Introduction
Lung cancer is the most common cause of
cancer-related death, of which non-small cell lung cancer (NSCLC)
comprises 85–90% (1). Despite the
development of treatments, the 5-year survival rate is <15%
(2). Paget's ‘seed-soil’ theory
demonstrates that the tumor microenvironment (TME) has a vital role
in tumor growth and progression (3). The TME is a complex and dynamic
community, among which immune infiltrating cells and vascular
endothelial cells are the most representative factors (4). Macrophages, important representatives
of immune infiltrating cells, act as vital components of the host's
defense, antigen-presenting cells and effector cells, and may be
classified into the classic M1 type or the alternative M2 type
(5,6). M1 type macrophages are a tumor
suppressor type that participate in inflammatory response, pathogen
removal and antitumor immunity, while M2 type macrophages promote
the occurrence and development of tumors by inducing angiogenesis
and anti-inflammation (7).
Macrophages have different biological properties due to different
distributions (8), so the selection
of macrophage markers and tissue sites of interest affect the
prognostic role of tumor-associated macrophages (TAMs) on NSCLC, to
a certain extent. CD68+ is the TAM marker that is
commonly considered to be a pan-macrophage marker, but it cannot
distinguish between M1 and M2 subtypes (9). M2 macrophages have a variety of
surface markers, including CD163, CD204 and CD206. Among them,
CD206, which is expressed on the surface of most classes of
macrophages and dendritic cell subgroups, is routinely used to
identify the M2 subtype (10).
Certain studies suggest that a higher stromal TAM density is an
independent prognostic factor and leads to poor prognosis (11,12).
However, M2 macrophage density is more closely related to poor
prognosis than CD68+ TAMs (13,14).
Studies have confirmed that a tumor is only a minor
and asymptomatic lesion prior to the formation of angiogenesis
(15,16). With the formation of angiogenesis,
the tumor size rapidly increases and has an enhanced potential for
distant metastasis (17,18). CD105 is an endoglin used to evaluate
blood vessels that is considered to only recognize abnormal blood
vessels induced by tumors, and it has higher specificity than CD34
(19,20). In addition, studies have indicated
that TAMs and cancer cells may promote tumor angiogenesis and
metastasis (21–26). Immune checkpoint inhibitors
targeting the programmed cell death protein-1 (PD-1)/PD-ligand 1
(PD-L1) pathway have demonstrated an impressive clinical benefit in
NSCLC and the expression of PD-L1 may partially predict the
treatment effectiveness (27). TAMs
are able to secrete vascular endothelial growth factors, such as
IL-10, secrete IL-1 β, induce regulatory T cells, increase PD-L1
expression in tumor cells and inhibit the function of effector T
cells, leading to infiltration and distant metastasis of cancer
cells (28).
The present study focused on the temporal-spatial
distribution and quantitative expression of CD68+ and
CD206+ TAMs in two intra-tumor areas, and CD105 and
PD-L1 in the TME, to investigate the heterogenic molecular profile
of the TME, in an attempt to provide a guide for improving the
individual treatment strategy for patients with NSCLC.
Materials and methods
Patients and samples
A total of 92 paraffin-embedded NSCLC samples were
collected from Zhejiang Cancer Hospital (Hangzhou, China) between
April 2008 and January 2014. Using these samples, 6 tissue
microarrays (TMAs) were constructed, as previously described
(29). For construction, a 3-mm
core was taken from each representative tumor tissue. The study
protocol was approved by The Ethics Committee of Zhejiang Cancer
Hospital (Hangzhou, China) and the patients provided written
informed consent regarding the use of their tissues. The main
patient inclusion criteria were as follows: i) Histologically
confirmed primary NSCLC; ii) patient underwent curative radical
surgery. Patients who had received other anticancer treatment prior
to surgery were excluded. Tumor staging was based on the 8th
Tumor-Node-Metastasis classification system of the American Joint
Committee on Cancer staging criteria (30). The last follow-up date was April
2017, at which point all patients had died. Overall survival (OS)
time was defined as the interval from the date of surgery to the
date of death. Disease-free survival (DFS) time was defined as the
interval from the date of surgery to the date of disease
progression.
Immunohistochemistry (IHC) and
multiplexed immunofluorescence
IHC staining for macrophages marked by CD68 and
CD206, and tumor neo-vessels marked by CD105 and PD-L1, was
performed. In brief, TMA slides were treated by deparaffinization
in xylene, hydration with graded alcohols and subjected to antigen
retrieval (98°C, 20 min). The slides were then placed in 3%
hydrogen peroxide for 10 min at room temperature to inactivate
endogenous peroxidases. After washing three times in PBS, the
slides were blocked with 2% BSA (cat. no. B2064; Sigma-Aldrich;
Merck KGaA) for 30 min at room temperature, followed by incubation
with primary antibodies against CD68 (1:200 dilution; cat. no.
ab125212; Abcam), CD206 (1:200; cat. no. 60143–1-Ig; ProteinTech
Group, Inc.), CD105 (1:500; cat. no. ab2529; Abcam) and PD-L1
(1:100; cat. no. ab205921; Abcam) at 4°C overnight. After washing
in PBS, the slides were incubated with secondary antibody (1:200;
Goat Anti-Rabbit IgG (horseradish peroxidase, cat. no. ab150077;
Abcam) for 60 min at 37°C. The slides were visualized using Dako
REAL EnVision™ (DAB; cat. no. PW017; Sangon Biotech, Co., Ltd.) and
counterstained with haematoxylin for 2 min at room temperature.
Multiplexed immunofluorescence staining for CD68 and
CD105 was also performed. The primary antibodies against CD68 and
CD105 were mixed. Similar to IHC, after the secondary
immunofluorescent antibody (1:2,000; Goat Anti-Rabbit IgG and Goat
Anti-Mouse IgG (horseradish peroxidase), cat. nos. ab6721 and
ab6789; Abcam) was incubated with the slides (37°C, 60 min), all
slides were covered by Fluoroshield containing DAPI (Abcam) for 10
min at room temperature to identify nuclei.
Quantification of IHC and
immunofluorescent staining
All slides were examined under an Olympus BX51
fluorescence microscope equipped with an Olympus DP72 camera
(Olympus Corporation). Positive staining was indicated by brownish
granules. The macrophages marked by CD68 and CD206 were counted in
three high-power fields selected at the tumor islets and tumor
stroma, and the mean number of CD68+ and
CD206+ cells in these three fields was documented. Tumor
islets were defined as areas where tumor cells accounted for
>70% of the total cells, and tumor stroma as areas where tumor
stromal cells accounted for >70% of the total cells (12). Tumor neo-vessels marked by CD105 and
tumor cells expressing PD-L1 were counted in six high-power fields
selected at the tumor site and the mean cell counts were
documented. Pathologists defined positively expressed cells
according to the Hue, Saturation, Intensity (HSI) color selection
system (H=0-30; S=0-255; I=0-255), specified cell size and filtered
non-specific positive color rendering noise <50 pixels, after
which the software automatically counted. Positive cell counting
was completed using Image-Pro Plus 6.0 software (Media Cybernetics,
Inc). The cut-off value according to the median of each group was
used to determine the density of infiltrating macrophages, tumor
neo-vessel density and PD-L1 expression. Two independent
pathologists who were blinded to the clinicopathological
characteristics of all tissue specimens participated in the data
evaluation.
Statistical analysis
Statistical analyses were performed with SPSS 25.0
(IBM Corp.) and R 4.2.2 (R Development Core Team). For categorical
data, the χ2 test was performed. Spearman's rank
correlation analysis was used to analyze the correlation between
macrophages, tumor neo-vessels and PD-L1 expression. Differences in
the CD68+ and CD206+ TAMs among the groups
were analyzed by the Mann-Whitney U-test. The Kaplan-Meier method
was used to estimate the survival curve for OS time, and the
log-rank or two-stage tests were used to assess the differences in
survival between groups. The Cox regression model was used to
assess the influence of the binary factors in univariate and
multivariate analyses. The factors with P<0.2 in the univariate
analysis were included in the multivariate analysis, and the
relationship between TME-related markers and prognosis was
examined. A two-tailed P<0.05 was considered to indicate
statistical significance.
Results
Major clinicopathological features of
the 92 NSCLC cases and heterogenic TME in TMAs
Among the 92 NSCLC cases included in the present
study, 71 (77.2%) were male and 21 (22.8%) were female, and they
were aged 39–75 (median, 61) years. With regards to staging, there
was 1 (1.1%) case of IA, 9 (9.8%) cases of IB, 7 (7.6%) of IIA, 23
(25%) of IIB, 44 (47.8%) of IIIA and 8 (8.7%) of IIIB. A total of
58 patients underwent adjuvant therapy, 40 of which received
adjuvant chemotherapy, 12 received adjuvant radiotherapy and
chemotherapy, 5 received adjuvant radiotherapy and 1 received
tyrosine kinase inhibitor treatment. A total of 16 patients did not
receive any adjuvant therapy and the therapy regimen of the
remaining 18 patients was unknown. The two-stage test demonstrated
that there was no significant difference in OS and DFS times
between the treatment and no-treatment groups (median OS, 30 vs. 23
months, respectively; P=0.571; median DFS, 11 vs. 13 months,
respectively; P=0.844; Fig. S1).
There were 73 known progression or recurrence events, and the
treatments of 51 patients were known. Among these 51 patients, 30
(58.8%) received two or more combined treatments, 19 (37.3%)
received one treatment strategy and 2 (3.9%) did not receive any
treatment. These treatments had no impact on the OS time between
single treatment, multiple treatments and no-treatment (median OS,
33 vs. 36 vs. 6 months, respectively; P=0.289; Fig. S1). Other major clinicopathological
characteristics data available, such as smoking status, tumor size,
histology and differentiation, are presented in Tables I and II.
 | Table I.Relationship between CD68+
TAMs, CD206+ TAMs and the clinicopathological features
of patients with non-small cell lung cancer. |
Table I.
Relationship between CD68+
TAMs, CD206+ TAMs and the clinicopathological features
of patients with non-small cell lung cancer.
|
|
| CD68+
TAMsa | CD206+
TAMs |
|---|
|
|
|
|
|
|---|
|
|
| Tumor islets | Tumor stroma | Tumor islets | Tumor stroma |
|---|
|
|
|
|
|
|
|
|---|
| Clinicopathological
feature | Total number of
patients | Low n=46 | High n=45 | P-value | Low n=46 | High n=45 | P-value | Low n=47 | High n=45 | P-value | Low n=46 | High n=46 | P-value |
|---|
| Sex |
|
|
| 0.193 |
|
| 0.759 |
|
| 0.390 |
|
| 0.804 |
|
Female | 21 | 8 (38.1) | 13 (61.9) |
| 10 (47.6) | 11 (52.4) |
| 9 (42.9) | 12 (57.1) |
| 11 (52.4) | 10 (47.6) |
|
|
Male | 71 | 38 (54.3) | 32 (45.7) |
| 36 (51.4) | 34 (48.6) |
| 38 (53.5) | 33 (46.5) |
| 35 (49.3) | 36 (50.7) |
|
| Age, years |
|
|
| 0.908 |
|
| 0.760 |
|
| 0.982 |
|
| 0.294 |
|
≤60 | 41 | 21 (51.2) | 20 (48.8) |
| 20 (48.8) | 21 (51.2) |
| 21 (51.2) | 20 (48.8) |
| 23 (56.1) | 18 (43.9) |
|
|
>60 | 51 | 25 (50.0) | 25 (50.0) |
| 26 (52.0) | 24 (48.0) |
| 26 (51.0) | 25 (49.0) |
| 23 (45.1) | 28 (54.9) |
|
| Smoking status |
|
|
| 0.320 |
|
| 0.691 |
|
| 0.552 |
|
| 1.000 |
| Never
smoker | 26 | 11 (42.3) | 15 (57.7) |
| 14 (53.8) | 12 (46.2) |
| 12 (46.2) | 14 (53.8) |
| 13 (50.0) | 13 (50.0) |
|
|
Current/former | 66 | 35 (53.8) | 30 (46.2) |
| 32 (49.2) | 33 (50.8) |
| 35 (53.0) | 31 (47.0) |
| 33 (50.0) | 33 (50.0) |
|
| Histology |
|
|
| 0.607 |
|
| 0.107 |
|
| 0.549 |
|
| 1.000 |
|
Adenocarcinoma | 54 | 28 (52.8) | 25 (47.2) |
| 23 (43.4) | 30 (56.6) |
| 29 (53.7) | 25 (46.3) |
| 27 (50.0) | 27 (50.0) |
|
|
Non-adenocarcinoma | 38 | 18 (50.5) | 20 (52.6) |
| 23 (60.5) | 15 (39.5) |
| 18 (47.4) | 20 (52.6) |
| 19 (50.0) | 19 (50.0) |
|
| Tumor size, cm |
|
|
| 0.423 |
|
| 0.606 |
|
| 0.879 |
|
| 0.381 |
| ≤5 | 60 | 28 (47.5) | 31 (52.5) |
| 31 (52.5) | 28 (47.5) |
| 31 (51.7) | 29 (48.3) |
| 32 (53.3) | 28 (46.7) |
|
|
>5 | 32 | 18 (56.3) | 14 (43.8) |
| 15 (46.9) | 17 (53.1) |
| 16 (50.0% | 16 (50.0) |
| 14 (43.8) | 18 (56.3) |
|
|
Differentiationb |
|
|
| 0.413 |
|
| 0.144 |
|
| 0.371 |
|
| 0.631 |
|
Low | 16 | 5 (33.3) | 10 (66.7) |
| 6 (40.0) | 9 (60.0) |
| 11 (68.8) | 5 (31.3) |
| 10 (62.5) | 6 (37.5) |
|
|
Moderate | 34 | 18 (52.9) | 16 (47.1) |
| 13 (38.2) | 21 (61.8) |
| 17 (50.0) | 17 (50.0) |
| 17 (50.0) | 17 (50.0) |
|
|
High | 31 | 16 (51.6) | 15 (48.4) |
| 19 (61.3) | 12 (38.7) |
| 15 (48.4) | 16 (51.6) |
| 15 (48.4) | 16 (51.6) |
|
| Lymph node
metastasis |
|
|
| 0.603 |
|
| 0.941 |
|
| 0.038 |
|
| 0.026 |
|
Negative | 30 | 14 (46.7) | 16 (53.3) |
| 15 (50.0) | 15 (50.0) |
| 20 (66.7) | 10 (33.3) |
| 20 (66.7) | 26 (41.9) |
|
|
Positive | 62 | 32 (52.5) | 29 (47.5) |
| 31 (50.8) | 30 (49.2) |
| 27 (43.5) | 35 (56.5) |
| 10 (33.3) | 36 (58.1) |
|
| Stage |
|
|
| 0.072 |
|
| 0.168 |
|
| 0.820 |
|
| 0.209 |
| I,
II | 42 | 25 (61.0) | 16 (39.0) |
| 24 (58.5) | 17 (41.5) |
| 22 (52.4) | 20 (47.6) |
| 24 (57.1) | 18 (42.9) |
|
|
III | 50 | 21 (42.0) | 29 (58.0) |
| 22 (44.0) | 28 (56.0) |
| 25 (50.0) | 25 (50.0) |
| 22 (44.0) | 28 (56.0) |
|
 | Table II.Relationship between CD105, PD-L1 and
the clinicopathological features of non-small cell lung cancer. |
Table II.
Relationship between CD105, PD-L1 and
the clinicopathological features of non-small cell lung cancer.
|
|
| CD105-positive
cells | PD-L1-positive
cells |
|---|
|
|
|
|
|
|---|
| Clinicopathological
feature | Total number of
patients | Low n=46 | High n=46 | P-value | Low n=46 | High n=46 | P-value |
|---|
| Sex |
|
|
| 0.804 |
|
| 0.082 |
|
Female | 21 | 11 (52.4) | 10 (47.6) |
| 14 (66.7) | 7 (33.3) |
|
|
Male | 71 | 35 (49.3) | 36 (50.7) |
| 32 (45.1) | 39 (54.9) |
|
| Age, years |
|
|
| 0.294 |
|
| 0.529 |
|
≤60 | 41 | 18 (43.9) | 23 (56.1) |
| 19 (46.3) | 22 (53.7) |
|
|
>60 | 51 | 28 (54.9) | 23 (45.1) |
| 27 (52.9) | 24 (47.1) |
|
| Smoking status |
|
|
| 0.643 |
|
| 0.552 |
| Never
smoked | 26 | 12 (46.2) | 14 (53.8) |
| 16 (61.5) | 10 (38.5) |
|
|
Current/former smoker | 66 | 34 (51.5) | 32 (48.5) |
| 30 (45.5) | 36 (47.0) |
|
| Histology |
|
|
| 0.672 |
|
| 0.165 |
|
Adenocarcinoma | 54 | 26 (48.1) | 28 (51.9) |
| 25 (46.3) | 29 (54.5) |
|
|
Non-adenocarcinoma | 38 | 20 (52.6) | 18 (47.4) |
| 21 (55.3) | 17 (44.7) |
|
| Tumor size, cm |
|
|
| 0.381 |
|
| 0.662 |
| ≤5 | 60 | 28 (46.7) | 32 (53.5) |
| 31 (51.7) | 29 (48.3) |
|
|
>5 | 32 | 18 (56.3) | 14 (43.8) |
| 15 (46.9) | 17 (53.1) |
|
|
Differentiationa |
|
|
| 0.691 |
|
| 0.399 |
|
Low | 16 | 9 (56.3) | 7 (43.8) |
| 7 (43.8) | 9 (56.3) |
|
|
Moderate | 34 | 15 (44.1) | 19 (55.9) |
| 16 (47.1) | 18 (52.9) |
|
|
High | 31 | 16 (51.6) | 15 (48.4) |
| 19 (61.3) | 12 (38.7) |
|
| Lymph node
metastasis |
|
|
| 0.656 |
|
| 0.656 |
|
Negative | 30 | 14 (46.7) | 16 (53.3) |
| 14 (46.7) | 16 (53.3) |
|
|
Positive | 62 | 32 (51.6) | 30 (48.4) |
| 32 (51.6) | 30 (48.4) |
|
| Stage |
|
|
| 0.675 |
|
| 0.209 |
| I,
II | 42 | 20 (47.6) | 22 (52.4) |
| 24 (57.1) | 18 (42.9) |
|
|
III | 50 | 26 (52.0) | 24 (48.0) |
| 22 (44.0) | 28 (56.0) |
|
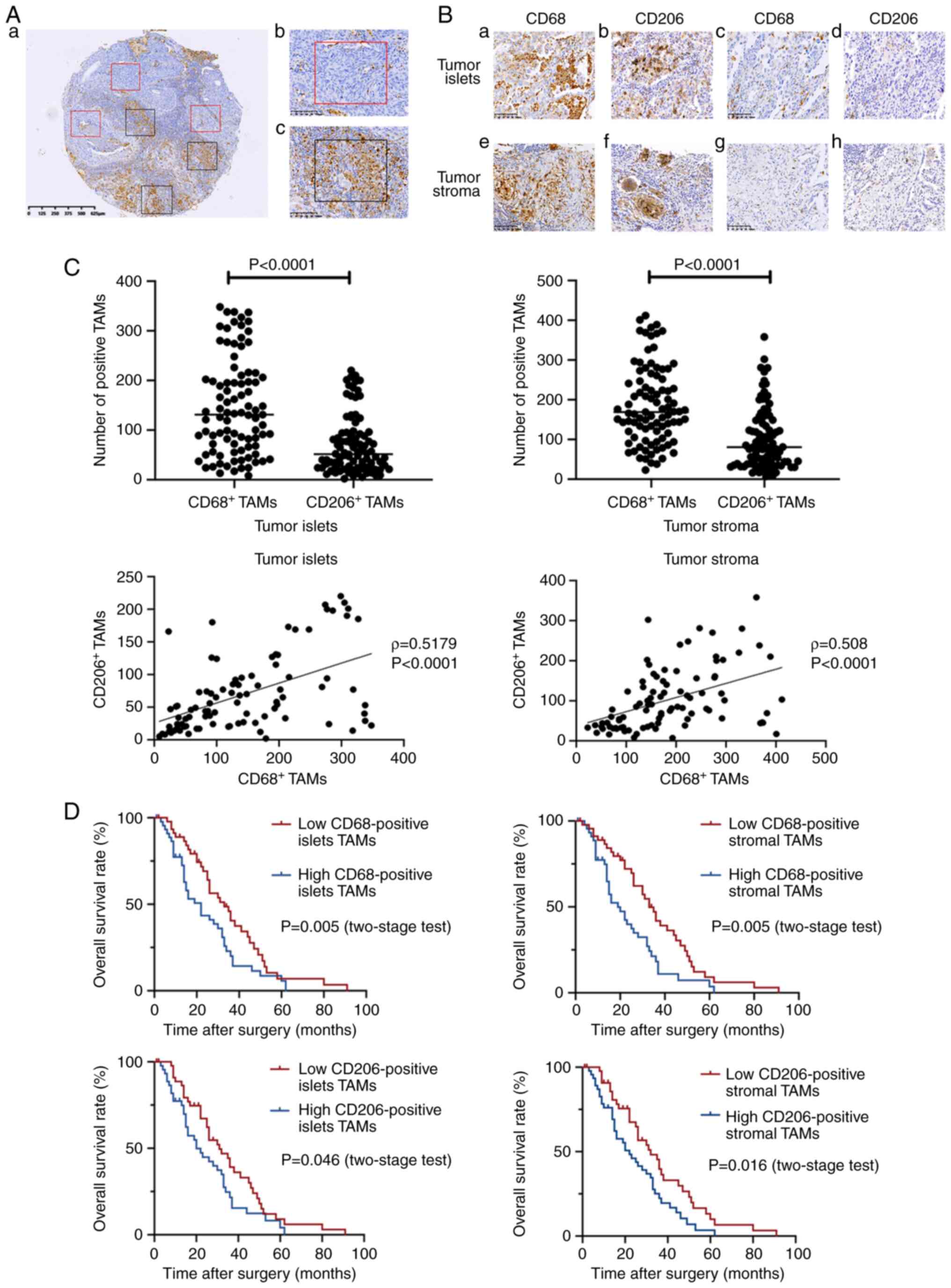
IHC analysis, including distribution and
quantitative measurement of CD68+ TAMs,
CD206+ TAMs, CD105 and PD-L1, was performed on all TMAs.
In certain cases, only few CD68+ and CD206+
TAMs were present compared with other cases with high expression
(‘expression’ here and throughout means the density of cells with
positive expression) (Fig. 1A and
B). The quantitative data demonstrated that in tumor islets,
the mean numbers of CD68+ and CD206+ TAMs
were 146 (median, 131; range, 8–348) and 70 (median, 52; range,
2–220), respectively (P<0.001). In tumor stroma, the mean
numbers of CD68+ and CD206+ TAMs were 186
(median, 169; range, 23–412) and 103 (median, 81; range, 7–358),
respectively (P<0.001). Therefore, the quantity of
CD68+ TAMs was higher than that of CD206+
TAMs in tumor islets and stroma. The CD68+ and
CD206+ TAMs also had a higher distribution in tumor
stroma than in tumor islets (both P<0.0001). In addition,
significant correlations were found between the distributions of
CD68+ and CD206+ TAMs in each area (tumor
islets, ρ=0.5179; tumor stroma, ρ=0.5081; both P<0.0001;
Fig. 1C). According to the median
of CD68+ and CD206+ TAMs in the tumor islets
and stroma as the cut-off, the patients were divided into the
low-density or high-density group. The survival analysis
demonstrated that patients with low expression of CD68+
and CD206+ TAMs in tumor islets and stroma had a
favorable prognosis (Fig. 1D).
CD105 and PD-L1 staining were mainly located in the
cytoplasm or on the cell membrane of the tumor stroma. Tumor
neo-vessels and PD-L1 were also heterogeneously expressed in the
TME, in certain cases with low expression and other cases with high
expression. The quantitative density of CD105+ cells in
tumor tissues was 19–368 (median, 156). The quantitative density of
PD-L1+ cells in tumor tissues was 9–493 (median, 103)
(Fig. 2A and B). According to the
median density of cells with positive CD105 and PD-L1 expression in
tumor tissues as the cut-off, patients were divided into the
low-density or high-density group. The survival analysis
demonstrated that the CD105 density had no association with OS time
in patients with NSCLC, whereas patients with high PD-L1 expression
had a higher risk of death (Fig.
2C).
Correlations between CD68+
and CD206+ TAMs, tumor neo-vessels, PD-L1 expression and
clinicopathological features
The quantitative data of CD68+ and
CD206+ TAM density are provided in Table I. For CD68+ and
CD206+ TAMs in tumor islets and stroma, the cut-off to
classify low and high subgroups. Subgroups were as follows: in the
tumor islets, less than 131 is the low CD68+TAM
expression group, more than or equal to 131 is the high
CD68+TAM expression group, less than 52 is the low
CD206+TAM expression group, more than or equal to 52 is
the high CD206+TAM expression group; in tumor stroma,
less than 169 is the low CD68+TAM expression group, more
than or equal to 169 is the high CD68+TAM expression
group, less than 81 is the low CD206+TAM expression
group, more than or equal to 81 is the high CD206+TAM
expression group. For tumor neo-vessels and PD-L1 in tumor tissues,
the cut-off to classify low and high subgroups was 156 and 103,
respectively. In the low and high CD68+ TAM subgroups,
the high tumor neo-vessel density cases were 20 (43.5%) and 26
(56.5%), respectively. In the low and high PD-L1 expression
subgroups, high densities of CD68+ TAMs were observed in
18 (40.9%) and 26 cases (59.1%), respectively. In the low and high
CD206+ TAM subgroups, 21 (45.7%) and 25 (54.3%) cases
had high tumor neo-vessel density, respectively. In the low and
high PD-L1 expression subgroups, there were 15 (33.3%) and 30
(66.7%) cases with high CD68+ TAM density, respectively.
Of note, tumor neo-vessels, CD68+ TAMs and PD-L1
expression were not significantly associated with any of the
clinicopathological characteristics, which indicated that these key
components of the TME were independent of clinical features,
including tumor size, tumor histological type, degree of
differentiation, lymph node metastasis and tumor staging (Tables I and II).
In addition, CD68+ TAMs were mostly
localized with tumor neo-vascularization, and the quantitative
analysis demonstrated that CD68+ TAMs and CD105 had
similar trends in expression (ρ=0.2401; P=0.021; Fig. 3), while there was no obvious
correlation between CD206+ TAMs and CD105 (ρ=0.109;
P>0.05; data not shown). Furthermore, the expression of
CD68+ TAMs was significantly correlated to the
expression of PD-L1 in tumor tissues (ρ=0.332; P=0.030; data not
shown) and there was a significant correlation between
CD206+ TAMs and PD-L1 (ρ=0.428; P=0.038; data not
shown).
Prognostic significance of tumor
stromal features in NSCLC
Univariate analyses demonstrated that clinical
factors, such as tumor differentiation, were associated with OS
time (P<0.05). PD-L1 and CD68+ TAM densities in tumor
islets and stroma were also negatively associated with DFS time
(both P<0.05), but there was no statistically significant
independent predictor of DFS time in NSCLC (Table SI). PD-L1 and CD68+ TAM
densities in tumor islets and stroma, as well as CD206+
TAM density in tumor stroma, were negatively associated with OS
time (P<0.05 for all). Furthermore, tumor size, differentiation
degree, high density of CD68+ TAMs in tumor islets and
PD-L1 expression were statistically significant independent
predictors of a poor prognosis in NSCLC (P<0.05 for all;
Table III).
 | Table III.Univariate and multivariate analyses
of the clinicopathological factors for overall survival time of
patients with non-small cell lung carcinoma. |
Table III.
Univariate and multivariate analyses
of the clinicopathological factors for overall survival time of
patients with non-small cell lung carcinoma.
|
| Univariate
analysis | Multivariate
analysis |
|---|
|
|
|
|
|---|
| Clinicopathological
factor | HR | (95% CI) | P-value | HR | (95% CI) | P-value |
|---|
| Sex (male vs.
female) | 0.980 | 0.572–1.678 | 0.941 |
|
|
|
| Age, years (>60
vs. ≤60) | 1.269 | 0.804–2.005 | 0.306 |
|
|
|
| Smoking status
(smoker vs. never-smoker) | 1.162 | 0.698–1.932 | 0.564 | 0.505 | 0.160–1.593 | 0.244 |
| Histological type
(adenocarinoma vs. non-adenocarinoma) | 0.734 | 0.462–1.168 | 0.192 | 0.444 | 0.167–1.183 | 0.104 |
| Tumor size, cm
(>5 vs. ≤5) | 1.373 | 0.850–2.218 | 0.195 | 1.945 | 1.089–3.475 | 0.025 |
|
Differentiation |
|
| 0.045 |
|
| 0.033 |
| Low vs.
moderate | 2.118 | 1.087–4.127 | 0.028 | 0.595 | 0.252–1.406 | 0.237 |
| Low vs.
high | 1.752 | 1.013–3.030 | 0.045 | 0.336 | 0.146–0.774 | 0.010 |
| Lymph node
metastasis (positive vs. negative) | 0.909 | 0.694–1.190 | 0.486 | 0.810 | 0.384–1.710 | 0.581 |
| Stage (III vs. I,
II) | 1.123 | 0.706–1.785 | 0.624 | 0.785 | 0.374–1.645 | 0.521 |
| CD105 expression
(high vs. low) | 1.106 | 0.698–1.753 | 0.667 | 1.002 | 0.998–1.005 | 0.301 |
| PD-L1 expression
(high vs. low) | 1.685 | 1.066–2.663 | 0.025 | 1.003 | 1.001–1.011 | 0.010 |
| CD68+
TAMs in tumor islets (high vs. low) | 1.666 | 1.051–2.641 | 0.030 | 1.006 | 1.001–1.011 | 0.031 |
| CD206+
TAMs in tumor islets (high vs. low) | 1.580 | 0.996–2.506 | 0.052 | 0.999 | 0.991–1.007 | 0.750 |
| CD68+
TAMs in tumor stroma (high vs. low) | 1.916 | 1.202–3.055 | 0.006 | 1.000 | 0.995–1.005 | 0.941 |
| CD206+
TAMs in tumor stroma (high vs. low) | 1.741 | 1.091–2.776 | 0.020 | 0.999 | 0.993–1.005 | 0.725 |
The aforementioned key components were explored
collectively to reveal the association between TME and NSCLC
prognosis. For the combined group, taking the median values for
tumor neo-vessels, macrophages and PD-L1 as the cut-off, the
patients could be divided into groups. The groups were assigned as
follows: Group 1, all components were expressed at a low level;
group 2, one or two of the components was expressed at a high
level; group 3, all components were expressed at a high level. The
combined analysis indicated that the OS rate of group 3 was worse
than that of groups 1 and 2 (Fig.
4).
Discussion
A number of conflicting results have been reported
regarding the prognostic significance of TAMs, tumor neo-vessels
and PD-L1/PD-1 expression in NSCLC from clinical practice (31–35).
The reasons for the inconsistent reports may be related to the
choice of markers, as well as differences in statistical power and
evaluation methods. In addition, these factors have not been
observed to be adequately reliable as a single biomarker to
evaluate the prognosis of patients with NSCLC (36,37).
To the best of our knowledge, the present study was the first to
compare TAM distribution detecting CD68+ and
CD206+ in two intra-tumor areas, and to compare the
distribution of TAMs, tumor neo-vessels and PD-L1 in NSCLC.
The results demonstrated that the number of
CD68+ and CD206+ TAMs was higher in the tumor
stroma but lower in tumor islets, and there was a correlation
between the distribution of CD68+ and CD206+
TAMs in tumor islets and stroma. Furthermore, the mean numbers of
CD68+ TAMs in each location of the tumor islets and
stroma were significantly higher than those of CD206+
TAMs. Univariate analysis demonstrated that a large number of
CD68+ and CD206+ TAMs in the tumor stroma
were associated with a shorter OS time, which is consistent with
the results of Li et al (12) and Dai et al (11). The former study also demonstrated
that the tumor stroma is the most suitable intra-tumor area for
evaluating the relationship between TAMs and prognosis of NSCLC
cases. The present study also found that CD206+ stromal
TAMs, CD105 and PD-L1 had a relationship with prognosis. When the
number of positive cells in each section (tumor islets and tumor
stroma) was summed, and CD68+ or CD206+ TAMs
were combined with the other two key components, the high density
of the three components may indicate a worse prognosis within 30
months of surgery.
New blood vessels support rapid tumor tissue growth,
providing nutrients and oxygen to thriving tumor cells (38). However, in the present study, tumor
neo-vessel density was not significantly correlated with the
prognosis of patients with NSCLC, but there was a significant
correlation between CD68+ and CD105. These results
suggested that macrophages have a significant role in tumor
neo-vessels in the process of cancer invasion and metastasis. TAMs
are considered to be ‘angiogenesis switches’ and a key factor
leading to a proangiogenic environment (26,39).
In the present study, it was observed that PD-L1
expression was correlated with the prognosis of NSCLC and may be
used as an independent prognostic factor for patients with NSCLC.
PD-L1 mediates immunosuppressive signals and certain studies
suggest that PD-L1 upregulation is associated with longer survival
time in early NSCLC (40), breast
carcinoma (41), gastric cancer
(42) and colorectal cancer
(43). However, another study has
indicated that there is no association between PD-L1 expression and
OS (44). A number of previous
studies have reported that high PD-L1 expression is associated with
poor prognosis in NSCLC (45–47).
In these studies, the definition of PD-L1+ or high
density was different, leading to difficulties in concluding on the
relationship between PD-L1 expression and NSCLC prognosis. Evidence
suggests that PD-L1 upregulation is an adaptive mechanism and may
be a response of tumor cells to host immune pressure (48). It is also understood that PD-L1
expression is related to the endogenous immune response, such as
tumor-infiltrating lymphocytes in NSCLC and indoleamine
2,3-dioxygenase-1 expression by dendritic cells (49). It may therefore be suggested that
any possible prognostic significance is not directly related to a
single immune signal but to the overall balance between the host's
antitumor immune response and tumor-mediated immunosuppression.
The present study demonstrated that the expression
of PD-L1 in cancer cells was correlated with the density of
CD68+ and CD206+ TAMs. M2 type macrophages
have a weak antigen-presenting capacity and suppress T-cell immune
responses by releasing immunosuppressive factors, such as TGF-β and
IL-10 (50). In the hypoxic TME,
the expression of certain immunosuppressive factors, such as
prostaglandin E2 (PGE-2) and IL-10, not only inhibits the
activation of M1 macrophages, but also converts the generated M1
type to the M2 type (51).
In conclusion, the distribution of stromal
macrophages and M2 type TAMs are important factors affecting other
key components in the TME. The present study demonstrated that the
different immunological molecular profiles of the TME were
associated with the prognosis of patients with NSCLC. There are
also certain limitations to the present study. The number of cases
was small and treatments of patients after postoperative
recurrent-metastasis is incomplete. Further studies with a larger
sample size are required to be conducted to gain a deeper
understanding and explanation of this mechanism. To the best of our
knowledge, the present study was the first to provide a
multi-component combined prognostic survival analysis of different
types of macrophages in different regions with tumor neo-vessels
and PD-L1, and the combined analysis of key components may improve
the prediction of the prognosis.
Supplementary Material
Supporting Data
Supporting Data
Acknowledgements
Not applicable.
Funding
This research was supported by the grants of The National
Natural Science Foundation of China (grant no. 81703018) and The
Zhejiang Medical and Health Science and Technology Project (grant
nos. 2020KY466 and 2022RC110), both to MF.
Availability of data and materials
The datasets generated and/or analyzed during the
current study are not publicly available due to restrictions
applied by The Cancer Hospital of the University of Chinese Academy
(Zhejiang Cancer Hospital, Hangzhou, China) but are available from
the corresponding author on reasonable request.
Authors' contributions
Conception and design: MF and XL. Administrative
support: MF and XL. Provision of study materials or patients: MF
and XL. Collection and assembly of data: MF, QH and HY. Data
analysis and interpretation: MF, QH, HY, GC and SY. Manuscript
writing: HY and QH. HY and MF confirm the authenticity of all the
raw data. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
All procedures performed in the present study
involving human participants were in accordance with the
Declaration of Helsinki (as revised in 2013). The study was
approved by the Institutional Ethics committee of Zhejiang Cancer
Hospital (Hangzhou, China; approval no. IRB-2021-111). Written
informed consent was obtained from each patient.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2020. CA Cancer J Clin. 70:7–30. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Liu X, Shen SL and Wang YP: Current ststus
of comprehensive interventional therapy for advanced non-small cell
lung cancer. Zhonghua Fei Bu Ji Bing Za Zhi (Dian Zi Ban).
10:486–489. 2017.(In Chinese).
|
|
3
|
Paget S: The distribution of secondary
growths in cancer of the breast. 1889. Cancer Metastasis Rev.
8:98–101. 1989.PubMed/NCBI
|
|
4
|
Catalano V, Turdo A, Di Franco S, Dieli F,
Todaro M and Stassi G: Tumor and its microenvironment: A
synergistic interplay. Semin Cancer Biol. 23:522–532. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mosser DM and Edwards JP: Exploring the
full spectrum of macrophage activation. Nat Rev Immunol. 8:958–969.
2008. View
Article : Google Scholar : PubMed/NCBI
|
|
6
|
Schmieder A, Michel J, Schonhaar K, Goerdt
S and Schledzewski K: Differentiation and gene expression profile
of tumor-associated macrophages. Semin Cancer Biol. 22:289–297.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Pollard JW: Tumour-educated macrophages
promote tumour progression and metastasis. Nat Rev Cancer. 4:71–78.
2004. View
Article : Google Scholar : PubMed/NCBI
|
|
8
|
Joshi N, Walter JM and Misharin AV:
Alveolar macrophages. Cell Immunol. 330:86–90. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Falini B, Flenghi L, Pileri S, Bigerna B,
Durkop H, Eitelbach F, Thiele J, Pacini R and Cavaliere A: PG-M1: A
new monoclonal antibody directed against a fixative-resistant
epitope on the macrophage-restricted form of the CD68 molecule. Am
J Pathol. 142:1359–1372. 1993.PubMed/NCBI
|
|
10
|
Gordon S: Alternative activation of
macrophages. Nat Rev Immunol. 3:23–35. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Dai F, Liu L, Che G, Yu N, Pu Q, Zhang S,
Ma J, Ma L and You Z: The number and microlocalization of
tumor-associated immune cells are associated with patient's
survival time in non-small cell lung cancer. BMC Cancer.
10:2202010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Li Z, Maeda D, Yoshida M, Umakoshi M,
Nanjo H, Shiraishi K, Saito M, Kohno T, Konno H, Saito H, et al:
The intratumoral distribution influences the prognostic impact of
CD68- and CD204-positive macrophages in non-small cell lung cancer.
Lung Cancer. 123:127–135. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Komohara Y, Jinushi M and Takeya M:
Clinical significance of macrophage heterogeneity in human
malignant tumors. Cancer Sci. 105:1–8. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Sumitomo R, Hirai T, Fujita M, Murakami H,
Otake Y and Huang CL: M2 tumor-associated macrophages promote tumor
progression in non-small-cell lung cancer. Exp Ther Med.
18:4490–4498. 2019.PubMed/NCBI
|
|
15
|
Hicklin DJ and Ellis LM: Role of the
vascular endothelial growth factor pathway in tumor growth and
angiogenesis. J Clin Oncol. 23:1011–1027. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Lin CY, Siow TY, Lin MH, Hsu YH, Tung YY,
Jang T, Recht L and Chang C: Visualization of rodent brain tumor
angiogenesis and effects of antiangiogenic treatment using 3D
ΔR2-µMRA. Angiogenesis. 16:785–793. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Sajib S, Zahra FT, Lionakis MS, German NA
and Mikelis CM: Mechanisms of angiogenesis in microbe-regulated
inflammatory and neoplastic conditions. Angiogenesis. 21:1–14.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Li S, Xu HX, Wu CT, Wang WQ, Jin W, Gao
HL, Li H, Zhang SR, Xu JZ, Qi ZH, et al: Angiogenesis in pancreatic
cancer: Current research status and clinical implications.
Angiogenesis. 22:15–36. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Weidner N, Folkman J, Pozza F, Bevilacqua
P, Allred EN, Moore DH, Meli S and Gasparini G: Tumor angiogenesis:
A new significant and independent prognostic indicator in
early-stage breast carcinoma. J Natl Cancer Inst. 84:1875–1887.
1992. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Akagi K, Ikeda Y, Sumiyoshi Y, Kimura Y,
Kinoshita J, Miyazaki M and Abe T: Estimation of angiogenesis with
anti-CD105 immunostaining in the process of colorectal cancer
development. Surgery. 131:S109–S113. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Wu TH, Li YY, Wu TL, Chang JWC, Chou WC,
Hsieh LL, Chen JR and Yeh KY: Culture supernatants of different
colon cancer cell lines induce specific phenotype switching and
functional alteration of THP-1 cells. Cell Immunol. 290:107–115.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Yeo EJ, Cassetta L, Qian BZ, Lewkowich I,
Li JF, Stefater JA III, Smith A, Wiechmann LS, Wang Y, Pollard JW
and Lang RA: Myeloid WNT7b mediates the angiogenic switch and
metastasis in breast cancer. Cancer Res. 74:2962–2973. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Ohba K, Miyata Y, Kanda S, Koga S, Hayashi
T and Kanetake H: Expression of urokinase-type plasminogen
activator, urokinase-type plasminogen activator receptor and
plasminogen activator inhibitors in patients with renal cell
carcinoma: Correlation with tumor associated macrophage and
prognosis. J Urol. 174:461–465. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Allavena P, Sica A, Solinas G, Porta C and
Mantovani A: The inflammatory micro-environment in tumor
progression: The role of tumor-associated macrophages. Crit Rev
Oncol Hematol. 66:1–9. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Han B, Li K, Zhao Y, Li B, Cheng Y, Zhou
J, Lu Y, Shi Y, Wang Z, Jiang L, et al: Anlotinib as a third-line
therapy in patients with refractory advanced non-small-cell lung
cancer: A multicentre, randomised phase II trial (ALTER0302). Br J
Cancer. 118:654–661. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Murdoch C, Muthana M, Coffelt SB and Lewis
CE: The role of myeloid cells in the promotion of tumour
angiogenesis. Nat Rev Cancer. 8:618–631. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Anagnostou VK and Brahmer JR: Cancer
immunotherapy: A future paradigm shift in the treatment of
non-small cell lung cancer. Clin Cancer Res. 21:976–984. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Noman MZ, Desantis G, Janji B, Hasmim M,
Karray S, Dessen P, Bronte V and Chouaib S: PD-L1 is a novel direct
target of HIF-1α, and its blockade under hypoxia enhanced
MDSC-mediated T cell activation. J Exp Med. 211:781–790. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Dancau AM, Simon R, Mirlacher M and Sauter
G: Tissue microarrays. Methods Mol Biol. 576:49–60. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Goldstraw P, Chansky K, Crowley J,
Rami-Porta R, Asamura H, Eberhardt WRR, Nicholson AG, Groome P,
Mitchell A, Bolejack V, et al: The IASLC lung cancer staging
project: Proposals for revision of the TNM stage groupings in the
forthcoming (Eighth) edition of the TNM Classification for lung
cancer. J Thorac Oncol. 11:39–51. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Zhang QW, Liu L, Gong CY, Shi HS, Zeng YH,
Wang XZ, Zhao YW and Wei YQ: Prognostic significance of
tumor-associated macrophages in solid tumor: A meta-analysis of the
literature. PLoS One. 7:e509462012. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Du ZY, Shi MH, Ji CH and Yu Y: Serum
pleiotrophin could be an early indicator for diagnosis and
prognosis of non-small cell lung cancer. Asian Pac J Cancer Prev.
16:1421–1425. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Keskin S, Kutluk AC and Tas F: Prognostic
and predictive role of angiogenic markers in non- small cell lung
cancer. Asian Pac J Cancer Prev. 20:733–736. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Huang W, Ran R, Shao B and Li H:
Prognostic and clinicopathological value of PD-L1 expression in
primary breast cancer: A meta-analysis. Breast Cancer Res Treat.
178:17–33. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Yagi T, Baba Y, Ishimoto T, Iwatsuki M,
Miyamoto Y, Yoshida N, Watanabe M and Baba H: PD-L1 Expression,
tumor-infiltrating lymphocytes, and clinical outcome in patients
with surgically resected esophageal cancer. Ann Surg. 269:471–478.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Patel SP and Kurzrock R: PD-L1 expression
as a predictive biomarker in cancer immunotherapy. Mol Cancer Ther.
14:847–856. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Brahmer J, Reckamp KL, Baas P, Crinò L,
Eberhardt WEE, Poddubskaya E, Antonia S, Pluzanski A, Vokes EE,
Holgado E, et al: Nivolumab versus docetaxel in advanced
squamous-cell non-small-cell lung cancer. New Eng J Med.
373:123–135. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Muz B, de la Puente P, Azab F and Azab AK:
The role of hypoxia in cancer progression, angiogenesis,
metastasis, and resistance to therapy. Hypoxia (Auckl). 3:83–92.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Mazzieri R, Pucci F, Moi D, Zonari E,
Ranghetti A, Berti A, Politi LS, Gentner B, Brown JL, Naldini L and
De Palma M: Targeting the ANG2/TIE2 axis inhibits tumor growth and
metastasis by impairing angiogenesis and disabling rebounds of
proangiogenic myeloid cells. Cancer Cell. 19:512–526. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Cooper WA, Tran T, Vilain RE, Madore J,
Selinger CI, Kohonen-Corish M, Yip P, Yu B, O'Toole SA, McCaughan
BC, et al: PD-L1 expression is a favorable prognostic factor in
early stage non-small cell carcinoma. Lung Cancer. 89:181–188.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Schalper KA, Velcheti V, Carvajal D,
Wimberly H, Brown J, Pusztai L and Rimm DL: In situ tumor PD-L1
mRNA expression is associated with increased TILs and better
outcome in breast carcinomas. Clin Cancer Res. 20:2773–2782. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Zheng Z, Bu Z, Liu X, Zhang L, Li Z, Wu A,
Wu X, Cheng X, Xing X, Du H, et al: Level of circulating PD-L1
expression in patients with advanced gastric cancer and its
clinical implications. Chin J Cancer Res. 26:104–111.
2014.PubMed/NCBI
|
|
43
|
Droeser RA, Hirt C, Viehl CT, Frey DM,
Nebiker C, Huber X, Zlobec I, Eppenberger-Castori S, Tzankov A,
Rosso R, et al: Clinical impact of programmed cell death ligand 1
expression in colorectal cancer. Eur J Cancer. 49:2233–2242. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Sorensen SF, Zhou W, Dolled-Filhart M and
Georgsen J: 1328ppd-L1 expression and survival among advanced
non-small cell lung cancer (Nsclc) patients treated with
chemotherapy. Ann Oncol. 25 (Suppl 4):iv467. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Li H, Xu Y, Wan B, Song Y, Zhan P, Hu Y,
Zhang Q, Zhang F, Liu H, Li T, et al: The clinicopathological and
prognostic significance of PD-L1 expression assessed by
immunohistochemistry in lung cancer: A meta-analysis of 50 studies
with 11,383 patients. Transl Lung Cancer Res. 8:429–449. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Keller MD, Neppl C, Irmak Y, Hall SR,
Schmid RA, Langer R and Berezowska S: Adverse prognostic value of
PD-L1 expression in primary resected pulmonary squamous cell
carcinomas and paired mediastinal lymph node metastases. Mod
Pathol. 31:101–110. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Igawa S, Sato Y, Ryuge S, Ichinoe M,
Katono K, Hiyoshi Y, Otani S, Nagashio R, Nakashima H, Katagiri M,
et al: Impact of PD-L1 expression in patients with surgically
resected non-small-cell lung cancer. Oncology. 92:283–290. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Taube JM, Anders RA, Young GD, Xu H,
Sharma R, McMiller TL, Chen S, Klein AP, Pardoll DM, Topalian SL
and Chen L: Colocalization of inflammatory response with B7-h1
expression in human melanocytic lesions supports an adaptive
resistance mechanism of immune escape. Sci Transl Med.
4:127ra1372012. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Mandarano M, Bellezza G, Belladonna ML,
Van den Eynde BJ, Chiari R, Vannucci J, Mondanelli G, Ludovini V,
Ferri I, Bianconi F, et al: Assessment of TILs, IDO-1, and PD-L1 in
resected non-small cell lung cancer: An immunohistochemical study
with clinicopathological and prognostic implications. Virchows
Arch. 474:159–168. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Sumitomo R, Hirai T, Fujita M, Murakami H,
Otake Y and Huang CL: PD-L1 expression on tumor-infiltrating immune
cells is highly associated with M2 TAM and aggressive malignant
potential in patients with resected non-small cell lung cancer.
Lung Cancer. 136:136–144. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Wen ZF, Liu H, Gao R, Zhou M, Ma J, Zhang
Y, Zhao J, Chen Y, Zhang T, Huang F, et al: Tumor cell-released
autophagosomes (TRAPs) promote immunosuppression through induction
of M2-like macrophages with increased expression of PD-L1. J
Immunother Cancer. 6:1512018. View Article : Google Scholar : PubMed/NCBI
|