Introduction
Osteosarcoma, a primary malignant bone tumor
originating from bone mesenchymal cells, is one of the most
prevalent malignancies affecting children, adolescents and young
adults (1–3). Despite its rarity, ~1,000 new cases
are diagnosed in the United States each year (4). Osteosarcoma manifests in primary and
secondary forms, together accounting for nearly 20% of all primary
bone tumors (5). Characterized by
its highly aggressive nature, osteosarcoma often metastasizes
early, with the lung being the most frequent site for distant
metastases. At the time of diagnosis, the majority of patients
already present with lung micro-metastases, which serve as the
primary cause of death (6).
Current treatment options for osteosarcoma include
surgical procedures, chemotherapy, biological immunotherapy,
molecular targeted therapy and other similar approaches. The
five-year overall survival (OS) rate following comprehensive
osteosarcoma treatment ranges from 66–82% (7). The standard treatment protocol
typically involves neoadjuvant chemotherapy, followed by surgery
and adjuvant chemotherapy (8).
Increasing evidence suggests that limb-sparing surgery is gradually
replacing amputation in the treatment of osteosarcoma (9,10).
Nevertheless, some studies argue that early and aggressive tumor
removal through amputation effectively prevents further fracture
development, making it a preferable choice for osteosarcoma cases
complicated with pathological fractures (11,12).
Han et al (13) conducted a meta-analysis of articles
published before 2015, comparing amputation with limb-salvage
surgery in patients with osteosarcoma, demonstrating higher
five-year survival rates and improved functionality with
limb-salvage surgery. Another meta-analysis published in 2022
compared the efficacy of limb-salvage surgery and amputation in
patients with osteosarcoma treated with neoadjuvant chemotherapy
(14).
The present study primarily focused on the
effectiveness of limb-salvage treatment for adolescent osteosarcoma
patients. By conducting a meta-analysis of the published literature
on osteosarcoma surgical treatment, the goal was to systematically
evaluate the clinical efficacy of both limb-salvage treatment and
amputation in order to determine the most appropriate treatment
strategies for adolescent patients. The current meta-analysis aimed
to provide guidance for the clinical treatment of osteosarcoma.
Materials and methods
Guideline, inclusion and exclusion
criteria for literature selection
In the present study, the PRISMA guidelines
(http://www.prisma-statement.org/)
were followed. Inclusion criteria were as follows: a definitive
diagnosis of osteosarcoma and articles written in English.
Exclusion criteria included duplicate publications, reviews,
editorials, single case reports and studies without full text,
incomplete information, or studies from which data extraction was
impossible.
Search strategy
PubMed (https://pubmed.ncbi.nlm.nih.gov/), Embase (https://www.embase.com/) and the Cochrane Library
(https://www.cochranelibrary.com/) were
searched for relevant literature. The search period extended from
the inception of each database to September 2022. The search terms
used included ‘Osteosarcoma’, ‘Osteosarcoma Tumor’, ‘Osteogenic
Sarcomas’, ‘Limb Salvage’ and ‘Amputation’. Specific search strings
for each database were as follows: PubMed: ‘osteosarcoma’[MeSH
Terms] OR ‘Osteosarcoma Tumor’[All Fields] OR ‘Osteogenic
Sarcomas’[All Fields] OR ‘limb salvage surgery’[All Fields] OR
‘amputation’[All Fields]; Embase: ‘osteosarcoma’/limb salvage
treatment’/amputation; Cochrane Library: (osteosarcoma): ti,ab,kw
OR (limb salvage surgery): ti,ab,kw (word variations were also
searched).
Literature screening and data
extraction
The authors of the present study independently
conducted literature search, screening and data extraction. Any
uncertainties were resolved through discussion with the
corresponding author. Extracted data included author, year, region,
study type, number of cases, OS, progression-free survival (PFS),
five-year OS rate, local recurrence rate and distant metastases
rate.
Literature quality assessment
The authors of the present study independently used
the Newcastle-Ottawa Scale (NOS) (15) to assess the quality of the included
studies. Discrepancies were resolved through consultation or by
seeking the opinion of a third party. The NOS comprises four items
(four points) for ‘Research Subject Selection’, one item (two
points) for ‘Comparability between Groups’ and three items (three
points) for ‘Outcome Measurement’, with a maximum score of nine
points. Studies scoring ≥7 were considered high quality, while
those scoring <7 were deemed lower quality.
Statistical methods
Hazard ratios (HR) and 95% confidence intervals (CI)
were used to evaluate OS and PFS, while odds ratios (OR) and 95% CI
were used to assess the five-year OS rate, local recurrence rate
and metastases rate. A fixed-effects model was employed for
combined analysis if the heterogeneity test yielded P≥0.1 and
I2≤50%; otherwise, a random-effects model was applied if
P<0.1 and I2>50%. Sensitivity analyses were
conducted to explore sources of heterogeneity when necessary. The
presence of publication bias was determined by assessing the
symmetry of funnel plots. All data were analyzed using Stata
(v.15.1; StataCorp LLC).
Results
Literature search outcomes
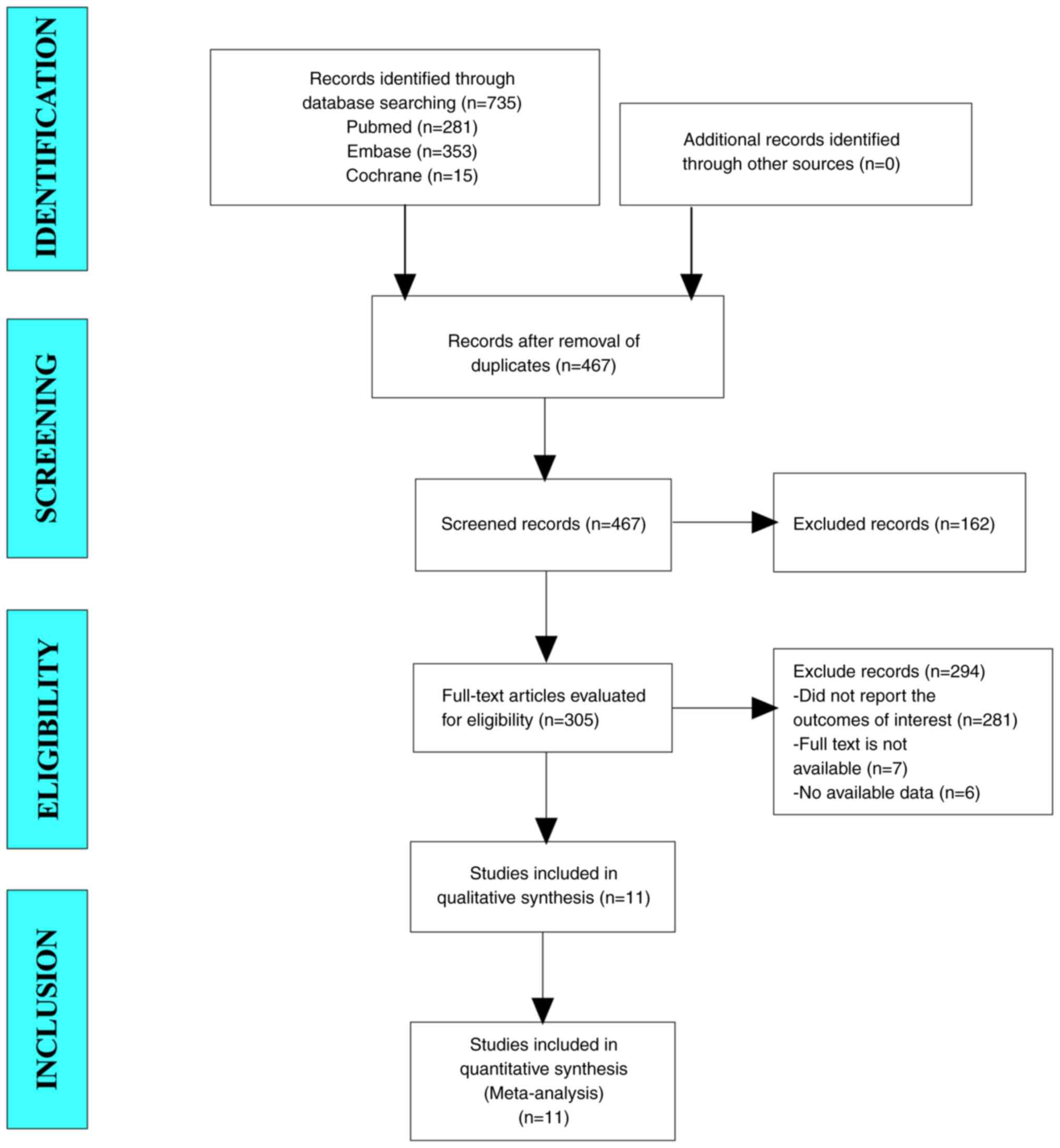
A comprehensive search of PubMed, Embase and
Cochrane Library yielded 735 articles. After removing duplicates, a
total of 467 unique articles remained. Upon reviewing the
abstracts, a total of 305 articles were selected for further
examination. Ultimately, after a thorough full-text evaluation, 11
articles were deemed suitable for inclusion in the meta-analysis
(Fig. 1).
Baseline characteristics and quality
assessment of included studies
The baseline characteristics and quality assessment
of the included studies are presented in Table I. All studies had NOS scores of ≥7
points, indicating satisfactory quality.
 | Table I.Summary of baseline characteristics
and quality assessment of included studies. |
Table I.
Summary of baseline characteristics
and quality assessment of included studies.
|
|
|
| Number of cases | Sex | Age |
|
|
|
|---|
|
|
|
|
|
|
|
|
|
|
|---|
| First author/s,
year | Region | Research type | Limb salvage | Amputation | Limb salvage | Amputation | Limb salvage | Amputation | Follow-up time
(year) | NOS score | (Refs.) |
|---|
| Kaneuchi et
al, 2022 | UK | Cohort | 65 | 17 | 32/50 |
| 8(3–9) |
| 10 | 7 | (23) |
| Qi et al,
2020 | China | Cohort | 2,447 | 916 | 1,330/1,117 | 578/388 | / | / | 5 | 7 | (10) |
| Yasin et al,
2020 | Malaysia | Cohort | 81 | 25 | / | / | / | / | 10 | 7 | (24) |
| Lin et al,
2018 | China | Cohort | 38 | 43 | / | / | / | / | 5 | 8 | (25) |
| Puri et al,
2017 | India | Cohort | 552 | 186 | 521/217 |
| 19 (3–64) |
| 3 (3–11) | 7 | (26) |
| Poudel et
al, 2017 | India | Cohort | 77 | 18 | 64/31 |
| / | / | 2.8 (0.3–6.8) | 8 | (27) |
| Kamal et al,
2016 | Indonesia | Cohort | 37 | 42 | / | / | 17 (14–23) |
| / | 8 | (28) |
| Faisham et
al, 2015 | Malaysia | Cohort | 80 | 41 | / | / | 19 (6–59) |
| 3.9 (3–7) | 8 | (29) |
| Mavrogenis et
al, 2012 | Italy | Cohort | 23 | 19 | 12/11 | 11/8 | 23 (10–51) | 29 (7–78) | 5.6 (0.7–23.9) | 7 | (20) |
| Bacci et al,
2002 | Italy | Cohort | 465 | 95 | 263/202 | 57/38 | / | / | 10.5 (5–17) | 7 | (30) |
| Abudu et al,
1996 | UK | Cohort | 27 | 13 | 26/14 |
| 18 (2–46) |
| 4.6 (0.7–14.6) | 7 | (21) |
Results of meta-analysis
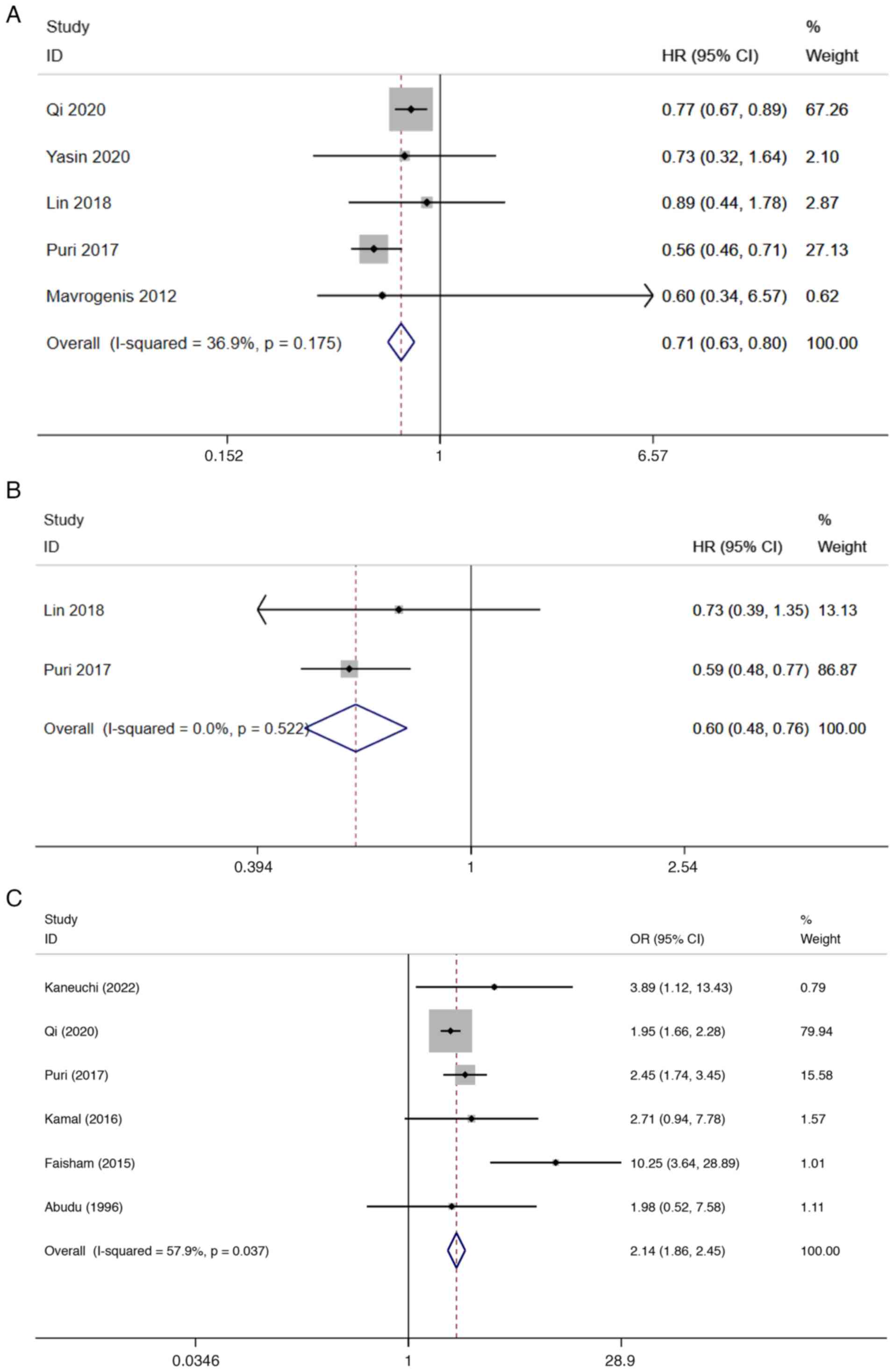
Firstly, the differences in OS following limb
salvage and amputation surgeries for osteosarcoma were
investigated. The analysis revealed that OS was significantly
longer after limb-salvage surgery compared with amputation surgery
(HR=0.71; 95% CI:0.63–0.80; P<0.001; I2=36.9%;
P=0.175; 5 articles included) (Fig.
2A). Moreover, the pooled results demonstrated that PFS after
limb-salvage surgery was also significantly longer than after
amputation surgery (HR=0.60; 95% CI: 0.48–0.76; P<0.001;
I2=0.0%; P=0.522; 2 articles included) (Fig. 2B). To further confirm the efficacy
of limb-salvage surgery, the five-year OS rate was analyzed, which
was 2.67 times higher after limb-salvage surgery compared with
amputation surgery (OR=2.14; 95% CI: 1.86–2.45; P=0.037;
I2=57.9%; P<0.001; 6 articles included) (Fig. 2C).
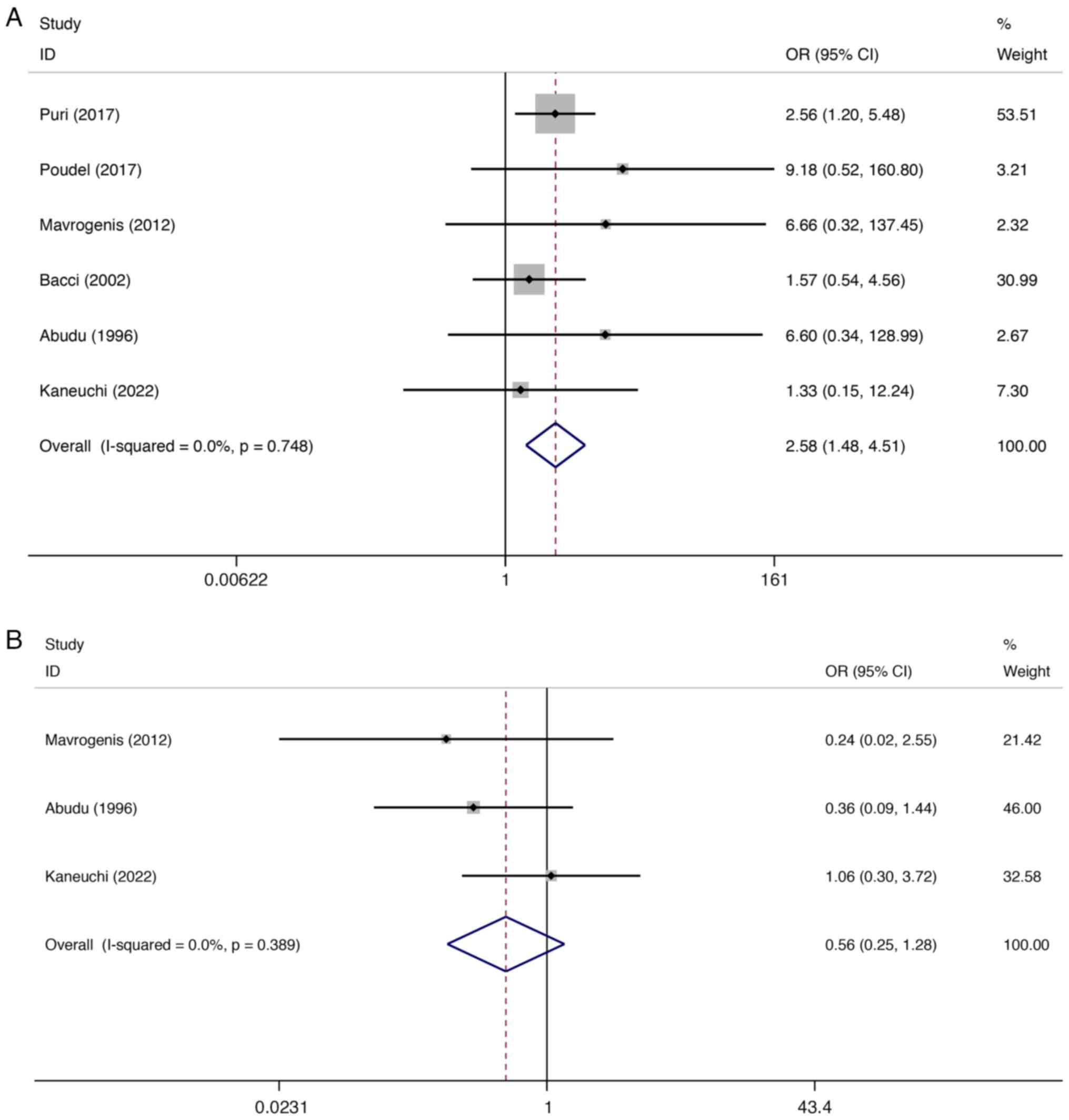
Additionally, the local recurrence and distant
metastasis rates between the two surgical approaches were compared.
The local recurrence rate following limb-salvage surgery was
significantly higher than after amputation (OR=2.58; 95% CI:
1.48–4.51; P=0.001; I2=0.0%, P=0.748; 5 articles
included) (Fig. 3A). However, there
was no statistically significant difference in the distant
metastasis rate between the two groups (OR=0.56; 95% CI: 0.25–1.28;
P=0.169; I2=0.0%; P=0.389; 3 articles included)
(Fig. 3B).
Sensitivity analysis
Sensitivity analyses were conducted to assess the
impact of individual studies on the overall meta-analysis results
by sequentially excluding each study and recalculating the combined
HR or OR values. The sensitivity analysis results are illustrated
in Fig. S1, Fig. S2, Fig.
S3. No study influenced excessively the meta-analysis outcomes,
indicating that the findings of the present study are stable and
reliable.
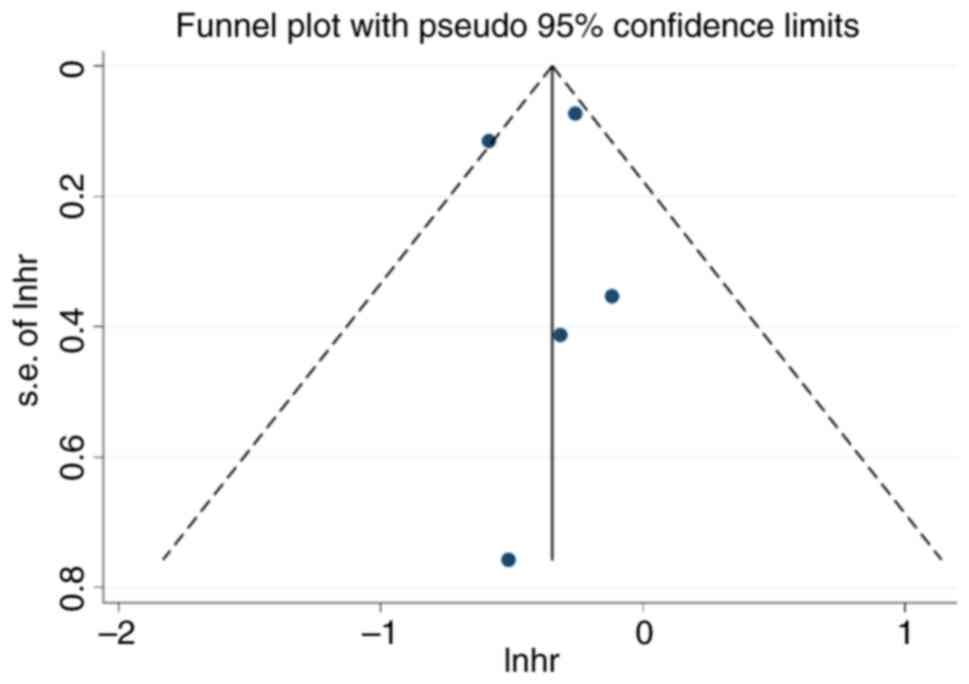
Publication bias
Due to the limited number of included articles
(n<12) for each variable, publication bias was assessed by using
funnel plots. As illustrated in Fig.
4, the funnel plots appeared asymmetric, suggesting potential
publication bias in the present study.
Discussion
Prior to the 1970s, amputation was the standard
treatment for osteosarcoma, yielding a five-year OS rate of <20%
post-surgery (16). However,
previous advancements in neoadjuvant chemotherapy, imaging
diagnostics, three-dimensional reconstruction technology and
enhanced chemotherapy effects have contributed to a significant
increase in patients with osteosarcoma opting for limb-salvage
surgery over amputation (17–19).
Nonetheless, existing literature presents contradictory findings
regarding survival rates and local recurrence rates in patients
undergoing limb salvage vs. amputation surgery (20). The present meta-analysis of 11
studies (encompassing 5,225 patients) aimed to provide clarity on
these rates, including OS, PFS, five-year OS rate, local recurrence
and distant metastasis for both limb salvage and amputation
surgeries.
The findings of the present study revealed that
patients in the limb-salvage treatment group exhibit longer OS and
PFS than those in the amputation group (HR=0.71; 95% CI: 0.63–0.80;
P<0.001 vs. HR=0.60; 95% CI: 0.48–0.76; P<0.001).
Additionally, the five-year OS rate was higher in the limb-salvage
group compared with the amputation group (OR=2.14; 95% CI:
1.86–2.45; P=0.037; I2=57.9%; P<0.001). While Abudu
et al (21) asserted that
amputation surgery does not prolong OS despite improved eradication
of local tumors, a different study argues that limb-salvage therapy
does not impact patient survival rates (22). The present comprehensive and
systematic analysis resolved these disputes, concluding that
limb-salvage surgery is more effective than amputation surgery in
treating osteosarcoma patients.
Concerning local recurrence rates, the present study
observed that the limb-salvage group had a significantly higher
rate compared with the amputation group (OR=2.58; 95% CI:
1.48–4.51; P=0.001). This contradicts the meta-analysis conducted
by Han et al (13), which
detected no differences in post-operative local recurrence rates
between the two groups. This discrepancy highlights the need for
clinicians to carefully consider the trade-off between therapeutic
effects and local recurrence rates when selecting limb-salvage
surgery for osteosarcoma treatment. Furthermore, the present study
indicated no significant difference in distant metastasis rates
between the limb salvage and amputation groups (OR=0.32; 95% CI:
0.10–1.06; P=0.062) (data not shown), aligning with the findings of
Mavrogenis et al (20).
However, due to the limited information on distant metastasis
rates, this conclusion is based on only two studies and
necessitates further investigation through high-quality randomized
controlled trials.
Despite the aforementioned findings, the present
study has certain limitations. The selection bias is the first
limitation of the present analysis. All included articles are
retrospective studies, with most of them possessing small sample
sizes, which may introduce systematic and random errors. Secondly,
factors such as tumor stage and metastasis could impact surgical
outcomes, but the present study was unable to account for these
variables due to the limited number of articles. This may
contribute to the observed heterogeneity. Lastly, the inability to
perform Egger's test for publication bias assessment may lead to
potential bias. Consequently, while the present study offers more
comprehensive evidence than previous research, the conclusions
warrant further validation through large-sample randomized
controlled trials of high quality.
In conclusion, the present meta-analysis underscored
the efficacy of limb-salvage therapy as a viable treatment option
for adolescent osteosarcoma patients. The OS and PFS rates of
patients undergoing limb-salvage surgery surpass those of
amputation. Furthermore, the five-year OS rate is notably higher in
comparison with amputation, while the rate of distant metastasis
remains analogous. However, it is important to note that the local
recurrence rate of limb-salvage surgery is significantly higher
than that of amputation.
Supplementary Material
Supporting Data
Acknowledgements
Not applicable.
Funding
This study was supported by the Project of MeiShan Science and
Technology Bureau (grant nos. kjzd202217, kjzd202218 and
kjzd202221), and Sichuan Provincial Nursing Research Project
Program (grant no. H20019).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
LW performed the literature search, helped with data
analysis, and drafted the manuscript. YF and YZ added new data to
the present meta-analysis, and performed some statistical analysis.
GZ conceptualized and designed the study. YF and YZ confirm the
authenticity of all the raw data. All authors read and approved the
final version of the manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Wang LL, Gebhardt MC and Rainusso N:
Osteosarcoma: Epidemiology, pathology, clinical presentation, and
diagnosis. UpToDate. 2022.
|
|
2
|
Beird HC, Bielack SS, Flanagan AM, Gill J,
Heymann D, Janeway KA, Livingston JA, Roberts RD, Strauss SJ and
Gorlick R: Osteosarcoma. Nat Rev Dis Primers. 8:772022. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Eaton BR, Schwarz R, Vatner R, Yeh B,
Claude L, Indelicato DJ and Laack N: Osteosarcoma. Pediatr Blood
Cancer. 68 (Suppl 2):e283522021. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
American cancer society, . Cancer facts
and figures 2020. American cancer society Inc.; Atlanta: pp. 1–52.
2020
|
|
5
|
Prater S and McKeon B: Osteosarcoma.
StatPearls Treasure Island, Fl: 2023
|
|
6
|
Luetke A, Meyers PA, Lewis I and Juergens
H: Osteosarcoma treatment-where do we stand? A state of the art
review. Cancer Treat Rev. 40:523–532. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Italiano A, Mir O, Mathoulin-Pelissier S,
Penel N, Piperno-Neumann S, Bompas E, Chevreau C, Duffaud F,
Entz-Werlé N, Saada E, et al: Cabozantinib in patients with
advanced Ewing sarcoma or osteosarcoma (CABONE): A multicentre,
single-arm, phase 2 trial. Lancet Oncol. 21:446–455. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Marec-Berard P, Dalban C, Gaspar N,
Brugieres L, Gentet JC, Lervat C, Corradini N, Castex MP, Schmitt
C, Pacquement H, et al: A multicentric randomized phase II clinical
trial evaluating high-dose thiotepa as adjuvant treatment to
standard chemotherapy in patients with resectable relapsed
osteosarcoma. Eur J Cancer. 125:58–68. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Carty CP, Dickinson IC, Watts MC, Crawford
RW and Steadman P: Impairment and disability following limb salvage
procedures for bone sarcoma. Knee. 16:405–408. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Qi L, Ren X, Liu Z, Li S, Zhang W, Chen R,
Chen C, Tu C and Li Z: Predictors and survival of patients with
osteosarcoma after limb salvage versus amputation: A
population-based analysis with propensity score matching. World J
Surg. 44:2201–2210. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Natarajan MV, Govardhan RH, Williams S and
Raja Gopal TS: Limb salvage surgery for pathological fractures in
osteosarcoma. Int Orthop. 24:170–172. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ebeid W, Amin S and Abdelmegid A: Limb
salvage management of pathologic fractures of primary malignant
bone tumors. Cancer Control. 12:57–61. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Han G, Bi WZ, Xu M, Jia JP and Wang Y:
Amputation Versus Limb-Salvage Surgery in Patients with
Osteosarcoma: A Meta-analysis. World J Surg. 40:2016–2027. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Abdelgawad MA, Parambi DGT, Ghoneim MM,
Alotaibi NH, Alzarea AI, Hassan AH and Abdelrahim MEA: A
meta-analysis comparing efficiency of limb-salvage surgery vs
amputation on patients with osteosarcoma treated with neoadjuvant
chemotherapy. Int Wound J. 19:1616–1624. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lo CK, Mertz D and Loeb M:
Newcastle-Ottawa Scale: comparing reviewers' to authors'
assessments. BMC Med Res Methodol. 14:452014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Bacci G, Ferrari S, Mercuri M, Longhi A,
Capanna R, Tienghi A, Brach del Prever A, Comandone A, Cesari M,
Bernini G and Picci P: Neoadjuvant chemotherapy for extremity
osteosarcoma-preliminary results of the Rizzoli's 4th study. Acta
Oncol. 37:41–48. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Tsuchiya H and Tomita K: Prognosis of
osteosarcoma treated by limb-salvage surgery: The ten-year
intergroup study in Japan. Jpn J Clin Oncol. 22:347–353. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Smeland S, Wiebe T, Böhling T, Brosjö O,
Jonsson K and Alvegård TA: Chemotherapy in osteosarcoma. The
scandinavian sarcoma group experience. Acta Orthop Scand Suppl.
75:92–98. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Loh AHP, Wu H, Bahrami A, Navid F,
McCarville MB, Wang C, Wu J, Bishop MW, Daw NC, Neel MD and Rao BN:
Influence of bony resection margins and surgicopathological factors
on outcomes in limb-sparing surgery for extremity osteosarcoma.
Pediatr Blood Cancer. 62:246–251. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Mavrogenis AF, Abati CN, Romagnoli C and
Ruggieri P: Similar survival but better function for patients after
limb salvage versus amputation for distal tibia osteosarcoma. Clin
Orthop Relat Res. 470:1735–1748. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Abudu A, Sferopoulos NK, Tillman RM,
Carter SR and Grimer RJ: The surgical treatment and outcome of
pathological fractures in localised osteosarcoma. J Bone Joint Surg
Br. 78:694–698. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Zeifang F, Sabo D and Ewerbeck V:
Pathological fracture in primary malignant bone tumors. Chirurg.
71:1121–1125. 2000.(In German). View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Kaneuchi Y, Yoshida S, Fujiwara T, Evans S
and Abudu A: Limb salvage surgery has a higher complication rate
than amputation but is still beneficial for patients younger than
10 years old with osteosarcoma of an extremity. J Pediatr Surg.
57:702–709. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Yasin NF, Abdul Rashid ML and Ajit Singh
V: Survival analysis of osteosarcoma patients: A 15-year
experience. J Orthop Surg (Hong Kong). 28:23094990198966622020.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Lin L, Deng S, Zhang F, Liang Y and Huang
Z: The extremity localized classic osteosarcomas have better
survival than the axial non-classics. World J Surg Oncol.
16:392018. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Puri A, Byregowda S, Gulia A, Crasto S and
Chinaswamy G: A study of 853 high grade osteosarcomas from a single
institution-are outcomes in Indian patients different? J Surg
Oncol. 117:299–306. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Poudel RR, Tiwari V, Kumar VS, Bakhshi S,
Gamanagatti S, Khan SA and Rastogi S: Factors associated with local
recurrence in operated osteosarcomas: A retrospective evaluation of
95 cases from a tertiary care center in a resource challenged
environment. J Surg Oncol. 115:631–636. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Kamal AF, Widyawarman H, Husodo K,
Hutagalung EU and Rajabto W: Clinical outcome and survival of
osteosarcoma patients in cipto mangunkusumo hospital: Limb salvage
surgery versus amputation. Acta Med Indones. 48:175–183.
2016.PubMed/NCBI
|
|
29
|
Faisham WI, Mat Saad AZ, Alsaigh LN, Nor
Azman MZ, Kamarul Imran M, Biswal BM, Bhavaraju VM, Salzihan MS,
Hasnan J, Ezane AM, et al: Prognostic factors and survival rate of
osteosarcoma: A single-institution study. Asia Pac J Clin Oncol.
13:e104–e110. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Bacci G, Ferrari S, Lari S, Mercuri M,
Donati D, Longhi A, Forni C, Bertoni F, Versari M and Pignotti E:
Osteosarcoma of the limb. Amputation or limb salvage in patients
treated by neoadjuvant chemotherapy. J Bone Joint Surg Br.
84:88–92. 2002. View Article : Google Scholar : PubMed/NCBI
|