Introduction
Lung cancer is the most frequently diagnosed cancer
with an estimated 2.20 million new cases and is the leading cause
of cancer-related deaths with 1.79 million deaths worldwide
(1). Gefitinib is an oral epidermal
growth factor receptor tyrosine kinase inhibitor (EGFR-TKI),
recommended as the first-choice treatment for patients with
advanced stage disease (2), and was
associated with a significantly higher frequency of grade 3 or
greater hepatotoxicity than the other EGFR-TKIs, erlotinib or
afatinib, although severe rash and diarrhea were less frequent than
afatinib (3). Drug-induced
hepatotoxicity is one of the major causes of approved drugs being
removed from the market (4).
Human induced pluripotent stem cells (iPSCs) have
opened new doors in biology and regenerative medicine (5). One advantage of iPSCs is that they can
be generated from human tissues of subjects with genetic variations
or various traits, such as drug sensitivity (6,7).
Remodeling the pathogenesis, iPSCs have been generated for various
diseases, such as severe combined immunodeficiency (ADA-SCID)
(8), type 1 diabetes (9), and Parkinson's disease (10). iPSCs could be also an ideal platform
for drug discovery or evaluation (11).
Various protocols for hepatic-differentiation from
iPSCs have been developed (12–15).
Despite differences among iPSC-derived hepatocytes (iPSC-heps),
hepatocyte cell lines, and primary hepatocytes (16,17),
iPSC-heps have been shown to have the potential to predict drug
toxicity and improve drug screening (7,18,19).
In this study, we generated iPSCs by reprogramming
peripheral blood mononuclear cells (PBMC) obtained from 2 groups of
gefitinib-treated patients who either had grade 3 or greater
hepatotoxicity (Toxicity group, T) or grade 1 or less
hepatotoxicity (No clinical toxicity group, N) in the Common
Terminology Criteria for Adverse Events (CTCAE v5.0). iPSCs were
differentiated into hepatocytes (iPSC-heps). We examined
gefitinib-induced cytotoxicity in both iPSCs and iPSC-heps from
both the T and N groups and evaluated the correlation between in
vitro cytotoxicity and clinical hepatocytotoxicity to compare
the cells from both groups.
Materials and methods
Antibodies
Anti-EGFR antibodies (sheep polyclonal,
Upstate®, Merck, Darmstadt, DE), phospho-EGFR (Y1068)
[mouse monoclonal (m), Abcam, Cambridge, UK], GAPDH (m, MBL,
Nagoya, Japan), human albumin (goat polyclonal, Bethyl
Laboratories, Montgomery, TX), α-fetoprotein [rabbit monoclonal (r,
mAb), Abcam, Cambridge, UK], and hepatocyte nuclear factor 4 alpha
(HNF4α) (r, mAb, Abcam, Cambridge, UK) were used for our
experiments.
Generation of iPSCs
Peripheral blood mononuclear cells (PBMCs)
culture and Reprogramming
iPSCs were established according to the protocol
described by Okita et al (20) with minor modifications. Peripheral
blood was obtained from the patients according to the Osaka Medical
and Pharmaceutical University Review Board's guidelines. PBMCs were
isolated using a BD Vacutainer®CPT™
mononuclear cell preparation tube with sodium citrate (BD
Biosciences, Franklin Lakes, NJ, USA), according to the
manufacturer's instructions. Half of the collected cells were
suspended in a STEM-CELL Banker® (ZENOEN PHARMA,
Fukushima, Japan), aliquoted into cryovials at
>2.5×106 cells/500 µl/vial, frozen, and stored at
−80°C. The rest of the cells were plated in 6-well plates in PBMC
culture medium: Stem Span-ACF (STEMCELL Technologies, Vancouver,
BC, Canada) with 10 ng/ml IL-3, 100 ng/ml IL-6, 300 ng/ml SCF, 300
ng/ml TPO, and 300 ng/ml Flt3 ligand, and cultured for 1 week with
more medium added as appropriate. Unless otherwise stated,
cytokines were purchased from FUJIFILM Wako Pure Chemical Corp.
(Osaka, Japan).
The plasmids pCXLE-hOCT3/4-shp53-F, pCXLE-hSK,
pCXLE-hUL, and pCXLE-EBANA required for reprogramming were
electroporated into 3–5×106 PBMCs using a Nucleofector
2b Device (Lonza, Basel, Switzerland) with an Amaxa human
CD34+ cell Nucleofector kit (Lonza, Basel, Switzerland)
according to the manufacturer's instructions. The transfected cells
were transferred into iMatrix 511 silk (TaKaRa, Shiga,
Japan)-coated 6-well plates in PBMC culture medium using a
sequential dilution. The PBMC medium was replaced with Stem Fit
AK03N w/o C solution (Ajinomoto, Tokyo, Japan) by adding 1.5 ml of
Stem Fit every other day, three times. The medium was replaced with
Stem Fit w/o C solution on the eighth day of culture. The cells
were cultured continuously, and iPSC colonies were picked when they
were approximately 1 mm in diameter. The iPSCs reprogramed from
patients (iPSCs) were used for further characterization.
iPSC culture
iPSCs were cultured in a feeder-free system.
Briefly, 6-well plates were pre-incubated in 1.5 ml/wells of Stem
Fit AK03N (Ajinomoto, Tokyo, Japan) containing 0.25% iMatrix 511
silk (TaKaRa, Shiga, Japan) and 10 µM Y-27632, a rho-associated
coiled-coil kinase (ROCK) inhibitor (FUJIFILM Wako Pure Chemical
Corp., Osaka, Japan), in a CO2 incubator. iPSCs
(1–1.4×104 cells), suspended in 500 µl of Stem Fit AK03N
(Ajinomoto, Tokyo, Japan) and then plated onto a pre-incubated
6-well plates. The following day, the medium was replaced with Stem
Fit AK03N (Ajinomoto, Tokyo, Japan) alone and changed every other
day.
iPSC passage
At confluency, iPSCs were washed twice with PBS
(FUJIFILM Wako Pure Chemical Corp., Osaka, Japan) and incubated
with Accutase™ (Innovative Cell Technologies, Inc., San
Diego, CA) for approximately 5 min at 37°C, after which the
supernatant was removed. The cells were washed with PBS, suspended
in Stem Fit AK03N (Ajinomoto, Tokyo, Japan), and counted using an
automated cell counter (TC20, Bio-Rad, Hercules, CA, USA). The
cells were cultured as described above.
Hepatocyte differentiation of
iPSC
iPSCs were plated at 60–80% of confluence with 1
ml/well of Stem Fit AK03N (Ajinomoto, Tokyo, Japan) containing
0.25% iMatrix 511 silk (TaKaRa, Shiga, Japan) and 10 µM Y-27632 in
a 12-well plate. Hepatic differentiation was performed using 4-step
protocol. (STAGE 1) The next day, the medium was changed to
RPMI1640 (Thermo Fisher Scientific, Waltham, MA) with 2% B27
(Thermo Fisher Scientific, Amarillo, TX) with insulin, 75 ng/ml
Activin A (FUJIFILM Wako Pure Chemical Corp., Osaka, Japan), 3 µM
CHIR99021 (FUJIFILM Wako Pure Chemical Corp., Osaka, Japan), GSK3β
inhibitor, and 10 µM LY294002 (FUJIFILM Wako Pure Chemical Corp.,
Osaka, Japan), PI3K inhibitor. The cells were then incubated for 5
days and the medium changed daily. (STAGE 2) The medium was
replaced with RPMI1640 (Thermo Fisher Scientific, Waltham, MA)
containing 2% B27 (Thermo Fisher Scientific, Amarillo, TX) with
insulin, 10 ng/ml BMP4 (FUJIFILM Wako Pure Chemical Corp., Osaka,
Japan), and 10 ng/ml FGF2 (FUJIFILM Wako Pure Chemical Corp.,
Osaka, Japan). The cells were then incubated for 5 days and the
medium changed daily. (STAGE 3) At day 11, the cells were incubated
with RPMI1640 (Thermo Fisher Scientific, Waltham, MA) containing 2%
B27 (Thermo Fisher Scientific, Amarillo, TX) with insulin, and 20
ng/ml HGF (FUJIFILM Wako Pure Chemical Corp., Osaka, Japan) for 5
days with daily medium change. (STAGE 4). On day 16, the medium was
again replaced with RPMI1640 (Thermo Fisher Scientific, Waltham,
MA) containing 2% B27 (Thermo Fisher Scientific, Amarillo, TX) with
insulin, 20 ng/ml Oncostatin M (FUJIFILM Wako Pure Chemical Corp.,
Osaka, Japan) for a further 5 days with daily medium change, after
which the iPSC-derived hepatocytes (iPSC-heps) were
characterized.
HaCaT cells culture
HaCaT cells, an immortalized human keratinocyte cell
line, obtained from COSMO BIO CO., Ltd. (300493-ACADEMIC) were
cultured in MCDB 153 medium containing 5% FBS and 10 µg epidermal
growth factor (FUJIFILM Wako Pure Chemical Corp., Osaka, Japan). To
collect the cell lysates, the cells were grown until they reached
80–100% confluence.
Western blot analysis
The samples were prepared with RIPA buffer and
quantified using a Pierce™ BCA Protein Assay Kit (Thermo
Fisher Scientific, Waltham, MA). The quantified samples were
electrophoresed and electroblotted using a semi-dry system
(Trans-Blot SD Semi-Dry Transfer cell, Bio-Rad, Hercules, CA, USA)
onto a PVDF membrane (Merck Millipore, Burlington, MA). The
membrane was then incubated with the appropriate primary antibodies
followed by HRP-conjugated anti-mouse or -rabbit secondary
antibodies (SouthernBiotech, Birmingham, AL) and developed using
Luminata™ Crescendo (Merck Millipore, Burlington, MA).
The images were captured using a FUSION SYSTEM FX7 (VILBER LOURMAT,
Marne-la-Vallée Cedex 3, France).
qPCR analysis
Total RNA was prepared using the
RNAzol®RT Reagent (Molecular Research Center, Inc.,
Cincinnati, OH, USA) and then transcribed into cDNA with a
PrimeScript™ RT reagent kit (Perfect Real Time) (TaKaRa,
Shiga, Japan), 1 µg of total RNA. TaqMan® probes for
AFP (Hs01040598_m1), ALB (Hs00609411_m1),
NANOG (Hs02387400_g1), and POU5F1 (Hs04260367_gH)
were obtained from Thermo Fisher Scientific (Waltham, MA), and qPCR
was performed using the StepOnePlus real-time PCR system (Thermo
Fisher Scientific, Waltham, MA). The data were analyzed using the
ΔΔCq method and expressed as relative quantities (RQ) according to
the manufacturer's instructions.
Lactate dehydrogenase (LDH) release
assay
iPSCs were plated in Stem Fit AK03N (Ajinomoto,
Tokyo, Japan) containing 0.25% iMatrix 511 silk (TaKaRa, Shiga,
Japan) and 10 µM Y-27632 (FUJIFILM Wako Pure Chemical Corp., Osaka,
Japan) in a 12-well plate. as described above. The following day,
the medium was replaced with Stem Fit AK03N (Ajinomoto, Tokyo,
Japan) containing gefitinib (0, 3, 6, and 10 µM). The medium was
collected on days 0, 1, and 2. The medium was not replaced during
gefitinib treatment. For iPSC-heps, gefitinib (0, 3, 6, and 10 µM)
was added on day 2 of STAGE 4, and the conditioned medium and iPSCs
were collected. LDH was measured using the LDH-Glo™
Cytotoxicity Assay combined with the GloMax Multi/Luminescence
System (Promega, Madison, WI, USA) according to the manufacturer's
instructions.
Statistical analysis
All analyses were performed using ‘MEPHAS’
(http://www.gen-info.osaka-u.ac.jp/testdocs/tomocom/).
One-way ANOVA with Dunnett's test or Tukey's test, and Student's-t
test were employed for statistical analyses. P<0.05 was
considered to indicate a statistically significant difference.
Results
Generation of iPSCs and iPSC-heps
To prevent dose reduction or cessation of gefitinib
treatment caused by hepatotoxicity, it is important to establish a
cell-based assay system that can predict gefitinib-induced toxicity
before clinical use. We hypothesized that iPSC-heps may predict
gefitinib-induced hepatotoxicity in vitro and thus generated
iPSCs from two groups of gefitinib-treated patients, those with
grade 3 or greater hepatotoxicity (T group), and those who had
grade 1 or less hepatotoxicity (N group) in the CTCAE v5.0. iPSCs
were generated from 6 patients, 3 each from T and N groups. The
patient characteristics are displayed in Table SI. We established 3 clones from a
patient and got 18 clones in total. To confirm the pluripotency, we
examined the mRNA expression levels of POU5F1 and
NANOG, stem cell markers, showing that the clones were in a
pluripotent state (Fig. 1A). In
addition, the other stem cell markers, alkaline phosphatase (ALP)
and SOX2, were highly expressed in the clones, whereas they were
barely detected in the differentiated cells, HaCaT cells, in
western blot analyses (Fig. S1).
Since all clones were in a pluripotent state, we randomly chose 1
clone from each of the patients (6 clones), and was subjected to
further analysis including the cyto/hepatotoxicity assay. We then
differentiated iPSCs into iPSC-heps. A qPCR analysis showed that
the expression levels of AFP and ALB,
hepatocyte-specific markers, in iPSC-heps were much higher than
those in iPSCs (Fig. 1B). In
contrast, NANOG and POU5F1 were not expressed in
iPSC-heps (Fig. 1A). A western blot
analysis also showed that HNF4α, ALBUMIN (ALB), and AFP,
hepatocyte-specific markers, were comparably expressed in iPSC-heps
(Fig. 1C). These data suggest that
iPSCs had differentiated into cells in a hepatocyte lineage. The
four-step protocol we used for differentiation of iPSCs into
iPSC-heps was depicted in Fig. 2.
Collectively, we concluded that the iPSC clones were successfully
differentiated into the iPSC-heps.
 | Figure 1.Characterization of patient-derived
iPSCs and the iPSC-heps. qPCR analysis of (A) pluripotent makers
and (B) hepatocyte markers in iPSCs and iPSC-heps, N-3 and T-1. The
values represented mean ± SD. POU5F1 and NANOG;
pluripotent makers. AFP and ALB; hepatocyte markers.
(C) Western blot analyses of hepatocyte markers in iPSC-heps, N-3
and T-1. GAPDH was used as a loading control. HNF4α, ALB and AFP;
hepatocyte markers. (D-G) LDH release from patient-derived
iPSC-heps by gefitinib treatment. iPSC-heps from (D) N-1, (E) N-3,
(F) T-1, (G) T-3, were treated with gefitinib at the concentrations
indicated (0, 3, 6, and 10 µM) for 2 days. LDH was measured each
day. Values were calculated and expressed as % of those of positive
control (0.1% Triton treated cell). T, toxicity; N, no toxicity;
iPSCs, induced pluripotent stem cells; iPSC-heps, iPSC-hepatocytes;
qPCR, quantitative PCR; ALB, albumin; LDH, lactate
dehydrogenase. |
Evaluation of hepatotoxicity by
gefitinib via LDH-release assay with iPSC-heps
To evaluate the hepatotoxicity of gefitinib, we
employed a chemiluminescence-based LDH release assay using
iPSC-heps. iPSCs (N-1, N-3, T-1, and T-3) were simultaneously
differentiated into iPSC-heps. Gefitinib (0, 3, 6, and 10 µM) was
administered on day 2 of STAGE 4 (Fig.
2). We confirmed that AFP and ALB, hepatocyte-specific markers,
were already expressed at the beginning of STAGE 4 (data not
shown). As hepatic maturation proceeded, evidence of naturally
dying cells appeared. To differentiate natural cell death from
gefitinib-related cytotoxicity as much as possible, day 2 of STAGE
4 was selected as the starting point. Each iPSC-heps were treated
with 0, 2, 6, and 10 µM gefitinib, and conditioned medium was
collected on days 0, 1, and 2 after administration. However, we
could not find dose- or group (N and T)-dependency (Fig. 1D-G). These data suggest that our
experimental design may need to be improved to be a good platform
for gefitinib-induced hepatotoxicity assays.
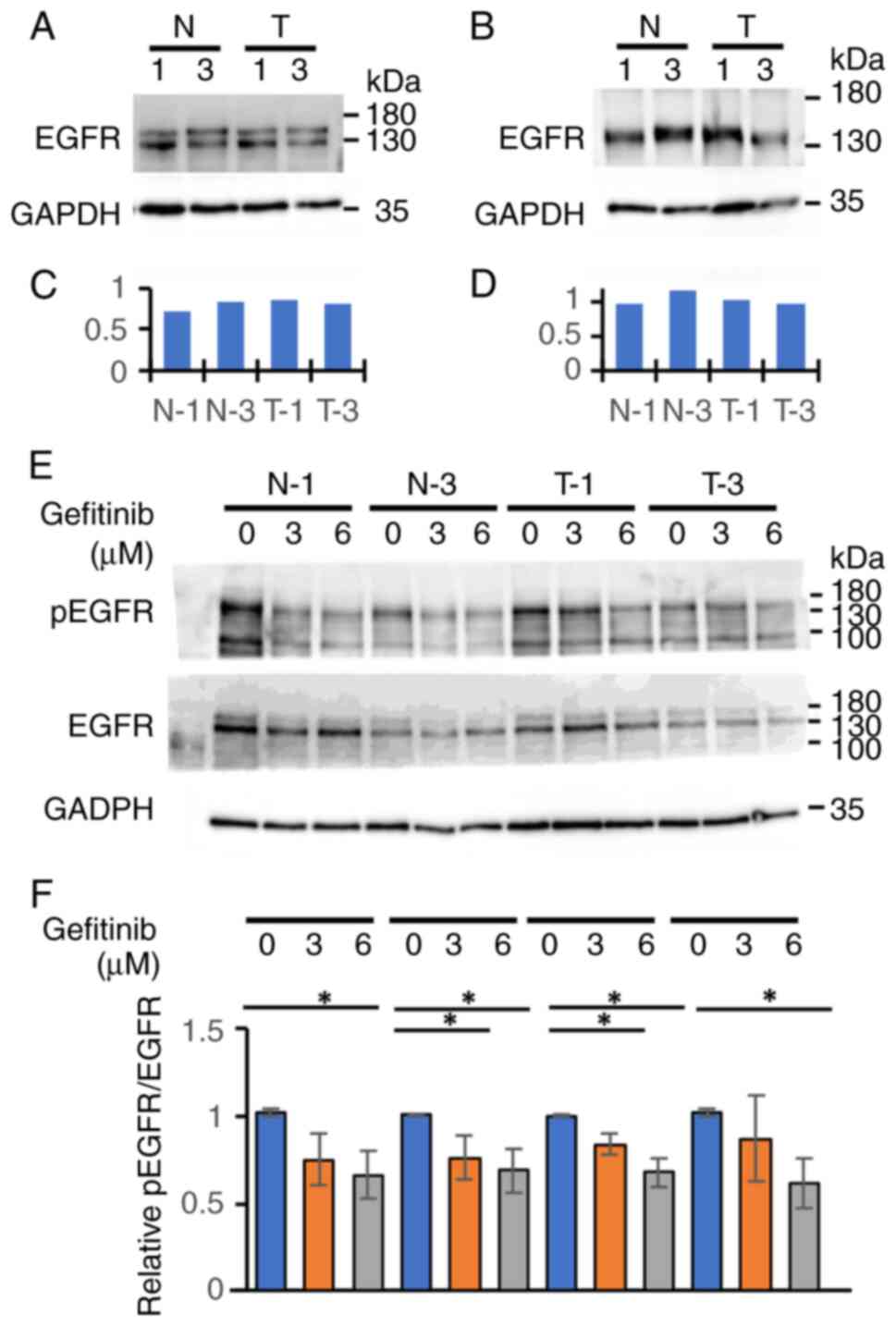
EGFR expression, and the
phosphorylation following gefitinib treatment in the clones of
iPSCs or iPSC-heps from the N or T group
Since gefitinib is an EGFR-TKI, we examined the
expression level of EGFR and the phosphorylation following
gefitinib treatment in the clones of iPSCs and iPSC-heps from the N
or T group. Western blot analyses showed that they were expressed
similarly among the clones of iPSCs (Fig. 3A and C) and iPSC-heps (Fig. 3B and D) from each group,
irrespective of whether those were from the N or T group. EGFR
phosphorylation status (the ratio of pEGFR to EGFR) were also
similar among the clones of iPSCs from the two groups following
gefitinib treatment (Fig. 3E and
F). Although treatment significantly suppressed EGFR
phosphorylation in a dose-dependent manner, we did not find any
differences in phosphorylation status between the two groups
following gefitinib treatment. Fig. 3E
and F shows that gefitinib treatment inhibited the EGFR
signaling pathway equally in each iPSCs. Taken together, an
LDH-release assay using iPSCs would potentially be a good predictor
of gefitinib-induced hepatotoxicity.
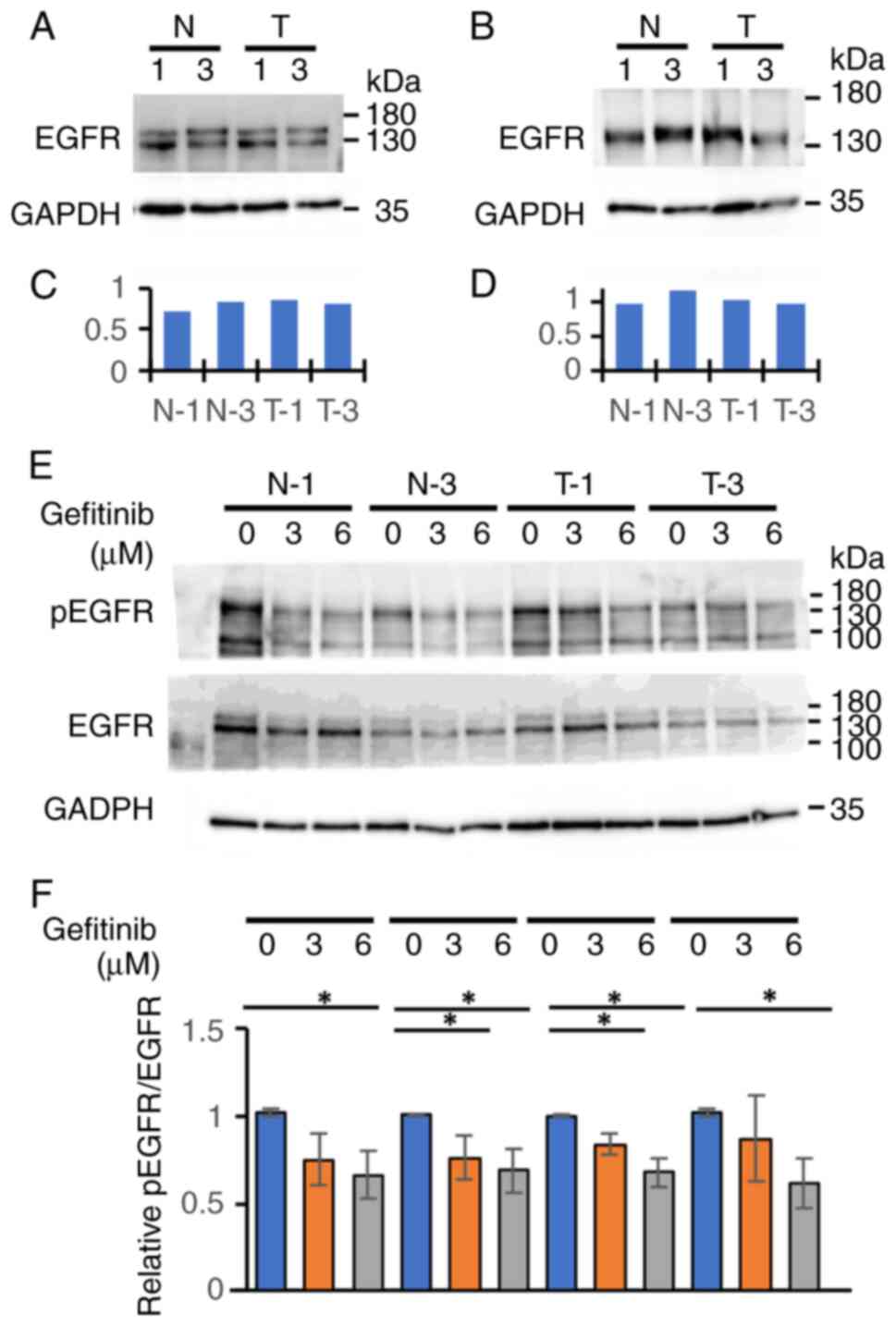 | Figure 3.EGFR expression, and the
phosphorylation following gefitinib treatment in the clones of
patient-derived iPSCs or iPSC-heps from the N or T group. Western
blot analyses of (A) iPSCs and (B) iPSC-heps from the N or T group.
EGFR expression was detected with an anti-EGFR antibody.
Densitometric analysis was performed using ImageJ software for (C)
iPSCs and (D) iPSC-heps. (E) iPSCs were cultured with gefitinib at
indicated concentrations (0, 3, 6 µM) for two days. The cell
lysates were subjected to western blot analysis. EGFR and pEGFR
expressions were detected with their respective antibodies (Upper
panel). GAPDH was used as a loading control. (F) Densitometric
analysis (n=3) was performed using ImageJ software (Lower panel).
The values represented mean ± SD. *P<0.05, Dunnett's test. T,
toxicity; N, no toxicity; EGFR, epidermal growth factor receptor;
pEGFR, phosphorylated EGFR; iPSCs, induced pluripotent stem cells;
iPSC-heps, iPSC-hepatocytes. |
Evaluation of gefitinib-induced
hepatotoxicity via LDH-release assay with iPSCs
While we evaluated the gefitinib-induced
hepatotoxicity with the iPSC-heps, we used iPSCs as a control in
the assays. We found that iPSCs in T group released LDH more than
those in N group after gefitinib treatment, and the increase was
dose dependent (Fig. 4A-F). Because
the difference between the groups at day 1 after gefitinib
treatment seemed to be the largest among the time points analyzed,
we focused on the toxicity at day 1. T-2 was significantly more
sensitive to gefitinib than N-1 after 6 µM gefitinib treatment
(Fig. 4H). There were no
significant differences between the T and N groups in any other
concentrations or combinations except that T-2 was significantly
more sensitive to gefitinib than N-1 after 6 µM gefitinib treatment
(Fig. 4G-I). However, iPSCs in T
group tended to have the cytotoxicity more than those in N group.
Therefore, we combined the data of each group and compared the 2
groups (Fig. 4J-L). The result
showed that iPSCs in T group had higher cytotoxicity than those in
N group after 6 or 10 µM gefitinib treatment (Fig. 4K and L), whereas there were no
significant differences between N and T groups after 3 µM treatment
(Fig. 4J). These results were
consistent with the data of the cell viability assay (Fig. S2) and the cell morphology (Fig. S3). The cell viability in T group at
day 2 after gefitinib treatment was significantly aggravated,
except for T-2 and T-3 at 3 µM and T-2 at 6 µM, whereas no
significant damages were observed in N group, except for N-1 and
N-3 at 10 µM (Fig. S2). In the
cell morphology at day 2 after gefitinib treatment, gefitinib
decreased the number and size of attached iPSCs in the T group in a
dose-dependent manner, whereas no significant damages were observed
in N group, except for N-2 that seemed to be slightly damaged at 10
µM treatment (Fig. S3).
 | Figure 4.LDH release from patient-derived
iPSCs by gefitinib treatment. iPSCs from (A) N-1, (B) N-2, (C) N-3,
(D) T-1, (E) T-2 and (F) T-3, were treated with gefitinib at the
concentrations indicated (0, 3, 6, and 10 µM) for 2 days. LDH was
measured at day 0, 1, and 2, and the values at day 1 and 2 were
shown (at day 0; undetermined). The values were calculated as % of
positive control (0.1% Triton treated cell), expressed as % of
control. (G-I) LDH release of iPSCs at day 1, treated with (G) 3
µM, (H) 6 µM and (I) 10 µM of gefitinib. The values of gefitinib
(−) were regarded as 1. The values represented mean ± SD.
*P<0.05, Tukey's test. (J-L) LDH release of N- and T-group, at
respective gefitinib concentrations, (J) 3 µM, (K) 6 µM and (L) 10
µM, data form each clone was consolidated each group, was
statistically analyzed. The values represented mean ± SD.
**P<0.01, *P<0.05, Student's t-test. T, toxicity; N, no
toxicity; LDH, lactate dehydrogenase; iPSCs, induced pluripotent
stem cells. |
Discussion
Drug-induced hepatotoxicity is a major concern in
drug development and clinical therapy (21,22).
Severe hepatotoxicity caused by gefitinib treatment often leads to
acute/chronic liver injury, drug discontinuation, and further
treatment failure (3,23,24).
To develop preclinical tests to predict hepatotoxicity of
gefitinib, we evaluated a cell-based assay system using iPSCs or
iPSC-heps generated from patients receiving gefitinib therapy. We
first tried iPSC-heps for the gefitinib-induced hepatotoxicity
assay. We estimated the hepatotoxicity by the measurement of LDH
amount released into the culture medium from iPSC-heps. The
hepatotoxicity assay using iPSC-heps did not reflect
gefitinib-induced liver injury in the clinical setting; there were
no significant differences between the 2 groups, although gefitinib
treatment increased LDH release in both groups in a dose- and
time-dependent manner (Fig. 1D-G).
This may be because of the high variability of gefitinib-related
cytotoxicity among the clones in the same group.
We next tried undifferentiated iPSCs for the
cytotoxicity assay. The result showed that iPSCs from the T group
had significantly higher cytotoxicity after gefitinib treatment
than that from the N group (Fig.
4). Although we considered to use cell lines for the positive
determination and feasibility of the assay, we did not try cell
lines for the assay. That is because the reactivity to drugs in
cell lines was quite different from that in primary cultured cells
in our experiences. Taken together, we concluded that the
cytotoxicity of gefitinib on patient-derived-iPSCs reflects
gefitinib-induced liver injury in the clinical setting more than
the hepatotoxicity of gefitinib on patient-derived-iPSC-heps,
showing that iPSCs may have a possibility to become a platform for
preclinical testing to predict gefitinib-induced
hepatotoxicity.
The possibility of applying iPSCs in disease
modeling and drug evaluation has been recently proposed by Sano
et al (2021) (25). They
used iPS cells transfected with ACE2, a SARS-CoV2 receptor
(ACE2-iPS cells) to recapitulate SARS-CoV2 infection and assess
anti-COVID-19 drug sensitivity in a pluripotent state and noticed
that ACE-iPS cells could be infected by the virus, and that the
virus could replicate in the cells. In addition, replication was
strongly inhibited by the approved anti-COVID19 drug, remdesivir,
but not by chloroquine (25),
findings consistent with clinical results (26,27).
Intriguingly, ACE2-iPS cells generated from men are more sensitive
to SARS-CoV2 infection than those from women (25). These results indicate that if a
molecular mechanism of a given clinical phenotype stems from a
fundamental biological event encoded in the genome, iPSCs can model
the phenotype. This might be the case in our gefitinib-induced
hepatotoxicity study.
To determine the molecular mechanism by which
gefitinib exerted higher toxicity against iPSCs from the T group
compared to those from the N group, we examined various molecules
in possible pathways such as pNFκB/NFκB and pTank-binding kinase
(TBK)1/TBK1 related to inflammation. However, we could not identify
gefitinib-induced changes for the pathways between N and T groups
(data not shown). The expression levels of the major metabolizing
enzyme of gefitinib, cytochrome p450 3A4 (CYP 3A4) (28–30),
in iPSCs from both groups (Fig.
S4) were also examined. It was shown that there were no
significant differences on the expression levels among the cells.
Interestingly, all the patients in the N group have an exon 19
deletion mutation in EGFR, while all the patients in the T group
have an Exon 21 L585R mutation (Table
SI). There is a possibility that different EGFR mutations have
an impact on gefitinib-induced hepatotoxicity. We are now
investigating the molecular mechanism of gefitinib-induced
hepatotoxicity.
Collectively, these results suggest that a
cell-based assay system using iPSCs may become a platform for
preclinical tests to predict gefitinib-induced hepatotoxicity.
Supplementary Material
Supporting Data
Supporting Data
Acknowledgements
Not applicable.
Funding
This work was partly supported by the grant-in-Aid for
Scientific Research© (grant no. 19K07179) from the Japan Society
for the Promotion of Science (to YF) and the OMC Internal Research
Grant (to MA).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YF, TN, KT and MA participated in the conception and
design of the study. YF and MW performed all the experiments with
help from TN, KT, NM, YT, SI and AI. TN and MA wrote the
manuscript. TN and MW performed the statistical analyses. YF, TN,
KT, NM, YT, SI, AI and MA evaluated the results. YF, TN, MW and MA
confirm the authenticity of all the raw data. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
The study was conducted according to the guidelines
of The Declaration of Helsinki and was approved by the Ethical
Committee of the Osaka Medical College (now Osaka Medical and
Pharmaceutical University) (approval no. 2100 on 10.03.2017).
Written informed consent was obtained from all study subjects.
Patient consent for publication
Written informed consent has been obtained from all
the study subjects to publish this paper.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Thai AA, Solomon BJ, Sequist LV, Gainor JF
and Heist RS: Lung cancer. Lancet. 398:535–554. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ettinger DS, Bepler G, Bueno R, Chang A,
Chang JY, Chirieac LR, D'Amico TA, Demmy TL, Feigenberg SJ, Grannis
FW Jr, et al: Non-small cell lung cancer clinical practice
guidelines in oncology. J Natl Compr Canc Netw. 4:548–582. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Takeda M, Okamoto I and Nakagawa K: Pooled
safety analysis of EGFR-TKI treatment for EGFR mutation-positive
non-small cell lung cancer. Lung Cancer. 88:74–79. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Lee WM: Acute liver failure in the United
States. Semin Liver Dis. 23:217–226. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sharma A, Mücke M and Seidman CE: Human
induced pluripotent stem cell production and expansion from blood
using a non-integrating viral reprogramming vector. Curr Protoc Mol
Biol. 122:e582018. View
Article : Google Scholar : PubMed/NCBI
|
|
6
|
Corbett JL and Duncan SA: iPSC-derived
hepatocytes as a platform for disease modeling and drug discovery.
Front Med (Lausanne). 6:2652019. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Davidson MD, Ware BR and Khetani SR: Stem
cell-derived liver cells for drug testing and disease modeling.
Discov Med. 19:349–358. 2015.PubMed/NCBI
|
|
8
|
Park IH, Arora N, Huo H, Maherali N,
Ahfeldt T, Shimamura A, Lensch MW, Cowan C, Hochedlinger K and
Daley GQ: Disease-specific induced pluripotent stem cells. Cell.
134:877–886. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Maehr R, Chen S, Snitow M, Ludwig T,
Yagasaki L, Goland R, Leibel RL and Melton DA: Generation of
pluripotent stem cells from patients with type 1 diabetes. Proc
Natl Acad Sci USA. 106:15768–15773. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Soldner F, Hockemeyer D, Beard C, Gao Q,
Bell GW, Cook EG, Hargus G, Blak A, Cooper O, Mitalipova M, et al:
Parkinson's disease patient-derived induced pluripotent stem cells
free of viral reprogramming factors. Cell. 136:964–977. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ellis J and Bhatia M: iPSC technology:
Platform for drug discovery. Point. Clin Pharmacol Ther.
89:639–641. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Carpentier A, Nimgaonkar I, Chu V, Xia Y,
Hu Z and Liang TJ: Hepatic differentiation of human pluripotent
stem cells in miniaturized format suitable for high-throughput
screen. Stem Cell Res. 16:640–650. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Varghese DS, Alawathugoda TT and Ansari
SA: Fine tuning of hepatocyte differentiation from human embryonic
stem cells: Growth factor vs small molecule-based approaches. Stem
Cells Int. 2019:59682362019. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Si-Tayeb K, Noto FK, Nagaoka M, Li J,
Battle MA, Duris C, North PE, Dalton S and Duncan SA: Highly
efficient generation of human hepatocyte-like cells from induced
pluripotent stem cells. Hepatology. 51:297–305. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Hay DC, Zhao D, Fletcher J, Hewitt ZA,
McLean D, Urruticoechea-Uriguen A, Black JR, Elcombe C, Ross JA,
Wolf R and Cui W: Efficient differentiation of hepatocytes from
human embryonic stem cells exhibiting markers recapitulating liver
development in vivo. Stem Cells. 26:894–902. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Gao X and Liu Y: A transcriptomic study
suggesting human iPSC-derived hepatocytes potentially offer a
better in vitro model of hepatotoxicity than most hepatoma cell
lines. Cell Biol Toxicol. 33:407–421. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Yamaguchi T, Matsuzaki J, Katsuda T, Saito
Y, Saito H and Ochiya T: Generation of functional human hepatocytes
in vitro: Current status and future prospects. Inflamm Regen.
39:132019. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ware BR, Berger DR and Khetani SR:
Prediction of drug-induced liver injury in micropatterned
co-cultures containing iPSC-derived human hepatocytes. Toxicol Sci.
145:252–262. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Zhou W, Graham K, Lucendo-Villarin B,
Flint O, Hay DC and Bagnaninchi P: Combining stem cell-derived
hepatocytes with impedance sensing to better predict human drug
toxicity. Expert Opin Drug Metab Toxicol. 15:77–83. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Okita K, Yamakawa T, Matsumura Y, Sato Y,
Amano N, Watanabe A, Goshima N and Yamanaka S: An efficient
nonviral method to generate integration-free human-induced
pluripotent stem cells from cord blood and peripheral blood cells.
Stem Cells. 31:458–466. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Ballet F: Hepatotoxicity in drug
development: Detection, significance and solutions. J Hepatol. 26
(Suppl 2):S26–S36. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Dirven H, Vist GE, Bandhakavi S, Mehta J,
Fitch SE, Pound P, Ram R, Kincaid B, Leenaars CHC, Chen M, et al:
Performance of preclinical models in predicting drug-induced liver
injury in humans: A systematic review. Sci Rep. 11:64032021.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Takeda M, Okamoto I, Tsurutani J, Oiso N,
Kawada A and Nakagawa K: Clinical impact of switching to a second
EGFR-TKI after a severe AE related to a first EGFR-TKI in
EGFR-mutated NSCLC. Jpn J Clin Oncol. 42:528–533. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ho C, Davis J, Anderson F, Bebb G and
Murray N: Side effects related to cancer treatment: CASE 1.
Hepatitis following treatment with gefitinib. J Clin Oncol.
23:8531–8533. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Sano E, Deguchi S, Sakamoto A, Mimura N,
Hirabayashi A, Muramoto Y, Noda T, Yamamoto T and Takayama K:
Modeling SARS-CoV-2 infection and its individual differences with
ACE2-expressing human iPS cells. iScience. 24:1024282021.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Beigel JH, Tomashek KM, Dodd LE, Mehta AK,
Zingman BS, Kalil AC, Hohmann E, Chu HY, Luetkemeyer A, Kline S, et
al: Remdesivir for the treatment of Covid-19-final report. N Engl J
Med. 383:1813–1826. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Axfors C, Schmitt AM, Janiaud P, van't
Hooft J, Abd-Elsalam S, Abdo EF, Abella BS, Akram J, Amaravadi RK,
Angus DC, et al: Mortality outcomes with hydroxychloroquine and
chloroquine in COVID-19 from an international collaborative
meta-analysis of randomized trials. Nat Commun. 12:23492021.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Culy CR and Faulds D: Gefitinib. Drugs.
62:2237–2250. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Cohen MH, Williams GA, Sridhara R, Chen G,
McGuinn WD Jr, Morse D, Abraham S, Rahman A, Liang C, Lostritto R,
et al: United states food and drug administration drug approval
summary: Gefitinib (ZD1839; Iressa) tablets. Clin Cancer Res.
10:1212–1218. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
McKillop D, McCormick AD, Millar A, Miles
GS, Phillips PJ and Hutchison M: Cytochrome P450-dependent
metabolism of gefitinib. Xenobiotica. 35:39–50. 2005. View Article : Google Scholar : PubMed/NCBI
|