Introduction
Colorectal cancer is the third most common cancer,
accounting for 10% of all cancer cases. It is also the second
leading cause of cancer-related deaths worldwide. The risk factors
of developing colorectal cancer include age, family history,
personal history and lifestyle factors (1). Combination of neoadjuvant chemotherapy
with radiotherapy is an optional treatment for patients with
locally advanced sigmoid colon cancer (2), and it usually accompanies complete
mesocolic excision (3,4). Considerable variation in the small
intestine and bladder following pelvic and lower abdomen
irradiation can lead to normal organ toxicity (5–7).
Consequently, the goal of treatment is to improve the prognosis of
patients, reduce toxicity and enable patients to complete treatment
without interruption. At present, the principal methods to reduce
the toxicity of radiotherapy for colon cancer include image-guided,
intensity-modulated radiotherapy (IMRT), volumetric modulated arc
therapy and treatment with a full bladder (8). To achieve these goals when treating
patients with sigmoid colon cancer, the MRIdian system (ViewRay
Technologies, Inc.) is employed (9). In the present study, for 1 patient
with sigmoid colon cancer, the treatment plan included 50 Gy
administered in 25 daily fractions. The Tomotherapy Hi-Art system
(Accuray, Inc.) was used for the first six fractions. However,
during the treatment, the location of the tumor differed
substantially from the CT simulation image each time. Attempts to
recreate the image were unsuccessful, leading to the arrangement
for the patient to receive daily treatment using online adaptive
radiotherapy with the MRIdian system. The online adaptive treatment
plan system, employed through MRIdian system, allows medical
professionals to correct for daily tumor variations in both tumor
and normal tissue, and to reoptimize the treatment plan online.
This correction helps to amplify the tumor dose and reduce the
planning target volume (PTV), thereby reducing side effects
(10,11). The MRIdian system not only offers
soft tissue contrast images that surpass those of CT but also
provides real-time images to monitor and track the position of the
tumor during treatment, ensuring that the treatment target is
accurately positioned before treatment delivery (9). The image alignment system of the
Tomotherapy Hi-Art system relies solely on megavoltage CT image
guidance. The soft-tissue contrast of these images is inferior to
that of MRI, making it infeasible to perform online adaptive
radiotherapy and track tumors that undergo substantial position
changes during treatment (12).
Case report
In October 2021, a 76-year-old man with neither a
family history of illness nor any unhealthy habits presented to
their local medical doctor (Pintung, Taiwan) with symptoms of
diarrhea and tarry feces that had persisted for a month. The
performance status was assessed as 1 based on the Eastern
Cooperative Oncology Group guidelines (13). Upon a blood examination, which
showed low hemoglobin levels, the attending physician referred the
patient to Antai Medical Care Coorperation Antai Tian-Sheng
Memorial Hospital (Pintung, Taiwan) for colonoscopy. A diagnosis of
moderately differentiated adenocarcinoma, a type of sigmoid colon
cancer, was made. Abdominal CT 1 day later revealed the sigmoid
colon tumor and suspected metastasis to the abdominal lymph nodes
(LNs) and the right lower lobe in the lung. Thus, the cancer was
categorized as clinical stage cT4aN2bM1a, stage 4A cancer (American
Joint Committee on Cancer 8th edition) (14). After being told the examination
result, the patient came to Kaohsiung Medical University Hospital
(Kaohsiung, Taiwan). Nearly 1 month later in November 2021, a
subsequent colonoscopy confirmed the malignancy through a pathology
report, noting that the distance of the tumor from the anal verge
was 17 cm. Given the large size of the tumor (7.2 cm) and visceral
peritoneum invasion, which posed challenges to safe resection, the
medical team chose to administer preoperative neoadjuvant
chemotherapy and radiotherapy. The chosen chemotherapy regimen was
12 cycles of FOLFIRI (180 mg/m2 Campto + 2,800
mg/m2/48 h 5-FU) + Erbitux (500 mg/m2/once
every 2 weeks). Radiotherapy commenced in December 2021. As the
treatment was for local advanced stage cancer, the prescribed dose
was 50 Gy, delivered in 2-Gy daily fractions. Initially, the
Tomotherapy Hi-Art system was selected for treatment. However,
during the megavoltage CT image guidance for the first six
fractions, it was observed that the location of the tumor had
changed by itself, exceeding the range of the PTV. This
displacement rendered other control methods ineffective. After the
first fraction, a CT re-simulation was arranged to correct the
treatment; however, this was unsuccessful. Consequently, the
decision was eventually made by the patient to switch to the
MRIdian system for treatment, starting at the seventh fraction. The
MRIdian system allowed for the performance of an online adaptive
treatment plan, using real-time image and target tracking functions
during dose delivery to ensure minimal differences in the treatment
target position. Both MRI and CT were used for simulation
positioning before treatment. The MRI simulation scan was conducted
using the MRIdian system, with bladder protection achieved by
maintaining a full bladder (the patient emptied the bladder and
drank 300 ml water 30 min before treatment). The MRI magnetic field
strength was 0.35 T, and the image sequence was captured using true
fast imaging with steady-state free precession, scanning a field of
view of 40×43×40 cm for 128 sec. The image quality sufficed for
radiation oncologists to delineate targets, including critical
organs, without the need for fiducial markers or contrast medium.
CT images were aligned with MRI to obtain electron density for
treatment planning calculations. The gross tumor volume (GTV) was
defined as visible lesions on the MRI simulation image. Margins of
3 mm were used for both the clinical target volume of GTV and the
PTV high (PTVH). The PTV median encompassed the regional LNs
(Fig. 1). Treatment began on
December 3, 2021, with six fractions of radiotherapy performed
using the Tomotherapy Hi-Art system, followed by the remaining 19
fractions using the MRIdian system, and was completed on December
14, 2021. The transition between the two technologies was seamless,
and the positioning of the patient remained constant throughout the
treatment process.
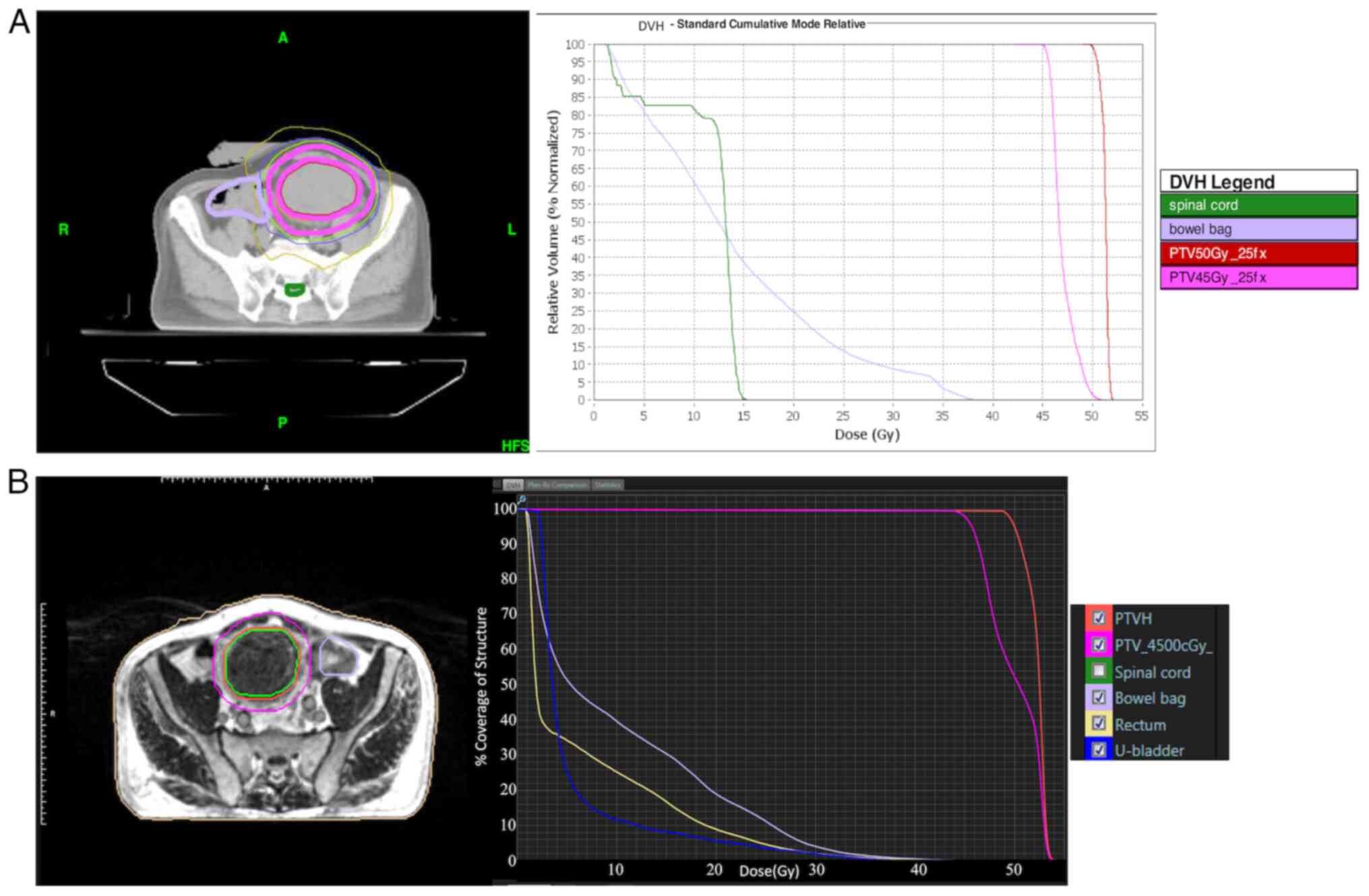
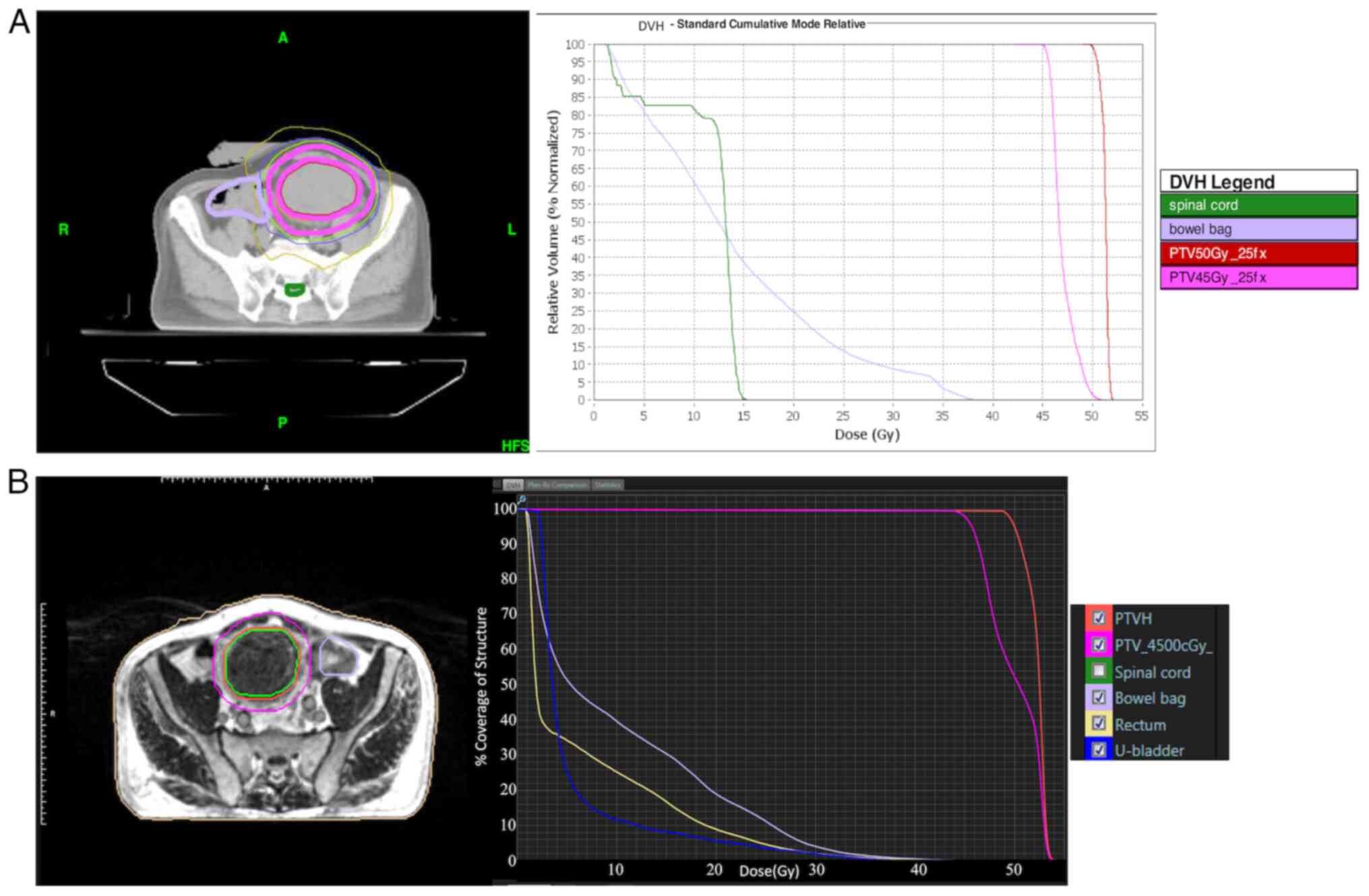 | Figure 1.Simulation images based on treatment
plan. (A) Treatment plan, including contour and DVH, using the
Tomotherapy Hi-Art system. (B) Treatment plan, including contour
and DVH, using the MRIdian system. DVH, dose-volume histogram; fx,
fractions; HFS, head-first supine; PTV, planning target volume;
PTVH, PTV high; PTVM, PTV median; U-bladder, urinary bladder. |
The MRI procedure during treatment was consistent
with that used during the simulation positioning phase. After
aligning the image, the radiation oncologists delineated the target
volume and critical organs as required by the situation, and they
reoptimized the treatment plan through daily Monte Carlo
calculations. Following dose calculation, a comparative evaluation
was conducted between the original plan and the reoptimized plan
with regard to their respective advantages and disadvantages. The
plan used step-and-shoot IMRT, using a 6 MV flattening filter free
beam and a dose rate of 600 MU/min. Comprising 13 angles and 123
segments, a total dose of 50 Gy was prescribed in 2 Gy daily
fractions. Throughout the treatment process, slight changes
occurred in the number of segments, target volume and dose volume
of critical organs due to the implementation of the adaptive
treatment plan. These changes were verified using online Monte
Carlo calculations and gamma comparisons at 2%/2 mm locally, with a
gamma pass rate >90% as the acceptance standard. Before
delivery, the target tracking function was activated, and images
were captured continually in the sagittal view at a rate of 8
frames per sec. The GTV was used as the tracking structure, with
the boundary defined by the PTV. If the GTV exceeded 5% of the PTV,
treatment was halted and resumed only when the target returned to
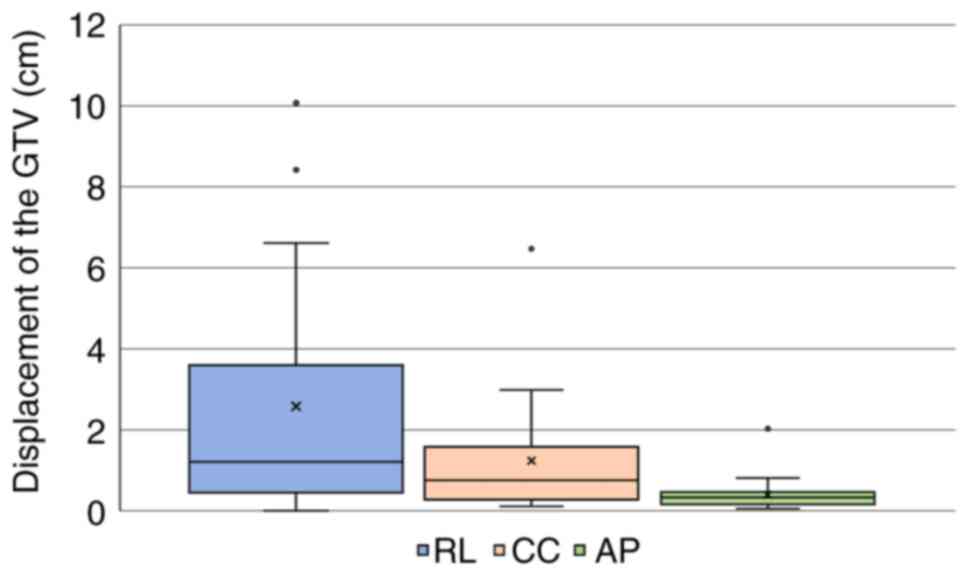
within 5% of the PTV. In the present case, it was observed that the
position of tumor varied from the image captured during each
MRIdian system treatment, and the distance between the three axes
and the original position in the 19 fractions was presented in a
box plot. The mean distance of the shifts in the right-left
direction was 2.58 cm (range, 0–10.07 cm), the mean distance of the
shifts in the cranial-caudal direction was 1.24 cm (range,
0.11-6.47 cm) and the mean distance of the shifts in the
anterior-posterior direction was 0.40 cm (range, 0.06-2.03 cm)
(Fig. 2). The workflow and the time
spent for MRIdian system treatment were as follows: Patient setup
took a mean time of 4 min (range, 2–8 min), simulation and image
fusion took a mean time of 10 min (range, 7–13 min), online
contouring took a mean time of 9 min (range, 4–18 min),
reoptimization took a mean time of 4 min (range, 3–7 min), delivery
took a mean time of 11 min (range, 10–15 min) and patient exit from
the treatment room took a mean time of 3 min (range, 2–4 min). The
mean time from the entry of the patient to treatment completion was
41 min (range, 33–52 min). Adaptive treatment plans were performed
in each of the 19 fractions, with two treatments repeated due to
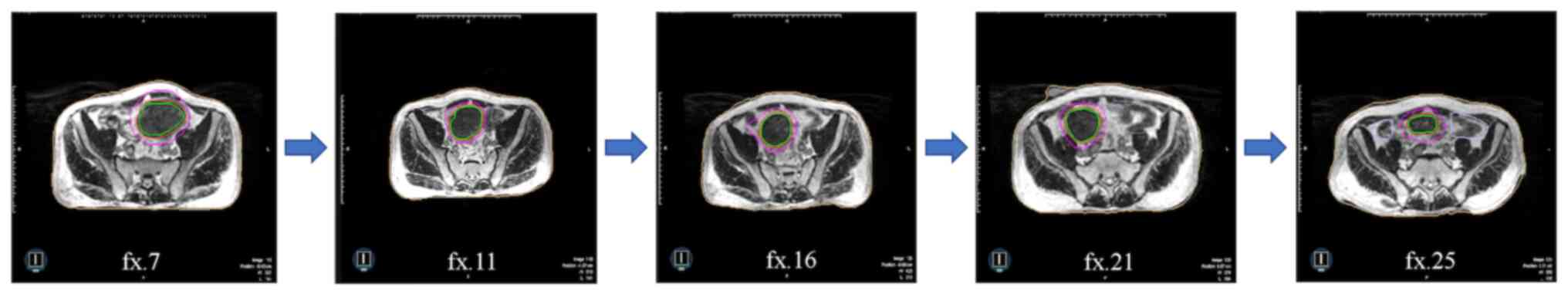
the tumor being out of tracking range. After irradiation with the
MRIdian system, the GTV shrank by 62% (Fig. 3) and the PTVH shrank by 57%. During
the treatment course, the patient experienced no side effects.
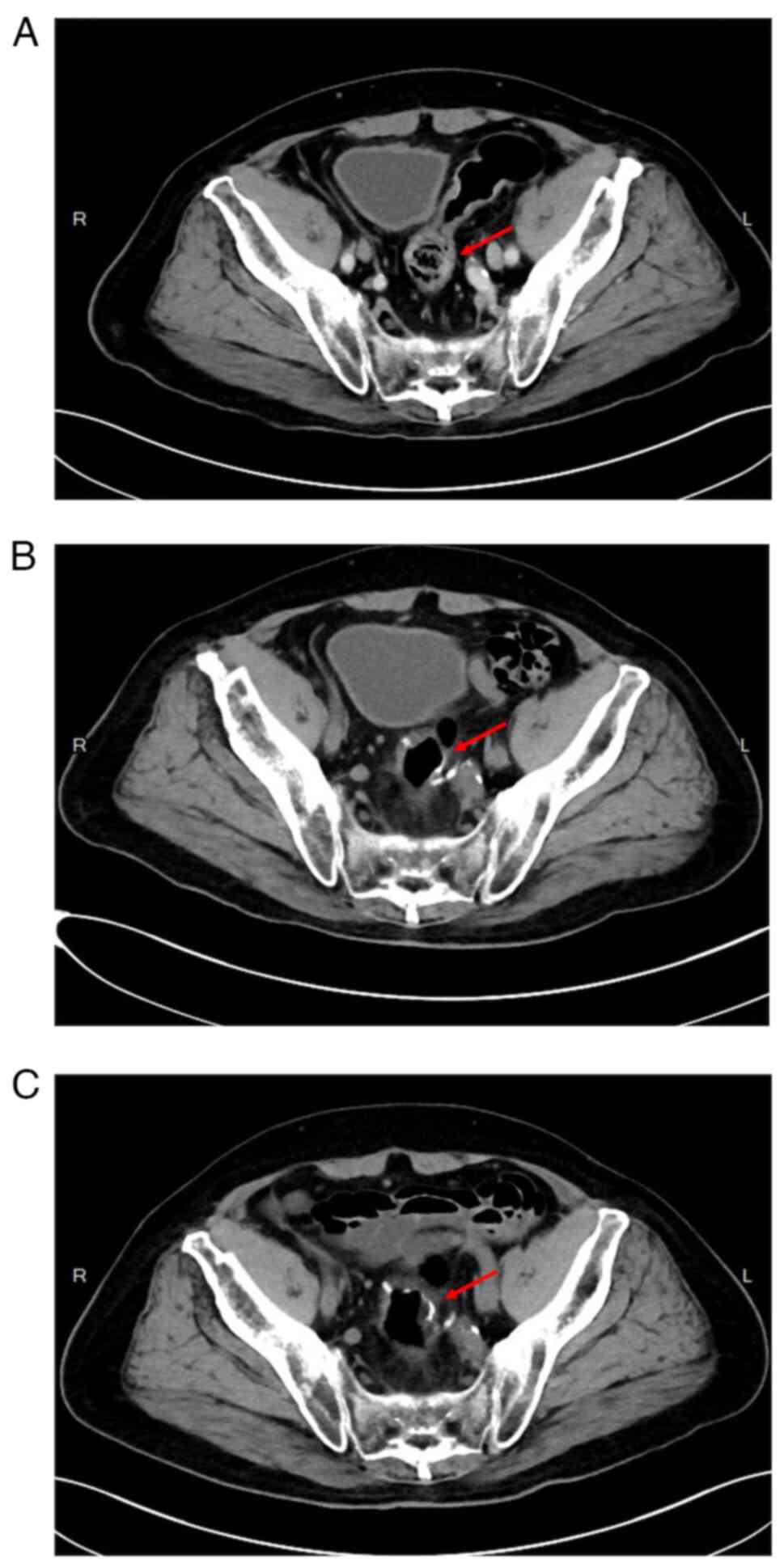
Treatment concluded on January 2022, spanning 41 days. A subsequent
CT scan in April 2022 revealed a marked reduction in tumor size,
categorized as a partial response (Response Evaluation Criteria in
Solid Tumours Version 1.1) (15)
(Fig. 4A), leading to the
scheduling of a low anterior resection in May 2022. The operation
lasted 5 h and 10 min, with blood loss of 50 ml, and proceeded
without complications. The total hospital stay was 19 days, and the
postoperative pathological report stage was ypT3N0 (American Joint
Committee on Cancer 8th edition) (14). Following surgery, a thoracoscopic
examination of the right lower lung was performed in November 2022,
revealing no evidence of malignancy in the pathological report. A
CT scan in November 2022 (Fig. 4B)
and April 2023 (Fig. 4C) indicated
no local recurrence at the surgical bed region. The patient is
currently alive without discomfort.
Discussion
Colorectal cancer is the third most common cancer
worldwide, and the application of neoadjuvant chemoradiotherapy for
locally advanced colon cancer is a common practice in Kaohsiung
Medical University Hospital in Kaohsiung, Taiwan; however,
clinically published cases of neoadjuvant chemoradiotherapy for
locally advanced colon cancer are limited (2). The focus of the present report were
the benefits of the online daily adaptive treatment plan using the
MRIdian system for patients, including reduced toxicity and full
coverage of the target by the PTV. Concerns regarding the process
of neoadjuvant chemoradiotherapy, whether for rectal or colon
cancer, typically center on excessive toxicity (16,17).
However, the present case demonstrated that the patient did not
experience any discomfort attributable to radiotherapy during the
treatment process.
When evaluating the overall duration of treatment,
the scarcity of clinical case reports of colon cancer necessitates
the use of rectal cancer cases with similar tumor locations as
reference points. Intven et al (18) reported rectal cancer treatment
involving five fractions with a total dosage of 25 Gy, resulting in
an mean total treatment time of 48 min, which was comparable to the
treatment time of the present case. Additionally, de Jong et
al (19) found that the
majority of patients with rectal cancer require ~40 min of
treatment. The mean total treatment time was 41 min for the present
case, reinforcing the feasibility of using the MRIdian system to
treat sigmoid colon cancer.
Compared with the image quality of cone beam CT
(CBCT) scans, the 0.35 T MRI of the MRIdian system potentially
offers superior soft tissue contrast, thereby enhancing the
accuracy of contouring (12). This
quality makes online adaptive radiation therapy an alternative to
CBCT imaging (20).
Abdominal organs frequently shift position during
treatment due to factors such as respiration or organ volume
transformation (21,22). Although methods such as breathing
control, compression and fasting can manage these shifts,
particularly in the upper abdomen, control of the colon to the
lower abdomen is less frequently addressed. At present, no
effective control method exists, making daily adaptive treatment
plans with tumor tracking preferable for colon cancer surgery
(23).
In the present case, the Tomotherapy Hi-Art system
was initially used for treatment, and the plan was to select the
treatment strategy and reposition to accommodate changes in tumor
position. However, the irregular movement of the tumor rendered the
chosen treatment plan ineffective. Thus, the patient was
transitioned to the MRIdian system for treatment with an online
adaptive treatment plan (24). The
tumor consistently decreased in size throughout the treatment
period, ultimately shrinking by 62%. If the treatment plan was not
adapted, the PTV covering an excess volume of normal organ could
lead to toxicity. Based on the outcomes in the present case, the
implementation of an adaptive treatment plan with the MRIdian
system was deemed feasible for locally advanced sigmoid colon
cancer in neoadjuvant chemoradiotherapy. At present, studies
related to radiotherapy for colon cancer are rare, and this case
may be the first clinical published case using the MRIdian system
with adaptive plan. The present case report contributes valuable
insights and may serve as a reference for future treatment of
locally advanced sigmoid colon cancer.
Acknowledgements
Not applicable.
Funding
The present study received funding from Kaohsiung Medical
University Hospital planning (grant no. KMUH111-M102).
Availability of data and materials
The datasets generated and/or analyzed during the
current study are not publicly available to protect the privacy of
the individual concerned but are available from the corresponding
author on reasonable request.
Authors' contributions
CHC, TYC and MYH contributed to the conception and
design of the study. CHC performed the statistical analysis and
drafted the initial manuscript. CHC, TYC and MYH wrote sections of
the manuscript. CHC and TYC confirm the authenticity of all the raw
data. All authors were actively involved in manuscript revision.
All authors have read and approved the final version of the
manuscript.
Ethics approval and consent to
participate
The study received approval from the Kaohsiung
Medical University Chung-Ho Memorial Hospital Institutional Review
Board [Kaohsuing, Taiwan; approval no. KMUHIRB-E(I)-20230082].
Patient consent for publication
Based on the study being a retrospective study and a
routine medical treatment, after institutional review board review,
the requirement for a subject consent form was waived, so an
informed consent form was not obtained from the patient.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Sung H, Ferlay J, Siegel RL, Laversanne M,
Soerjomataram I, Jemal A and Bray F: Global cancer statistics 2020:
GLOBOCAN estimates of incidence and mortality worldwide for 36
cancers in 185 countries. CA Cancer J Clin. 71:209–249. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Krishnamurty DM, Hawkins AT, Wells KO,
Mutch MG, Silviera ML, Glasgow SC, Hunt SR and Dharmarajan S:
Neoadjuvant radiation therapy in locally advanced colon cancer: A
cohort analysis. J Gastrointest Surg. 22:906–912. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hohenberger W, Weber K, Matzel K,
Papadopoulos T and Merkel S: Standardized surgery for colonic
cancer: Complete mesocolic excision and central ligation-technical
notes and outcome. Colorectal Dis. 11:354–365. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Gao Z, Wang C, Cui Y, Shen Z, Jiang K,
Shen D, Wang Y, Zhan S, Guo P, Yang X, et al: Efficacy and safety
of complete mesocolic excision in patients with colon cancer:
Three-year results from a prospective, nonrandomized, double-blind,
controlled trial. Ann Surg. 271:519–526. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Buckley JG, Dowling JA, Sidhom M, Liney
GP, Rai R, Metcalfe PE, Holloway LC and Keall PJ: Pelvic organ
motion and dosimetric implications during horizontal patient
rotation for prostate radiation therapy. Med Phys. 48:397–413.
2021. View
Article : Google Scholar : PubMed/NCBI
|
|
6
|
Mahantshetty U, Naga P, Nachankar A, Ghadi
Y, Dheera A, Scaria L, Epili D, Chopra S, Lavanya G and Shrivastava
S: Set-up errors, organ motion, tumour regression and its
implications on internal target volume-planning target volume
during cervical cancer radiotherapy: Results from a prospective
study. Clin Oncol (R Coll Radiol). 34:189–197. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Shortall J, Vasquez Osorio E, Cree A, Song
Y, Dubec M, Chuter R, Price G, McWilliam A, Kirkby K, Mackay R and
van Herk M: Inter- and intra-fractional stability of rectal gas in
pelvic cancer patients during MRIgRT. Med Phys. 48:414–426. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Benson AB III, Arnoletti JP, Bekaii-Saab
T, Chan E, Chen YJ, Choti MA, Cooper HS, Dilawary RA, Engstrom PF,
Enzinger PC, et al: Colon cancer. J Natl Compr Canc Netw.
9:1238–1290. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Liney GP, Whelan B, Oborn B, Barton M and
Keall P: MRI-linear accelerator radiotherapy systems. Clin Oncol (R
Coll Radiol). 30:686–691. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Avgousti R, Antypas C, Armpilia C,
Simopoulou F, Liakouli Z, Karaiskos P, Kouloulias V, Kyrodimos E,
Moulopoulos LA and Zygogianni A: Adaptive radiation therapy: When,
how and what are the benefits that literature provides? Cancer
Radiother. 26:622–636. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Nierer L, Eze C, da Silva Mendes V, Braun
J, Thum P, von Bestenbostel R, Kurz C, Landry G, Reiner M, Niyazi
M, et al: Dosimetric benefit of MR-guided online adaptive
radiotherapy in different tumor entities: Liver, lung, abdominal
lymph nodes, pancreas and prostate. Radiat Oncol. 17:532022.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wen N, Cao Y and Cai J: Editorial:
Magnetic resonance imaging for radiation therapy. Front Oncol.
10:4832020. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Oken MM, Creech RH, Tormey DC, Horton J,
Davis TE, McFadden ET and Carbone PP: Toxicity and response
criteria of the eastern cooperative oncology group. Am J Clin
Oncol. 5:649–656. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Weiser MR: AJCC 8th edition: Colorectal
cancer. Ann Surg Oncol. 25:1454–1455. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Eisenhauer EA, Therasse P, Bogaerts J,
Schwartz LH, Sargent D, Ford R, Dancy J, Arbuck S, Gwyher S, Mooney
M, et al: New response evaluation criteria in solid tumours:
Revised RECIST guideline (version 1.1). Eur J Cancer. 45:228–247.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Tam SY and Wu VWC: A review on the special
radiotherapy techniques of colorectal cancer. Front Oncol.
9:2082019. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Sauer R, Fietkau R, Wittekind C, Rödel C,
Martus P, Hohenberger W, Tschmelitsch J, Sabitzer H, Karstens JH,
Becker H, et al: Adjuvant vs neoadjuvant radiochemotherapy for
locally advanced rectal cancer: The German trial CAO/ARO/AIO-94.
Colorectal Dis. 5:406–415. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Intven MPW, de Mol van Otterloo SR, Mook
S, Doornaert PAH, de Groot-van Breugel EN, Sikkes GG,
Willemsen-Bosman ME, van Zijp HM and Tijssen RHN: Online adaptive
MR-guided radiotherapy for rectal cancer; feasibility of the
workflow on a 1.5T MR-linac: Clinical implementation and initial
experience. Radiother Oncol. 154:172–178. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
de Jong R, Visser J, van Wieringen N,
Wiersma J, Geijsen D and Bel A: Feasibility of Conebeam CT-based
online adaptive radiotherapy for neoadjuvant treatment of rectal
cancer. Radiat Oncol. 16:1362021. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Klüter S: Technical design and concept of
a 0.35 T MR-Linac. Clin Transl Radiat Oncol. 18:98–101.
2019.PubMed/NCBI
|
|
21
|
Ozhasoglu C and Murphy MJ: Issues in
respiratory motion compensation during external-beam radiotherapy.
Int J Radiat Oncol Biol Phys. 52:1389–1399. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Abbas H, Chang B and Chen ZJ: Motion
management in gastrointestinal cancers. J Gastrointest Oncol.
5:223–235. 2014.PubMed/NCBI
|
|
23
|
de Jong R, Visser J, Crama KF, van
Wieringen N, Wiersma J, Geijsen ED and Bel A: Dosimetric benefit of
an adaptive treatment by means of plan selection for rectal cancer
patients in both short and long course radiation therapy. Radiat
Oncol. 15:132020. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Keall PJ, Mageras GS, Balter JM, Emery RS,
Forster KM, Jiang SB, Kapatoes JM, Low DA, Murphy MJ, Murray BR, et
al: The management of respiratory motion in radiation oncology
report of AAPM Task Group 76. Med Phys. 33:3874–3900. 2006.
View Article : Google Scholar : PubMed/NCBI
|