radiotherapy was unknown;
therefore, surgery was adopted. Neck dissection was avoided since
the first biopsy results indicated no carcinoma. Resection of the
parotid tumour was performed, and the ipsilateral lower cervical
lymph node was resected to make a final diagnosis.
Since there are no specific disease markers for
IDCS, diagnosis relies on the exclusion of other diseases, such as
melanoma, other dendritic cell-related neoplasias, metastases of
other malignant neoplasias, and histiocytic sarcoma (HS) (2,11). In
the evaluated specimen, the cytoplasm was mainly eosinophilic with
an indistinct border, and the nuclei were irregular, moderately to
highly atypical, and pleomorphic. Although these histological
findings established the IDCS diagnosis, HS was not ruled out.
Expression of S100, CD68, CD163, CD209, and fascin was observed
using immunohistochemical analysis. Although expression of these
markers is distinctive of IDCS and HS, the extent of S100 (diffuse
and strong) and CD209 expression (CD209 has not been reported in
HS) confirmed the diagnosis of IDCS (1,2). Other
diseases, including melanoma and other dendritic cell-related
neoplasias, were ruled out based on histological findings and
negative immunohistochemical staining results (2). Moreover, bone marrow aspiration biopsy
may also help to exclude tumour invasion and other hematopoietic
diseases, although this was not performed in the present case
report.
The patient in the present study was fairly young
(29 years old) compared with those in the 4 other reported cases of
IDCS in the parotid gland, all of whom were >50 years of age
(3). A young age may indicate a
poor prognosis, based on the results of a previous study (12); however, owing to the limited
evidence from the small number of cases of parotid gland IDCS
previously reported, this hypothesis may not be correct. A previous
review suggested that surgical resection may improve survival rate,
although there is no general consensus on treatment strategy
(1). In the present case report,
surgery was performed based on intraoperative frozen diagnosis,
which was used to identify the surgical margin. Complete surgical
tumour resection is expected to be an effective method to control
IDCS without relapse, if the tumour is localised and resectable.
Close follow-up with some imaging studies after surgery is also
required. Additionally, several examinations, such as bone marrow
aspiration biopsy, may be necessary when the patient's condition
worsens, as PET/CT is not always sensitive for hematopoietic
tumours. Moreover, genetic sequencing of tumour tissue may provide
an explanation for the present patient's long disease-free survival
time as well as add valuable information to the diagnosis, since
numerous sarcomas have fusion gene mutations; this was not
conducted in the present study, as the patient did not give
permission for the analysis. To date, only a few previous reports
describe the association between gene mutation and IDCS (13).
IDCS undergoes diverse clinical courses and its
aetiology remains unknown (3,4). Until
sufficient clinical information is available, patients with IDCS
will continue to undergo treatment without an established strategy.
Moreover, it is difficult to define a treatment strategy if the
health condition of the patient worsens due to a delayed final
diagnosis. In the present case report, the patient achieved a
long-term survival time of 40 months (at the last follow-up) after
surgical resection even though postoperative adjuvant therapy was
not performed, according to the choice of the patient.
In conclusion, the case of a patient with IDCS
located in the parotid gland with a 40-month disease-free survival
time after surgical resection was described in the present study.
IDCS management is characterised by challenges in diagnosis and a
lack of a standardised treatment protocol. The present case report
suggests that surgical resection may be an effective treatment
option for local IDCS, supporting long-term disease-free survival
time. Further studies are required to establish a definitive
diagnosis and treatment strategy for IDCS.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analysed during the current
are available from the corresponding author on reasonable
request.
Authors' contributions
AT, HU, MM, MT and TK contributed to the study's
conception and design. Material preparation, data collection and
analysis were performed by AT, HU and MM. The first draft of the
manuscript was written by AT, and all authors commented on previous
versions of the manuscript. AT and MM confirm the authenticity of
all the raw data. All authors read and approved the final version
of the manuscript.
Ethics approval and consent to
participate
The study design was approved by The Ethics
Committee of The Nara Medical University Hospital (Kashihara,
Japan; proposal no. 3298), and the study was conducted in
accordance with the guidelines of the Declaration of Helsinki.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of this case report.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
IDCS
|
interdigitating dendritic cell
sarcoma
|
|
FDG
|
18F-fludeoxyglucose
|
|
PET/CT
|
positron emission tomography/ computed
tomography
|
|
HS
|
histiocytic sarcoma
|
References
|
1
|
Muhammed A, Ahmed ARH, Maysa H, Mohamed
AES, Abd-ElLateef AA and Elnakib E: New insights inside the
interdigitating dendritic cell sarcoma-pooled analysis and review
of literature. Ann Hematol. 98:2641–2651. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Facchetti F, Pileri SA, Lorenzi L,
Tabanelli V, Rimsza L, Pittaluga S, Dirnhofer S, Copie-Bergman C,
de Leval L, Rosenwald A, et al: Histiocytic and dendritic cell
neoplasms: What have we learnt by studying 67 cases. Virchows Arch.
471:467–489. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Lupato V, Romeo S, Franchi A, Mantovani M,
Dei Tos AP, Tirelli G, Da Mosto MC and Boscolo-Rizzo P: Head and
neck extranodal interdigitating dendritic cell sarcoma: Case report
and review of the literature. Head Neck Pathol. 10:145–151. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Xue T, Jiang XN, Wang WG, Zhou XY and Li
XQ: Interdigitating dendritic cell sarcoma: Clinicopathologic study
of 8 cases with review of the literature. Ann Diagn Pathol.
34:155–160. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Diego CR, Luis MJS and Samir D:
Interdigitating dendritic cell sarcoma. Atlas Genet Cytogenet Oncol
Haematol. 23:317–319. 2019.PubMed/NCBI
|
|
6
|
Sharma M, Ahsan F, Ah-See KW, McKean ME,
Kain R and Chapman AD: Interdigitating dendritic cell sarcoma of
the parotid gland. J Laryngol Otol. 120:244–246. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Efune G, Sumer BD, Sarode VR, Wang HY and
Myers LL: Interdigitating dendritic cell sarcoma of the parotid
gland: Case report and literature review. Am J Otolaryngol.
30:264–268. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Barwell N, Howatson R, Jackson R, Johnson
A, Jarrett RF and Cook G: Interdigitating dendritic cell sarcoma of
salivary gland associated lymphoid tissue not associated with HHV-8
or EBV infection. J Clin Pathol. 57:87–89. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Park YH, Kim SI, Choi SJ, Lim JH, Yi HG,
Lee MH and Kim CS: A case of disseminated extranodal
interdigitating dendritic cell sarcoma arising from parotid gland.
Kosin Med J. 30:163–169. 2015. View Article : Google Scholar
|
|
10
|
Olnes MJ, Nicol T, Duncan M, Bohlman M and
Erlich R: Interdigitating dendritic cell sarcoma: A rare malignancy
responsive to ABVD chemotherapy. Leuk Lymphoma. 43:817–821. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Johnson RL, Boisot S, Ball ED and Wang HY:
A case of interdigitating dendritic cell sarcoma/histiocytic
sarcoma-a diagnostic pitfall. Int J Clin Exp Pathol. 7:378–385.
2013.PubMed/NCBI
|
|
12
|
Saygin C, Uzunaslan D, Ozguroglu M,
Senocak M and Tuzuner N: Dendritic cell sarcoma: A pooled analysis
including 462 cases with presentation of our case series. Crit Rev
Oncol Hematol. 88:253–271. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wang HY, Li S, Woodford RL, Mills SE and
Cousar JB: BCL2 chromosomal translocation is not a general feature
of the interdigitating dendritic cell sarcoma. Diagn Mol Pathol.
19:169–171. 2010. View Article : Google Scholar : PubMed/NCBI
|