Introduction
Radiotherapy is a treatment option for esophageal
cancer, and chemoradiotherapy (CRT) is the standard method of
treatment for patients with unresectable esophageal cancer
(1,2). The number of elderly patients
diagnosed with unresectable esophageal cancer is increasing given
the aging population and the occurrence of complications.
Consequently, the number of patients undergoing CRT is also
increasing. Notably, the radical irradiation field in esophageal
cancer, including the prophylactic lymph node region, is quite
large. Furthermore, the dose delivered to the heart is increased,
particularly if the primary tumor is located in the middle thoracic
esophagus or below. Pericardial effusion, pericarditis, and
myocarditis are acute adverse events of the heart, and ischemic
heart disease, coronary artery disease, atherosclerosis, and
valvular disease are late adverse events (3,4). The
development of radiotherapy-induced cardiotoxicity is a
well-recognized complication in the treatment of left breast
cancer. Additionally, a correlation between cardiac mortality and
the dose delivered to the heart has been reported (5–8).
However, several reports of cardiotoxicity are delayed effects, and
the acute effects on the heart remain to be clarified. Brain
natriuretic peptide (BNP) is a peptide hormone synthesized in the
ventricle that protects the heart. Moreover, its secretion is
increased in response to the damage to the heart. Hence, it is
clinically used as a biochemical marker of heart failure (9,10). The
present study focused on the fluctuations of BNP levels to
investigate the early effects of radiotherapy on the heart. The
purpose of this study was to investigate the effectiveness of BNP
as a predictor of the effects of radiotherapy on the heart of
patients with esophageal cancer.
Materials and methods
Patients
A total of 41 patients with esophageal cancer were
enrolled in the present study. Following a thorough explanation of
the clinical stage and prognosis, treatment goals, schedules, and
adverse events, all included patients provided written informed
consent for chemoradiotherapy. All patients underwent definitive
CRT at Hirosaki University Hospital (Hirosaki, Japan) between
September 2014 and June 2019. The median age of the cohort,
including 34 men and 7 women, was 68 years (age range, 54–78
years). Patient evaluation included physical examination, biopsy
using esophagogastroduodenoscopy, blood counts, blood chemistry
tests, respiratory function tests, blood gas analysis, and
electrocardiography. The levels of BNP were determined in all
patients before and after CRT. According to the 8th edition of the
Union for International Cancer Control guidelines, the clinical
staging was performed using chest radiographs, chest-pelvic
computed tomography (CT) scans, and positron-emission tomography/CT
(PET/CT) scans. This study was approved by the institutional
research review board of our institution (approval no.
2020-089).
Chemoradiotherapy
A 3D conformal radiotherapy planning procedure was
performed in all patients. Serial CT images at 2.5 mm intervals
were obtained. The gross tumor volume was defined as the volume of
the primary tumor and metastatic lymph nodes determined by
esophagogastroduodenoscopy, CT, and PET/CT imaging prior to
treatment. Metastatic lymph nodes were defined as lymph nodes
measuring ≥1 cm in size on CT imaging or positive on PET/CT
imaging. The clinical target volume was defined as the primary
tumor plus longitudinal margins of ≥5.0 cm, lateral margins of 0.5
cm, metastatic lymph nodes plus 0.5-cm margins, and prophylactic
lymph node area. The planning target volume was the clinical target
volume plus 0.5-cm margins. A 10 MV linear accelerator (Varian
Clinac iX, Varian Medical Systems) was used, and radiotherapy was
performed using the anterior-posterior opposing field technique
until a dose of 40 Gy was delivered. The field-in-field method was
used depending on the location of the primary lesion, as
appropriate. Following the delivery of 40 Gy, the spinal cord was
avoided using oblique opposing fields with the target volume,
excluding the prophylactic lymph node area from the planning target
volume. The total irradiation dose for the primary lesion and lymph
node metastasis ranged from 50–60 Gy (median, 60 Gy) at the
isocenter. All patients received concurrent chemotherapy. The
chemotherapy regimen included a combination of cisplatin (70
mg/m2 on day 1) and fluorouracil (700
mg/m2/day on days 1–4) as intravenous infusion. One or
two cycles of chemotherapy were administered during radiation
therapy.
Evaluation and analysis
The BNP measurement was outsourced to LSI Medience
Corporation (license no. 220AIAMX0000200) using a chemiluminescent
immunoassay. The upper limit of normal BNP was defined as 18.4
pg/ml, which is the reference value utilized by the company. The
range, median, mean and change ratio (± SD) of the BNP levels on
the first (pre-CRT) and the last (post-CRT) day of CRT were
calculated. The change ratio was calculated as follows: [(BNP
post-CRT)-(BNP pre-CRT)]/(BNP pre-CRT). The heart, including the
pericardium, was contoured based on the CT scans used for actual
radiotherapy planning to calculate the cardiac dosimetric
parameters. The upper end of the heart on CT was defined as the
area immediately below the left pulmonary artery (11). Following heart contouring, the mean
dose, V5, V10, V20, V30, V40, and V50 for the heart were obtained
from dose-volume histograms using radiotherapy planning software
(Monaco, version 5.11; Elekta). V5, V10, V20, V30, V40, and V50 are
the heart volume ratio irradiated with 5, 10, 20, 30, 40, and 50
Gy, or more radiation, respectively. Subsequently, the range,
median, and mean ± SD of the mean dose, V5, V10, V20, V30, V40, and
V50 were calculated. The BNP levels pre- and post-CRT were compared
using the Wilcoxon signed-rank test. The relationships between the
cardiac dosimetric parameters and the ratio of change in BNP were
analyzed using Spearman's correlation coefficient. The relationship
between BNP and survival was investigated using the Kaplan-Meier
method. The cumulative survival rate was calculated from the first
day of CRT, and the differences were compared using a log-rank
test. P<0.05 was considered to indicate a statistically
significant difference. All analyses were performed using GraphPad
Prism version 9.0 (GraphPad Software, Inc.). Treatment toxicity was
evaluated using the Common Terminology Criteria for Adverse Events
(version 4.0) established by the U.S. National Cancer Institute
(12).
Results
A summary of the patient's characteristics is
provided in Table I. All 41
patients were diagnosed with squamous cell carcinoma. The clinical
stages were as follows: stages I, II, III, and IV in 10, 5, 13, and
13 patients, respectively. The site of the primary lesion was the
cervical, upper thoracic, middle thoracic, and lower thoracic
esophagus in 6, 12, 13, and 10 patients, respectively. The number
of radiotherapy fractions ranged from 25–33, with a fraction size
of 1.8–2 Gy. The median total dose was 60 Gy (range, 50–60 Gy).
Prior to the diagnosis of esophageal cancer, cardiovascular
complications were observed in 26 patients (63%). Hypertension was
a cardiovascular complication that occurred in the majority of
patients. During the period of analysis, 18 patients were alive and
23 patients died. For all patients, the median follow-up period was
29.2 months (range, 1.7–82 months). For the surviving patients, the
median follow-up period was 55.6 months (range, 31.3–82
months).
 | Table I.Patient characteristics. |
Table I.
Patient characteristics.
| Characteristic | Value |
|---|
| Sex |
|
| Male | 34 (83) |
|
Female | 7 (17) |
| Age, years |
|
|
Median | 68 |
|
Range | 54-78 |
| Performance status, n
(%) |
|
| 0-1 | 40 (98) |
| 2 | 1 (2) |
| Stage, n (%) |
|
| I | 10 (24) |
| II | 5 (12) |
| III | 13 (32) |
| IV | 13 (32) |
| Site of primary
lesion, n (%) |
|
|
Cervical | 6 (15) |
| Upper
thoracic | 12 (29) |
| Middle
thoracic | 13 (32) |
| Lower
thoracic | 10 (24) |
| Radiation doses,
Gy |
|
|
Median | 60 |
|
Range | 50-60 |
| Cardiovascular
complications, n (%)a |
|
|
Hypertension | 25 (61) |
|
Diabetes | 6 (15) |
|
Dyslipideamia | 5 (12) |
| Follow-up duration,
months |
|
|
Median | 29.2 |
|
Range | 1.7–82 |
| Status, n (%) |
|
|
Alive | 18 (44) |
| Dead | 23 (56) |
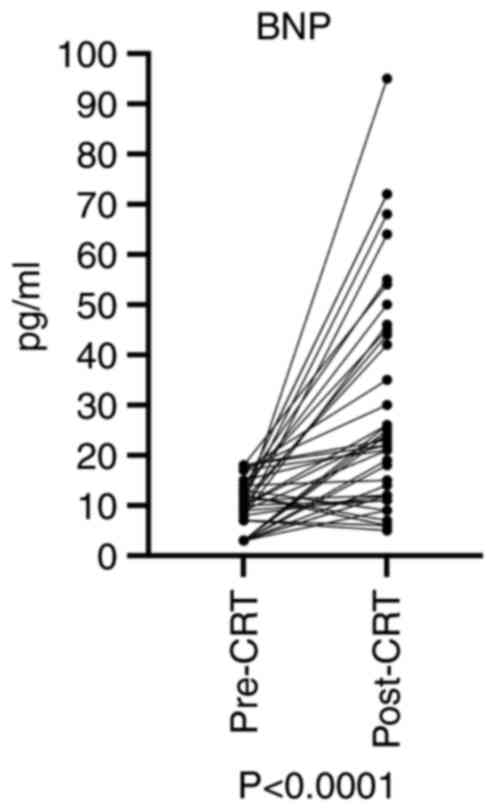
The BNP levels pre- and post-CRT and the change
ratio of BNP in all 41 patients are shown in Table II. The BNP levels pre-CRT ranged
from 3–18 pg/ml; the median and mean levels were 10 and 10.15
pg/ml, respectively. The BNP levels post-CRT ranged from 5–95
pg/ml; the median and mean levels were 22 and 29.02 pg/ml,
respectively. The change ratio of BNP ranged from −50-766.67%; the
median and mean levels were 200 and 246.11%, respectively.
Following CRT, 63% of patients had abnormally high BNP levels. In
the group with a higher change ratio (that is, above the median),
only 19% of patients (4/21) remained within the normal range after
CRT. However, in the group with a lower change ratio (that is,
below the median), 51% of patients (11/20) remained within the
normal range after CRT. The results of the comparison of BNP levels
pre- and post-CRT are shown in Fig.
1. The BNP levels were significantly elevated post-CRT compared
with pre-CRT (P<0.0001).
 | Table II.BNP before and after CRT and change
ratio of BNP. |
Table II.
BNP before and after CRT and change
ratio of BNP.
| Measurement | BNP pre-CRT,
pg/ml | BNP post-CRT,
pg/ml | Change ratio,
% |
|---|
| Range | 3-18 | 5-95 | −50-850 |
| Median | 10 | 22 | 200 |
| Mean ± SD | 10.15±4.78 | 29.02±21.95 | 246.11±255.97 |
The range, median, and mean ± SD values of the mean
dose, V5, V10, V20, V30, V40, and V50 for the heart are shown in
Table III. The median values were
33.9 Gy, 83.0, 76.8, 70.8, 62.3, 51.9, and 20.0%, respectively. The
mean values were 28.3 Gy, 70.5, 65.6, 59.8, 52.7, 42.2, and 19.6%,
respectively. The correlation coefficients for cardiac dosimetric
parameters and the change ratio are shown in Table IV. Significant correlations were
observed between the change ratio and mean dose (P=0.041), V5
(P=0.004), V10 (P=0.004), V20 (P=0.006), and V30 (P=0.016). Scatter
diagrams between the change ratio and mean dose, V5, V10, V20, and
V30 are shown in Fig. 2.
 | Table III.Dosimetric parameters of heart. |
Table III.
Dosimetric parameters of heart.
| Measurement | MD, Gy | V5, Gy | V10, Gy | V20, Gy | V30, Gy | V40, Gy | V50, Gy |
|---|
| Range | 0.9–44.8 | 3.5–96.9 | 1.8–94.2 | 0.3–89.3 | 0-82.7 | 0-75.4 | 0-51.8 |
| Median | 33.9 | 83.0 | 76.8 | 70.8 | 62.3 | 51.9 | 20.0 |
| Mean ± SD | 28.3±12.3 | 70.5±26.9 | 65.6±26.4 | 59.8±25.5 | 52.7±24.1 | 42.2±23.6 | 19.6±14.8 |
 | Table IV.Speaman's correlation coefficient by
rank for Change ratio of BNP and dosimetric parameters of
heart. |
Table IV.
Speaman's correlation coefficient by
rank for Change ratio of BNP and dosimetric parameters of
heart.
| Dose | R (95% confidence
interval), n=41 | P-value |
|---|
| Mean dose | 0.32
(0.005–0.578) | 0.041 |
| V5 | 0.44
(0.146–0.665) | 0.004 |
| V10 | 0.44
(0.146–0.665) | 0.004 |
| V20 | 0.42
(0.122–0.651) | 0.006 |
| V30 | 0.37
(0.066–0.618) | 0.015 |
| V40 | 0.24
(−0.081–0.518) | 0.128 |
| V50 | 0.14
(−0.181–0.440) | 0.370 |
A list of adverse events following CRT is shown in
Table V. Adverse events were
investigated using medical records and imaging tests, such as CT
and PET/CT scans. Cardiac events occurred in 14 patients.
Pericardial effusion, cardiomegaly, acute exacerbation of chronic
heart failure, and decreased ejection fraction (defined as a
decrease of <50%) were observed in 8, 4, 1, and 1 patients,
respectively. These cardiac events occurred between 1.4 and 52
months after CRT. All cardiac events were grade ≤2. A Mann-Whitney
U-test was used to compare the median dosimetric parameters, the
median change ratio, and median pre-CRT BNP levels between 14
patients who experienced cardiac events and 27 patients who did not
(Fig. 3). Significant differences
were observed in the V5 (P=0.002), V10 (P=0.007), V20 (P=0.012),
V30 (P=0.009), and change ratio (P=0.009). There was no significant
difference in pre-CRT BNP levels. In addition to cardiac events,
dermatitis, esophagitis, and myelosuppression were observed as
acute adverse events. A Mann-Whitney U-test was used to compare the
median change ratio and median pre-CRT BNP levels between low and
intermediate grades of these adverse events, but there was no
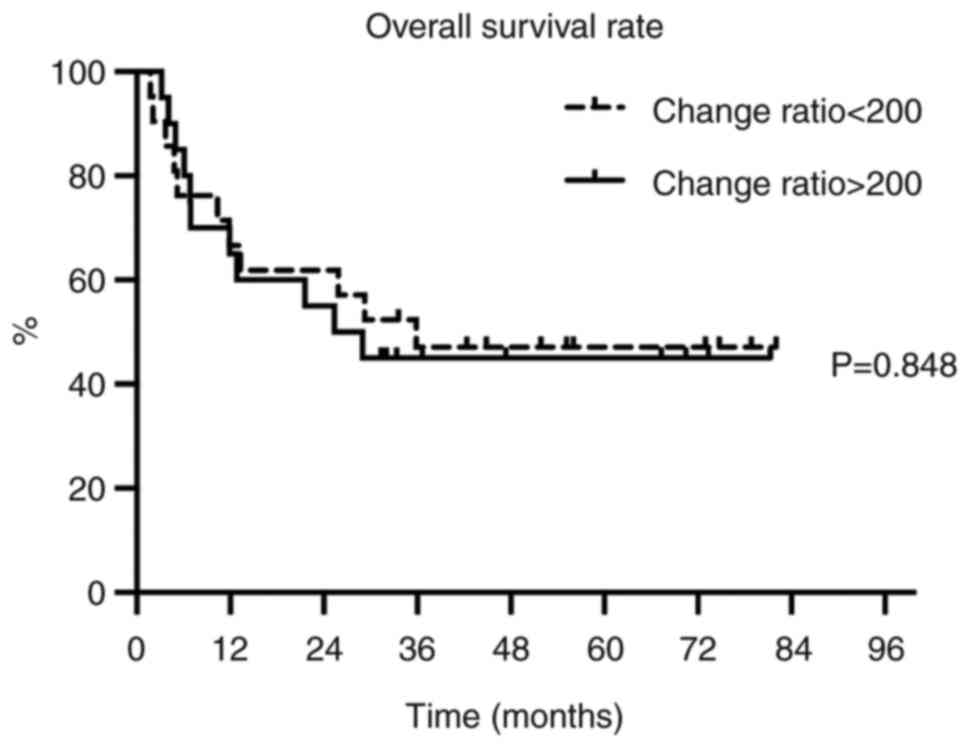
significant association with BNP. The relationship between BNP and
survival was investigated using the Kaplan-Meier method. However,
there was no significant difference between 20 patients with a
lower change ratio (that is, below the median) and 21 patients with
a higher change ratio (that is, above the median) (Fig. 4).
 | Table V.Adverse events of
chemoradiotherapy. |
Table V.
Adverse events of
chemoradiotherapy.
| Adverse events | Grade 1, n | Grade 2, n | Grade 3, n |
|---|
| Cardiac events |
|
|
|
|
Pericardial effusion | 0 | 8 | 0 |
|
Cardiomegaly | 4 | 0 | 0 |
| Acute
exacerbation of chronic heart failure | 0 | 1 | 0 |
|
Decreased ejection
fraction | 0 | 1 | 0 |
| Dermatitis | 34 | 7 | 0 |
| Esophagitis | 8 | 30 | 3 |
|
Myelosuppression | 4 | 17 | 20 |
Discussion
The present study focused on the fluctuations of BNP
levels. Thus far, only a few previous studies have investigated the
relationship between radiotherapy and atrial natriuretic peptide
(ANP). Wondergem et al (13)
investigated 121 patients with Hodgkin's disease and breast cancer.
They reported that patients who experienced cardiac events after
radiotherapy had significantly higher ANP levels compared with
those who did not. Additionally, studies conducted on rhesus
monkeys or rats reported similar findings, indicating that ANP
levels were increased after total-body irradiation or whole-heart
irradiation (14,15). No reports were published on the
relationship between radiotherapy and BNP until around the year
2000. Nevertheless, a few studies have suggested that BNP is an
effective predictor of various cardiac dysfunctions in patients
with heart failure (9,10). To the best of our knowledge, Jingu
et al (16) was the first to
report that BNP levels were significantly increased ≥9 months vs.
<9 months after radiotherapy. In the present study, BNP levels
were determined on the last day of CRT. The BNP levels post-CRT
were also significantly elevated compared with those recorded
pre-CRT. This finding suggests that BNP levels in the heart may
have been elevated by radiotherapy.
A previous study reported that the change ratio of
BNP is a predictor of cardiac events. In patients with nonischemic
chronic heart failure, a ≥15% increase in BNP levels was considered
a risk factor for the occurrence of cardiac events (17). In another study, involving patients
with chronic heart failure, the relationship between the change
ratio and mortality in the N-terminal-pro-BNP, a precursor BNP was
investigated. The results demonstrated that the rate of all-cause
mortality was increased in parallel with the change ratio (18). Based on these reports showing the
usefulness of the change ratio of BNP, the correlation between
dosimetric parameters of the heart and change ratio was
investigated to explore the relationship between the degree of BNP
elevation after radiotherapy and the dose delivered to the heart.
In the present study, significant correlations were observed
between the dosimetric parameters of the heart and the change
ratio, except for V40 and V50. However, the correlation
coefficients were ~0.4 for these parameters, and although there
were significant differences, the correlations were weak. In
contrast, there were no significant correlations observed between
the absolute BNP levels after radiotherapy and dosimetric
parameters of the heart (data not shown).
Similarly, there was a prospective study that
investigated the correlation coefficients between dosimetric
parameters of the heart and BNP in 43 cases of left breast cancer
(19). This study examined the
normalized BNP concentration, which is defined as the
post-treatment BNP levels divided by the pre-treatment BNP levels.
The results demonstrated significant correlations in V20, V25, V30,
and V45 with the mean dose of the heart. This evidence is
consistent with the findings of the present study, suggesting that
an elevation in BNP levels due to radiotherapy is associated with
low- to medium-dose irradiation rather than high-dose
irradiation.
A long-term toxicity study used the Radiation
Therapy Oncology Group/European Organization for Research and
Treatment of Cancer late radiation morbidity scoring scheme to
investigate 139 patients with thoracic esophageal cancer who
underwent CRT. The results demonstrated that 16 patients (11.5%)
developed symptomatic grade ≥2 pericarditis (20). In the present study, 14 patients
(34%) developed cardiac events, with the majority of events being
pericardial effusions (20%). In addition, all cases of pericardial
effusion were asymptomatic and grade 2, as evaluated using Common
Terminology Criteria for Adverse Events version 4. Of note, lethal
events were not observed in the present study. The median period
for the development of cardiac events was 12 months (range: 1.4–43
months). However, as pericardial effusion and cardiomegaly are
often detected through imaging, the actual time of development may
have been earlier. It is hypothesized that performing imaging
analyses every 3–6 months at our institution may have resulted in
this delay. Therefore, numerous cardiac events observed in this
study were acute to subacute adverse events. The relationship
between the development of cardiac events and the change ratio of
BNP and dosimetric parameters of the heart was investigated. The
median change ratio, V5, V10, V20, and V30 were significantly
higher in patients who developed a cardiac event vs. those who did
not. The results indicated that BNP might be an early predictor of
cardiac stress due to radiotherapy, similar to previous reports
(16,19). It was also suggested that the change
ratio of BNP and percentage of low- to medium-dose area irradiated
to the heart might be an effective predictor of cardiac event
development.
Due to aging, CRT is frequently utilized in Japan
for the treatment of esophageal cancer, including cases of
medically unresectable stage I cancer (21,22). A
previous report indicated that the 4-year survival rate for stage I
esophageal cancer is ~80% (23).
Additionally, the outcomes of CRT have improved over the past few
years. The effects of chemotherapy on the heart should also be
considered when administering CRT. A study on the cardiac effects
of preoperative treatment for esophageal cancer reported more
cardiac complications with CRT vs. chemotherapy alone (24,25).
Therefore, to reduce the risk of adverse events in the hearts of
patients for longer-term survival, it is necessary to decrease the
dose delivered to the heart.
This study has some limitations. As this was a
single institute study, the number of included patients was small,
the follow-up period was short, and the development of cardiac
events may not have been fully grasped. The reason for the short
follow-up period was that 26 patients with stage III or IV disease
were included in the study and >50% of the 26 patients succumbed
to cancer or other coexisting complications at a relatively early
time following CRT. Therefore, the value of BNP as a predictor of
survival could not be determined. Imaging tests such as
echocardiography, nuclear medicine examination, and cardiac MRI
have been reported to be useful in evaluating myocardial damage
associated with cancer therapy (26,27).
As this study was a retrospective study, unfortunately, these
imaging tests were not performed in all patients. Regarding
irradiation technology, numerous institutions have recently begun
using intensity-modulated radiation therapy. In this study, several
patients received conventional radiotherapy; thus, it is important
to use intensity-modulated radiation therapy to reduce the cardiac
dose and investigate patients treated with intensity-modulated
radiation therapy in the future.
In conclusion, the present study revealed that BNP
levels after CRT were significantly increased in patients with
esophageal cancer, and the change ratio pre- and post-CRT
correlated with the dose delivered to the heart, particularly the
percentage of low- to medium-dose areas. Furthermore, it was found
that the change ratio and the percentage of the low- to medium-dose
areas were significantly higher in patients who experienced a
cardiac event compared with those who did not. The change ratio of
BNP pre- and post-CRT may thus be a useful predictor of cardiac
events.
Acknowledgments
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YH, MT, CY, KI, IF, MS, HK and MA contributed to the
study conception and design. SK, RO, and AK collected and analyzed
the data. YH wrote the manuscript, analyzed data, and performed the
literature search. All authors have read and approved the final
manuscript. YH, SK, RO, and AK confirm the authenticity of all raw
data.
Ethics approval and consent to
participate
This study was approved by the institutional
research review board of the Hirosaki University Graduate School of
Medicine (approval no. 2020-089). The Institutional Research Review
Board of the Hirosaki University Graduate School of Medicine waived
the requirement for informed consent due to the retrospective
nature of the study. This study was performed using the opt-out
method on the hospital website.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that there are no competing
interests.
References
|
1
|
Herskovic A, Martz K, Al-Sarraf M,
Leichman L, Brindle J, Vaitkevicius V, Cooper J, Byhardt R, Davis L
and Emami B: Combined chemotherapy and radiotherapy compared with
radiotherapy alone in patients with cancer of the esophagus. N Engl
J Med. 326:1593–1598. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kato K, Nakajima TE, Ito Y, Katada C,
Ishiyama H, Tokunaga SY, Tanaka M, Hironaka S, Hashimoto T, Ura T,
et al: Phase II study of concurrent chemoradiotherapy at the dose
of 50.4 Gy with elective nodal irradiation for stage II–III
esophageal carcinoma. Jpn J Clin Oncol. 43:608–615. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Darby SC, Cutter DJ, Boerma M, Constine
LS, Fajardo LF, Kodama K, Mabuchi K, Marks LB, Mettler FA, Pierce
LJ, et al: Radiation-related heart disease: Current knowledge and
future prospects. Int J Radiat Oncol Biol Phys. 76:656–665. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Gagliardi G, Constine LS, Moiseenko V,
Correa C, Pierce LJ, Allen AM and Marks LB: Radiation dose-volume
effects in the heart. Int J Radiat Oncol Biol Phys. 76 (3
Suppl):S77–S85. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sardaro A, Petruzzelli MF, D'Errico MP,
Grimaldi L, Pili G and Portaluri M: Radiation-induced cardiac
damage in early left breast cancer patients: Risk factors,
biological mechanisms, radiobiology, and dosimetric constraints.
Radiother Oncol. 103:133–142. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Correa CR, Litt HI, Hwang WT, Ferrari VA,
Solin LJ and Harris EE: Coronary artery findings after left-sided
compared with right-sided radiation treatment for early-stage
breast cancer. J Clin Oncol. 25:3031–3037. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Rutqvist LE, Lax I, Fornander T and
Johansson H: Cardiovascular mortality in a randomized trial of
adjuvant radiation therapy versus surgery alone in primary breast
cancer. Int J Radiat Oncol Biol Phys. 22:887–896. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Gyenes G, Rutqvist LE, Liedberg A and
Fornander T: Long-term cardiac morbidity and mortality in a
randomized trial of pre- and postoperative radiation therapy versus
surgery alone in primary breast cancer. Radiother Oncol.
48:185–190. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Cowie MR, Struthers AD, Wood DA, Coats AJ,
Thompson SG, Poole-Wilson PA and Sutton GC: Value of natriuretic
peptides in assessment of patients with possible new heart failure
in primary care. Lancet. 350:1349–1353. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Maisel AS, Krishnaswamy P, Nowak RM,
McCord J, Hollander JE, Duc P, Omland T, Storrow AB, Abraham WT, Wu
AH, et al: Rapid measurement of B-type natriuretic peptide in the
emergency diagnosis of heart failure. N Engl J Med. 347:161–167.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Feng M, Moran JM, Koelling T, Chughtai A,
Chan JL, Freedman L, Hayman JA, Jagsi R, Jolly S, Larouere J, et
al: Development and validation of a heart atlas to study cardiac
exposure to radiation following treatment for breast cancer. Int J
Radiat Oncol Biol Phys. 79:10–18. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
National Cancer Institute NIH, US
Department of Health and Human Sevices (2009), . Common terminology
criteria for adverse events. version 4.0. https://evs.nci.nih.gov/ftp1/CTCAE/CTCAE_4.03/CTCAE_4.03_2010-06-14_QuickReference_8.5×11.pdfJuly
7–2023
|
|
13
|
Wondergem J, Strootman EG, Frölich M, Leer
JW and Noordijk EM: Circulating atrial natriuretic peptide plasma
levels as a marker for cardiac damage after radiotherapy. Radiother
Oncol. 58:295–301. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wondergem J, Persons K, Zurcher C, Frölich
M, Leer JW and Broerse J: Changes in circulating atrial natriuretic
peptide in relation to the cardiac status of Rhesus monkeys after
total-body irradiation. Radiother Oncol. 53:67–75. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kruse JJ, Strootman EG, Bart CI, Visser A,
Leer JW and Wondergem J: Radiation-induced changes in gene
expression and distribution of atrial natriuretic peptide (ANP) in
different anatomical regions of the rat heart. Int J Radiat Biol.
78:297–304. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Jingu K, Nemoto K, Kaneta T, Oikawa M,
Ogawa Y, Ariga H, Takeda K, Sakayauchi T, Fujimoto K, Narazaki K,
et al: Temporal change in brain natriuretic peptide after
radiotherapy for thoracic esophageal cancer. Int J Radiat Oncol
Biol Phys. 69:1417–1423. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Nishiyama K, Tsutamoto T, Yamaji M,
Kawahara C, Fujii M, Yamamoto T and Horie M: Biological variation
of brain natriuretic peptide and cardiac events in stable
outpatients with nonischemic chronic heart failure. Circ J.
75:341–347. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Masson S and Latini R: Amino-terminal
pro-B-type natriuretic peptides and prognosis in chronic heart
failure. Am J Cardiol. 101:56–60. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Palumbo I, Palumbo B, Fravolini ML,
Marcantonini M, Perrucci E, Latini ME, Falcinelli L, Sabalich I,
Tranfaglia C, Schillaci G, et al: Brain natriuretic peptide as a
cardiac marker of transient radiotherapy-related damage in
left-sided breast cancer patients: A prospective study. Breast.
25:45–50. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ishikura S, Nihei K, Ohtsu A, Boku N,
Hironaka S, Mera K, Muto M, Ogino T and Yoshida S: Long-term
toxicity after definitive chemoradiotherapy for squamous cell
carcinoma of the thoracic esophagus. J Clin Oncol. 21:2697–2702.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Watanabe M, Tachimori Y, Oyama T, Toh Y,
Matsubara H, Ueno M, Kono K, Uno T, Ishihara R, Muro K, et al:
Comprehensive registry of esophageal cancer in Japan, 2013.
Esophagus. 18:1–24. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Watanabe M, Toh Y, Ishihara R, Kono K,
Matsubara H, Murakami K, Muro K, Numasaki H, Oyama T, Ozawa S, et
al: Comprehensive registry of esophageal cancer in Japan, 2014.
Esophagus. 19:1–26. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Kato H, Sato A, Fukuda H, Kagami Y,
Udagawa H, Togo A, Ando N, Tanaka O, Shinoda M, Yamana H and
Ishikura S: A phase II trial of chemoradiotherapy for stage I
esophageal squamous cell carcinoma: Japan Clinical Oncology Group
Study (JCOG9708). Jpn J Clin Oncol. 39:638–643. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Lund M, Alexandersson von Döbeln G,
Nilsson M, Winter R, Lundell L, Tsai JA and Kalman S: Effects on
heart function of neoadjuvant chemotherapy and chemoradiotherapy in
patients with cancer in the esophagus or gastroesophageal
junction-a prospective cohort pilot study within a randomized
clinical trial. Radiat Oncol. 10:162015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Zhang Z and Zhang H: Impact of neoadjuvant
chemotherapy and chemoradiotherapy on postoperative cardiopulmonary
complications in patients with esophageal cancer. Dis Esophagus.
30:1–7. 2007. View Article : Google Scholar
|
|
26
|
Plana JC, Galderisi M, Barac A, Ewer MS,
Ky B, Scherrer-Crosbie M, Ganame J, Sebag IA, Agler DA, Badano LP,
et al: Expert consensus for multimodality imaging evaluation of
adult patients during and after cancer therapy: A report from the
American Society of Echocardiography and the European Association
of Cardiovascular Imaging. J Am Soc Echocardiogr. 27:911–939. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Jordan JH, Vasu S, Morgan T, D'Agostino RB
Jr, Meléndez GC, Hamilton CA, Arai AE, Liu S, Liu CY, Lima JA, et
al: Anthracycline-associated T1 mapping characteristics are
elevated independent of the presence of cardiovascular
comorbidities in cancer survivors. Circ Cardiovasc Imaging.
9:e0043252016. View Article : Google Scholar : PubMed/NCBI
|