Introduction
Cervical cancer ranks among the leading causes of
female cancer-associated mortality worldwide, especially in
low-income countries and populations from socioeconomically
disadvantaged areas, thereby posing a serious threat to women's
health (1,2). Surgery via radical hysterectomy and
systematic pelvic lymphadenectomy currently serves as the standard
treatment for early-stage cervical cancer. In recent decades,
minimally invasive approaches have become increasingly accepted and
implemented in the global management of early-stage gynecologic
cancer. Philp et al (3)
previously compared the safety, morbidity and survival outcomes of
abdominal radical hysterectomy (ARH) and laparoscopic radical
hysterectomy (LRH), revealing lower short-term morbidity and
similar survival outcomes in the LRH group compared with ARH
(3). Jensen et al (4) revealed that the adoption of robotic
minimally invasive surgery (MIS) for early-stage cervical cancer
was not associated with increased risk of recurrence or a reduction
in survival outcomes.
Prior to 2016, our gynecological departments
(Department of Gynecology, Jinhua Maternity and Child Health Care
Hospital, and Department of Gynecology, Jinhua Hospital of Zhejiang
University; both Jinhua, China) used minimally invasive methods
with a uterine manipulator to perform radical surgery for cervical
cancer; however, since a number of cases of short-term central
recurrence were subsequently observed, the surgical approach was
revised. As of 2017, utilization of the uterine manipulator, myoma
drill and vaginal cuff was discontinued. Following this
modification, a notable decline in the incidence of central
recurrence was detected among patients. Notably, the Laparoscopic
Approach to Cervical Cancer (LACC) trial in 2018, which focused on
the oncological safety of MIS for early-stage cervical cancer,
indicated that the abdominal approach conferred a survival
advantage over MIS (5). In light of
these unexpected findings from the LACC trial, the majority of
gynecologic oncology centers across Europe and the United States
revised their clinical protocols regarding the management of women
with early-stage cervical cancer, reversing from minimally invasive
techniques to the previously established abdominal surgical
approach (6–8). In conventional MIS, the vagina is
accessed laparoscopically above the manipulator, which can lead to
exposure of the peritoneal cavity to tumor cells through
insufflation of carbon dioxide. Potential tumor spillage into the
peritoneal cavity may underlie the inferior outcomes of MIS.
However, given the advantages of laparoscopic surgery, a
significant number of patients select MIS as the preferred mode of
surgical treatment. Combined with data from our analysis of
patients with cervical cancer who underwent LRH showing a decreased
rate of tumor recurrence (Hu et al, unpublished data), the
current study provides a detailed evaluation of the oncologic
outcomes of patients with early cervical cancer undergoing
laparoscopic surgery incorporating protective methods to avoid
tumor spread with a median follow-up time of 51 months (range,
30–72 months) after surgery.
Materials and methods
Patient selection
This multicenter (Department of Gynecology, Jinhua
Maternity and Child Health Care Hospital, and Department of
Gynecology, Jinhua Hospital of Zhejiang University) study involved
a retrospective analysis of patients diagnosed with cervical cancer
who received treatment at between January 2017 and June 2020.
Patients eligible for inclusion in the study were
those diagnosed with IA1 lymphovascular space invasion [LVSI (+)]
to IIA1 and IIIC1p cervical cancer [International Federation of
Gynecology and Obstetrics (FIGO) 2018 (9)] who underwent LRH (type B-C). The
exclusion criteria included cases with tumor sizes >4 cm, a past
history of cervical colonization within 2 years, previous
chemotherapy or radiation, and conversion from MIS to laparotomy. A
total of 350 patients were identified who underwent LRH with
complete pelvic lymphadenectomy. All eligible patients were
informed of the potential complications, benefits and risks of both
ARH and LRH procedures before enrollment. The operating time was
recorded from the first skin incision to final closure. The tumor
diameter was determined with the aid of pelvic MRI scans. Operative
blood loss was estimated by collecting blood into suction bottles
during the surgical procedure.
Surgical techniques
All surgical interventions were conducted by five
proficient gynecologists. Patients were placed in the Trendelenburg
position at an angle of 30°. After general anesthesia, the vaginal
cuff was created in the upper third of the vaginal region for
patients with exophytic cervical cancer (tumor size >2 cm).
Subsequently, the laparoscopic procedure was conducted using five
trocars.
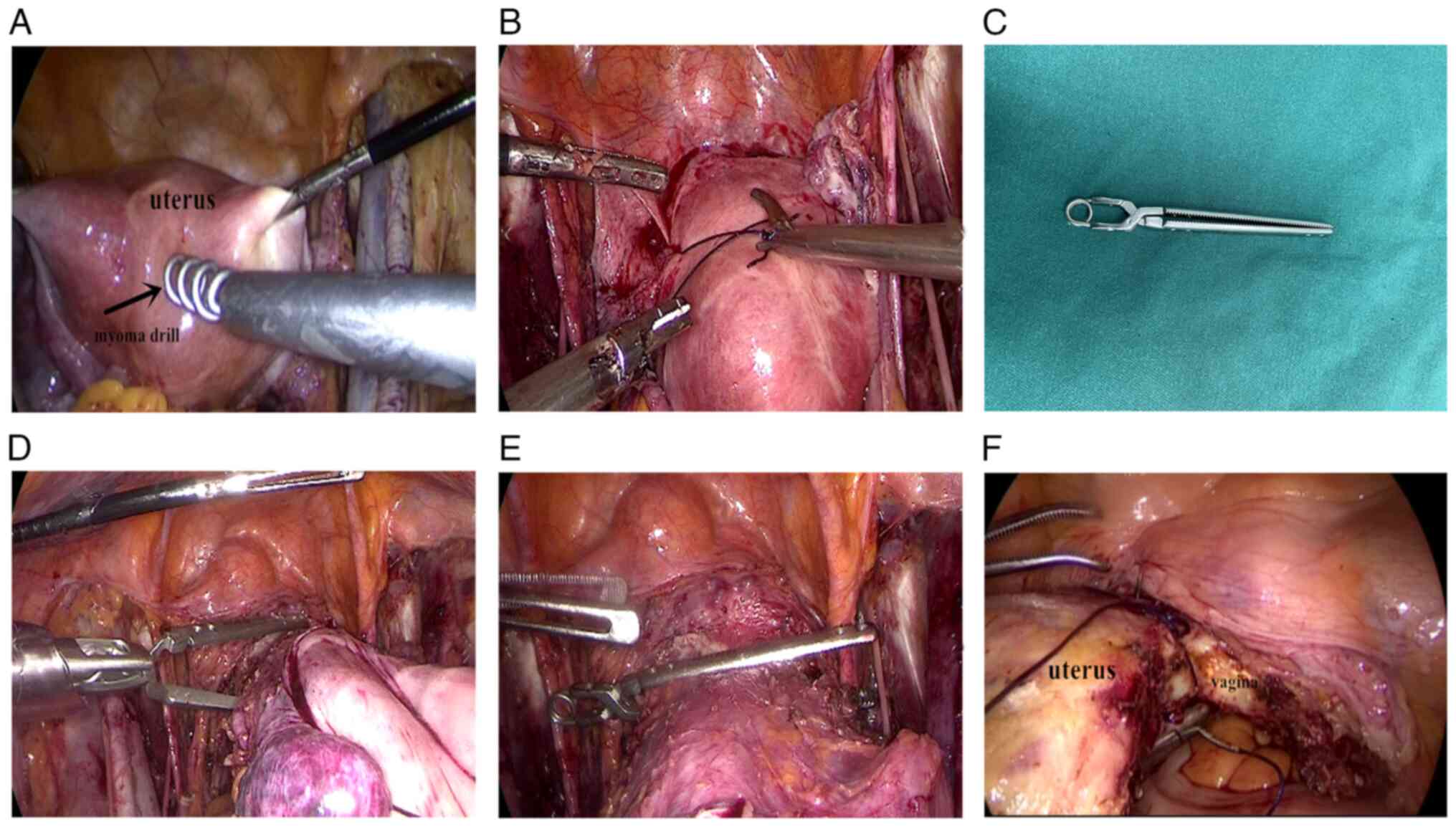
Initially, a myoma drill was applied (Fig. 1A) to grip the uterus for
manipulation purposes; however, to prevent uterine tearing, and
potential urologic and vascular complications associated with the
use of a myoma drill, the approach was modified to incorporate
thread fixation of the uterus (Fig.
1B), facilitating laparoscopic manipulation. During surgery,
the use of a uterine manipulator was avoided, while using the
remaining components of the MIS procedure. In addition, during the
operation, excised specimens, such as lymph nodes, were placed in a
specimen bag. In the final step before removal of the uterus, a
special clamp was used to secure the vaginal tube in cases of
endophytic type and ulcerative type cervical cancer (tumor size ≤2
cm; Fig. 1C-E). Cervical cancer
classification was based on clinical observations with ulcerative
type cervical cancer referring to cancerous tissue that developed
ulcers. To ensure that the clamp remained in place during the
surgery, both ends were fixed. During the later stages of the
process, vaginal suturing was performed (Fig. 1F) prior to colpotomy in patients
with smaller tumors (≤2 cm).
The steps incorporated (collection of excised
specimens in a specimen bag, vaginal cuffing, vaginal suturing and
clamping) were specifically designed to prevent tumor spillage
during laparoscopic procedures. Following colpotomy, the vaginal
cuff was secured above the special clamp, enabling the vaginal
delivery of the specimen. The specimens included the uterus,
fallopian tubes, a section of the vagina, parametrium and pelvic
lymph nodes.
Statistical analysis
Statistical analyses were conducted using SPSS
version 17.0 (SPSS, Inc.) Data were summarized using descriptive
statistics. For time-to-event data, Kaplan-Meier estimates were
provided. The estimates of hazard ratio (HR) and its 95% confidence
interval (CI) were calculated using Cox proportional hazards model,
and corresponding P-values were calculated using the log-rank test.
P<0.05 was considered to indicate a statistically significant
difference.
Results
Between January 2017 and June 2020, a total of 350
patients were recruited who were diagnosed with cervical cancer and
underwent radical hysterectomy for stages IA1 LVSI (+) to IIA1. The
baseline clinical characteristics of all patients are summarized in
Table I. Overall, 83 patients
(23.71%) were subjected to radiotherapy and/or adjuvant
chemoradiation. After radical hysterectomy, 53 patients underwent
brachytherapy and teletherapy, and 30 received chemotherapy
alongside brachytherapy and teletherapy. Over a median follow-up
period of 51 months (range, 30–72 months), five patients were lost
to follow-up and three refused treatment following surgery (these
patients were censored in the Kaplan-Meier analyses), the
disease-free survival (DFS) and overall survival rates (OS) were
95.71% (335/350) and 98.86% (346/350), respectively. The
peri-operative outcomes of the study population are summarized in
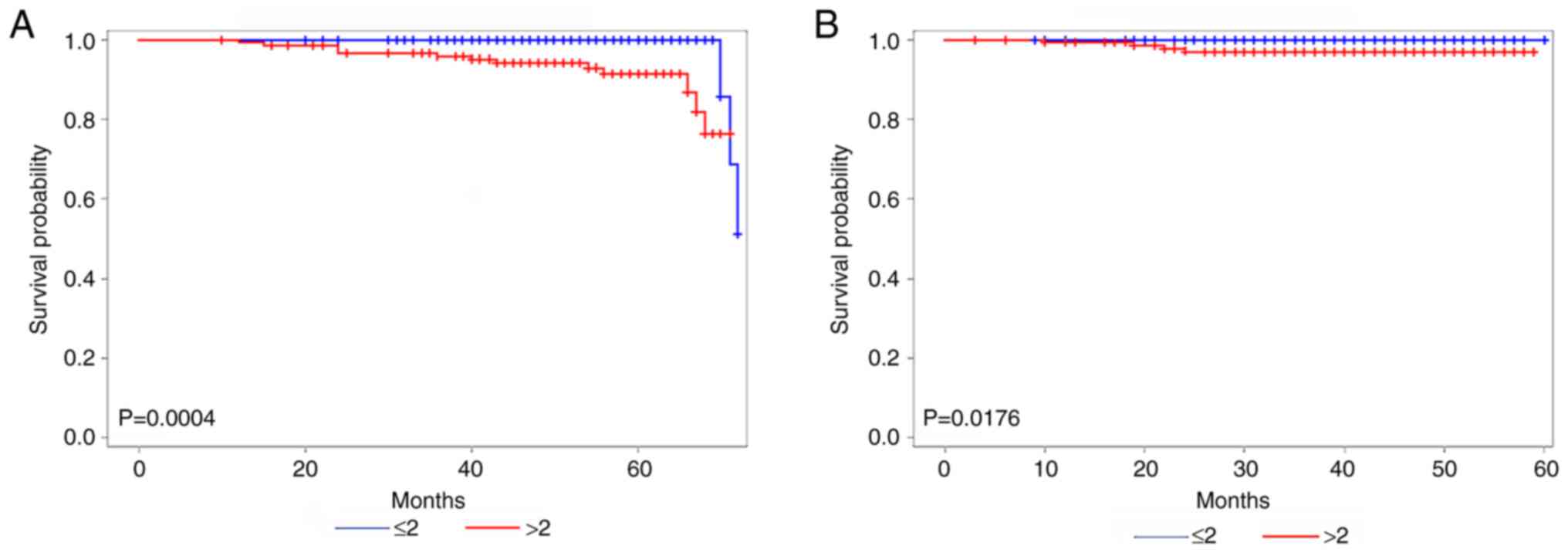
Table II. Unadjusted Kaplan-Meier
curves are illustrated in Fig. 2A and
B. In the subgroup of 201 patients with tumor sizes ≤2 cm,
three relapses (1.49%) and no deaths were recorded. Fig. 2A shows the DFS of patients with
tumors sized ≤2 and >2 cm; the patients with tumor sizes ≤2 cm
that underwent MIS had a reduced likelihood of relapse compared to
those with tumors >2 cm in size (HR, 0.110; 95% CI, 0.025–0.488;
P=0.0004). Fig. 2B shows the OS of
patients with tumors sized ≤2 and >2 cm; there was no
significant difference between the two groups (P=0.0176).
 | Table I.Patient characteristics. |
Table I.
Patient characteristics.
| Characteristic | Value |
|---|
| Median age, years
(range) | 43 (25–70) |
| Median BMI,
kg/m2 (range) | 22.5 (19.2–25.3) |
| Histology, n (%) |
|
|
Squamous | 269 (76.86%) |
|
Adenocarcinoma | 75 (21.43%) |
|
Adenosquamous | 6 (1.71%) |
| FIGO stage, n
(%) |
|
| IA1 LVSI
(+) | 22 (6.29%) |
| IA2 | 36 (10.29%) |
| IB1 | 137 (39.14%) |
| IB2 | 126 (36.00%) |
| IIA1 | 14 (4.00%) |
|
IIIC1P | 15 (4.29%) |
| Tumor size, n |
|
| ≤2
cm | 201 |
| 2–4
cm | 149 |
| Conversion to
laparotomy | 0 |
| Grading, n |
|
| G1 | 101 |
| G2 | 192 |
| G3 | 57 |
 | Table II.Peri-operative outcomes of the study
population. |
Table II.
Peri-operative outcomes of the study
population.
| Characteristic | Value |
|---|
| Median surgical time,
min (range) | 221 (181–265) |
| Median estimated
blood loss, ml (range) | 145 (50–250) |
| LVSI, n |
|
|
Negative | 270 |
|
Positive | 80 |
| Median number of
lymph nodes (range) | 25 (16–38) |
| Histology of lymph
nodes, n |
|
| Tumor
free | 335 |
| Tumor
involved | 15 |
| Post-operative
complications, n |
|
| Tumor
tissue exposed to pelvic cavity after closure | 0 |
| Poor
healing of vaginal stump | 0 |
| Lymphatic
complications | 0 |
| Positive pathological
examination of vaginal margin, n | 0 |
| Adjuvant therapy,
n |
|
|
Radiotherapy and/or
chemoradiotherapy | 83/350 |
| Median follow-up,
months (range) | 51 (30–72) |
| Recurrence, n | 15/350 |
| Death, n | 4/350 |
| Liver
cancer | 1/4 |
| Cervical
cancer | 3/4 |
Discussion
Radical hysterectomy is the standard surgical mode
of therapy for patients diagnosed with early-stage cervical cancer
(10). Previous studies have
suggested that LRH yields comparable oncologic outcomes to those
achieved with ARH (11–13). Similarly, Gallotta et al
(14) demonstrated that LRH
provides equivalent or superior intraoperative and short-term
postoperative outcomes compared with ARH. However, Sert et
al (15) and Kohler et
al (16) showed no significant
differences in the recurrence and survival rates between the two
approaches. The benefits associated with MIS have led to an
increasing preference for LRH in the management of cervical cancer.
In a meta-analysis by Wang et al (11) on 12 studies comparing LRH with open
radical hysterectomy (754 vs. 785 cases) for cervical cancer, no
significant differences in the 5-year OS and DFS rates were
observed between the two approaches. However, a phase III
randomized clinical trial conducted in 2018 reported that minimally
invasive radical hysterectomy was associated with lower rates of
DFS (3-year rate, 91.2 vs. 97.1%) and OS (3-year rate, 93.8 vs.
99.0%) compared with ARH (17). In
addition, several retrospective studies have demonstrated an
association of minimally invasive radical hysterectomy with shorter
survival compared with ARH (5,11,18);
the observed shorter survival outcomes could be attributed to a
number of factors, including a lower extent of resection, the level
of surgeon's experience or the use of a uterine manipulator. Kim
et al (19) observed no
significant differences in the frequency of positive margins and,
in most institutions, only individuals who had undergone several
years of supervised training with a long learning curve were
capable of effectively performing laparoscopic surgery. Therefore,
the use of a uterine manipulator may be more significantly
associated with decreased survival outcomes. Doo et al
(20) reported no statistical
difference in recurrence risk (P=0.22) and risk of death (P=0.18)
between ARH and robotic radical hysterectomy groups. These
conflicting data necessitate reconsideration of whether the
decision to abandon MIS is in the best interest of patients.
Since 2013, the Department of Gynecology of Jinhua
Maternity and Child Health Care Hospital, and Department of
Gynecology, Jinhua Hospital of Zhejiang University has employed
minimally invasive radical hysterectomy with a uterine manipulator
as the preferred surgical procedure for early-stage cervical
cancer, reflecting the global shift towards minimal invasive
approaches worldwide. However, a number of cases involving tumors
with larger diameters displayed recurrence only ~1 year after
surgical treatment, regardless of subsequent radiotherapy and/or
chemotherapy, and the majority of these individuals died as a
result of central recurrence. Notably, one of the patients
experiencing two episodes of central recurrence underwent
laparoscopic surgery, and has survived for 11 years. Considering
the short-term central recurrence and poor prognosis of larger
tumors, it was considered that the issue of tumor exposure to the
peritoneum was insufficiently addressed. As of 2017, the strategy
for surgical treatment of early-stage cervical cancer was modified
and a list of ‘no-tumor’ principles was designed, with the aim of
improving patient survival while maintaining optimal quality of
life. To facilitate further promotion of the surgical approach of
abandoning the uterine manipulator in radical hysterectomy, a
proposal for a new project within our hospital has been
submitted.
Various strategies have been implemented to prevent
contamination of the peritoneal cavity in the current study, such
as application of a vaginal cuff prior to surgical intervention, as
well as the use of a special vaginal clamp and vaginal suture
before colpotomy, particularly in cases where the cervical tumor is
encased within the vagina. However, the use of the clamp is solely
restricted to endophytic type and ulcerative type cancer cases
displaying smaller tumors (≤2 cm) without vaginal invasion.
Notably, in accordance with the ‘no-tumor’ principle, the clamp
needs to be repositioned from the vagina to cervix to close the
vaginal canal. Failure to do so may mobilize tumor cells,
potentially resulting in metastasis. Given the limitations of clamp
usage, vaginal suture was performed prior to colpotomy in patients
with smaller tumors (≤2 cm). The process of vaginal suturing is
associated with an increased risk of mobilization of tumor cells;
however, subsequent investigation revealed no instances of central
recurrence in the present study. For tumors >2 cm, the vaginal
cuff technique was primarily used, which is capable of effectively
avoiding tumor spread; however, this procedure presents technical
challenges, particularly in patients where cervix exposure is
difficult, such as those who are obese or nulliparous (19). On the other hand, during the type C
procedure, an incision was made into the deep uterine vein around
the ureter and the vaginal wall was subsequently transected;
however, the position of the vaginal incision in laparoscopic
surgery may not always be consistent with the level of the vaginal
cuff, leading to positioning failure in colpotomy and challenges in
proceeding with the operation. Additionally, the use of the myoma
drill carries the risk of uterine perforation and subsequent damage
to pelvic vessels or ureters. Considering the possible
complications, the myoma drill approach was modified to a uterine
suture approach at a later period of the study.
In the present study, myoma drill or uterine suture
techniques were applied combined with protective vaginal closure
techniques, such as clamping, vaginal cuffing or vaginal suturing,
to avoid tumor spillage before colpotomy. In addition, the specimen
was placed in a collection bag to prevent tumor spillage and its
extraction was performed via the vaginal route. Based on the
pathological results, 83 (23.71%) patients received radiotherapy
and/or adjuvant chemoradiation. No central recurrences were
observed after a median follow-up of 51 months (range, 30–72
months), with favorable DFS and OS outcomes of 95.71% (335/350) and
98.86% (346/350), respectively. The survival outcomes in all
patients were comparable to the LACC trial laparotomy group (3-year
DFS and OS rates of 97.1 and 99% respectively), which could be
attributed to the techniques implemented for avoiding tumor
spillage. and evolving treatment approaches for cervical cancer.
Moreover, the subgroup of patients with tumors ≤2 cm that underwent
MIS had a significantly lower likelihood of relapse compared to
those with tumors >2 cm (P=0.0005). In contrast to the LACC
trial, the current study did not reveal inferior outcomes
associated with MIS. The strict principle of no contact with the
tumor during excision may be a significant contributory factor. In
addition, the lower percentage of lymph node positivity in all
cases (4.29 vs. 12.4%) and relatively short follow-up compared with
the LACC trial may have influenced the OS and DFS rates. Other
studies (4,21) have similarly shown that MIS does not
yield inferior oncological outcomes. For example, two cohort
studies in Denmark and Sweden (4,22)
demonstrated that a nationwide adoption of robot-assisted MIS for
cervical cancer did not negatively impact oncologic outcomes,
consistent with the current findings. While the follow-up duration
in the present study was relatively short, it is important to
highlight that at the time of analysis, 60.29% of cases (211/350)
had successfully reached the 4-year time point. From the
aforementioned results, it may be inferred that the laparotomy may
not be the most appropriate method for treating early-stage
cervical cancer and MIS approaches warrant further
consideration.
The current study has a number of limitations that
should be taken into consideration. The follow-up period was
relatively brief, with a median of 51 months. Moreover, this
investigation is an observational retrospective analysis and lacks
a control group. The results highlight the need for further
surveillance through new prospective randomized trials comparing
LRH free from manipulators with ARH, with the goal of achieving
optimal DFS over longer follow-up durations.
In conclusion, the procedure performed in the
present study avoided the use of a uterine manipulator and
implemented protective vaginal closure over the entire tumor to
minimize the risk of tumor spillage in MIS. The results indicated
no inferior oncologic outcomes, particularly in the subgroup of
patients with tumor sizes ≤2 cm.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
MH conceived and designed the study. LiJ, LaJ and MS
acquired, analyzed and interpretated the data. LiJ and MH drafted
the article and revised it critically for important intellectual
content. LiJ and LaJ confirm the authenticity of all the raw data.
All authors read and approved the final version of the
manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Jinhua Hospital of Zhejiang University and Jinhua Maternity and
Child Health Care Hospital (ethics approval no. 2020-268). All
patients provided written informed consent before recruitment.
Patient consent for publication
All patients provided written informed consent for
publication of the images and data presented.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2020. CA Cancer J Clin. 70:7–30. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Casarin J, Buda A, Bogani G, Fanfani F,
Papadia A, Ceccaroni M, Malzoni M, Pellegrino A, Ferrari F, Greggi
S, et al: Predictors of recurrence following laparoscopic radical
hysterectomy for early-stage cervical cancer: A multi-institutional
study. Gynecol Oncol. 159:164–170. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Philp L, Covens A, Vicus D, Kupets R,
Pulman K and Gien LT: Feasibility and safety of same-day discharge
after laparoscopic radical hysterectomy for cervix cancer. Gynecol
Oncol. 147:572–576. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Jensen PT, Schnack TH, Frøding LP, Bjørn
SF, Lajer H, Markauskas A, Jochumsen KM, Fuglsang K, Dinesen J,
Søgaard CH, et al: Survival after a nationwide adoption of robotic
minimally invasive surgery for early-stage cervical cancer-a
population-based study. Eur J Cancer. 128:47–56. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ramirez PT, Frumovitz M, Pareja R, Lopez
A, Vieira M, Ribeiro R, Buda A, Yan X, Shuzhong Y, Chetty N, et al:
Minimally invasive versus abdominal radical hysterectomy for
cervical cancer. N Engl J Med. 379:1895–1904. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Charo LM, Vaida F, Eskander RN, Binder P,
Saenz C, McHale M and Plaxe S: Rapid dissemination of
practice-changing information: A longitudinal analysis of
real-world rates of minimally invasive radical hysterectomy before
and after presentation of the LACC trial. Gynecol Oncol.
157:494–499. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hillemanns P, Brucker S, Holthaus B, Lampe
B, Runnebaum I, Ulrich U, Wallwiener M, Solomayer E, Fehm T and
Tempfer C: Comment on the LACC trial investigating early-stage
cervical cancer by the uterus commission of the study group for
gynecologic oncology (AGO) and the study group for gynecologic
endoscopy (AGE) of the German society for gynecology and obstetics
(DGGG). Geburtshilfe Frauenheilkd. 78:766–767. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Park JY and Nam JH: How should gynecologic
oncologists react to the unexpected results of LACC trial? J
Gynecol Oncol. 29:e742018. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
National Comprehensive Cancer Network, .
NCCN Clinical Practice Guidelines in Oncology - Cervical Cancer,
Version 4. 2019.https://www2.tri-kobe.org/nccn/guideline/gynecological/english/cervical.pdfDecember
30–2021
|
|
10
|
Cibula D, Pötter R, Planchamp F,
Avall-Lundqvist E, Fischerova D, Haie Meder C, Köhler C, Landoni F,
Lax S, Lindegaard JC, et al: The European society of gynaecological
oncology/European society for radiotherapy and oncology/European
society of pathology guidelines for the management of patients with
cervical cancer. Int J Gynecol Cancer. 28:641–655. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wang YZ, Deng L, Xu HC, Zhang Y and Liang
ZQ: Laparoscopy versus laparotomy for the management of early stage
cervical cancer. BMC Cancer. 15:9282015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Nam JH, Park JY, Kim DY, Kim JH, Kim YM
and Kim YT: Laparoscopic versus open radical hysterectomy in
early-stage cervical cancer: Long-term survival outcomes in a
matched cohort study. Ann Oncol. 23:903–911. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Chen Y, Xu H, Li Y, Wang D, Li J, Yuan J
and Liang Z: The outcome of laparoscopic radical hysterectomy and
lymphadenectomy for cervical cancer: A prospective analysis of 295
patients. Ann Surg Oncol. 15:2847–2855. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Gallotta V, Conte C, Federico A, Vizzielli
G, Gueli Alletti S, Tortorella L, Pedone Anchora L, Cosentino F,
Chiantera V, Fagotti A, et al: Robotic versus laparoscopic radical
hysterectomy in early cervical cancer: A case matched control
study. Eur J Surg Oncol. 44:754–759. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Sert BM, Boggess JF, Ahmad S, Jackson AL,
Stavitzski NM, Dahl AA and Holloway RW: Robot-assisted versus open
radical hysterectomy: A multi-institutional experience for
early-stage cervical cancer. Eur J Surg Oncol. 42:513–522. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Köhler C, Hertel H, Herrmann J, Marnitz S,
Mallmann P, Favero G, Plaikner A, Martus P, Gajda M and Schneider
A: Laparoscopic radical hysterectomy with transvaginal closure of
vaginal cuff-a multicenter analysis. Int J Gynecol Cancer.
29:845–850. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Shah CA, Beck T, Liao JB, Giannakopoulos
NV, Veljovich D and Paley P: Surgical and oncologic outcomes after
robotic radical hysterectomy as compared to open radical
hysterectomy in the treatment of early cervical cancer. J Gynecol
Oncol. 28:e822017. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Melamed A, Margul DJ, Chen L, Keating NL,
Del Carmen MG, Yang J, Seagle BL, Alexander A, Barber EL, Rice LW,
et al: Survival after minimally invasive radical hysterectomy for
early-stage cervical cancer. New Engl J Med. 379:1905–1914. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kim SI, Cho JH, Seol A, Kim YI, Lee M, Kim
HS, Chung HH, Kim JW, Park NH and Song YS: Comparison of survival
outcomes between minimally invasive surgery and conventional open
surgery for radical hysterectomy as primary treatment in patients
with stage iB1-IIA2 cervical cancer. Gynecol Oncol. 153:3–12. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Doo DW, Kirkland CT, Griswold LH, McGwin
G, Huh WK, Leath CA III and Kim KH: Comparative outcomes between
robotic and abdominal radical hysterectomy for IB1 cervical cancer:
Results from a single high volume institution. Gynecol Oncol.
153:242–247. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Alfonzo E, Wallin E, Ekdahl L, Staf C,
Rådestad AF, Reynisson P, Stålberg K, Falconer H, Persson J and
Dahm-Kähler P: No survival difference between robotic and open
radical hysterectomy for women with early-stage cervical cancer:
Results from a nationwide population based cohort study. Eur J
Cancer. 116:169–177. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Wenzel HHB, Smolders RGV, Beltman JJ,
Lambrechts S, Trum HW, Yigit R, Zusterzeel PLM, Zweemer RP, Mom CH,
Bekkers RLM, et al: Survival of patients with early-stage cervical
cancer after abdominal or laparoscopic radical hysterectomy: A
nationwide cohort study and literature review. Eur J Cancer.
133:14–21. 2020. View Article : Google Scholar : PubMed/NCBI
|