Introduction
Lateral lymph node metastasis is a form of
postoperative recurrence in lower rectal cancer. Local resection,
radiotherapy, and systemic chemotherapy are indicated for the local
recurrence of rectal cancer. Regarding solitary lateral lymph node
recurrence, it is reported that it may offer a favorable long-term
prognosis when treated with local resection (1). However, small tumors or lymph nodes
can be difficult to detect due to their location in the deep pelvic
region and the impact of reoperation. Furthermore, the resection
margin is difficult to determine due to the presence of surrounding
tissues. Therefore, CT-guided marking techniques, which are
commonly used in pulmonary surgery, but are only rarely applied in
abdominal surgeries (2), should be
considered. India ink marking has been widely used and it is
considered safe and effective (3).
In the past, the effectiveness of CT-guided marking with India ink
has been reported in abdominal surgery (4). In addition, CT-guided marking using
microcoils has been reported to be safe and effective (5–7).
Microcoil localization has the advantages of accuracy, high success
rate, low complications, and good tolerance (8–10).
We herein report a case of laparoscopic resection of
lateral lymph node recurrence of rectal cancer that was
successfully treated with preoperative CT-guided marking with India
ink and microcoils.
Case report
A 48-year-old man had undergone laparoscopic low
anterior resection with D3 lymph node dissection and left lateral
lymph node dissection for rectal cancer in September 2019 at the
Japanese Red Cross Society Karatsu Red Cross Hospital (Karatsu,
Japan). The tumor had mainly been located in the upper rectum above
the peritoneal reflection. A digital rectal examination palpated
the inferior margin of the tumor, 7 cm from the anus. The final
findings were pT3N1bM0 and pStage IIIb according to the 8th edition
of the UICC classification (11).
Postoperative adjuvant chemotherapy consisting of capecitabine was
administered for 6 months. Oxaliplatin was not administered due to
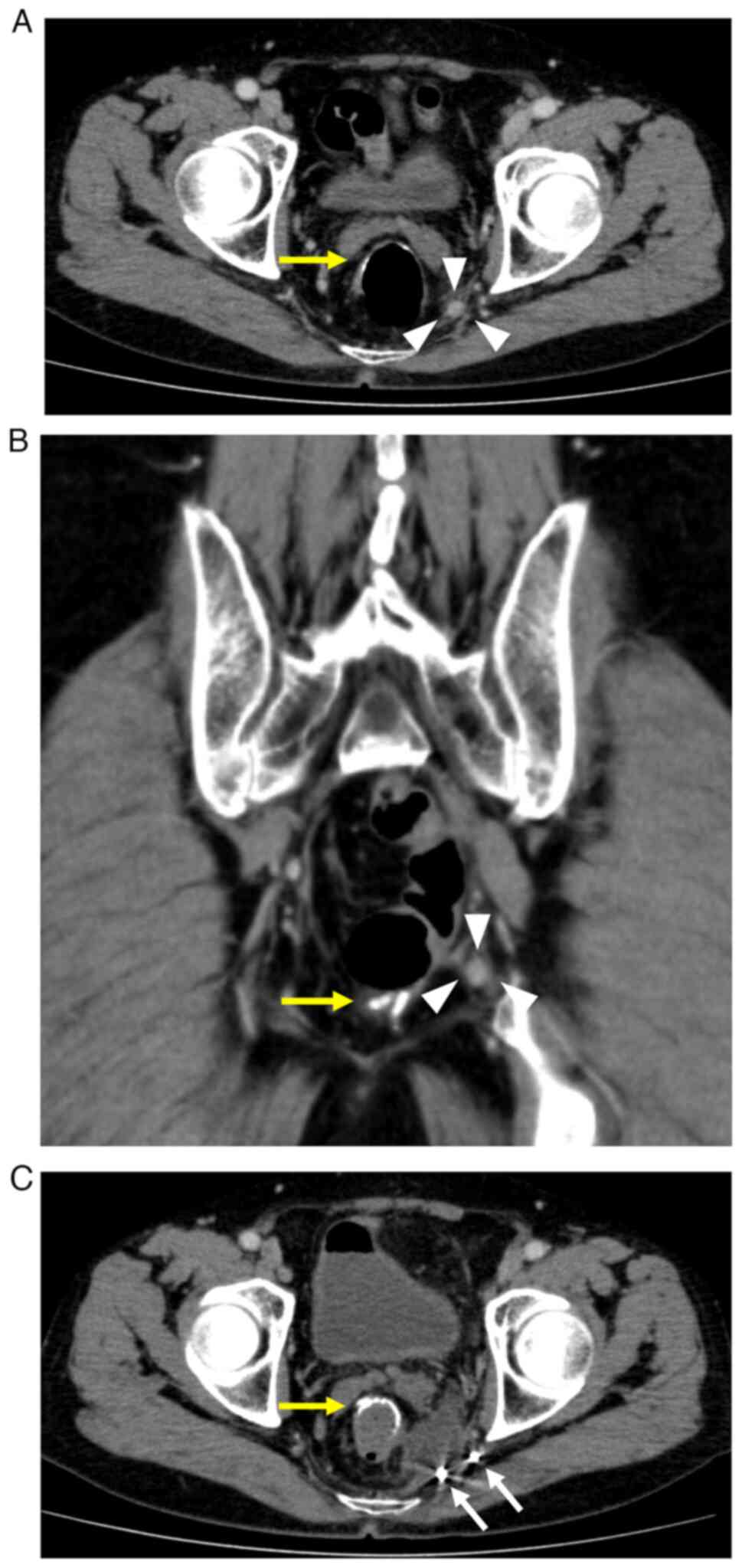
occupational reasons. However, at 6 months postoperatively, a
solitary mass (diameter: 10 mm) was found in the left lateral
region on enhanced abdominal computed tomography (CT), and he was
diagnosed to have local recurrence because of an accompanying
increase in the tumor marker levels. Systemic chemotherapy
(irinotecan, S-1, and bevacizumab) was administered for 2 years.
Stable disease persisted as the lesion decreased to 8 mm, and the
carcinoembryonic antigen (CEA) and carbohydrate antigen 19-9
(CA19-9) levels fell to within the normal range. Fluorodeoxyglucose
(FDG) positron emission tomography CT showed no accumulation of
18F-FDG (early SUVmax, 1.3; delayed SUVmax, 2.0). However, the
lesion again increased in size to 10 mm at 3.5 years after surgery
(Fig. 1A and B). FDG positron
emission tomography CT showed the minor accumulation of 18F-FDG
(early SUVmax 1.6, delayed SUVmax, 2.8). The patient's CEA and
CA19-9 levels were within the normal ranges. No palpable tumorous
lesions were observed on a digital rectal examination. The lesion
had mildly increased in size, and PET-CT showed a minor
accumulation. As a result, a relapse was suspected. Hence,
percutaneous CT-guided biopsy was not considered due to the risk of
dissemination. Resection of the solitary left lateral lymph node
was considered, because no other new lesions had appeared. A high
degree of operative difficulty was expected due to reoperation, the
tumor location in the deep pelvis, and visibility problems
regarding lesion identification. Therefore, preoperative marking
with CT guidance was performed before surgery to ensure a secure
and safe resection. Written informed consent was obtained for the
CT-guided marking and surgical procedures. The patient was placed
in a prone position on the CT table, and a 21-gauge needle was
percutaneously inserted into the pelvis near the tumor. After local
anesthesia, saline solution (2.0 ml) was topically injected near
the tumor using a fine needle to maintain the space for placement
of the microcoil so as not to injure the surrounding nerve and
vasculature. India ink (1.0 ml) was injected between the tumor and
the pelvic side, and two microcoils, originally designed for
vascular embolization (Hilal Embolization Microcoil™, Cook
Medical Japan), were implanted by a radiologist. The two coils were
placed on either side (i.e., the interior and exterior) of the
tumor on the morning of the surgery (Fig. 1C). The ureteral stent was placed by
a urologist to avoid injury to the left ureter. Subsequently,
laparoscopic surgery was performed. After the sharp dissection of
adhesions between the large intestine and the pelvic wall, the left
ureter was identified and preserved. A rectal examination was
performed intraoperatively to avoid any rectal injury. After
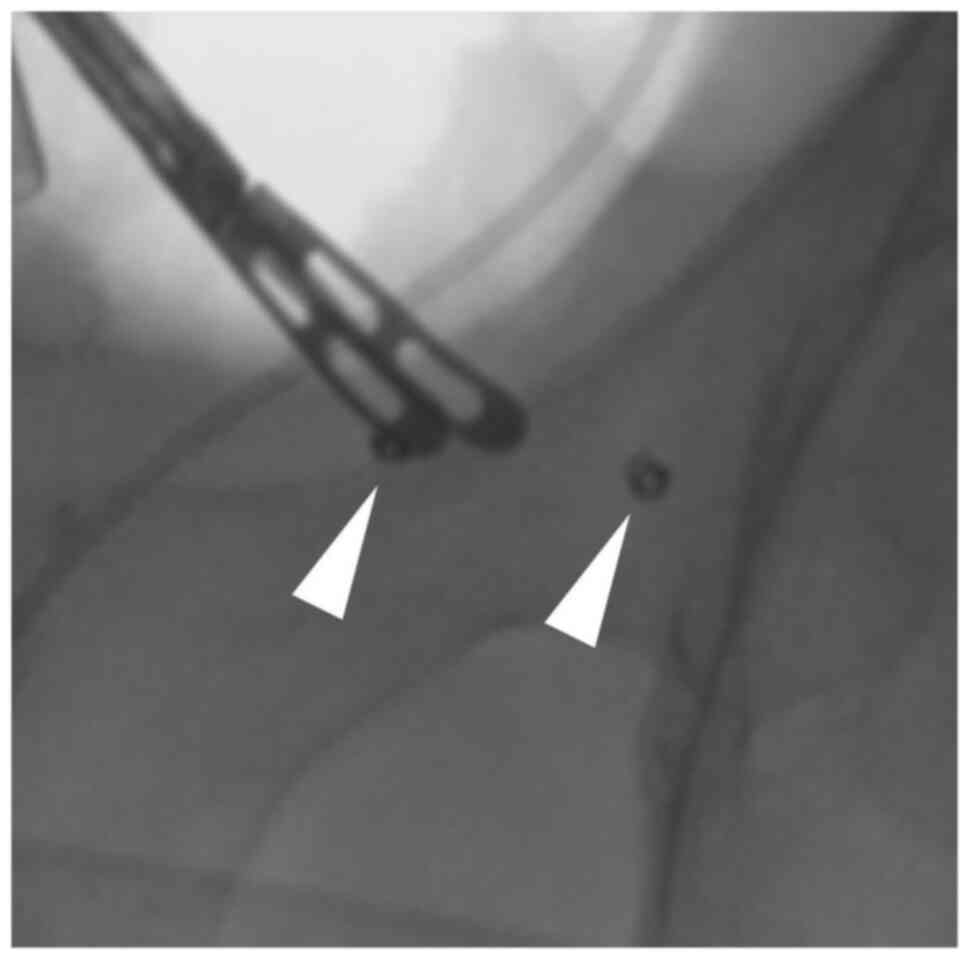
careful dissection, the targeted tumor was identified
intraoperatively using the two embolization microcoils as landmarks
and intraoperative fluoroscopy (Fig.
2). The embolization microcoils were not visible, but they were
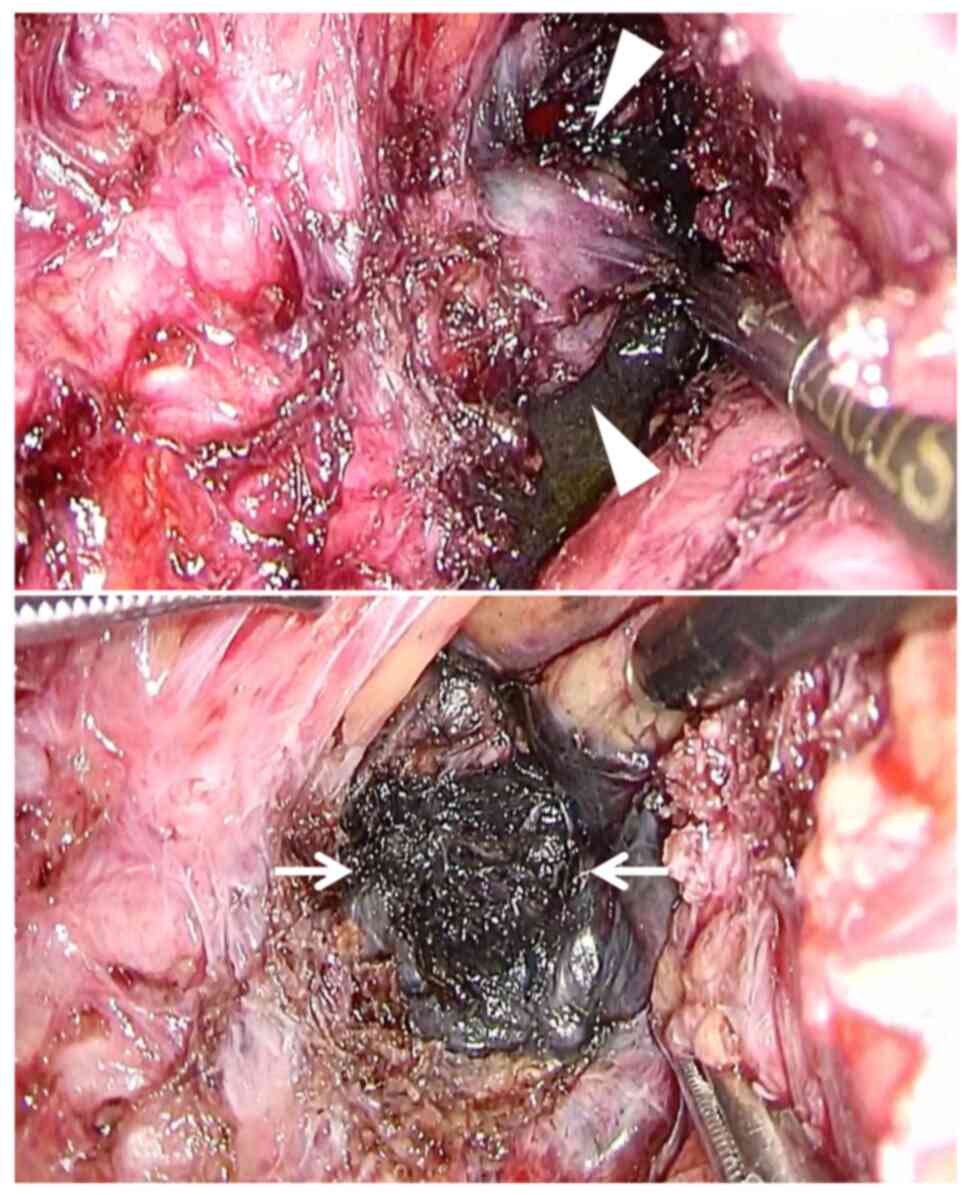
useful for identifying the extent of resection. The tumor was
identified between the two coils and thus was successfully
exfoliated with the surrounding fat. During resection, black ink
was visibly identified (Fig. 3).
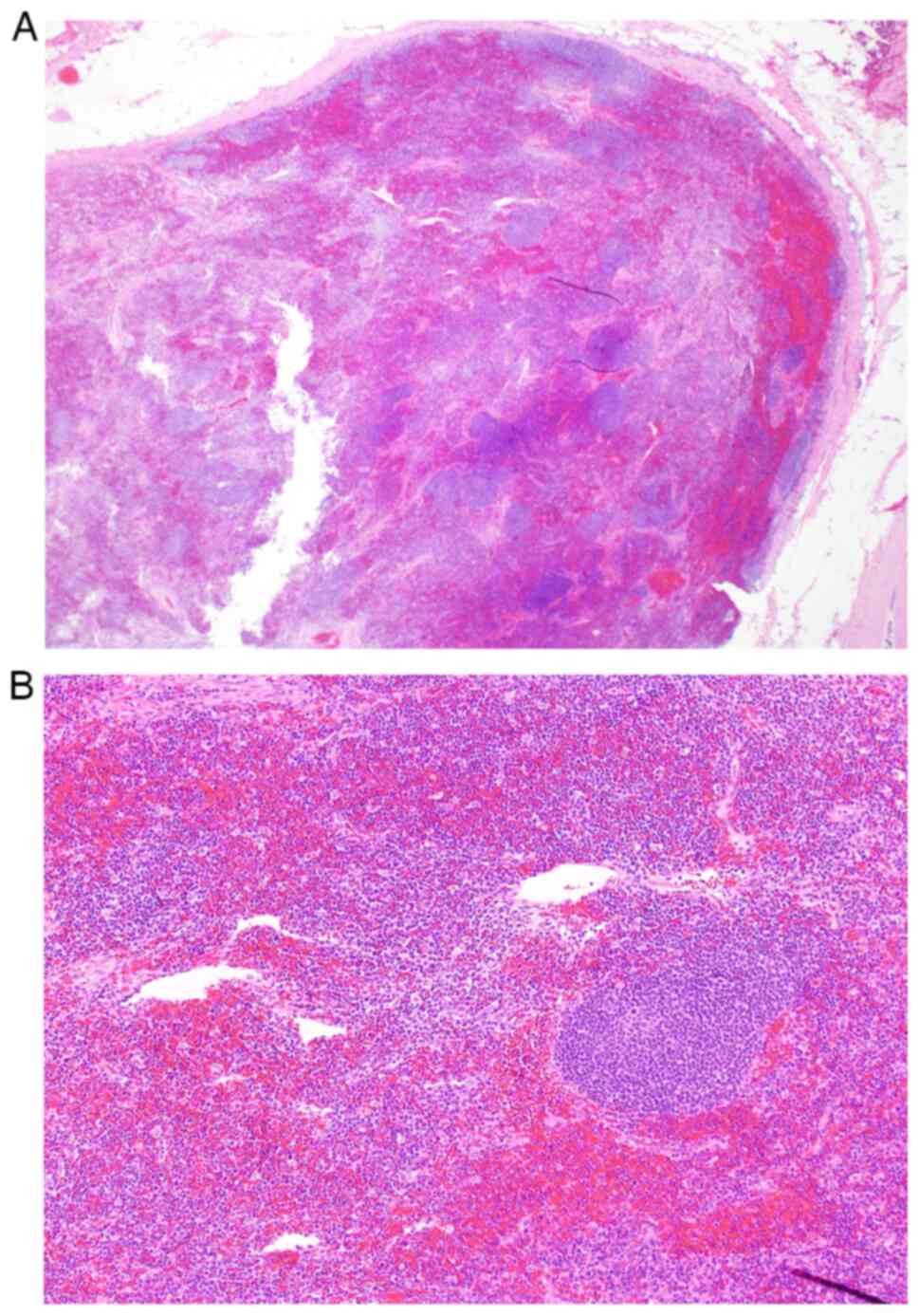
Laparoscopic lymphadenectomy was completed within 5 h and 7 min
with 100 ml of blood loss. The resected specimen was a solid nodule
measuring 10 mm in size. The pathological diagnosis revealed no
viable tumor cells in the dissected lymph nodes (Fig. 4). The patient was discharged on
postoperative day 5 without any complications and remained
disease-free for 7 months postoperatively.
Discussion
Postoperative pelvic recurrence is a clinical
condition experienced by some patients after curative resection for
rectal cancer. The indications for treatment are based on a
comprehensive consideration of the number of recurrences, location,
and postoperative period. Regarding lateral lymph node recurrence,
it has been reported that even if lateral lymph node metastasis
occurs, the disease can be controlled if there are <2 metastatic
lymph nodes (12). Local resection
can achieve a favorable long-term prognosis in patients with
solitary lateral lymph node metastasis (1). Thus, surgical resection may be
considered if the disease is localized and no other recurrent
lesions are observed. However, surgical resection involves various
procedural difficulties associated with reoperation, a location in
the deep pelvis, and the visual identification of lesions.
Preoperative CT-guided marking for tumor
identification is frequently reported to be effective for
intraoperative identification of small tumors in the lung and for
accurate surgical resection in respiratory surgery (13). However, there have been few reports
on CT-guided marking in abdominal surgery, and its effectiveness
and indications have not yet been established. The key issue is
that lateral lymph node metastasis sometimes occurs in the deep
pelvic space and after surgery. In this case, we considered that
CT-guided marking may be effective for recognizing the target and
resecting the tumor with sufficient surgical margins, as it was
very small and the dissection layer was difficult to identify due
to reoperation. A search of PubMed with the key words
‘preoperative’ and ‘CT-guided marking’ revealed one case report on
preoperative CT-guided marking in abdominal surgery, which reported
the efficacy of CT-guided marking with India ink and iopamidol for
the recurrence of ascending colon cancer (diameter: 2 cm) in the
right pararenal region (4).
Hookwire, ICG, India ink, and Lipiodol are often
used for markings (14,15). India ink and microcoils were used in
this study. India ink has been conventionally used, and its
effectiveness and safety have been established (3). Because the ink is black, it is
considered to have excellent visibility. However, there is concern
that the ink may spread to the surrounding tissue and thereby
obscure the objective. Moreover, such markings may not be visible
during surgery. Therefore, microcoils were used to increase the
chance of intraoperative confirmation and to accurately resect the
tumor. Microcoils have been used for vascular embolization and have
shown good tissue compatibility. In addition, such microcoils are
soft and thus do not cause significant damage to the tissue after
implantation into the body (16,17).
CT-guided microcoils have been reported to be safe and effective
tools for easy and fast video-assisted thoracoscopic surgery
(5–7). Therefore, we decided to use microcoils
to treat this patient after obtaining sufficient written informed
consent. As previously reported, iopamidol was used instead of the
microcoils (4). However, there was
a concern that it may not be visible on fluoroscopy because it
could spread to the surrounding tissue and become diluted because
it is a liquid. In addition, when performing preoperative CT-guided
marking, careful examination is required to avoid complications
such as bleeding and infection (18). As a result, X-ray fluoroscopy made
it easy to recognize the markings and accurately resect the tumor
laparoscopically. CT-guided marking with India ink and microcoils
using fluoroscopy is useful for abdominal surgery. Although few
reports have previously described this method, it may be useful for
the curative resection of small tumors.
In conclusion, CT-guided marking with India ink and
microcoils is useful for ensuring curative surgery for small
tumors. To our knowledge, this is the first English case report of
successful laparoscopic surgery using CT-guided marking with India
ink and microcoils.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
All of the authors contributed to the diagnosis and
treatment of the patient. SF and MH drafted the manuscript. TO, YT
and RS edited the manuscript. RS supervised the study and approved
the final version of the manuscript. MH and RS confirm the
authenticity of all the raw data. All authors read and approved the
final version of the manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained from the
patient for publication of this case report and accompanying
images.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
CT
|
computed tomography
|
|
CEA
|
carcinoembryonic antigen
|
|
CA19-9
|
carbohydrate antigen 19-9
|
|
FDG
|
fluorodeoxyglucose
|
References
|
1
|
Miura T, Tsunenari T, Sasaki T, Yokoyama T
and Fukuhara K: A curatively resected case of lateral lymph node
metastasis five-years after initial surgery for rectal cancer. Gan
To Kagaku Ryoho. 44:1405–1407. 2017.(In Japanese). PubMed/NCBI
|
|
2
|
Mun M, Matsuura Y, Nakao M, Ichinose J,
Nakagawa K and Okumura S: Noninvasive computed tomography-guided
marking technique for peripheral pulmonary nodules. J Thorac Dis. 8
(Suppl 9):S672–S676. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
McArthur C, Roayaie S and Waye J: Safety
of preoperation endoscopic tattoo with india ink for identification
of colonic lesions. Surg Endosc. 13:397–400. 1999. View Article : Google Scholar
|
|
4
|
Koyama H, Noma S, Tamaki Y, Goto K,
Kitamura E, Maeda T, Matsumoto S, Sano A and Sugimura K: CT
localisation of small pulmonary nodules prior to thorascopic
resection: Evaluation of a point marker system. Eur J Radiol.
65:468–472. 2008. View Article : Google Scholar
|
|
5
|
Liu L, Zhang LJ, Chen B, Cao JM, Lu GM,
Yuan L, Li K and Xu J: Novel CT-guided coil localization of
peripheral pulmonary nodules prior to videoassisted thoracoscopic
surgery: A pilot study. Acta Radiol. 55:699–706. 2014. View Article : Google Scholar
|
|
6
|
Huang ZG, Wang CL, Sun HL, Li CD, Gao BX,
Chen H and Yang MX: CT-guided microcoil localization of small
peripheral pulmonary nodules to direct video-assisted thoracoscopic
resection without the aid of intraoperative fluoroscopy. Korean J
Radiol. 22:1124–1131. 2021. View Article : Google Scholar
|
|
7
|
An J, Dong Y, Li Y, Han X, Niu H, Zou Z,
Wu J, Tian Y and Chen Z: CT-guided placement of microcoil end in
the pleural cavity for video-assisted thoracic surgical resection
of ground-glass opacity: A retrospective study. J Cardiothorac
Surg. 17:3162022. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Powell TI, Jangra D, Clifton JC,
Lara-Guerra H, Church N, English J, Evans K, Yee J, Coxson H, Mayo
JR and Finley RJ: Peripheral lung nodules: Fluoroscopically guided
video-assisted thoracoscopic resection after computed
tomography-guided localization using platinum microcoils. Ann Surg.
240:481–488. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Mayo JR, Clifton JC, Powell TI, English
JC, Evans KG, Yee J, McWilliams AM, Lam SC and Finley RJ: Lung
nodules: CT-guided placement of microcoils to direct video-assisted
thoracoscopic surgical resection. Radiology. 250:576–585. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Lempel JK, Raymond DP, Ahmad U, O'Malley
S, Bolen MA, Graham R, Azok JT, Bullen J, Raja S and Murthy S:
Video-assisted thoracic surgery resection without intraoperative
fluoroscopy after CT-guided microcoil localization of peripheral
pulmonary nodules. J Vasc Interv Radiol. 29:1423–1428. 2018.
View Article : Google Scholar
|
|
11
|
UICC, . TNM Classification of Malignant
Tumours. 8th edition. John Wiley & Sons Ltd.; New York, NY:
2017
|
|
12
|
Homma Y, Hamano T, Otsuki Y, Shimizu S and
Kobayashi Y: Total number of lymph node metastases is a more
significant risk factor for poor prognosis than positive lateral
lymph node metastasis. Surg Today. 45:168–174. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ueki H, Fujimoto T, Okuno M, Kusuda Y,
Taguchi I, Itou Y, Kiyonaka S and Kawabata G: The use of CT-guided
marking for the laparoscopic resection of a solitary
retroperitoneal metastasis of colon cancer. J Endourol Case Rep.
4:120–123. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ashida R, Yamao K, Okubo K, Sawaki A,
Mizuno N, Nakamura T, Tajika M, Kawai H and Shimizu Y: Indocyanine
green is an ideal dye for endoscopic ultrasound-guided fine-needle
tattooing of pancreatic tumors. Endoscopy. 38:190–192. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kang DY, Kim HK, Kim YK, Yong HS, Kang EY
and Choi YH: Needlescopy-assisted resection of pulmonary nodule
after dual localization. Eur Respir J. 37:13–17. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hwang S, Kim TG and Song YG: Comparison of
hook wire versus coil localization for video-assisted thoracoscopic
surgery. Thorac Cancer. 9:384–389. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Hu L, Gao J, Chen C, Zhi X, Liu H and Hong
N: Comparison between the application of microcoil and hookwire for
localizing pulmonary nodules. Eur Radiol. 29:4036–4043. 2019.
View Article : Google Scholar
|
|
18
|
Fumimoto S, Sato K, Koyama M, Yamamoto K,
Narumi Y, Hanaoka N and Katsumata T: Combined lipiodol marking and
video-assisted thoracoscopic surgery in a hybrid operating room. J
Thorac Dis. 10:2940–2947. 2018. View Article : Google Scholar : PubMed/NCBI
|