Introduction
Rhabdomyosarcoma (RMS) is a prevalent soft-tissue
sarcoma comprising striated muscle and rhabdomyoblast cells at
different stages of differentiation (1,2). RMS
may occur not only in areas with striated muscle but also in areas
without striated muscle (3). RMS is
classified as embryonal, alveolar, pleomorphic and spindle
cell/sclerotic according to the World Health Organisation 2020
classification of soft-tissue and bone tumors (1,2).
Alveolar RMS (ARMS) accounts for 31% of all cases and occurs
commonly in individuals aged 10–25 years, mostly in the
extremities, followed by the trunk or the perineural region
(4). Occurrence in the stomach is
extremely rare and an early definitive diagnosis is difficult
(5). The tumors are highly
malignant and prone to distant lymph node metastasis (6). RMS of the stomach is extremely rare,
with only four previously published cases (4–7). The
reported cases have included epithelioid (4,5),
pleomorphic (6) and embryonal
(7) RMS of the stomach. To the best
of our knowledge, the present study contains the first reported
case of primary gastric ARMS. There is very little information on
the outcome of chemotherapy and imaging information of gastric
rhabdomyosarcoma that has been reported. The present study
describes a case of primary gastric alveolar RMS that was
successfully treated in Handan Central Hospital (Handan, China).
Moreover, the differential diagnosis is discussed in terms of
diagnostic imaging.
Case report
A healthy 20-year-old female patient visited Handan
Central Hospital in March 2021 with intermittent abdominal pain for
>1 month, which was noticeable after meals and gradually
worsened, accompanied by melena. The physical examination revealed
no specific findings. The iron level was 2.5 µmol/l (reference
range, 7.8-32.2 µmol/l). Gastroscopy revealed a 2.5-cm deep ulcer
on the side of the lower greater curvature of the gastric body. The
ulcer was covered with white moss and the surrounding mucosa was
edematous. The biopsy tissue pathology revealed a neuroendocrine
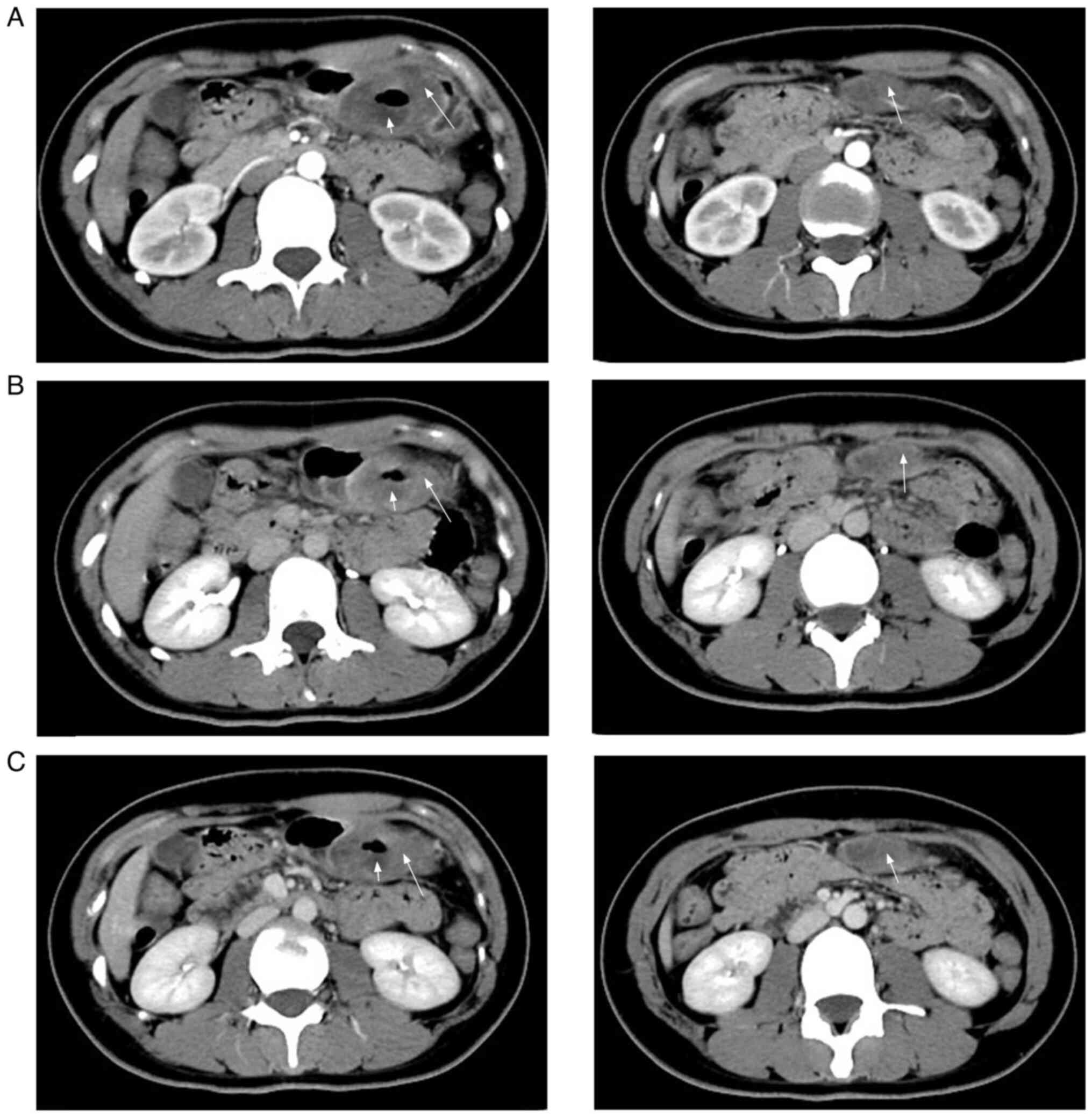
tumor. An abdominal enhancement computed tomography (CT) scan
showed a thick and ulcerated distal wall of the gastric body
bulging into the gastric cavity (>4.5×2.0 cm). A deep depression
with poorly defined borders was also evident (Fig. 1A). In the venous (Fig. 1B) and equilibrium (Fig. 1C) phases, the ulcer was not
strengthened, whereas the peripheral parenchyma was slightly
strengthened. A round nodule with uneven density, slight
hypointensity in the middle and well-defined borders was detected
beneath the lesion (Fig. 1A).
Enhancement scans revealed curved enhancement at the nodal edges.
In the coronal scans, the second lesion was poorly demarcated from
the gastric mucosa, and the two lesions were connected in the
coronal position in the venous phase (Fig. 2). It was difficult to establish
whether it was an enlarged lymph node or a tumor protruding from
the gastric body. Considering the age of the patient and the
present illness, the imaging diagnosis revealed lateral
displacement of the greater curvature of the stomach with malignant
difficulty.
A laparoscopic-assisted radical distal gastrectomy
(Bi II anastomosis) was performed under general anesthesia.
Intraoperatively, the tumor was located on the lateral side of the
greater curvature of the gastric body (~6×5 cm) and protruded from
the body. No mass was observed outside the body. The sections were
lightly counterstained with hematoxylin and eosin.
Immunohistochemical staining was performed using the horseradish
peroxidase complex, and reaction products were visualized by
benzidine reaction. The sections were observed using a light
microscope at a scale of 100 microns. The postoperative pathology
showed small round tumor cells under light microscopy (Fig. 3). Immunohistochemistry showed the
following results: CD56, vimentin and desmin, positive;
MyoD1, nuclear weakly positive; Bcl-2 and CD99,
partially weakly positive; and myogenin, myoglobin,
myeloperoxidase, epithelial membrane antibody, smooth muscle actin,
CK, chromogranin A, cytokeratin (CK)8/18, CK20, CD30, CD4,
synaptophysin, Wilms tumor protein, anaplastic lymphoma kinase and
friend leukemia virus integration, negative. The Ki67 positive
index was ~70%. A definitive diagnose was difficult and so the
patient was initially diagnosed with a gastric ulcer round cell
malignancy. However, the specimen was sent to Renmin Hospital of
Wuhan University for further testing, where fluorescence in
situ hybridization (FISH) detected FOX01 gene isolation with
amplification. The final diagnosis after combining
immunohistochemistry and FISH testing results was gastric ARMS. The
pathology of the second lesion revealed that it was a lymphatic
metastasis. At 1 month post-surgery, enlarged lymph nodes were
noted at the left supracostal margin and right supraclavicular
region. Pathology revealed malignant metastasis. Therefore,
adjuvant chemotherapy was started, and four cycles of 3 mg
vindesine + 1 g cyclophosphamide and three cycles of 60 mg
epirubicin were administered. Vindesine and cyclophosphamide were
administered on a 4-week cycle. Epirubicin was administered on a
3-week cycle. Vindesine was administered on days 1, 8, 15 and 22 of
the cycle. Cyclophosphamide was administered on days 1, 2, 3, 4 and
5 of the cycle. Epirubicin was administered on day 1 of the cycle.
During this period, the leukocyte-raising therapy was performed
against leukopenia due to chemotherapy-induced myeloid inhibition.
The patient was eventually discharged 1 month later after the
symptoms resolved and is currently doing well. The case is being
followed up every 2 months.
Discussion
RMS is a malignant mesenchymal tumor that accounts
for <1% of all mesenchymal tumors in the gastrointestinal system
(8). RMS of the stomach is
extremely rare, with only four previously published cases (4–7). RMSs
in the stomach are primary tumors, and no cases of metastasis in
the stomach have been documented (3). Patients typically present with no
symptoms in the early stages, followed by appetite loss and
abdominal pain, or with non-specific pressure symptoms in the late
stages when the tumor is large. The present case was similar to the
cases documented in the literature. The signs of RMS are atypical
on CT and magnetic resonance imaging (MRI), which makes the imaging
diagnosis difficult and the condition easy to misdiagnose
clinically. However, CT and MRI are critical in the preoperative
diagnosis (the current patient did not consent to an MRI
examination), as they can reveal the location of the lesion and
they show the relationship between the tumor and the surrounding
tissues, and the degree of invasion of the surrounding tissues.
Finally, these techniques indicate the recurrence and metastasis
risks after surgery (9). Therefore,
it is important to raise awareness of the need for imaging for this
disease.
According to the present case, the following types
of gastric tumors need to be differentiated during the diagnosis of
primary gastric ARMS: i) Neuroendocrine neoplasms, which often
occur among the elderly, with multiple low-density small nodules
(<2 cm) under the gastric mucosa, but with a density that is
higher than that of muscle enhancement. The extent of uniform
moderate enhancement in the arterial phase is higher than that of
the gastric mucosa. Clinical manifestations include increased
gastrin secretion and increased PH level. The primary pathological
diagnosis of a neuroendocrine tumor, in this case, may be
attributed to small round cells and immunohistochemical CD56
expression positivity. Gastrointestinal neuroendocrine tumors are
more common than RMS and are easily misdiagnosed as neuroendocrine
tumors. This case is that of a young patient with uneven mild and
moderate enhancement on a CT enhancement scan, which can be used as
a differential point. ii) Gastric stromal tumors, the most common
benign tumors in the gastrointestinal tract, are often found in the
upper part of the gastric fundus (7). The boundary is distinct with uniform
density. Calcification is a common occurrence. In ARMS, there are
few ulcers, but the boundary is unclear and the density is uneven.
Calcification rarely occurs (10).
Therefore, the two tumors can easily be distinguished. (iii)
Gastric carcinoma often occurs among the elderly, with stiff
gastric mucosa and blurred fat space around the stomach; its
clinical manifestations include anemia and cachexia. ARMS often
occurs in adolescents with good continuity of the gastric mucosa
and no cachexia clinically. These two diseases can easily be
distinguished.
In summary, although RMS is extremely rare in the
adult stomach, the outcome of a young beneficiary with abdominal
occupancy combined with lymph node growth should be considered a
possibility, and should not be diagnosed as benign without
assessment. The occurrence of distant lymph node metastasis in the
present patient 1 month after surgery is consistent with the
literature, which states that adult RMS is highly malignant, prone
to recurrence and metastasis, and has a worse prognosis than RMS in
children (11–13). Pathology is required to confirm the
final diagnosis.
In conclusion, the current study presents a rare
case of primary ARMS in the stomach. Efforts to increase awareness
of the disease should be increased to improve the early clinical
diagnosis and treatment.
Acknowledgements
The authors would like to thank Miss Shixing Zhao
from the Department of Pathology, Handan Central Hospital (Handan,
China) for performing the histopathological analysis.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
SY and XZ were responsible for study conception and
design. XZ and ZY performed the collection and assembly of data,
including obtaining the laboratory results and medical images. SY
and XZ analyzed and interpreted the data. All authors wrote the
manuscript. SY, ZY and XZ confirm the authenticity of all the raw
data. All authors have read and approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained from the
patient.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
CT
|
computed tomography
|
|
RMS
|
rhabdomyosarcoma
|
|
MRI
|
magnetic resonance imaging
|
References
|
1
|
Gong QX and Fan QH: Updates of the 2020
WHO classification of the soft tissue tumors: part I. Zhonghua Bing
Li Xue Za Zhi. 50:180–184. 2021.(In Chinese). PubMed/NCBI
|
|
2
|
Gong QX and Fan QH: Updates of the 2020
WHO classification of soft tissue tumors: part II. Zhonghua Bing Li
Xue Za Zhi. 50:314–318. 2021.(In Chinese). PubMed/NCBI
|
|
3
|
Fujiie M, Yamamoto M, Taguchi K, Iwanaga
A, Ohgaki K, Egashira A, Minami K, Toh Y, Oda Y and Okamura T:
Gastric carcinosarcoma with rhabdomyosarcomatous differentiation: A
case report and review. Surg Case Rep. 2:522016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Wang Y, Guo P, Zhang Z, Jiang RD and Li Z:
Primary epithelioid rhabdomyosarcoma of the stomach: A case report
and review of literature. Diagn Pathol. 14:1372019. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Shah LK, Mony NJ, Mishra S and Pant B: An
exceptionally rare primary epithelioid rhabdomyosarcomas of the
stomach: A case report. Cureus. 14:e260462022.PubMed/NCBI
|
|
6
|
Palermo M, Mastronardi LM, García RH,
Solari I and Tarsitano FJ: Primary gastric rhabdomyosarcoma. Case
report. Acta Gastroenterol Latinoam. 42:131–134. 2012.PubMed/NCBI
|
|
7
|
Gandhi JS, Pasricha S, Gupta G, Mahanta A,
Mehta A, Doudagoudar C, Goswami V and Doval DC: Synchronous
embryonal rhabdomyosarcoma (NOS) of the Mid-oesophagus and stomach.
J Gastrointest Cancer. 43 (Suppl 1):S217–S220. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Mance M, Smuđ-Orehovec S,
Vrbanović-Mijatović V and Mijatović D: Primary Alveolar
rhabdomyosarcoma of the breast in a 17-year-old girl. JCO Oncol
Pract. 16:93–95. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Latack JT, Hutchinson RJ and Heyn RM:
Imaging of rhabdomyosarcomas of the head and neck. Am J
Neuroradiol. 8:353–359. 1987.PubMed/NCBI
|
|
10
|
Tang W, Ren G, Cai R, He WG, Ni J and Chen
J: Primary rhabdomyosarcoma in adults: Clinicopathological
characteristics, CT and MRI findings. J Diagnostics Concepts
Practice. 16:301–305. 2017.
|
|
11
|
Heske CM and Mascarenhas L: Relapsed
Rhabdomyosarcoma. J Clin Med. 10:8042021. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ferrari A, Dileo P, Casanova M, Bertulli
R, Meazza C, Gandola L, Navarria P, Collini P, Gronchi A, Olmi P,
et al: Rhabdomyosarcoma in adults. A retrospective analysis of 171
patients treated at a single institution. Cancer. 98:571–580. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Mäkinen VN, Safwat A and
Aggerholm-Pedersen N: Rhabdomyosarcoma in adults: A retrospective
analysis of case records diagnosed between 1979 and 2018 in Western
Denmark. Sarcoma. 2021:99488852021. View Article : Google Scholar : PubMed/NCBI
|