Introduction
Malignant biliary obstruction (MBO) is a spectrum of
disorders in which malignant tumors cause narrowing of the bile
ducts, thereby affecting bile excretion. Common causes include
cholangiocarcinoma, gallbladder cancer, pancreatic cancer, bladder
cancer and metastatic tumors. However, this disease usually
progresses insidiously, resulting in >80% of patients being
ineligible for radical surgery at the time of diagnosis (1,2).
Therefore, endoscopic retrograde cholangiopancreatography (ERCP)
combined with biliary stenting has become the treatment of choice
for patients with MBO who cannot undergo radical surgery. This
approach is favored for its minimally invasive nature, high success
rate and good patient tolerability (3,4).
However, a study in the United Kingdom reported an early mortality
rate of 19.1% within 30 days after ERCP, with ahigher rate of 25.3%
in patients with severe biliary obstruction (5,6). In
patients with early mortality within 30 days postoperatively, the
main purpose of ERCP stent implantation is to ensure biliary
patency and drainage. In such cases, the placement of plastic
stents is sufficient to guarantee the continuation of the life of
the patient, and the advantages of metal stents in terms of
duration of use and patency are null and void, whereas their high
cost imposes a significant financial burden on the patient and the
healthcare system (7). Therefore,
it is urgent to predict the risk of early postoperative mortality
and to select clinical protocols based on the expected survival
time of patients with MBO.
Currently, most studies on early death within 30
days after ERCP in patients with MBO have focused on the analysis
of risk factors associated with postoperative death (6,8),
whilst modeling studies aimed at predicting early death within 30
days after ERCP in patients with MBO are scarce. This makes it
difficult to effectively predict the risk of early postoperative
death with preoperative data and to screen high-risk patients with
preoperative information. Kalaitzakis (9) predicted the risk of early death within
30 days after ERCP in patients with biliary obstruction by
analyzing demographic characteristics, mode of admission and
comorbidities; however, the study included patients with benign
biliary obstruction. Zhu et al (10) reported that factors such as distant
metastasis, total bilirubin level, post-ERCP complications and
successful drainage were associated with early death within 30 days
after ERCP in patients with MBO; however, the exploration of the
general condition of the patients and tumor-related factors was not
comprehensive. Furthermore, most of these studies were limited to a
small number of laboratory indicators, and their predictive ability
still needs to be further validated and evaluated. To achieve
accurate early warning of early death within 30 days after surgery,
new early warning models need to be constructed and validated based
on more comprehensive preoperative data, including laboratory
indicators, tumor-related factors and the general health status of
patients.
It is currently common practice to use traditional
statistical methods, such as logistic regression, to build simple
and easy-to-use predictive models. However, as patients with MBO
may have multiple tumor types, which results in increased
complexity of features and possible correlations among features,
traditional statistical methods may not be able to effectively
address this complexity (11,12).
By contrast, an artificial neural network (ANN), as an advanced
machine learning technique, can learn the relationship between
complex features and outcomes from a large amount of heterogeneous
data (13), which provides new
ideas and strong support for the establishment of clinical
prediction models.
Therefore, the present study aimed to assess the
potential clinical predictors of death within 30 days after ERCP in
patients with MBO using comprehensive clinical data and construct a
visualized prediction model. Furthermore, the present study aimed
to build a simple ANN model to evaluate its predictive ability and
compare it with the traditional model to verify the advantages and
disadvantages of the performance of both in clinical
applications.
Materials and methods
Patient selection
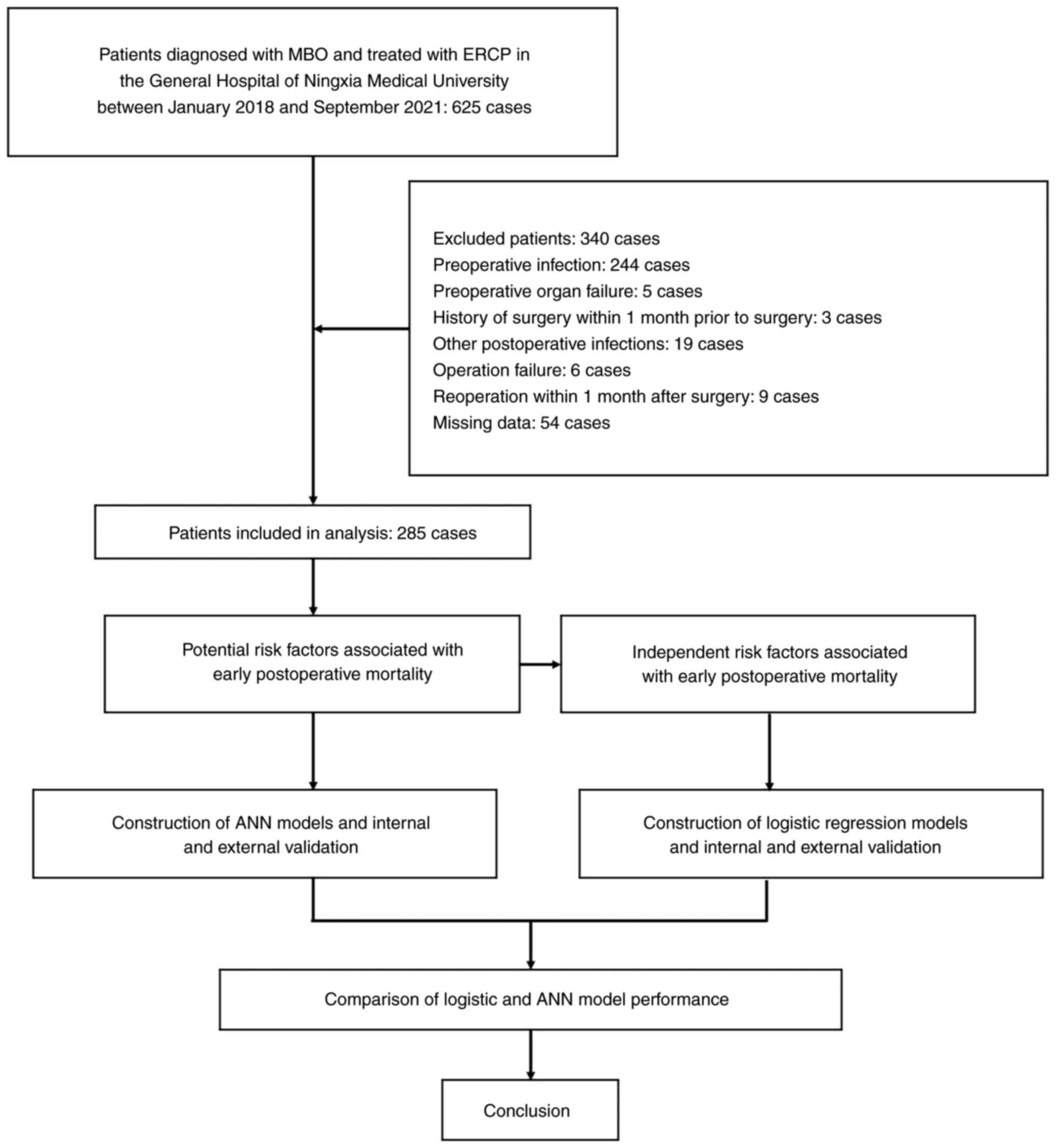
A total of 625 patients, diagnosed with MBO through
imaging and/or pathology and treated with ERCP combined with
biliary stenting at the Department of Hepatobiliary Surgery in the
General Hospital of Ningxia Medical University (Yinchuan, China)
between January 2018 and September 2021, were included in the
present study. After excluding 340 patients, a total of 285
patients were included. The specific study procedure and patient
selection are outlined in Fig. 1.
Prior to surgery, all patients provided written informed consent
for the procedure. The study was approved by the Ethics Committee
of the General Hospital of Ningxia Medical University (approval no.
KYLL-2023-0450). The inclusion criteria were as follows: i) Age of
>18 years; ii) sufficient evidence (imaging and pathology) to
diagnose MBO; and iii) inability to perform surgical resection of
the lesion due to lesion progression, metastasis and poor general
condition. The exclusion criteria were as follows: i) Serious
infection or organ failure before surgery; ii) Eastern Cooperative
Oncology Group (ECOG) score of 4 (14); iii) received other antitumor
treatment within 1 month after surgery, such as percutaneous
transhepatic cholangial drainage or endoscopic ultrasound-guided
biliary stenting (except symptomatic supportive treatment); iv)
incomplete clinical data; v) other surgery within 30 days after
surgery; and vi) other accidental death due to non-disease causes
(such as from traffic accidents or suicide).
Data collection
The data collected included several clinical
characteristics of the patients. Demographic information, such as
age, sex and body mass index, was recorded. General information,
such as liver function Child-Pugh classification (15), ECOG score, history of previous ERCP,
history of abdominal surgery and history of gallstones, was also
documented. Laboratory markers, including white blood cell count,
hemoglobin, total bilirubin, direct bilirubin, albumin and glucose
levels, neutrophil-lymphocyte ratio count (NLR), cancer antigen
19-9 (CA19-9), carcinoembryonic antigen (CEA), alanine
aminotransferase, aspartate aminotransferase, lactate dehydrogenase
and alkaline phosphatase levels, and prothrombin time, were
measured and recorded. Other indicators, such as the length and
location of the obstruction, presence of biliary infection,
presence of liver metastasis, presence of abdominal lymph node
metastasis, presence of distant metastasis and type of stent used,
were also documented. Surgical time was categorized as <30 and
≥30 min based on previous studies (16,17).
In the present study, due to the limitation of the number of cases,
obstruction was categorized according to the location of the
obstruction, with high biliary obstruction considered as above the
site of the confluence of the cystic duct and common bile duct, and
low biliary obstruction considered as below it (18). Obstruction length was determined
using intraoperative ERCP angiography.
The data collection process was performed
retrospectively, ensuring that all relevant clinical information
was recorded accurately and comprehensively. This comprehensive
dataset allowed for a thorough analysis of the potential risk
factors associated with early death after ERCP in patients with
MBO.
ERCP method of operation
A thorough preoperative laboratory and examination
was performed to rule out contraindications to ERCP. CT and MRI
were performed to assess the location of the tumor, the degree of
invasion and the type of bile duct stricture. The intraoperative
decision to perform a sphincterotomy of Oddi was based on the
difficulty of intubation. Stents were selected based on
observations of the location and extent of the stricture, and the
internal diameter of the bile duct. In certain patients with high
MBO obstruction, pathological sampling and stenting were performed
under direct vision using the Spyglass transoral choledochoscope
fiberoptic direct vision system (Olympus, Corp.). Postoperatively,
the patients were treated with primary care, acid and enzyme
suppression, prophylactic anti-infectives and other symptomatic
supportive therapy.
Study endpoints and related
definitions
According to the relevant literature, early deaths
are defined as those occurring within 30 days following ERCP
(6,19). Therefore, the endpoint event of the
present study was to determine whether early death occurred in
patients with MBO after undergoing ERCP combined with biliary stent
placement. Patient death was primarily due to disease progression
or disease-related events, excluding accidental deaths unrelated to
the underlying condition (such as traffic accidents or
suicides).
Statistical analysis
Statistical analyses were performed using SPSS 26.0
software (IBM Corp.) and the R language package (4.1.3; R Package
for Statistical Computing; www.r-project.org). Data are presented as median
(interquartile range) or n (%). The unpaired Student's t-test or
the Mann-Whitney U test were used for continuous variables, and
Pearson's χ2 test or Fisher's exact test were used for
categorical data. Univariate analysis was used in the training
group to screen for potential risk factors associated with 30-day
mortality, P<0.05 was considered to indicate a statistically
significant difference.
Potential risk factors identified in a
multifactorial analysis were included in the logistic regression
model, which was constructed using independent risk factors, with
P<0.05. The odds ratio (OR) and 95% confidence interval (CI) for
the predictors were calculated, and the model was visualized using
a column-line graph based on the logistic results. Furthermore, the
‘Neural Network’ module in SPSS 26.0 software was used to construct
the ‘Multilayer Perceptron’ ANN model. The model had three layers:
Input layer, hidden layer and output layer. The covariates were
rescaled using a standardized method. The activation function of
the hidden layer was the hyperbolic tangent function; the training
type was batch training; the optimization algorithm chose conjugate
gradient; the initial sigma was set to 0.00005; the interval offset
was ±0.5; the maximum training time was set to 15 min; the minimum
relative change of training error was 0.0001; the minimum relative
change of the training error rate was 0.001; and the output layer
used the softmax function and the error function used
cross-entropy. As training progressed, the neural network model
gradually increased the accuracy of its correlation weight
coefficients, and when the training was complete, the ANN was
constructed.
In the present study, the predictive ability of the
logistic and ANN models was comprehensively assessed, validated and
compared through different indicators, including area under the
curve (AUC) with 95% confidence interval (CI), accuracy,
sensitivity and specificity. AUC is a key indicator for assessing
the discriminative ability of a model; it can be used to reflect
the overall discriminative ability of a model for positive and
negative samples by plotting receiver operator characteristic (ROC)
curves. Moreover, the 95% CIs of AUC values demonstrate the
statistical reliability of the results and can assess the stability
and significance of the model performance. Accuracy is an important
indicator for assessing the correct classification of the model,
which can evaluate the overall performance of the dataset.
Sensitivity measures the ability of the model to detect positive
cases, which can be used to assess the model's ability to recognize
positive cases and helps assess the model's false-negative rate,
and specificity reflects the ability of the model to correctly
identify the negative cases, which helps to assess the misdiagnosis
rate of the model. These metrics comprehensively evaluate the
performance of the model from multiple dimensions, such as overall
performance, positive case detection ability and negative case
exclusion ability, respectively. Therefore, these indicators of AUC
with 95% CI, accuracy, sensitivity and specificity can be used to
compare the predictive performance of logistic regression models
and ANN models, and to clarify their respective advantages and
disadvantages, to more comprehensively guide the selection in
practical applications.
Results
Baseline characteristics
The 285 patients who were included in the present
study were randomized into a training group (n=200) and a
validation group (n=85). A total of 155 patients were male and 130
were female, with ages ranging from 35-90 years. The distribution
of cancer types was as follows: Cholangiocarcinoma, n=95;
gallbladder carcinoma, n=12; pancreatic carcinoma, n=58;
hepatocellular carcinomas involving the first hepatic hilar, n=28;
pancreatic carcinoma, n=39; and metastatic carcinoma, n=53. The
incidence of early postoperative death was 20.0% (57/285). Of these
cases, 39 occurred in the training group and 18 in the validation
group. Analysis of the case records revealed that the causes of
death were progressive malignant disease in 32 cases, cholangitis
in 17 cases, acute liver failure in 5 cases, gastrointestinal
hemorrhage in 1 case, cardiac arrest in 1 case and acute pulmonary
edema in 1 case. No statistically significant differences were
demonstrated between the modeling and validation groups for any of
the assessed characteristics. The data for the characteristics of
each group are presented in Table
I.
 | Table I.Characteristics of the patients in
the training and validation groups. |
Table I.
Characteristics of the patients in
the training and validation groups.
| Variable | Training group
(n=200) | Validation group
(n=85) |
χ2/Z | P-value |
|---|
| Sex |
|
|
|
|
|
Male | 108 (54.0) | 47 (55.3) | 0.04 | 0.841 |
|
Female | 92 (46.0) | 38 (44.7) |
|
|
| Age, years | 72.0
(64.0–78.0) | 73.0
(67.5–79.0) | −0.946 | 0.344 |
| BMI,
kg/m2 | 22.0
(20.3–24.6) | 22.2
(21.5–23.3) | −0.446 | 0.655 |
| Infections |
|
|
|
|
|
Yes | 51 (25.5) | 28 (32.9) | 1.648 | 0.199 |
| No | 149 (74.5) | 57 (67.1) |
|
|
| Death |
|
|
|
|
|
Yes | 39 (19.5) | 18 (21.2) | 0.105 | 0.746 |
| No | 161 (80.5) | 67 (78.8) |
|
|
| Ascites |
|
|
|
|
|
Yes | 24 (12.0) | 6 (7.1) | 1.546 | 0.214 |
| No | 176 (88.0) | 79 (92.9) |
|
|
| History of
ERCP |
|
|
|
|
|
Yes | 61 (30.5) | 27 (31.8) | 0.045 | 0.833 |
| No | 139 (69.5) | 58 (68.2) |
|
|
| History of
abdominal surgery |
|
|
|
|
|
Yes | 49 (24.5) | 14 (16.5) | 2.233 | 0.135 |
| No | 151 (75.5) | 71 (83.5) |
|
|
| Liver
metastasis |
|
|
|
|
|
Yes | 34 (17.0) | 8 (9.4) | 2.734 | 0.098 |
| No | 166 (83.0) | 77 (90.6) |
|
|
| Lymph node
metastases |
|
|
|
|
|
Yes | 34 (17.0) | 10 (11.8) | 1.252 | 0.263 |
| No | 166 (83.0) | 75 (88.2) |
|
|
| Distant
metastasis |
|
|
|
|
|
Yes | 12 (6.0) | 3 (3.5) | 0.329 | 0.567 |
| No | 188 (94.0) | 82 (96.5) |
|
|
| ECOG score |
|
|
|
|
| 0 | 7 (3.5) | 4 (4.7) | −0.132 | 0.895 |
| 1 | 45 (22.5) | 18 (21.2) |
|
|
| 2 | 104 (52.0) | 43 (50.6) |
|
|
| 3 | 44 (22.0) | 20 (23.5) |
|
|
| Child-Pugh
class |
|
|
|
|
| A | 15 (7.5) | 13 (15.3) | −1.166 | 0.224 |
| B | 172 (86.0) | 65 (76.5) |
|
|
| C | 13 (6.5) | 7 (8.2) |
|
|
| Type of
malignancy |
|
|
|
|
|
Gallbladder cancer | 8 (4.0) | 4 (4.7) | 0.547 | 0.990 |
|
Cholangiocarcinoma | 67 (33.5) | 28 (32.9) |
|
|
|
Pancreatic cancer | 41 (20.5) | 17 (20.0) |
|
|
| Liver
cancer | 21 (10.5) | 7 (8.2) |
|
|
|
Ampullary cancer | 27 (13.5) | 12 (14.1) |
|
|
|
Metastatic cancer | 36 (18.0) | 17 (20.0) |
|
|
| Obstruction
site |
|
|
|
|
| High
obstruction | 78 (39.0) | 38 (44.7) | 0.805 | 0.370 |
| Low
obstruction | 122 (61.0) | 47 (55.3) |
|
|
| Obstruction length,
mm | 21.0
(11.2–31.8) | 20.0
(13.0–31.0) | −0.385 | 0.700 |
| Stent type |
|
|
|
|
| Plastic
stent | 32 (16.0) | 13 (15.3) | 1.587 | 0.662 |
| Metal
stent | 36 (18.0) | 17 (20.0) |
|
|
| Metal +
nasobiliary drainage | 48 (24.0) | 15 (17.6) |
|
|
| Nasal
biliary drainage | 84 (42.0) | 40 (47.1) |
|
|
| CA19-9 |
|
|
|
|
| ≥240
U/ml | 103 (51.5) | 41 (48.2) | 0.254 | 0.614 |
| <240
U/ml | 97 (48.5) | 44 (51.8) |
|
|
| CEA |
|
|
|
|
| ≥5
ng/ml | 76 (38.0) | 25 (29.4) | 1.923 | 0.166 |
| <5
ng/ml | 124 (62.0) | 60 (70.6) |
|
|
| WBC,
×109/l | 6.4 (5.0–7.7) | 6.5 (5.5–8.1) | −1.379 | 0.168 |
| NLR | 3.9 (2.6–5.8) | 4.4 (2.4–6.1) | −0.790 | 0.429 |
| HGB, g/l | 125.0
(111.0–135.0) | 124.0
(108.5–134.5) | −0.526 | 0.599 |
| TBIL, µmol/l | 198.3
(93.2–296.3) | 189.0
(67.5–307.0) | −0.595 | 0.552 |
| DBIL, µmol/l | 102.5
(27.8–181.6) | 103.0
(14.0–187.5) | −0.137 | 0.891 |
| ALB, g/l | 33.4
(30.0–37.1) | 32.6
(29.3–36.9) | −0.888 | 0.374 |
| ALT, U/l | 124.8
(69.8–192.3) | 125.0
(68.9–204) | −0.016 | 0.987 |
| AST, U/l | 112.0
(58.6–205.1) | 109.0
(60.8–200.5) | −0.150 | 0.881 |
| LDH, U/l | 485.0
(375.0–648.0) | 471.0
(367.0–617.0) | −0.778 | 0.436 |
| ALP, U/l | 341.3
(230.2–541.0) | 314.0
(205.5–624.5) | −0.095 | 0.924 |
| PT, sec | 12.3
(11.3–13.2) | 12.6
(11.4–13.7) | −1.582 | 0.114 |
Risk factor analysis for early
death
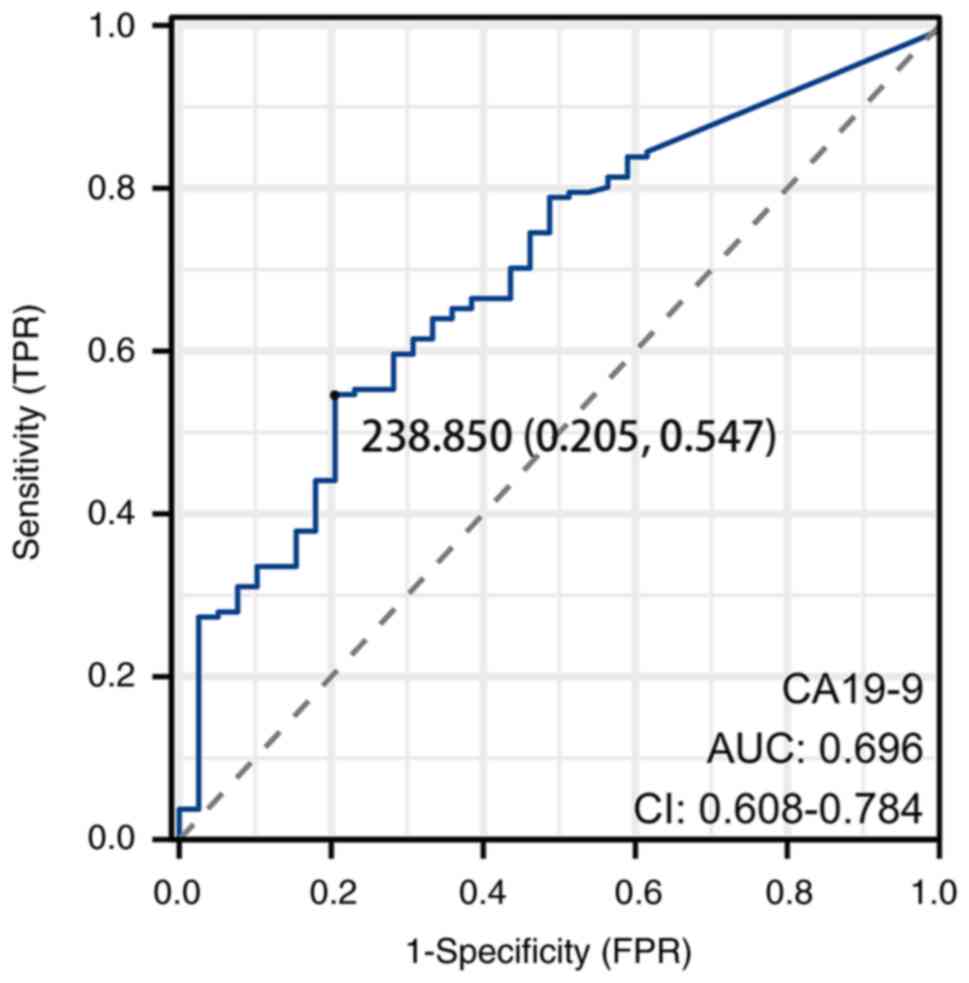
The results of univariate analysis in the training
group revealed five potential risk factors associated with the risk
of 30-day post-ERCP mortality in patients with MBO. These factors
included a history of previous ERCP surgery, CA19-9 levels, CEA
levels, liver metastasis and NLR (Table II). CA19-9 levels ranged from 2
U/ml to 1,200 U/ml, and for the purpose of statistical analysis,
the optimal cutoff value of 240 U/ml was determined based on the
maximum Jordon index (20). This
value was then categorized into high and low levels (Fig. 2) and transformed into a binary
variable. Similarly, the range of values for CEA was also wide, and
the upper limit of the normal value (4.7 ng/ml) was used as the
cutoff value. To simplify the statistical analysis, a cutoff value
of 5 ng/ml was used, transforming it into a dichotomous
variable.
 | Table II.Univariate analysis of 30-day
mortality-related risk factors. |
Table II.
Univariate analysis of 30-day
mortality-related risk factors.
| Variable | Died within 30 days
(n=39) | No death within 30
days (n=161) |
χ2/Z | P-value |
|---|
| Sex |
|
|
|
|
|
Male | 22 (56.4) | 86 (53.4) | 0.113 | 0.736 |
|
Female | 17 (43.6) | 75 (46.6) |
|
|
| Age, years | 75.0
(67.0–78.0) | 72.0
(64.0–78.0) | −1.273 | 0.203 |
| BMI,
kg/m2 | 21.9
(19.6–24.5) | 22.4
(20.6–24.7) | −0.785 | 0.433 |
| Infections |
|
|
|
|
|
Yes | 11 (28.2) | 40 (24.8) | 0.187 | 0.666 |
| No | 28 (71.8) | 121 (75.2) |
|
|
| Ascites |
|
|
|
|
|
Yes | 4 (10.3) | 20 (12.4) | 0.139 | 0.709 |
| No | 35 (89.7) | 141 (87.6) |
|
|
| History of
ERCP |
|
|
|
|
|
Yes | 19 (48.7) | 42 (26.1) | 7.585 | 0.006 |
| No | 20 (51.3) | 119 (73.9) |
|
|
| History of
abdominal surgery |
|
|
|
|
|
Yes | 9 (23.1) | 40 (24.8) | 0.053 | 0.818 |
| No | 30 (76.9) | 121 (75.2) |
|
|
| Liver
metastasis |
|
|
|
|
|
Yes | 11 (28.2) | 23 (14.3) | 4.311 | 0.038 |
| No | 28 (71.8) | 138 (85.7) |
|
|
| Lymph node
metastases |
|
|
|
|
|
Yes | 9 (23.1) | 25 (15.5) | 1.268 | 0.260 |
| No | 30 (76.9) | 136 (84.5) |
|
|
| Distant
metastasis |
|
|
|
|
|
Yes | 4 (10.3) | 8 (5.0) | 0.742 | 0.389 |
| No | 35 (89.7) | 153 (95.0) |
|
|
| ECOG score |
|
|
|
|
| 0 | 1 (2.6) | 6 (3.7) | −0.923 | 0.356 |
| 1 | 7 (17.9) | 38 (23.6) |
|
|
| 2 | 21 (53.8) | 83 (51.6) |
|
|
| 3 | 10 (25.6) | 34 (21.1) |
|
|
| Child-Pugh
class |
|
|
|
|
| A | 1 (2.6) | 14 (8.7) | −0.668 | 0.504 |
| B | 36 (92.3) | 136 (84.5) |
|
|
| C | 2 (5.1) | 11 (6.8) |
|
|
| Type of
malignancy |
|
|
|
|
|
Gallbladder cancer | 0 (0.0) | 8 (5.0) | 7.218 | 0.205 |
|
Cholangiocarcinoma | 10 (25.6) | 57 (35.4) |
|
|
|
Pancreatic cancer | 12 (30.8) | 29 (18.0) |
|
|
| Liver
cancer | 5 (12.8) | 16 (9.9) |
|
|
|
Ampullary cancer | 6 (15.4) | 21 (13.0) |
|
|
|
Metastatic carcer | 6 (15.4) | 30 (18.6) |
|
|
| Obstruction
site |
|
|
|
|
| High
obstruction | 15 (38.5) | 63 (39.1) | 0.006 | 0.939 |
| Low
obstruction | 24 (61.5) | 98 (60.9) |
|
|
| Obstruction length,
mm | 23.0
(15.0–35.0) | 21.0
(11.0–31.5) | −1.014 | 0.311 |
| Stent type |
|
|
|
|
| Plastic
stent | 6 (15.4) | 31 (19.3) | 5.736 | 0.125 |
| Metal
stent | 8 (20.5) | 28 (14.7) |
|
|
| Metal
stent and nasobiliary drainage | 14 (35.9) | 32 (19.9) |
|
|
| Nasal
biliary drainage | 11 (28.2) | 70 (43.5) |
|
|
| CA19-9 |
|
|
|
|
| ≥240
U/ml | 30 (76.9) | 73 (45.3) | 12.536 | <0.001 |
| <240
U/ml | 9 (23.1) | 88 (54.7) |
|
|
| CEA |
|
|
|
|
| ≥5
ng/ml | 21 (53.8) | 55 (34.2) | 5.163 | 0.023 |
| <5
ng/ml | 18 (46.2) | 106 (65.8) |
|
|
| WBC,
×109/l | 7.0 (5.3–8.5) | 6.2 (5.0–7.6) | −1.912 | 0.056 |
| NLR | 5.9 (4.2–8.9) | 3.5 (2.4–5.0) | −4.655 | <0.001 |
| HGB, g/l | 124.0
(111.0–140.0) | 125.0
(111.0–134.5) | −0.295 | 0.768 |
| TBIL, µmol/l | 203.0
(72.8–267.0) | 194.5
(97.5–305.2) | −0.544 | 0.586 |
| DBIL, µmol/l | 121.0
(74.8–163.7) | 86.9
(14.7–185.1) | −1.573 | 0.116 |
| ALB, g/l | 32.5(28.9–35) | 33.6
(30.0–37.3) | −1.221 | 0.222 |
| ALT, U/l |
133.3(98.5–193.0) | 114.0
(67.3–192.0) | −1.238 | 0.216 |
| AST, U/l | 120.2
(73.0–195.0) | 111.0
(54.9–206.6) | −0.683 | 0.495 |
| LDH, U/l | 527.0
(346.0–690.0) | 471.0
(375.0–644.0) | −0.791 | 0.429 |
| ALP, U/l | 401.3
(265.7–536.0) | 328.0
(220.1–544.9) | −0.937 | 0.349 |
| PT, sec | 12.4
(11.6–13.1) | 12.1
(11.3–13.3) | −0.578 | 0.563 |
Logistic regression model
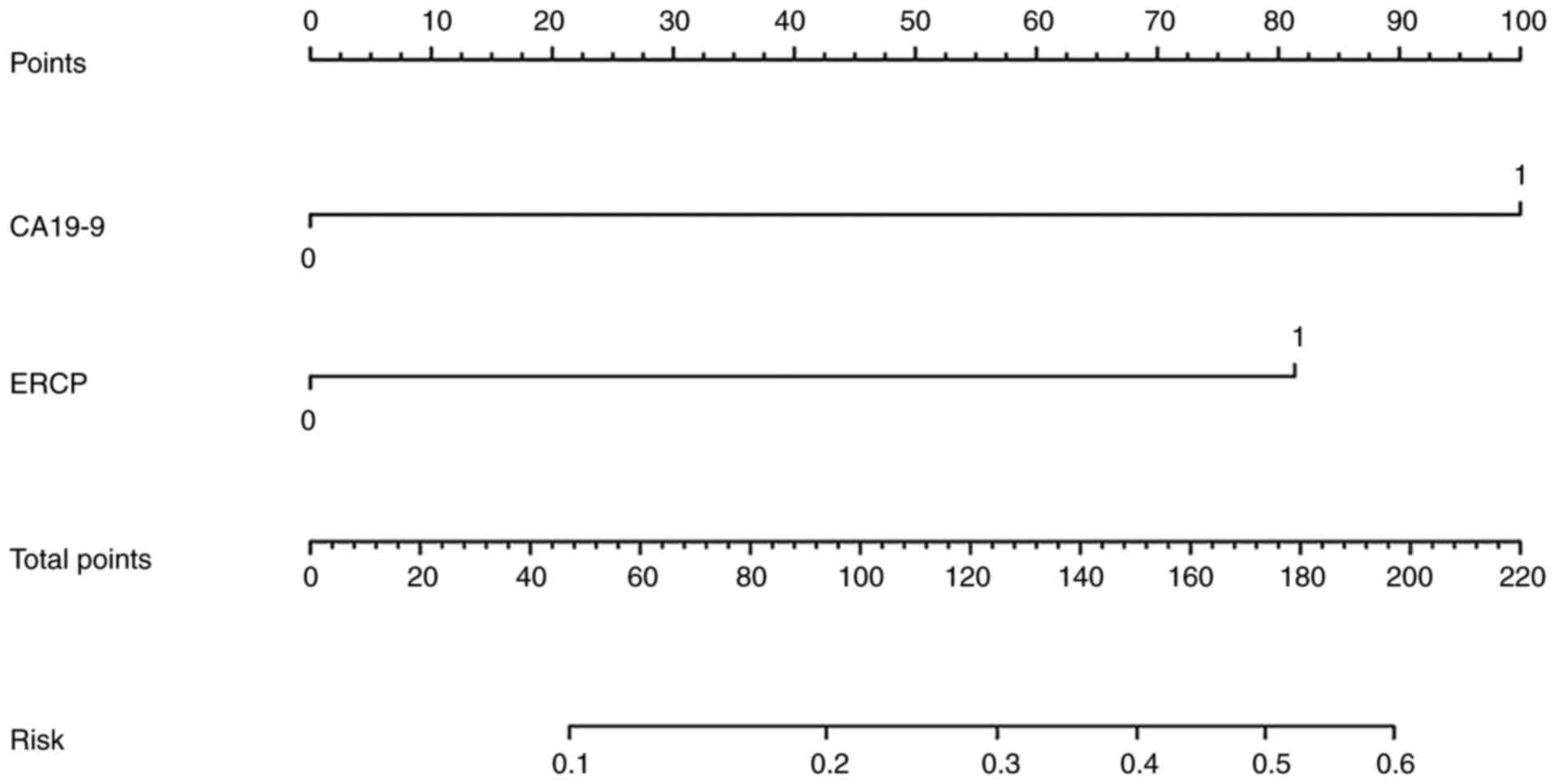
A total of two independent risk factors, ERCP
history and CA 19-9 levels, were identified through multifactorial
logistic regression analysis (Table
III). A logistic regression model was then constructed: Y=Logit
P=−3.899 + 1.690 × CA19-9 + 1.366 × ERCP history. To visualize the
model, a nomogram was created (Fig.
3).
 | Table III.Multivariate logistic regression
analysis. |
Table III.
Multivariate logistic regression
analysis.
| Variable | ß | SE | Wald | P-value | Exp(B) | 95% CI |
|---|
| CA19-9 | 1.690 | 0.457 | 13.685 | <0.001 | 5.417 | 2.213–13.259 |
| History of
ERCP | 1.366 | 0.430 | 10.081 | 0.001 | 3.919 | 1.687–9.106 |
| Liver
metastasis | 0.788 | 0.479 | 2.704 | 0.100 | 2.200 | 0.860–5.630 |
| NLR | 0.083 | 0.044 | 3.586 | 0.058 | 1.087 | 0.997–1.185 |
| CEA | 0.717 | 0.409 | 3.066 | 0.080 | 2.048 | 0.918–4.570 |
| Constant | −3.899 | 0.560 | 48.189 | <0.001 | 0.020 | - |
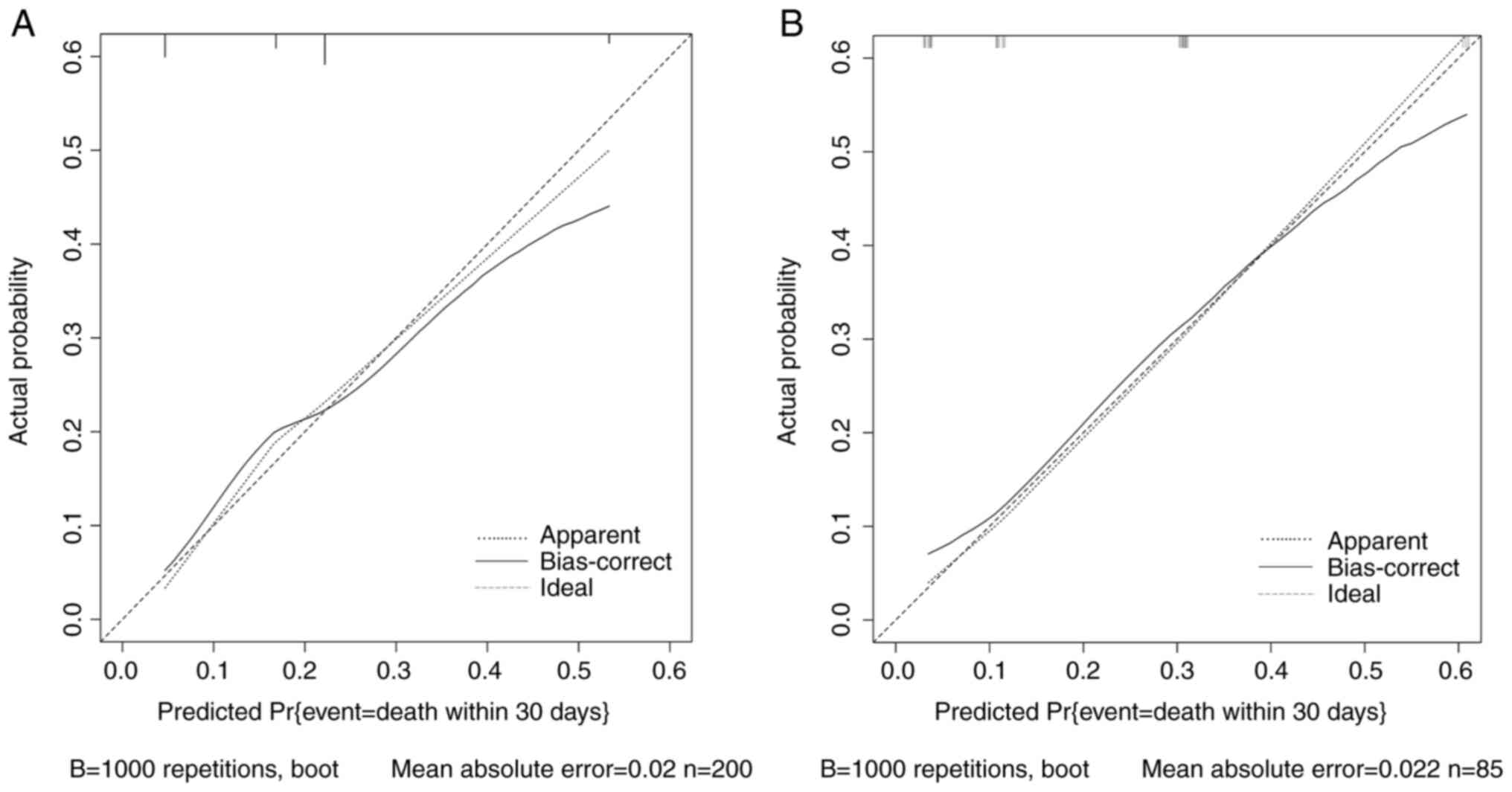
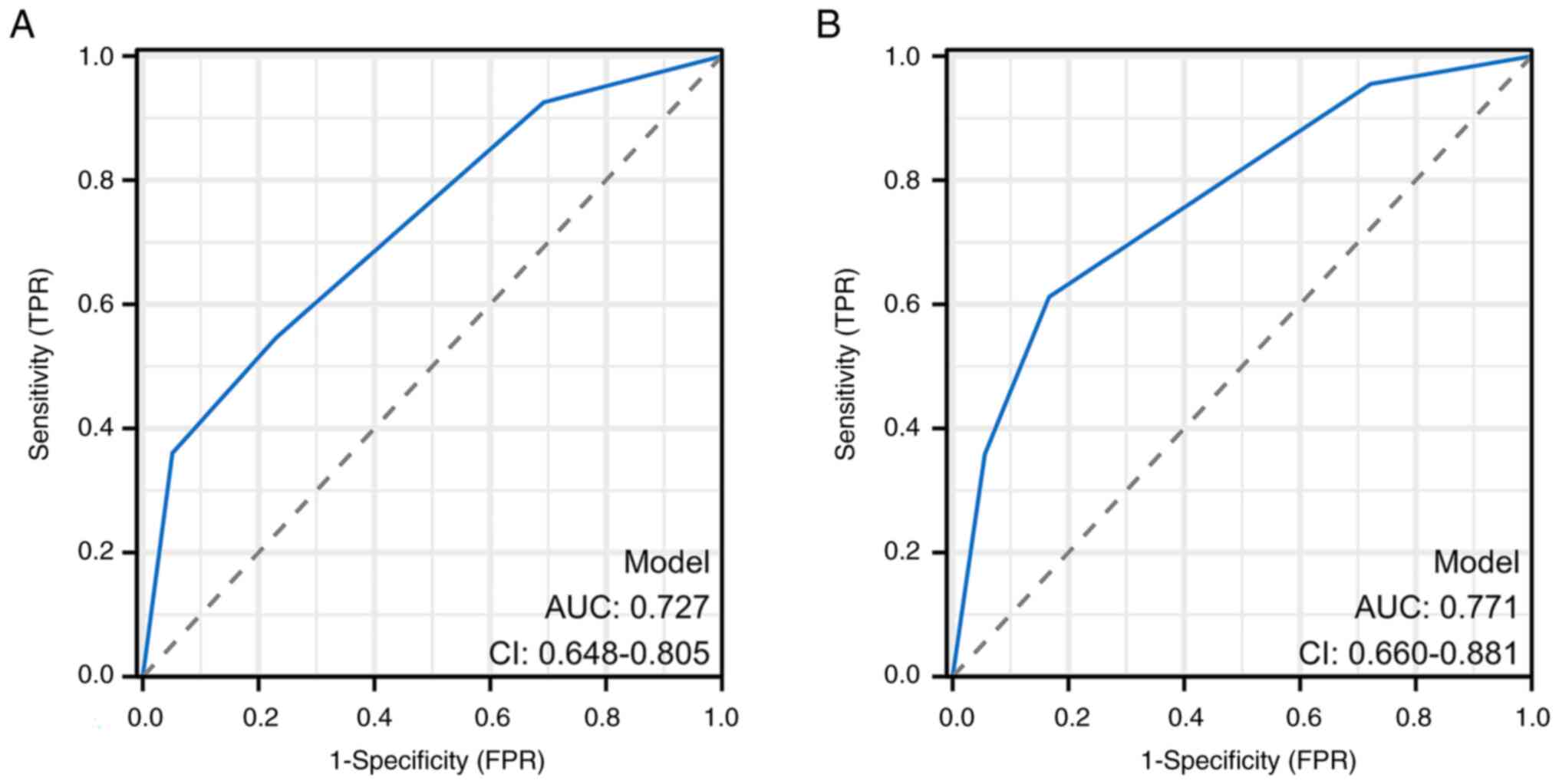
Logistic model calibration plots demonstrated no
statistically significant difference between predicted and true
values (Fig. 4). The Bootstrap
method revealed a c-value of 0.727 for the training group and 0.761
for the validation group, and the Hosmer-Leme show test
demonstrated a P-value of 0.934 for the training group and 0.915
for the validation group. Therefore, this indicated that the model
had good prediction performance. Furthermore, the AUC values for
each group determined using the ROC curves were 0.727 for the
training group and 0.771 for the validation group (Fig. 5; Table
IV).
 | Table IV.Prediction efficiency of the logistic
model training and validation groups. |
Table IV.
Prediction efficiency of the logistic
model training and validation groups.
| Variable | Training group | Validation
group |
|---|
| Sensitivity, % | 54.7 | 61.2 |
| Specificity, % | 76.9 | 83.3 |
| Accuracy, % | 59.0 | 65.0 |
| Area under the
curve | 0.727 | 0.771 |
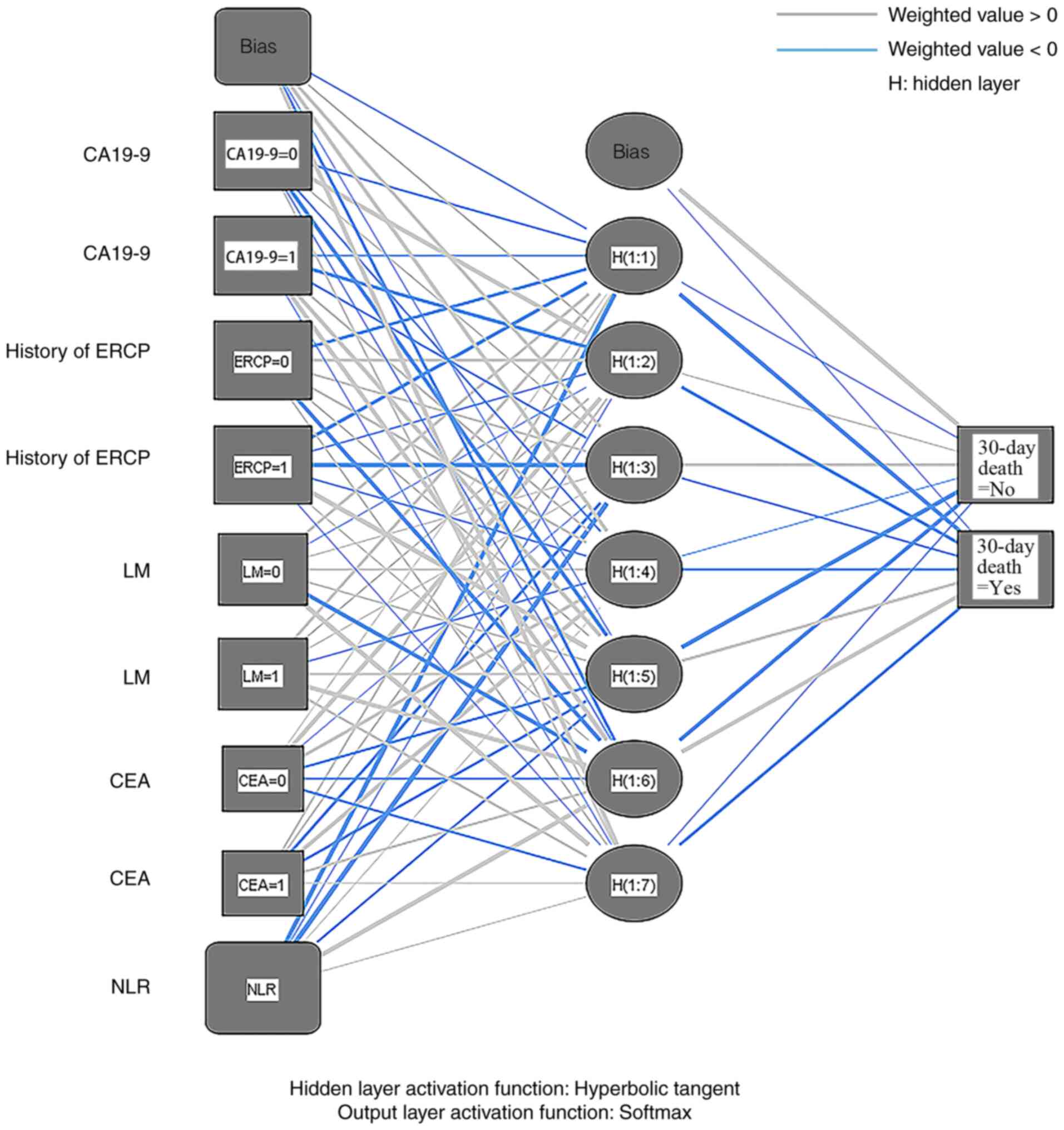
ANN model
ANN models were constructed based on the five
potential risk factors obtained from univariate analysis using
samples from the training and validation groups. Among them, NLR
was used as a covariate, and the remaining four variables were
dichotomous, including CA19-9 level, CEA level, liver metastasis
and history of ERCP surgery. The ANN model used in the present
study was a multilayer perceptron ANN, including an input layer
(five variables), an implicit layer and an output layer
(dichotomous endings) (Fig. 6).
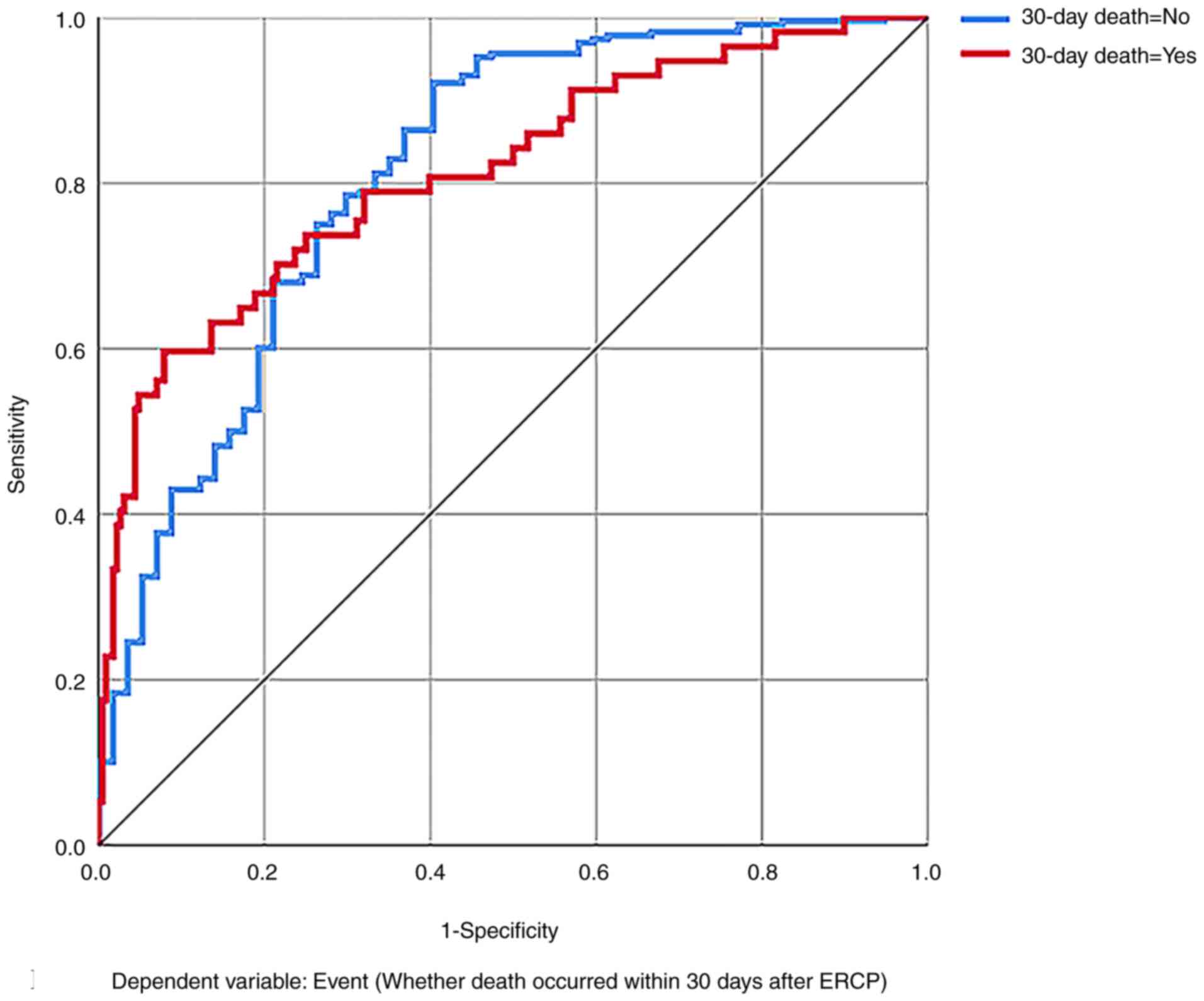
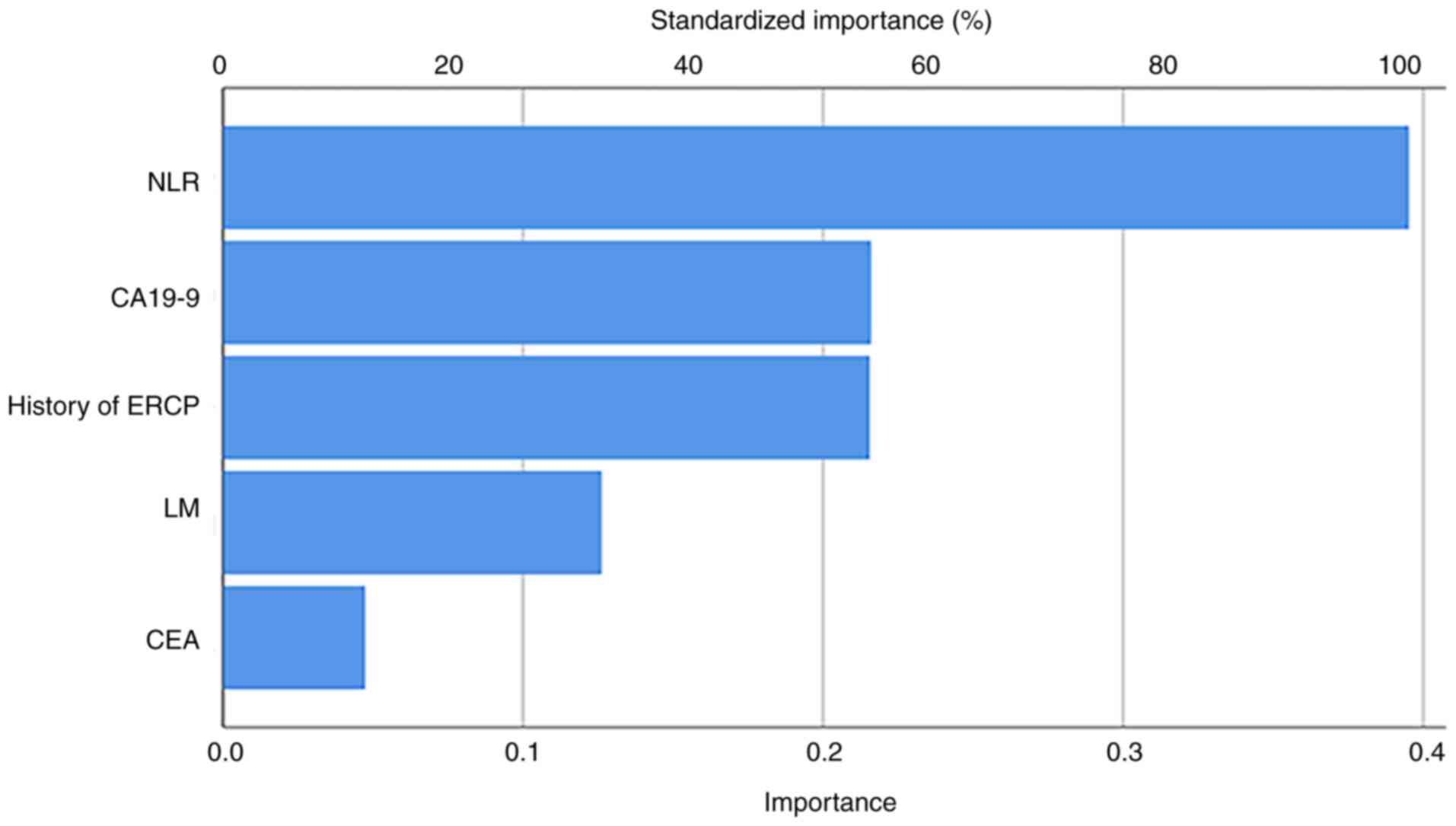
Moreover, the ANN model had an AUC value of 0.813 (Fig. 7), and the degree of importance of
the variables in the ANN model was expressed in terms of
significance and standardized significance in descending order
(Table V; Fig. 8). The prediction efficiency of the
ANN model is presented in Table
VI.
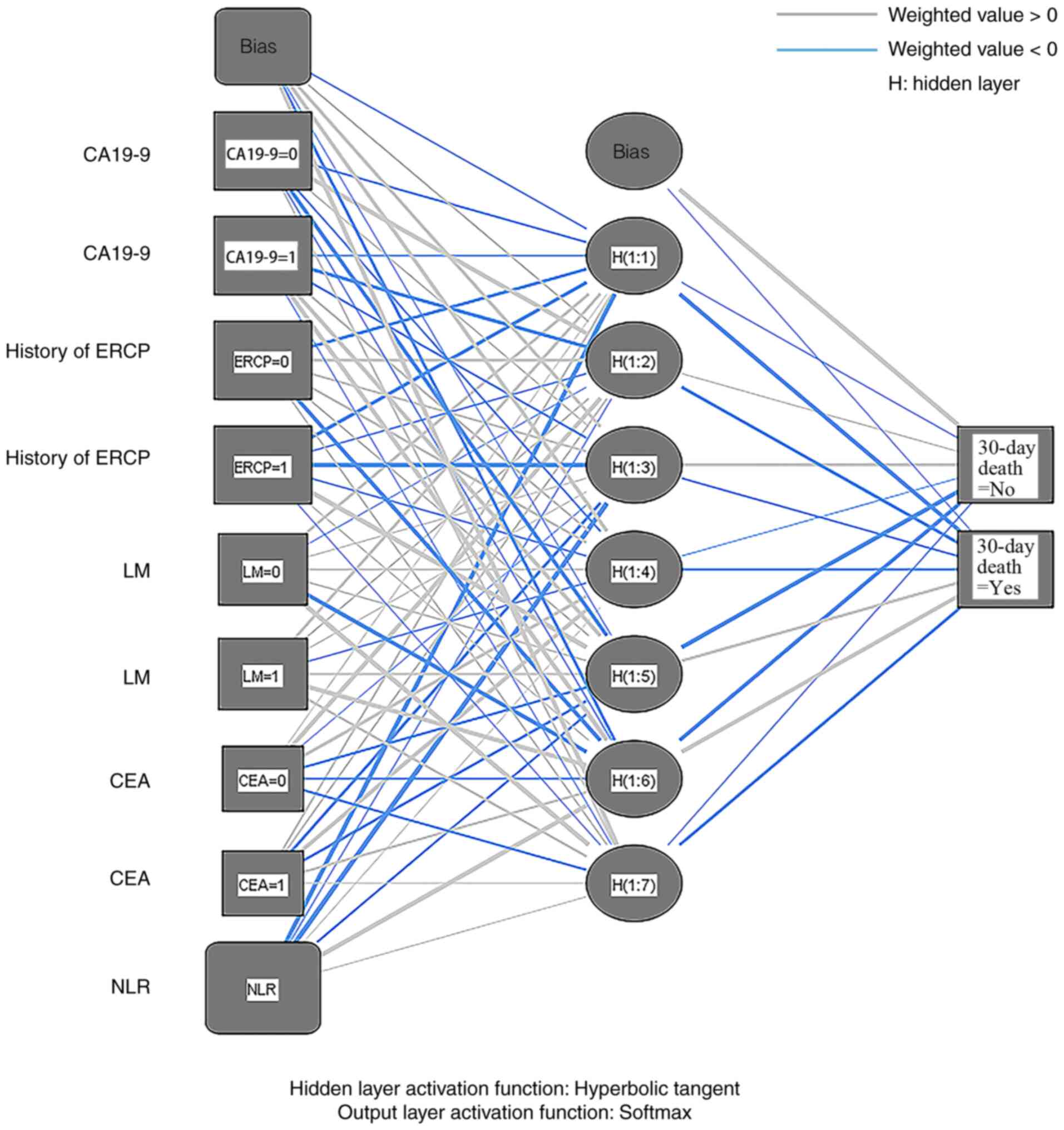 | Figure 6.Artificial neural network model for
predicting the risk of early death occurring within 30 days after
ERCP combined with biliary stenting. The first layer is the input
layer, the second layer is the hidden layer, using the hyperbolic
tangent function, and the third layer is the output layer, using
the softmax function. The grey connection lines indicate a positive
weight value, and the blue connection lines indicate a negative
weight value. CA19-9, cancer antigen 19-9; ERCP, endoscopic
retrograde cholangiopancreatography; LM, liver metastasis; CEA,
carcinoembryonic antigen; NLR, neutrophil-to-lymphocyte ratio; H,
hidden layer. |
 | Table V.Importance of independent variables
and normalization in the artificial neural network model. |
Table V.
Importance of independent variables
and normalization in the artificial neural network model.
| Variable | Importance | Standardized
importance, % |
|---|
| CA19-9 | 0.216 | 54.6 |
| History of
ERCP | 0.215 | 54.5 |
| Liver
metastasis | 0.126 | 31.9 |
| CEA | 0.047 | 12.0 |
| NLR | 0.395 | 100.0 |
 | Table VI.Prediction efficiency of the
artificial neural network model in the training and validation
groups. |
Table VI.
Prediction efficiency of the
artificial neural network model in the training and validation
groups.
| A, Training
group |
|---|
|
|---|
|
| Prediction |
|
|---|
|
|
|
|
|---|
| Actual
measurement | 0 | 1 | Correctness, % |
|---|
| 0 | 151 | 10 | 93.8 |
| 1 | 19 | 20 | 51.3 |
| Overall, % | 85.0 | 15.0 | 85.5 |
|
| B, Validation
group |
|
|
|
Prediction |
|
|
|
|
|
| Actual
measurement | 0 | 1 | Correctness,
% |
|
| 0 | 64 | 3 | 95.5 |
| 1 | 7 | 11 | 61.1 |
| Overall, % | 83.5 | 16.5 | 88.2 |
Validation and comparison of
models
The predictive performance of the logistic and ANN
models was internally and externally validated in the training and
validation groups, and the predictive abilities were compared
(Table VII). The accuracy of the
logistic model was 59.0 and 65.0% in the training and validation
groups, respectively, and the accuracy of the ANN model was 85.5
and 88.2% in the training and validation groups, respectively. The
latter was markedly higher than that of the logistic model,
indicating that the ANN model had a stronger overall predictive
ability. The sensitivity of the logistic model in the training and
validation groups was 54.7 and 61.2% in the training and validation
groups respectively, and the sensitivity of the ANN model was 51.3%
in the training group and 61.1% in the validation group; therefore,
the difference between the models was not notably different in the
same group. However, the sensitivity of the ANN model was still
slightly weaker, suggesting that it may have certain deficiencies
in the capture of positive samples. Furthermore, the specificity of
the logistic model was 76.9 and 83.3% in the training and
validation groups, respectively, while the specificity of the ANN
model was as high as 93.8 and 95.5% in the training and validation
groups, respectively. This indicates that the ANN model has an
improved predictive ability and a marked advantage in identifying
negative samples.
 | Table VII.Comparison of the prediction
performance between the logistic and ANN models. |
Table VII.
Comparison of the prediction
performance between the logistic and ANN models.
| A, Logistic
model |
|---|
|
|---|
| Group | Accuracy, % | Sensitivity, % | Specificity, % |
|---|
| Training | 59.0 | 54.7 | 76.9 |
| Validation | 65.0 | 61.2 | 83.3 |
|
| B, ANN
model |
|
| Group | Accuracy,
% | Sensitivity,
% | Specificity,
% |
|
| Training | 85.5 | 51.3 | 93.8 |
| Validation | 88.2 | 61.1 | 95.5 |
Discussion
MBO is a group of diseases in which the bile duct is
blocked or compressed by a malignant tumor, resulting in biliary
stricture or obstruction of bile drainage. Currently, ERCP is the
palliative treatment of choice for patients with MBO (5). ERCP treatment involves placement of
biliary stents, and plastic and metal stents are common options.
Studies have reported that there is no significant difference in
the use of metal and plastic stents in the effectiveness of biliary
drainage and risk of adverse events in patients who die within 30
days of ERCP treatment (21,22);
however, plastic stents are more cost-effective, providing
effective treatment and saving healthcare resources whilst reducing
the economic burden on patients and society (8,23).
Accurate prediction of prognosis after ERCP is of great importance
for clinical decision support and appropriate treatment selection.
Currently, there are few existing reports on predicting this risk
in patients with MBO. Therefore, the aim of the present study was
to construct a model to predict the risk of death within 30 days
after ERCP combined with biliary stent placement in patients with
MBO. The model utilized preoperative clinical data and employed
both logistic and ANN models. The predictive ability of these two
models was evaluated and compared.
In the present study, all indicators associated with
the risk factors, including history of previous ERCP surgery,
CA19-9 levels, CEA levels, liver metastasis and NLR, were easily
available before the surgery. The logistic model was presented
succinctly and intuitively through column-line graphs, whereas the
ANN model appeared to be complex and inconvenient to use. In both
the training and validation groups, the accuracy of the ANN model
(85.5 and 88.2%, respectively) was notably higher than that of the
logistic model (59.0 and 65.0%, respectively), suggesting that the
ANN model had a stronger overall predictive ability. This may be
attributed to the more complex structure and non-linear fitting
ability of the ANN model, allowing it to capture deeper features in
the data. However, it is important to note that ANN models may
overfit the training data, which potentially reduces the
generalization ability when dealing with new data (24). Sensitivity is an important measure
of the ability of a model to recognize positive samples. The
sensitivity of the logistic model in the training and validation
groups was 54.7 and 61.2%, respectively, whilst the sensitivity of
the ANN model was 51.3 and 61.1%, respectively. Despite the slight
increase in the sensitivity of the ANN model in the validation
group compared with the training group, the overall sensitivity of
both models was low, especially the sensitivity of the ANN model,
which was markedly lower than its specificity. This may indicate
certain limitations in the performance of the ANN model in the case
of an insufficient number of positive samples or a sample
imbalance. This also suggests the necessity of further studies to
be performed with large samples. The specificity of the ANN model
reached 93.8 and 95.5% in the training and validation groups,
respectively, which was notably higher than that of the logistic
model (76.9 and 83.3%, respectively). This indicated that the high
specificity of the ANN model provided a significant advantage in
reducing misdiagnosis rates, making it more suitable compared with
the logistic model for identifying patients who die within 30 days
after ERCP. The AUC value of the ANN model was 0.813, which was
higher than that of the logistic model (AUC, 0.727), indicating
that the ANN model had an improved performance in distinguishing
between positive and negative samples. The difference in the AUC
values further supports the superiority of the ANN model in terms
of its overall performance, especially when dealing with complex
data structures.
In addition, the ability of the ANN model to assign
weights to predictor variables could aid in the identification of
variables among the numerous risk factors that have the greatest
impact on outcome. This is important for predicting early death
within 30 days after ERCP. Conversely, the logistic model could
only account for the impact of changes within variables on outcome
(25,26). For example, in the present study,
the ANN model identified NLR as the most important factor in
predicting the risk of death after ERCP in patients with MBO (with
an importance of 0.395 and a standardized importance of 100.0%),
but the logistic model could only account for the effect of risk
factors on outcomes by considering the results of the model and the
OR values for each indicator.
In summary, the ANN model in the present study
generally outperformed the logistic model in terms of prediction
performance. The ANN model had strong non-linear approximation
ability and was suitable for solving non-linear problems (27); it could self-learn and adjust
according to the degree of error deviation to select the best
model. By contrast, the logistic model was more suitable for
datasets with relatively simple features and strong linear
correlation. Nevertheless, there are certain disadvantages of using
ANN models. First, there is a risk of overfitting the model, which
may lead to overconfident predictions (28). Secondly, ANN models tend to be more
complex in clinical applications compared with logistic models,
which are more convenient. However, Pergialiotis et al
(29) reported that these issues
can be addressed by large sample studies. Small datasets may not be
applicable to large cohorts, but the reverse is also possible.
Based on multifactorial regression analysis, the
logistic model incorporated two independent risk factors: CA19-9
and a history of ERCP surgery. ERCP combined with biliary stenting
does not prevent tumor progression (30,31),
and ERCP surgery disrupts the biliary mucosal defense system as
well as the physiological barrier between the bile ducts and
intestines, which makes it easier for bacteria to invade the
biliary system and cause prolonged inflammatory irritation of the
bile ducts. These factors may accelerate the progression and
metastasis of malignant tumors and severely affect the prognosis
(32–34). CA19-9 has been recognized as an
important prognostic factor in several tumors, including
gallbladder, bile duct, pancreatic and bladder cancer (35–37).
The present study demonstrated that a CA19-9 level of ≥240 U/ml was
an independent predictor of death within 30 days after ERCP in
patients with MBO [OR (95% CI), 5.417 (2.213–13.259); P<0.001].
Other potential risk factors have also been reported as prognostic
predictors for biliopancreas-related malignancies, including NLR,
CEA and liver metastases (23,38,39).
These potential risk factors were not selected into the logistic
model after multifactorial regression analysis but were important
predictive variables in the ANN model. ANN models can obtain enough
information from a set of variables to construct a predictive
model, as ANN algorithms can derive complex and abstract non-linear
relationships from the variables (40). The NLR is regarded as an amplifier
of the systemic inflammatory response (41,42).
Neutrophils influence the activation and recruitment of
inflammatory cells through cytokines and chemokines, which in turn
affects the proliferation and metastasis of tumor cells (43,44).
By contrast, lymphocytes monitor the tumor immune microenvironment
and inhibit the maturation of tumor cells, and a decrease in the
total number of lymphocytes in the blood often predicts a poor
prognosis (41,45). Moreover, elevated CEA levels are a
prognostic factor for poor survival in certain patients with
advanced malignancies (46,47). The incidence of liver metastases
also increases with decreasing pathological differentiation,
especially in cases of malignant biliary obstruction, and it has
been reported that the survival time of patients with liver
metastasis in MBO is significantly shortened compared with those
without liver metastasis (48,49).
There are several limitations of the present study.
First, the data were all retrospective, which is less persuasive
than prospective data. Second, the samples used were all from a
single center, were limited in number and were not validated with
data external to the model, which may limit the generalizability of
the model. Therefore, caution must be exercised in applying the
findings to a wider population. Third, there may be a certain
degree of subjectivity in the assessment of certain predictor
variables, such as abdominal pain and ECOG score. Fourth, the ANN
model constructed in the present study is the simplest one and
needs further optimization. Due to the ‘black box’ nature of the
ANN model, its internal processes involve complex neuronal
computations and parameter adjustments, making it difficult to
describe the input-output mapping using simple rules. This can pose
challenges in the practical interpretation and application of the
model; therefore, future studies should construct a simple and
easy-to-use software or tool to facilitate the use of the ANN
model. To overcome these limitations, prospective, multicenter and
large-sample studies would be beneficial. Such a study design could
provide more robust and reliable results that would optimize the
model and more accurately predict the risk of death within 30 days
after ERCP in patients with MBO.
In conclusion, the present study constructed and
compared the performance of logistic and ANN models in predicting
the risk of death within 30 days after ERCP combined with biliary
stent placement in patients with MBO. The ANN model outperformed
the logistic model in terms of overall predictive ability, accuracy
and specificity. The ANN model was able to efficiently capture the
complex non-linear relationships in the data, highlight important
predictors such as NLR, and provide more accurate early warning
information for clinical decision-making. In the future,
multi-center and large-sample prospective validation should be
performed and simple and easy-to-use ANN model tools should be
developed to further improve the generalization ability and
operability of the model, which will be helpful for its wide
application in clinical practice. Temporary alternative efficient
and economical methods of biliary decompression should be
recommended for high-risk patients who die within 30 days.
Acknowledgements
Not applicable.
Funding
The present study was supported by the ‘Optimization of
degradation-controllable magnesium alloy microparticles and their
synergistic TACE against hepatocellular carcinoma and its
mechanism’ project (grant no. 2023SF13).
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
YM, JQ, XZ, KL, YL, XY, YB and BC contributed to the
conception and design of the study. Material preparation, data
collection and analysis were performed by YM, JQ and XZ. The first
draft of the manuscript was written by YM. XY, KL and YL proposed
amendments to the paper. YB and BC designed the study, provided
guidance on manuscript writing, and contributed to its revision. YM
and BC confirm the authenticity of all the raw data. All authors
read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of the General Hospital of Ningxia Medical University
(approval no. KYLL-2023-0450).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Termsinsuk P, Charatcharoenwitthaya P and
Pausawasdi N: Development and validation of a 90-day mortality
prediction model following endobiliary drainage in patients with
unresectable malignant biliary obstruction. Front Oncol.
12:9223862022. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Farani M, Saldi SRF, Maulahela H, Abdullah
M, Syam AF and Makmum D: Survival, stent patency, and
cost-effectiveness of plastic biliary stent versus metal biliary
stent for palliation in malignant biliary obstruction in a
developing country tertiary hospital. JGH Open. 5:959–965. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Dar FS, Abbas Z, Ahmed I, Atique M, Aujla
UI, Azeemuddin M, Aziz Z, Bhatti ABH, Bangash TA, Butt AS, et al:
National guidelines for the diagnosis and treatment of hilar
cholangiocarcinoma. World J Gastroenterol. 30:1018–1042. 2024.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Drapek LC, Kerlan RK Jr and Acquisto S:
Guidelines for biliary stents and drains. Chin Clin Oncol. 9:92020.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Harvey PR, Baldwin S, Mytton J, Dosanjh A,
Evison F, Patel P and Trudgill NJ: Higher volume providers are
associated with improved outcomes following ERCP for the palliation
of malignant biliary obstruction. EClinicalMedicine. 18:1002122020.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
On W, Saleem MA, Hegade VS, Huggett MT,
Paranandi B and Everett SM: Factors predicting 30-day mortality
after ERCP in patients with inoperable malignant hilar biliary
obstruction: A single tertiary referral centre experience and
systematic review. BMJ Open Gastroenterol. 9:e0008782022.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Lam R and Muniraj T: Fully covered metal
biliary stents: A review of the literature. World J Gastroenterol.
27:6357–6373. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lee TH, Moon JH and Park SH: Biliary
stenting for hilar malignant biliary obstruction. Dig Endosc.
32:275–286. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kalaitzakis E: All-cause mortality after
ERCP. Endoscopy. 48:987–994. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zhu Z, Hu K, Zhao F, Liu W, Zhou H, Zhu Z
and Li H: Machine learning-based nomogram for 30-day mortality
prediction for patients with unresectable malignant biliary
obstruction after ERCP with metal stent: A retrospective
observational cohort study. BMC Surg. 23:2602023. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Luo Y, Tan H, Yu T, Tian J and Shi H: A
novel artificial neural network prognostic model based on a
cancer-associated fibroblast activation score system in
hepatocellular carcinoma. Front Immunol. 13:9270412022. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Rajula HSR, Verlato G, Manchia M,
Antonucci N and Fanos V: Comparison of conventional statistical
methods with machine learning in medicine: Diagnosis, drug
development, and treatment. Medicina (Kaunas). 56:4552020.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ataei A, Deng J and Muhammad W: Liver
cancer risk quantification through an artificial neural network
based on personal health data. Acta Oncol. 62:495–502. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kitano R, Inoue T, Ibusuki M, Kobayashi Y,
Ohashi T, Sumida Y, Nakade Y, Ito K and Yoneda M: Safety and
efficacy of endoscopic retrograde cholangiopancreatography in
patients with performance status 4. Dig Dis Sci. 66:1291–1296.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kumada T, Toyoda H, Tada T, Yasuda S and
Tanaka J: Changes in background liver function in patients with
hepatocellular carcinoma over 30 years: Comparison of child-pugh
classification and albumin bilirubin grade. Liver Cancer.
9:518–528. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Chan E, Neeman T and Thomson A: Follow-up
to determine unplanned hospitalization and complications after
endoscopic retrograde cholangiopancreatography. ANZ J Surg.
88:E142–E146. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Teoh AYB, Napoleon B, Kunda R, Arcidiacono
PG, Kongkam P, Larghi A, Van der Merwe S, Jacques J, Legros R,
Thawee RE, et al: EUS-Guided Choledocho-duodenostomy using lumen
apposing stent versus ERCP with covered metallic stents in patients
with unresectable malignant distal biliary obstruction: A
multicenter randomized controlled trial (DRA-MBO Trial).
Gastroenterology. 165:473–482. e4722023. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Fu Z, Song J, Pi Y, Sun X, Liu M, Xiao Z
and Chen J: A risk prediction model for post-endoscopic retrograde
cholangiopancreatography pancreatitis after stent insertion for
malignant biliary obstruction: Development and validation. Dig Dis
Sci. 68:1574–1584. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Krill TS, Crain R, Al-Saadi Y, Stubbs S,
Roark R, Chatila A, Haddad C, Kaushik C, Marcondes F, Guturu P and
Parupudi S: Predictors of 30-day readmission after inpatient
endoscopic retrograde cholangiopancreatography: A single-center
experience. Dig Dis Sci. 65:1481–1488. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Zhou HF, Lu J, Zhu HD, Guo JH, Huang M, Ji
JS, Lv WF, Li YL, Xu H, Chen L, et al: Early warning models to
estimate the 30-day mortality risk after stent placement for
patients with malignant biliary obstruction. Cardiovasc Intervent
Radiol. 42:1751–1759. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kanno Y, Koshita S, Ogawa T, Kusunose H,
Masu K, Sakai T, Yonamine K, Miyamoto K, Murabayashi T, Kozakai F,
et al: Inside plastic stents versus metal stents for treating
unresectable malignant perihilar biliary obstructions: A
retrospective comparative study. Clin Endosc. 53:735–742. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Park CH, Park SW, Jung JH, Jung ES, Kim JH
and Park DH: Comparative efficacy of various stents for palliation
in patients with malignant extrahepatic biliary obstruction: A
systematic review and network meta-analysis. J Pers Med. 11:862021.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Gong M, Li Q, Xu Y and Fu Y: The
evaluation of clinical status of endoscopic retrograde
cholangiography for the placement of metal and plastic stents in
cholangiocarcinoma therapy. Comput Math Methods Med.
2022:57414372022. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Serghiou S and Rough K: Deep learning for
epidemiologists: An introduction to neural networks. Am J
Epidemiol. 192:1904–1916. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Jiang H, Guo J, Li J, Li C, Du W, Canavese
F, Baker C, Ying H and Hua J: Artificial neural network modeling to
predict neonatal metabolic bone disease in the prenatal and
postnatal periods. JAMA Netw Open. 6:e22518492023. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Liu X, Wang X, Yu L, Hou Y, Jiang Y, Wang
X, Han J and Yang Z: A novel prognostic score based on artificial
intelligence in hepatocellular carcinoma: A long-term follow-up
analysis. Front Oncol. 12:8178532022. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Tu JV: Advantages and disadvantages of
using artificial neural networks versus logistic regression for
predicting medical outcomes. J Clin Epidemiol. 49:1225–1231. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Cao B, Zhang KC, Wei B and Chen L: Status
quo and future prospects of artificial neural network from the
perspective of gastroenterologists. World J Gastroenterol.
27:2681–2709. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Pergialiotis V, Pouliakis A, Parthenis C,
Damaskou V, Chrelias C, Papantoniou N and Panayiotides I: The
utility of artificial neural networks and classification and
regression trees for the prediction of endometrial cancer in
postmenopausal women. Public Health. 164:1–6. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Canakis A and Sharaiha RZ: Radiofrequency
ablation for pancreatobiliary disease: An updated review. Ann
Gastroenterol. 36:497–503. 2023.PubMed/NCBI
|
|
31
|
Nabi Z and Reddy DN: Endoscopic palliation
for biliary and pancreatic malignancies: Recent advances. Clin
Endosc. 52:226–234. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Grein JD and Murthy RK: New developments
in the prevention of gastrointestinal scope-related infections.
Infect Dis Clin North Am. 32:899–913. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Labib PL, Goodchild G and Pereira SP:
Molecular pathogenesis of cholangiocarcinoma. BMC Cancer.
19:1852019. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Özcan Ö and Arikan S: Determining the risk
factors of complications due to endoscopic retrograde
cholangiopancreatography. Cureus. 16:e516662024.PubMed/NCBI
|
|
35
|
Agrawal S, Gupta A, Gupta S, Goyal B,
Siddeek RAT, Rajput D, Chauhan U, Kishore S, Gupta M and Kant R:
Role of carbohydrate antigen 19-9, carcinoembryonic antigen, and
carbohydrate antigen 125 as the predictors of resectability and
survival in the patients of carcinoma gall bladder. J Carcinog.
19:42020. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Bekki Y, Von Ahrens D, Takahashi H,
Schwartz M and Gunasekaran G: Recurrent intrahepatic
cholangiocarcinoma-review. Front Oncol. 11:7768632021. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Yang H, Li W, Ren L, Yang Y, Zhang Y, Ge
B, Li S, Zheng X, Liu J, Zhang S, et al: Progress on diagnostic and
prognostic markers of pancreatic cancer. Oncol Res. 31:83–99. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Kubo S, Shinkawa H, Asaoka Y, Ioka T,
Igaki H, Izumi N, Itoi T, Unno M, Ohtsuka M, Okusaka T, et al:
liver cancer study group of japan clinical practice guidelines for
intrahepatic cholangiocarcinoma. Liver Cancer. 11:290–314. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Zhu J, Wang D, Liu C, Huang R, Gao F, Feng
X, Lan T, Li H and Wu H: Development and validation of a new
prognostic immune-inflammatory-nutritional score for predicting
outcomes after curative resection for intrahepatic
cholangiocarcinoma: A multicenter study. Front Immunol.
14:11655102023. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Bai Z, Yin Y, Xu W, Cheng G and Qi X:
Predictive model of in-hospital mortality in liver cirrhosis
patients with hyponatremia: An artificial neural network approach.
Sci Rep. 14:287192024. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Li Y, Xu T and Wang X, Jia X, Ren M and
Wang X: The prognostic utility of preoperative
neutrophil-to-lymphocyte ratio (NLR) in patients with colorectal
liver metastasis: A systematic review and meta-analysis. Cancer
Cell Int. 23:392023. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Saputra HM, Hidayatullah F, Kloping YP,
Renaldo J, Chung E and Hakim L: Prognostic value of
neutrophil-to-lymphocyte ratio (NLR) in penile cancer: A systematic
review and meta-analysis. Ann Med Surg (Lond).
81:1043352022.PubMed/NCBI
|
|
43
|
Buonacera A, Stancanelli B, Colaci M and
Malatino L: Neutrophil to lymphocyte ratio: An emerging marker of
the relationships between the immune system and diseases. Int J Mol
Sci. 23:36362022. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Wu L, Saxena S and Singh RK: Neutrophils
in the tumor microenvironment. Adv Exp Med Biol. 1224:1–20. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Mouchli M, Reddy S, Gerrard M, Boardman L
and Rubio M: Usefulness of neutrophil-to-lymphocyte ratio (NLR) as
a prognostic predictor after treatment of hepatocellular carcinoma.
Review article. Ann Hepatol. 22:1002492021. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Ney A, Garcia-Sampedro A, Goodchild G,
Acedo P, Fusai G and Pereira SP: Biliary strictures and
cholangiocarcinoma-untangling a diagnostic conundrum. Front Oncol.
11:6994012021. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Tarighati E, Keivan H and Mahani H: A
review of prognostic and predictive biomarkers in breast cancer.
Clin Exp Med. 23:1–16. 2023.PubMed/NCBI
|
|
48
|
Zu QQ, Zhang JX, Wang B, Ye W, Liu S and
Shi HB: Percutaneous transpapillary biliary stent placement for
distal malignant biliary obstruction: Outcomes and survival
analysis. Turk J Gastroenterol. 30:714–721. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Singh I, Chou JF, Capanu M, Park J, Yu KH,
Varghese AM, Park W, Zervoudakis A, Keane F, Rolston VS, et al:
Morbidity and mortality in patients with stage IV pancreatic
adenocarcinoma and acute cholangitis: Outcomes and risk
prognostication. Pancreatology. 24:608–615. 2024. View Article : Google Scholar : PubMed/NCBI
|