Introduction
Globally, more than 50% of the esophageal cancer
cases in occur in China (1).
Squamous cell carcinoma (SCC) is a major subtype of esophageal
carcinoma in China, Japan, and other East Asian countries (2). According to a study in 2021, the
5-year overall survival (OS) rate of patients with esophageal
cancer after esophagectomy was 59.3% in Japan (3). In Japan, Europe, and America,
esophageal cancer is treated in much the same method as in China.
In addition to differences in tumor characteristics across these
countries and regions, the largest difference is the extent of
lymph node (LN) dissection. Professor Akiyama's study showed that
three-field lymphadenectomy increased 5-year OS in patients with
esophageal cancer compared to systematic thoracoabdominal two-field
lymphadenectomy (55.0% vs. 38.3%) (4). Thus, LN metastasis is an important
factor affecting OS in esophageal cancer; this has been confirmed
in an increasing number of studies (5–9).
According to the literature, at least 15 LNs should be removed
during esophageal cancer surgery. Similar findings have been
confirmed by the National Comprehensive Cancer Network. However,
studies encouraging the removal of more than 15 LNs are still
controversial (10–12). A series of studies carried out by
Professor Liu, involving two-field and three-field lymphadenectomy,
has sparked widespread discussion among Chinese surgeons (13,14).
While a large number of studies have indicated that LN dissection
can reduce the likelihood of recurrence and increase OS, some have
also shown that extensive LN dissection incurs greater surgical
trauma and increases the incidence and mortality of postoperative
complications (15).
The appropriate extent of LN removal necessary to
limit surgical trauma and postoperative complications remains a
problem that must be resolved. In February 2021, a Chinese
single-center randomized controlled study showed that three-field
LN dissection could allow more precise staging of middle and lower
thoracic SCC than two-field LN dissection, but there was no
improvement in OS and disease-free survival (DFS) (16). However, the choice of procedure is
usually individualized based on the case and patient preferences.
For patients without suspicious tumor-positive cervical LNs,
two-field systematic LN dissection for esophageal SCC (ESCC) is
sufficient, while for patients with suspicious tumor-positive
cervical LNs, three-field systematic LN dissection for ESCC is
necessary. In both cases, the number of LNs resected during surgery
should be adjusted. To this end, this study was designed to
elucidate the impact of the number of resected LNs (RLNs) on the OS
of patients with middle and lower thoracic ESCC.
Materials and methods
Data were obtained from the Sichuan Cancer Hospital
& Institute Esophageal Cancer Case Management Database. We
retrospectively evaluated middle and lower thoracic esophageal
cancer patients who underwent esophagectomy from January 2010 to
April 2020. Patient records were reviewed for clinicopathologic
findings and outcomes. Approximate esophagectomy was performed
through a right transthoracic procedure with two-field or
three-field lymphadenectomy. Surgical approaches depended on
patient characteristics and surgeon preferences; for example,
patients with enlargement of specific cervical LN groups underwent
three-field lymphadenectomy. Disease stage was presented according
to the American Joint Committee on Cancer 8th edition
tumor-node-metastasis (TNM) system. There were three inclusion
criteria: (1) patients who
underwent esophagectomy, (2) tumor
located in the thoracic esophagus, and (3) tumor with pathological evidence of SCC.
The following exclusion criteria were also considered: (1) less than 15 RLNs, (2) presence of other malignant tumors,
(3) pathological T
stage=Tis/Ia/IVb, and (4) absence
of any required data.
Patients were followed up once every 3 months for
the first 2 years and once every 6 months for the next 3–5 years.
OS was estimated from the month and year of surgery to death or
last follow-up in April 2022. The study was approved by the Ethics
Committee for Medical Research and New Medical Technology of
Sichuan Cancer Hospital (SCCHEC-02-2022-050). All patients were
fully informed before providing verbal consent as per approved
ethics protocol.
Patients were grouped depending on the presence or
absence of suspicious tumor-positive cervical LNs. The reference
standard was LN short diameter ≥1 cm observed on contrast-enhanced
computed tomography (17,18). Patients were divided into two groups
based on the presence of suspicious tumor-positive cervical LNs. In
cases without suspicious tumor-positive cervical LNs, two-field
systematic LN dissection for ESCC was performed and patients were
categorized into the ‘2F group’. For patients with suspicious
tumor-positive cervical LNs, three-field systematic LN dissection
for ESCC was performed and the patients were categorized into the
‘3F group’.
According to the quartile number of RLNs, four
subgroups from both groups were designed for analysis depending on
the extent of lymphadenectomy. In the 2F group, patients with
15–18, 19–22, 23–29, and more than 30 RLNs were divided into the ‘A
group’, ‘B group’, ‘C group’, and ‘D group’, respectively. In the
3F group, patients with 17–30, 31–37, 38–50, and more than 51 RLNs
were divided into the ‘A group’, ‘B group’, ‘C group’, and ‘D
group’, respectively.
Statistical analysis
Categorical variables are reported as percentages.
They were investigated using the chi-square or Fisher's exact test.
Univariate and multivariate logistic regression analyses were used
to calculate the independent risk factors associated with LN
metastasis, and the hazard ratio and 95% confidence interval (CI)
are used to describe each variable. The Cox proportional hazards
regression model was used to evaluate the impact of all baseline
covariates on the outcome. A graphical representation of the model
was developed using GraphPad Prism (GraphPad Software, Boston, MA,
USA). OS was evaluated by plotting Kaplan-Meier curves, compared
using the log-rank test, and described as the median rate and value
at specific time points with 95% CIs. Statistical significance was
defined as a P-value less than 0.05. All analyses were conducted
using SPSS version 23.0 software (SPSS Inc., Chicago, IL, USA).
Results
A total of 1659 patients were included in the
analysis. A flowchart describing the study enrollment is shown in
Fig. 1. The clinicopathological and
pathological characteristics of the 2F and 3F groups are shown in
Tables I and II. Two-field systematic LN dissection was
performed in 1562 of 1659 patients (94.2%) and categorized as the
2F group; 97 of 1659 patients (5.8%) underwent three-field
systematic lymphadenectomy and were categorized as the 3F group.
Additionally, postoperative pathological examination showed that 20
of the 97 patients (20.6%) in the 3F group had tumor-positive
cervical LNs.
 | Table I.Baseline demographic and patient
characteristics of the 2F (n=1,562) group. |
Table I.
Baseline demographic and patient
characteristics of the 2F (n=1,562) group.
| Variables | Group A (n=393) | Group B (n=373) | Group C (n=421) | Group D (n=375) |
|---|
| Sex |
|
|
|
|
| Male | 337 (85.8%) | 317 (85.0%) | 375 (89.1%) | 343 (91.5%) |
|
Female | 56 (14.2%) | 56 (15.0%) | 46 (10.9%) | 32 (8.5%) |
| Age, years |
|
|
|
|
| Median
(range) | 62 (39–84) | 63 (36–81) | 62 (37–85) | 62 (39–84) |
|
<75 | 365 (92.9%) | 355 (95.2%) | 403 (95.7%) | 359 (95.7%) |
|
≥75 | 28 (7.1%) | 18 (4.8%) | 18 (4.3%) | 16 (4.3%) |
| Pathological
differentiation grade |
|
|
|
|
|
Moderate or Well G1-2 | 240 (61.1%) | 241 (64.6%) | 267 (63.4%) | 248 (66.1%) |
| Poor or
undifferentiated G3 | 153 (38.9%) | 132 (35.4%) | 154 (36.6%) | 127 (33.9%) |
| Tumor location |
|
|
|
|
|
Middle | 269 (68.4%) | 258 (69.2%) | 287 (68.2%) | 240 (64.0%) |
|
Lower | 124 (31.6%) | 115 (30.8%) | 134 (31.8%) | 135 (36.0%) |
| Pathological T
stage |
|
|
|
|
|
T1b | 45 (11.5%) | 42 (11.3%) | 39 (9.3%) | 32 (8.5%) |
| T2 | 120 (30.5%) | 103 (27.6%) | 116 (27.6%) | 94 (25.1%) |
| T3 | 207 (52.7%) | 198 (53.1%) | 238 (56.5%) | 218 (58.1%) |
| T4 | 21 (5.3%) | 30 (8.0%) | 28 (6.7%) | 31 (8.3%) |
| N stage |
|
|
|
|
| N0 | 180 (45.8%) | 170 (45.6%) | 140 (33.2%) | 138 (36.8%) |
| N1 | 124 (31.5%) | 104 (27.9%) | 138 (32.8%) | 106 (28.3%) |
| N2 | 69 (17.6%) | 64 (17.1%) | 95 (22.6%) | 71 (18.9%) |
| N3 | 20 (5.1%) | 35 (9.4%) | 48 (11.4%) | 60 (16.0%) |
| 8th TNM Stage |
|
|
|
|
| I | 36 (9.2%) | 39 (10.5%) | 28 (6.7%) | 12 (3.2%) |
| II | 145 (36.9%) | 128 (34.3%) | 113 (26.8%) | 125 (33.3%) |
|
III | 186 (47.3%) | 167 (44.7%) | 224 (53.2%) | 170 (45.4%) |
| IV | 26 (6.6%) | 39 (10.5%) | 56 (13.3%) | 68 (18.1%) |
| Radical resection
rate |
|
|
|
|
| R0 | 387 (98.5%) | 358 (96.0%) | 413 (98.1%) | 365 (97.3%) |
|
R1/2 | 6 (1.5%) | 15 (4.0%) | 8 (1.9%) | 10 (2.7%) |
| Thoracic
surgery |
|
|
|
|
|
MIE | 226 (57.5%) | 207 (55.5%) | 224 (53.2%) | 179 (47.7%) |
| OE | 167 (42.5%) | 166 (44.5%) | 197 (46.8%) | 196 (52.3%) |
| Abdominal
surgery |
|
|
|
|
|
MIE | 194 (49.4%) | 178 (47.7%) | 210 (49.9%) | 160 (42.7%) |
| OE | 199 (50.6%) | 195 (52.3%) | 211 (50.1%) | 215 (57.3%) |
 | Table II.Baseline demographic and patient
characteristics of the 3F (n=97) group. |
Table II.
Baseline demographic and patient
characteristics of the 3F (n=97) group.
| Variables | Group A (n=24) | Group B (n=25) | Group C (n=24) | Group D (n=24) |
|---|
| Sex |
|
|
|
|
|
Male | 18 (75.0%) | 18 (72.0%) | 20 (83.3%) | 23 (95.8%) |
|
Female | 6 (25.0%) | 7 (28.0%) | 4 (16.7%) | 1 (4.2%) |
| Age (years) |
|
|
|
|
| Median
(range) | 61 (44–71) | 61 (39–70) | 61.5 (46–67) | 61 (40–75) |
|
<75 | 24 (100%) | 25 (100%) | 24 (100%) | 22 (91.7%) |
|
≥75 | 0 (0%) | 0 (0%) | 0 (0%) | 2 (8.3%) |
| Pathological
differentiation grade |
|
|
|
|
|
Moderate or Well G1-2 | 12 (50.0%) | 18 (72.0%) | 16 (66.7%) | 13 (54.2%) |
| Poor or
undifferentiated G3 | 12 (50.0%) | 7 (28.0%) | 8 (33.3%) | 11 (45.8%) |
| Tumor location |
|
|
|
|
|
Middle | 18 (75.0%) | 21 (84.0%) | 19 (79.2%) | 17 (70.8%) |
|
Lower | 6 (25.0%) | 4 (16.0%) | 5 (20.8%) | 7 (29.2%) |
| Pathological T
stage |
|
|
|
|
|
T1b | 3 (12.5%) | 2 (8.0%) | 1 (4.2%) | 0 (0%) |
| T2 | 9 (37.5%) | 8 (32.0%) | 9 (37.5%) | 6 (25.0%) |
| T3 | 12 (50.0%) | 15 (60.0%) | 12 (50.0%) | 16 (66.7%) |
| T4 | 0 (0%) | 0 (0%) | 2 (8.3%) | 2 (8.3%) |
| N stage |
|
|
|
|
| N0 | 8 (33.3%) | 8 (32.0%) | 7 (29.2%) | 7 (29.2%) |
| N1 | 7 (29.2%) | 10 (40.0%) | 6 (25.0%) | 9 (37.5%) |
| N2 | 8 (33.3%) | 4 (16.0%) | 6 (25.0%) | 4 (16.7%) |
| N3 | 1 (4.2%) | 3 (12.0%) | 5 (20.8%) | 4 (16.7%) |
| 8th TNM Stage |
|
|
|
|
| I | 2 (8.3%) | 2 (8.0%) | 2 (8.3%) | 0 (0%) |
| II | 5 (20.8%) | 6 (24.0%) | 5 (20.8%) | 6 (25.0%) |
|
III | 16 (66.7%) | 13 (52.0%) | 10 (41.7%) | 13 (54.2%) |
| IV | 1 (4.2%) | 4 (16.0%) | 7 (29.2%) | 5 (20.8%) |
| Radical resection
rate |
|
|
|
|
| R0 | 24 (100.0%) | 25 (100.0%) | 24 (100.0%) | 24 (100.0%) |
| Thoracic
surgery |
|
|
|
|
|
MIE | 20 (83.3%) | 18 (72.0%) | 19 (79.2%) | 15 (62.5%) |
| OE | 4 (16.7%) | 7 (28.0%) | 5 (20.8%) | 9 (37.5%) |
| Abdominal
surgery |
|
|
|
|
|
MIE | 20 (83.3%) | 17 (68.0%) | 19 (79.2%) | 15 (62.5%) |
| OE | 4 (16.7%) | 8 (32.0%) | 5 (20.8%) | 9 (37.5%) |
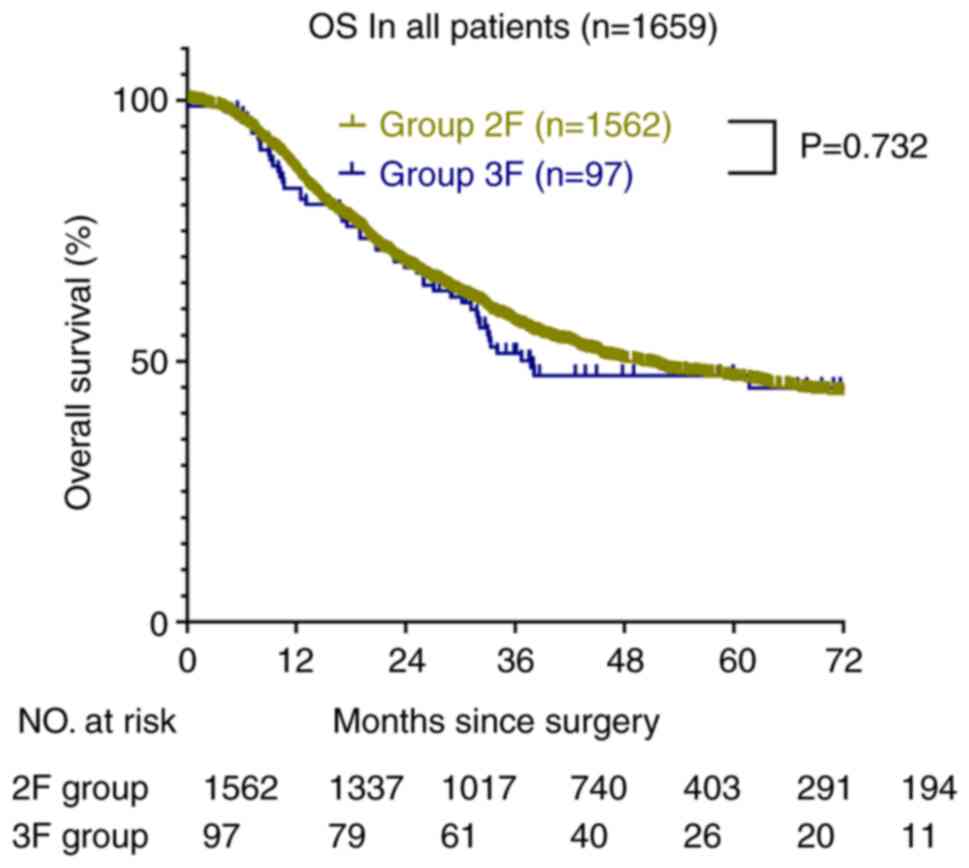
After 50.7 months (95% CI, 47.2-54.1) of median
follow-up, 1659 patients who underwent esophagectomy were enrolled.
The median OS of the 2F group was 50.0 months (95% CI, 46.6-53.5)
and that of the 3F group was 58.5 months (95% CI, 45.5-71.5). The
OS rates at 1, 3, and 5 years were 86, 57, and 47%, respectively,
in the 2F group (Fig. 2). In the 3F
group, the OS rates at 1, 3, and 5 years were 83, 52, and 47%,
respectively (P=0.732). However, the 3F B group did not reach the
median OS time, and the average OS of the 3F B and 3F D groups was
57.7 months (95% CI, 47.3-68.0) and 30.2 months (95% CI,
22.5-37.9), respectively. The OS rates at 1, 3, and 5 years were
92, 71, and 65%, respectively, in the 3F B group. In the 3F D
group, the OS rates at 1, 3, and 5 years were 79, 28, and 28%,
respectively (hazard ratio, 3.095; 95% CI, 1.318-7.273;
P=0.01). In the 2F subgroups, the OS was not significantly
different between the A, B, C, and D groups (Fig. 3).
Kaplan-Meier curves showed that the OS of the four
subgroups of the 2F group were all similar. However, the OS in the
four subgroups of the 3F group were all significantly different,
particularly between groups B and D (P<0.05). This result
suggested that the best strategy for lymphadenectomy in patients
with enlarged specific cervical LNs was the resection of 31 to 37
LNs. Therefore, we compared the clinical and pathological
characteristics of the patients. However, there were no significant
differences between the 3F B and D groups, as shown in Table III.
 | Table III.Summary of pathological
characteristics compared between the 2F/3F and 3F B/D
subgroups. |
Table III.
Summary of pathological
characteristics compared between the 2F/3F and 3F B/D
subgroups.
|
| Total esophageal
cancer (n=1659) | Esophageal cancer
3F (n=97) |
|---|
|
|
|
|
|---|
| Variables | 2F Group
(n=1562) | 3F Group
(n=97) | P-value | Group B (n=25) | Group D (n=24) | P-value |
|---|
| Sex |
|
| 0.065 |
|
| 0.024 |
|
Male | 1372 (87.8%) | 79 (81.4%) |
| 18 (72.0%) | 23 (95.8%) |
|
|
Female | 190 (12.2%) | 7 (18.6%) |
| 7 (28.0%) | 1 (4.2%) |
|
| Age (years) |
|
| 0.177 |
|
| 0.141 |
|
<75 | 1482 (94.9%) | 95 (97.9%) |
| 25 (100%) | 22 (91.7%) |
|
|
≥75 | 80 (5.1%) | 2 (2.1%) |
| 0 (0%) | 2 (8.3%) |
|
| Pathological
differentiation grade |
|
| 0.559 |
|
| 0.196 |
|
Moderate or Well G1-2 | 996 (63.8%) | 59 (60.8%) |
| 18 (72.0%) | 13 (54.2%) |
|
| Poor or
undifferentiated G3 | 566 (36.2%) | 38 (39.2%) |
| 7 (28.0%) | 11 (45.8%) |
|
| Tumor location |
|
| 0.044 |
|
| 0.269 |
|
Middle | 1054 (67.5%) | 75 (77.3%) |
| 21 (84.0%) | 17 (70.8%) |
|
|
Lower | 508 (32.5%) | 22 (22.7%) |
| 4 (16.0%) | 7 (29.2%) |
|
| Pathological T
stage |
|
| 0.32 |
|
| 0.231 |
|
T1b | 158 (10.1%) | 6 (6.2%) |
| 2 (8.0%) | 0 (0%) |
|
| T2 | 433 (27.7%) | 32 (33.0%) |
| 8 (32.0%) | 6 (25.0%) |
|
| T3 | 861 (55.1%) | 55 (56.7%) |
| 15 (60.0%) | 16 (66.7%) |
|
| T4 | 110 (7.1%) | 30 (30.9%) |
| 0 (0%) | 2 (8.3%) |
|
| N stage |
|
| 0.313 |
|
| 0.971 |
| N0 | 628 (40.2%) | 30 (30.9%) |
| 8 (32.0%) | 7 (29.2%) |
|
| N1 | 472 (30.2%) | 32 (33.0%) |
| 10 (40.0%) | 9 (37.5%) |
|
| N2 | 299 (19.1%) | 22 (22.7%) |
| 4 (16.0%) | 4 (16.7%) |
|
| N3 | 163 (10.4%) | 13 (13.4%) |
| 3 (12.0%) | 4 (16.7%) |
|
| 8th TNM Stage |
|
| 0.12 |
|
| 0.554 |
| I | 115 (7.4%) | 6 (6.2%) |
| 2 (8.0%) | 0 (0%) |
|
| II | 511 (32.7%) | 22 (22.7%) |
| 6 (24.0%) | 6 (25.0%) |
|
|
III | 747 (47.8%) | 52 (53.6%) |
| 13 (52.0%) | 13 (54.2%) |
|
| IV | 189 (12.1%) | 17 (17.5%) |
| 4 (16.0%) | 5 (20.8%) |
|
| Radical resection
rate |
|
| 0.115 |
|
|
|
| R0 | 1523 (97.5%) | 97 (100.0%) |
| 25 (100.0%) | 24 (100.0%) |
|
|
R1/2 | 39 (2.5%) | 0 |
| 0 | 0 |
|
| Thoracic
surgery |
|
| <0.001 |
|
| 0.478 |
|
MIE | 1523 (97.5%) | 72 (74.2%) |
| 18 (72.0%) | 15 (62.5%) |
|
| OE | 39 (2.5%) | 25 (25.8%) |
| 7 (28.0%) | 9 (37.5%) |
|
| Abdominal
surgery |
|
| <0.001 |
|
| 0.686 |
|
MIE | 742 (47.5%) | 71 (73.2%) |
| 17 (68.0%) | 15 (62.5%) |
|
| OE | 820 (52.5%) | 26 (26.8%) |
| 8 (32.0%) | 9 (37.5%) |
|
Univariate analysis of patients without suspicious
tumor-positive cervical LNs indicated that sex (P=0.001), age
(P=0.045), tumor grade G3 (P<0.001), pathological T1b/T2/T3/T4
stage, pathological N0/N1/N2/N3 stage, 8th TNM stage I/II/III/IV,
radical resection (P<0.001), thoracic surgery (P<0.001), and
abdominal surgery (P<0.001) significantly influenced the 5-year
OS after esophagectomy (Table IV).
Further analysis using multivariate methods indicated that sex
(P=0.008), age (P<0.001), tumor grade G3 (P=0.007), pathological
T1b/T3/T4 stage, N0/N2/N3 stage, and radical resection (P=0.026)
affected the 5-year OS after esophagectomy (Table IV).
 | Table IV.Univariate and multivariate Cox
regression analysis factors affecting survival in the 2F group. |
Table IV.
Univariate and multivariate Cox
regression analysis factors affecting survival in the 2F group.
|
| Univariate | Multivariate |
|---|
|
|
|
|
|---|
| Variables | HR | 95% CI | P-value | HR | 95% CI | P-value |
|---|
| Sex |
|
| 0.001 |
|
| 0.008 |
|
Male | 1.49 | 1.171-1.897 |
| 1.394 | 1.090-1.783 |
|
|
Female | 1 | 0 |
| 1 | 0 |
|
| Age (years), |
|
| 0.045 |
|
| <0.001 |
|
<75 | 1 | 0 |
| 1 | 0 |
|
|
≥75 | 1.371 | 1.008-1.865 |
| 2.006 | 1.465-2.747 |
|
| Pathological
differentiation grade |
|
| <0.001 |
|
| 0.007 |
|
Moderate or Well G1-2 | 1 | 0 |
| 1 | 0 |
|
| Poor or
undifferentiated G3 | 1.415 | 1.226-1.634 |
| 1.226 | 1.058-1.420 |
|
| Tumor location |
|
| 0.879 |
|
|
|
|
Middle | 1.012 | 0.869-1.178 |
|
|
|
|
|
Lower | 1 | 0 |
|
|
|
|
| Pathological T
stage |
|
|
|
|
|
|
|
T1b | 1 | 0 | <0.001 | 1 | 0 | <0.001 |
| T2 | 1.761 | 1.242-2.495 | 0.001 | 1.289 | 0.864-1.923 | 0.213 |
| T3 | 2.675 | 1.930-3.707 | <0.001 | 1.777 | 1.196-2.641 | 0.004 |
| T4 | 4.505 | 3.061-6.631 | <0.001 | 2.388 | 1.404-4.062 | 0.001 |
| N stage |
|
|
|
|
|
|
| N0 | 1 | 0 | <0.001 | 1 | 0 | <0.001 |
| N1 | 1.869 | 1.538-2.271 | <0.001 | 1.523 | 0.957-2.424 | 0.076 |
| N2 | 3.855 | 3.167-4.693 | <0.001 | 2.877 | 1.768-4.682 | <0.001 |
| N3 | 5.391 | 4.307-6.747 | <0.001 | 3.5 | 1.674-7.318 | 0.001 |
| 8th TNM Stage |
|
|
|
|
|
|
| I | 1 | 0 | <0.001 | 1 | 0 | 0.83 |
| II | 1.692 | 1.083-2.643 | <0.001 | 1.128 | 0.684-1.861 | 0.636 |
|
III | 4.033 | 2.627-6.193 | <0.001 | 1.383 | 0.672-2.844 | 0.379 |
| IV | 8.814 | 5.633-13.791 | <0.001 | 1.412 | 0.549-3.631 | 0.474 |
| Radical resection
rate |
|
| <0.001 |
|
| 0.026 |
| R0 | 1 | 0 |
| 1 | 0 |
|
|
R1/2 | 2.272 | 1.586-3.256 |
| 1.527 | 1.051-2.219 |
|
| Thoracic
surgery |
|
| <0.001 |
|
| 0.683 |
|
MIE | 1 | 0 |
| 1 | 0 |
|
| OE | 1.43 | 1.238-1.650 |
| 0.941 | 0.703-1.259 |
|
| Abdominal
surgery |
|
| <0.001 |
|
| 0.366 |
|
MIE | 1 | 0 |
| 1 | 0 |
|
| OE | 1.404 | 1.212-1.626 |
| 1.146 | 0.853-1.539 |
|
In the 3F group, univariate analysis indicated that
age (P=0.018), pathological N0/N2/N3 stage, and 8th TNM stage I
(P=0.006) significantly influenced the 5-year OS after
esophagectomy (Table V). Further
analysis using multivariate methods indicated that pathological N0
stage (P=0.003) significantly affected the 5-year OS after
esophagectomy (Table V).
 | Table V.Univariate and multivariate Cox
regression analysis of factors affecting survival among patients in
the 3F group. |
Table V.
Univariate and multivariate Cox
regression analysis of factors affecting survival among patients in
the 3F group.
|
| Univariate | Multivariate |
|---|
|
|
|
|
|---|
| Variables | HR | 95% CI | P-value | HR | 95% CI | P-value |
|---|
| Sex |
|
|
|
|
|
|
|
Male | 1.085 | 0.525-2.241 | 0.826 |
|
|
|
|
Female | 1 |
|
|
|
|
|
| Age (years) |
|
|
|
|
|
|
|
<75 | 1 |
|
|
|
|
|
|
≥75 | 5.744 | 1.353-24.384 | 0.018 | 3.68 | 0.800-16.939 | 0.094 |
| Pathological
differentiation grade |
|
|
|
|
|
|
|
Moderate or Well G1-2 | 1 |
|
|
|
|
|
| Poor or
undifferentiated G3 | 1.556 | 0.881-2.749 | 0.128 |
|
|
|
| Tumor location |
|
|
|
|
|
|
|
Middle | 1.573 | 0.831-2.979 | 0.164 |
|
|
|
|
Lower | 1 |
|
|
|
|
|
| Pathological T
stage |
|
| 0.457 |
|
|
|
|
T1b | 1 |
|
|
|
|
|
| T2 | 1.334 | 0.306-5.804 | 0.701 |
|
|
|
| T3 | 1.298 | 0.308-5.465 | 0.722 |
|
|
|
| T4 | 3.306 | 0.551-19.822 | 0.191 |
|
|
|
| N stage |
|
| <0.001 |
|
| 0.003 |
| N0 | 1 |
|
| 1 |
|
|
| N1 | 1.974 | 0.827-4.715 | 0.126 | 0.604 | 0.150-2.432 | 0.479 |
| N2 | 8.438 | 3.495-20.371 | <0.001 | 2.716 | 0.645-11.445 | 0.173 |
| N3 | 4.833 | 1.840-12.692 | 0.001 | 2.003 | 0.284-14.150 | 0.486 |
| 8th TNM Stage |
|
| 0.006 |
|
| 0.198 |
| I | 1 |
|
| 1 |
|
|
| II | 0.526 | 0.096-2.873 | 0.458 | 0.543 | 0.099-2.969 | 0.481 |
|
III | 2.694 | 0.642-11.302 | 0.176 | 2.82 | 0.421-18.879 | 0.285 |
| IV | 3.464 | 0.771-15.559 | 0.105 | 1.751 | 0.182-16.884 | 0.628 |
| Thoracic
surgery |
|
|
|
|
|
|
|
MIE | 1 |
|
|
|
|
|
| OE | 1.005 | 0.522-1.933 | 0.989 |
|
|
|
| Abdominal
surgery |
|
|
|
|
|
|
|
MIE | 1 |
|
|
|
|
|
| OE | 1.056 | 0.548-2.032 | 0.871 |
|
|
|
Discussion
This study clarified the influence of the number of
LNs resected during lymphadenectomy on long-term survival. Patients
who underwent two-field lymphadenectomy exhibited no improvement in
OS as the number of RLNs increased, but the OS of patients who
underwent three-field lymphadenectomy was significantly different
in the B and D groups. In addition, there were no statistically
significant differences in the characteristics of patients between
the B and D groups, except sex.
From the study findings, it can be seen that the
most reasonable number of RLNs is between 31 and 37; deviations
greater or less than this are both detrimental to the OS of
patients with suspicious tumor-positive cervical LNs. There was a
significant reduction in OS when the number of RLNs was greater
than 50. However, this was not observed in patients without
suspicious tumor-positive cervical LNs who underwent two-field
lymphadenectomy. Consistent with these results, research by the
Cleveland Clinic in Cleveland show that up to 25 to 30 RLNs can
improve the OS of patients (19),
while more than 30 RLNs reduce the OS. This suggests that surgical
strategies should be individualized to optimize OS in different
patients.
Few studies have been conducted on the extent of LN
dissection by grouping according to this scheme recently. Although
articles examining LN dissection have been published, the
conclusions are not comparable due to different strategies being
examined (20). As more studies
focus on comprehensive treatment options for esophageal cancer, the
debate now centers around how and when chemotherapy and radiation
should be administered, rather than the details of lymphadenectomy
(21–23).
In the Chemoradiotherapy for Oesophageal Cancer
followed by Surgery Study (CROSS), the median OS of the neoadjuvant
chemoradiotherapy plus surgery group was 48.6 months and the 5-year
OS rate was 47% whereas the median OS of the surgery alone group
was 24.0 months and the 5-year OS rate was 33% (16). In the CheckMate 577 study, the
median DFS of the neoadjuvant chemoradiotherapy plus surgery and
surgery alone groups was 22.4 months and 11.0 months, respectively,
and the 5-year OS rates were both lower than at our center
(22). However, histological
classification may be an important factor that influences survival,
along with strategies of lymphadenectomy. In the NEOCRTEC5010
Clinical Trial, the median OS was 66.5 months (21), which is better than the median OS
achieved at our center and may have been influenced by
lymphadenectomy (13,21–23).
According to research from Fudan University Shanghai Cancer Center,
the differences in OS and DFS were not significant between
three-field and two-field lymphadenectomy for middle and lower
thoracic esophageal cancer; a 5-year OS of 63% was observed in both
groups (23). In our study, the
5-year OS in the 2F group was 41%, and there were no significant
differences based on the number of RLNs. This may be due to various
differences in case characteristics such as pathological T/N
stage.
Theoretically, on the one hand, if the intensity of
lymphadenectomy is too low, the metastatic LNs would not be removed
and the risk of recurrence and metastasis would remain very high
(24). On the other hand, if the
intensity is too high, the lymphatic system may be damaged, which
is not conducive to immune function. Consequently, OS will not
improve significantly (25,26).
Therefore, it is crucial to find an appropriate
lymphadenectomy intensity in the treatment of esophageal cancer.
The Japan Esophageal Society guidelines state that three-field
systematic LN dissection is indispensable in the treatment of upper
thoracic ESCC. As for middle and lower thoracic ESCC, the condition
of the cervical LN needs to be checked carefully. The international
current consensus is that two-field systematic LN dissection is
enough to treat patients without suspicious tumor-positive cervical
LNs, whereas three-field systematic lymphadenectomy is required to
treat patients with suspicious tumor-positive cervical LNs
(27). Consequently, different
cases will require removal of the LN station in different zones as
well as different number of RLNs. Thus, the treatment of middle and
lower thoracic ESCC should involve lymphadenectomy of different
numbers and zones of RLNs based on whether tumor-positive cervical
LNs are present.
According to the Chinese Society of Clinical
Oncology guidelines for the diagnosis and treatment of malignant
LNs published in 2021, the number of RLNs during surgery should be
≥15 for ESCC, consistent with the 8th Union for International
Cancer Control edition standards (27,28).
However, variations by case, such as tumor location and LN
condition, and the uniform standard for ≥15 RLNs during
esophagectomy must be discussed further.
Some limitations in this study may have affected the
results. Esophagectomy was performed by 12 surgeons in our center
from January 2010 to April 2017. The main surgical types were
McKeown esophagectomy and Ivor-Lewis esophagectomy with two-field
lymphadenectomy or three-field lymphadenectomy, and there was
heterogeneity in lymph node dissection at each station. And there
was a difference in the rates of minimally invasive surgery between
the 2F group and the 3F group, but MIE showed no significant
statistical difference according to the multivariate analysis.
Thus, there may be subjective selection bias in the results.
Additionally, because we retrospectively analyzed data from a
single center, the representativeness of the results needs to be
considered. The clinical value and efficacy of different LN
stations were different, and the results may vary based on tumor
location (29). These aspects can
be examined further in future studies.
Based on a 5-year follow-up period in this study,
the OS of patients without tumor-positive cervical LNs does not
improve when more than 15 LNs are dissected. However, patients with
suspected tumor-positive cervical LNs should undergo three-field
lymphadenectomy and the number of RLNs should range from 31 to 37.
Therefore, optimal surgical strategies must be selected based on
the patient and case characteristics.
Acknowledgements
The authors would like to thank Professor Lihua Chen
(Division of Thoracic Surgery, Sichuan Cancer Research Center for
Cancer, Sichuan Cancer Hospital and Institute, Sichuan Cancer
Center, Affiliated Cancer Hospital of University of Electronic
Science and Technology of China, Chengdu, China) for their
instruction.
Funding
This work was supported by the Wu Jieping Medical Foundation
(grant no. 320.6750.2020-15-3, Bethune Charitable Foundation (grant
no. HZB-20190528-19), the Science and Technology Department of
Sichuan Province (grant nos. 2020YFH0169, 2021YJ0118, 23QYCX0261
and 23ZDYF2430) and Sichuan Province Clinical Key Specialty
Construction Project.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
KXL, KYD, KL, XN, CDL, WWH, KZL, CHW, ZYL, KZ, TQM,
LLJ, HJL, YM, QX, QF, YTH, XFL and LP contributed to the study
concept and design; acquisition, analysis, or interpretation of
data; and critical revision of the article for important
intellectual content. KXL drafted the article. KYD performed
statistical analysis. LP obtained funding. YTH and LP provided
administrative, technical, or material support and supervised the
study. KXL and KYD confirm the authenticity of all the raw data.
KXL and XFL had full access to all the data in the study and take
responsibility for the integrity of the data and the accuracy of
the data analysis. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
All procedures performed in this study involving
human participants were in accordance with the Declaration of
Helsinki (as revised in 2013). This study was approved by the
Ethical Committee of the Sichuan Cancer Hospital (approval no.
NCC2014ZC-01), and informed consent was obtained from all
participants.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
CI
|
confidence interval
|
|
DFS
|
disease-free survival
|
|
ESCC
|
esophageal squamous cell carcinoma
|
|
LN
|
lymph node
|
|
OS
|
overall survival
|
|
RLN
|
resected lymph node
|
|
SCC
|
squamous cell carcinoma
|
|
TNM
|
tumor-node-metastasis
|
|
2F group
|
patients who underwent two-field
systematic lymph node dissection
|
|
3F group
|
patients who underwent three-field
systematic lymph node dissection
|
References
|
1
|
Sung H, Ferlay J, Siegel RL, Laversanne M,
Soerjomataram I, Jemal A and Bray F: Global cancer statistics 2020:
GLOBOCAN estimates of incidence and mortality worldwide for 36
cancers in 185 countries. CA Cancer J Clin. 71:209–249. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Liang H, Fan JH and Qiao YL: Epidemiology,
etiology, and prevention of esophageal squamous cell carcinoma in
China. Cancer Biol Med. 14:33–41. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Watanabe M, Tachimori Y, Oyama T, Toh Y,
Matsubara H, Ueno M, Kono K, Uno T, Ishihara R, Muro K, et al:
Comprehensive registry of esophageal cancer in Japan, 2013.
Esophagus. 18:1–24. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Akiyama H, Tsurumaru M, Udagawa H and
Kajiyama Y: Radical lymph node dissection for cancer of the
thoracic esophagus. Ann Surg. 220:364–373. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Altorki N, Kent M, Ferrara C and Port J:
Three-field lymph node dissection for squamous cell and
adenocarcinoma of the esophagus. Ann Surg. 236:177–183. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Koenig AM, Prenzel KL, Bogoevski D,
Yekebas EF, Bubenheim M, Faithova L, Vashist YK, Gawad KA, Baldus
SE, Pantel K, et al: Strong impact of micrometastatic tumor cell
load in patients with esophageal carcinoma. Ann Surg Oncol.
16:454–462. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Okholm C, Svendsen LB and Achiam MP:
Status and prognosis of lymph node metastasis in patients with
cardia cancer-a systematic review. Surg Oncol. 23:140–146. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Stein HJ, Feith M, Bruecher BL, Naehrig J,
Sarbia M and Siewert JR: Early esophageal cancer: Pattern of
lymphatic spread and prognostic factors for long-term survival
after surgical resection. Ann Surg. 242:566–575. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Zhang M, Li Z, Ma Y, Zhu G, Zhang H and
Xue Y: Prognostic predictors of patients with carcinoma of the
gastric cardia. Hepatogastroenterology. 59:930–933. 2012.PubMed/NCBI
|
|
10
|
Xia W, Liu S, Mao Q, Chen B, Ma W, Dong G,
Xu L and Jiang F: Effect of lymph node examined count on accurate
staging and survival of resected esophageal cancer. Thorac Cancer.
10:1149–1157. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wang Y, Zhang X, Zhang X, Liu-Helmersson
J, Zhang L, Xiao W, Jiang Y, Liu K and Sang S: Prognostic value of
the extent of lymphadenectomy for esophageal cancer-specific
survival among T1 patients. BMC Cancer. 21:4032021. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Rizk NP, Ishwaran H, Rice TW, Chen LQ,
Schipper PH, Kesler KA, Law S, Lerut TE, Reed CE, Salo JA, et al:
Optimum lymphadenectomy for esophageal cancer. Ann Surg. 251:46–50.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Liu S, Wang Z and Wang F: Optimal
lymphadenectomy for thoracic esophageal cancer: Three-field or
modified two-field lymphadenectomy. Zhonghua Wei Chang Wai Ke Za
Zhi. 19:975–978. 2016.(In Chinese). PubMed/NCBI
|
|
14
|
Zheng Y, Wang Z, Wang F, Huang Q and Liu
S: Proposed modifications of supraclavicular lymph node metastasis
in the esophageal squamous cell carcinoma staging system for
improved survival stratification. Oncotarget. 8:41563–41571. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Hu Y, Hu C, Zhang H, Ping Y and Chen LQ:
How does the number of resected lymph nodes influence TNM staging
and prognosis for esophageal carcinoma? Ann Surg Oncol. 17:784–790.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Shapiro J, van Lanschot JJB, Hulshof MCCM,
van Hagen P, van Berge Henegouwen MI, Wijnhoven BPL, van Laarhoven
HWM, Nieuwenhuijzen GAP, Hospers GAP, Bonenkamp JJ, et al:
Neoadjuvant chemoradiotherapy plus surgery versus surgery alone for
oesophageal or junctional cancer (CROSS): Long-term results of a
randomised controlled trial. Lancet Oncol. 16:1090–1098. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Choi J, Kim SG, Kim JS, Jung HC and Song
IS: Comparison of endoscopic ultrasonography (EUS), positron
emission tomography (PET), and computed tomography (CT) in the
preoperative locoregional staging of resectable esophageal cancer.
Surg Endosc. 24:1380–1386. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Onbaş O, Eroglu A, Kantarci M, Polat P,
Alper F, Karaoglanoglu N and Okur A: Preoperative staging of
esophageal carcinoma with multidetector CT and virtual endoscopy.
Eur J Radiol. 57:90–95. 2006. View Article : Google Scholar
|
|
19
|
Raja S, Rice TW, Murthy SC, Ahmad U,
Semple ME, Blackstone EH and Ishwaran H; Worldwide Esophageal
Cancer Collaboration Investigators, : Value of lymphadenectomy in
patients receiving neoadjuvant therapy for esophageal
adenocarcinoma. Ann Surg. 274:e320–e327. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Zheng YZ, Li XQ, Wang JY, Yang H, Wen J,
Zhai WY, Yuan LX, Fu SS, Liao HY and Fu JH: Impact of examined
lymph node count for esophageal squamous cell carcinoma in patients
who underwent right transthoracic esophagectomy. Ann Surg Oncol.
28:3025–3033. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Yang H, Liu H, Chen Y, Zhu C, Fang W, Yu
Z, Mao W, Xiang J, Han Y, Chen Z, et al: Neoadjuvant
chemoradiotherapy followed by surgery versus surgery alone for
locally advanced squamous cell carcinoma of the esophagus
(NEOCRTEC5010): A phase III multicenter, randomized, open-label
clinical trial. J Clin Oncol. 36:2796–2803. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Kelly RJ, Ajani JA, Kuzdzal J, Zander T,
Van Cutsem E, Piessen G, Mendez G, Feliciano J, Motoyama S, Lièvre
A, et al: Adjuvant nivolumab in resected esophageal or
gastroesophageal junction cancer. N Engl J Med. 384:1191–1203.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Li B, Zhang Y, Miao L, Ma L, Luo X, Zhang
Y, Ye T, Li H, Zhang J, Li Y, et al: Esophagectomy with three-field
versus two-field lymphadenectomy for middle and lower thoracic
esophageal cancer: Long-term outcomes of a randomized clinical
trial. J Thorac Oncol. 16:310–317. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Yu L, Zhang XT, Guan SH, Cheng YF and Li
LX: The number of negative lymph nodes is positively associated
with survival in esophageal squamous cell carcinoma patients in
China. Open Med (wars). 15:152–159. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Guo X, Wang Z, Yang H, Mao T, Chen Y, Zhu
C, Yu Z, Han Y, Mao W, Xiang J, et al: Impact of lymph node
dissection on survival after neoadjuvant chemoradiotherapy for
locally advanced esophageal squamous cell carcinoma: From the
results of NEOCRTEC5010, a randomized multicenter study. Ann Surg.
227:259–266. 2023. View Article : Google Scholar
|
|
26
|
Chao YK, Liu HP, Hsieh MJ, Wu YC, Liu YH,
Yeh CH, Chang HK and Tseng CK: Lymph node dissection after
chemoradiation in esophageal cancer: A subgroup analysis of
patients with and without pathological response. Ann Surg Oncol.
19:3500–3505. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Chinese society of clinical oncology
(CSCO), . Guidelines of the Chinese Society of Clinical Oncology
(CSCO) Esophageal Cancer. 2022.(In Chinese).
|
|
28
|
Amin MB, Edge SB, Greene FL, Byrd DR,
Brookland RK, Washington MK, Gershenwald JE, Compton CC, Hess KR,
Sullivan DC, et al: AJCC cancer staging manual. 8th edition.
Springer; New York: 2017, View Article : Google Scholar
|
|
29
|
Tachimori Y, Ozawa S, Numasaki H,
Matsubara H, Shinoda M, Toh Y, Udagawa H, Fujishiro M, Oyama T and
Uno T; Registration Committee for Esophageal Cancer of the Japan
Esophageal Society, : Efficacy of lymph node dissection by node
zones according to tumor location for esophageal squamous cell
carcinoma. Esophagus. 13:1–7. 2016. View Article : Google Scholar : PubMed/NCBI
|