Introduction
Acute myeloid leukemia (AML) is a heterogeneous
malignant disease with diverse biological features. AML occurs in
approximately 60% of patients, most of whom are older than 60 years
(1). These elderly patients
normally do not respond as well to the current conventional
chemotherapy as their younger counterparts. This is due to the
intrinsic resistant nature of their leukemic cells and/or poor
tolerance to conventional chemotherapy regimens (2). Progress has been ongoing in the
treatment outcome of AML, especially in elderly patients. However,
outcome has been poor with only 25–30% of adult patients being
cured (3–5). Although prognosis varies among AML
subtypes, the majority of patients relapse following an initial
complete response (CR) and ultimately succumb due to resistant
disease. Patients with AML who experience a particularly short
first CR and those who fail to achieve CR after two induction
attempts are unlikely to respond to any currently available
chemotherapeutic agents. Similarly, patients with high-risk
myelodysplastic syndromes likely to progress to AML [refractory
anemia with excess blasts (RAEB) or refractory anemia with excess
blasts in transformation (RAEBT)] have an estimated survival of
less than one year (6). Supportive
therapy remains the standard care for this population since
intensive chemotherapy regimens, such as those used in AML, were
reported to produce high rates of treatment-related mortality with
rare durable remissions (7,8).
Therefore, novel approaches and alternative
therapeutic strategies need to be explored. The role of
angiogenesis in hematologic malignancies has been elucidated by
several investigators; thus, inhibitors of angiogenesis are
currently under investigation in these disorders. Thalidomide has
antiangiogenic and immunomodulatory properties. However,
thalidomide has shown only modest activity as a single agent in the
therapy of AML. In addition, no study in the literature identifies
a dose or schedule that should be followed when using thalidomide.
Therefore, more studies are required to design a strategy to
enhance the antileukemic effect of thalidomide. Such an approach is
beneficial if the proper combination with other chemotherapeutic
agents, such as interleukin-2 (IL-2) and arsenic trioxide
(As2O3), is used. The current study examined
the effect of the combination of thalidomide and the suggested
chemotherapeutic agents on the KG-1a (human AML with early
phenotype) cell line. The present study aimed to test the
hypothesis that combining thalidomide with the correct
chemotherapeutic agent/agents may be more efficient in the therapy
of AML.
Materials and methods
Human KG-1a acute myeloid leukemia
cells
The KG-1a cells, which are an early phenotype of
human AML (American Type Culture Collection, Manassas, VA, USA),
were grown in complete growth medium (Iscove’s Modified Dulbeco’s
Medium; American Type Culture Collection) supplemented with 20%
fetal bovine serum (Sigma-Aldrich, UK) and 1%
penicillin-streptomycin (Gibco Invitrogen Corporation, Carlsbad,
CA, USA) at 37°C in a humidified 5% CO2 incubator.
Treatment of human KG-1a acute myeloid
leukemia cells
The KG-1a cells were cultured for 48 h in 12-well
tissue culture plates, each containing complete growth medium at a
concentration of 2×106 cells/ml. Each well contained a
total volume of 2 ml. Thalidomide (Tocris Bioscience, Ellisville,
MO, USA) was added at concentrations of 5 mg/l, either alone or in
combination with other chemotherapeutic agents. IL-2
(Proleukin®, Aldesleuken for injection) (Chiron
Therapeutics, Emeryville, CA, USA) was added at a concentration of
200 IU/ml, either alone or in combination with thalidomide and
As2O3. As2O3
(Sigma-Aldrich, Inc., St. Louis, MO, USA) was added at two
concentrations of 2 and 4 μM with and without 100 μM of ascorbic
acid (AA) in the first flow cytometry study, and at 4 μM in the
remaining studies; either alone or combined with thalidomide and
IL-2. A control culture containing neither thalidomide nor IL-2 nor
As2O3 was established in conditions that were
otherwise identical. Duplicate control and treated cultures were
established and incubated for 48 h at 37°C in a humidified 5%
CO2 incubator. The incubation time was selected to allow
adequate time for apoptosis and necrosis to occur in the KG-1a
human myeloid leukemia cells [modified from Lu and Hassan (9)].
Detection of apoptosis and necrosis using
flow cytometry
The detection of apoptosis and necrosis by Annexin
V-FITC assay using flow cytometry was performed as described in the
Annexin V-FITC apoptosis detection kit manual (BioVision, Inc.,
Mountain View, CA, USA). Staurosporine (Sigma-Aldrich, Inc.) was
used as a positive control at a concentration of 10 μM and was
incubated for only 24 h with the leukemia cells. Briefly, following
incubation for 48 h, the KG-1a cells were harvested by
centrifugation at 1,300 rpm for 5 min. Cells were resuspended in
500 μl of 1X binding buffer. Annexin V-FITC (5 μl) and propidium
iodide (PI) (5 μl) were added to the tubes (except the negative
control which contained no staining nor treatment where only
Annexin V-FITC was added for the Annexin V-FITC controls and only
PI was added for the PI control). Tubes were incubated at room
temperature for 5 min in the dark. Samples were then checked by the
FACSCalibur Flow Cytometer (BD-Biosciences, San Jose, CA, USA) and
apoptotic and necrotic cells were counted according to their
staining with Annexin V or PI, respectively [modified from Yang
et al (10)].
Statistical analysis
Results were subjected to one-way ANOVA. Statistical
significant differences between means was set at p<0.05.
Results
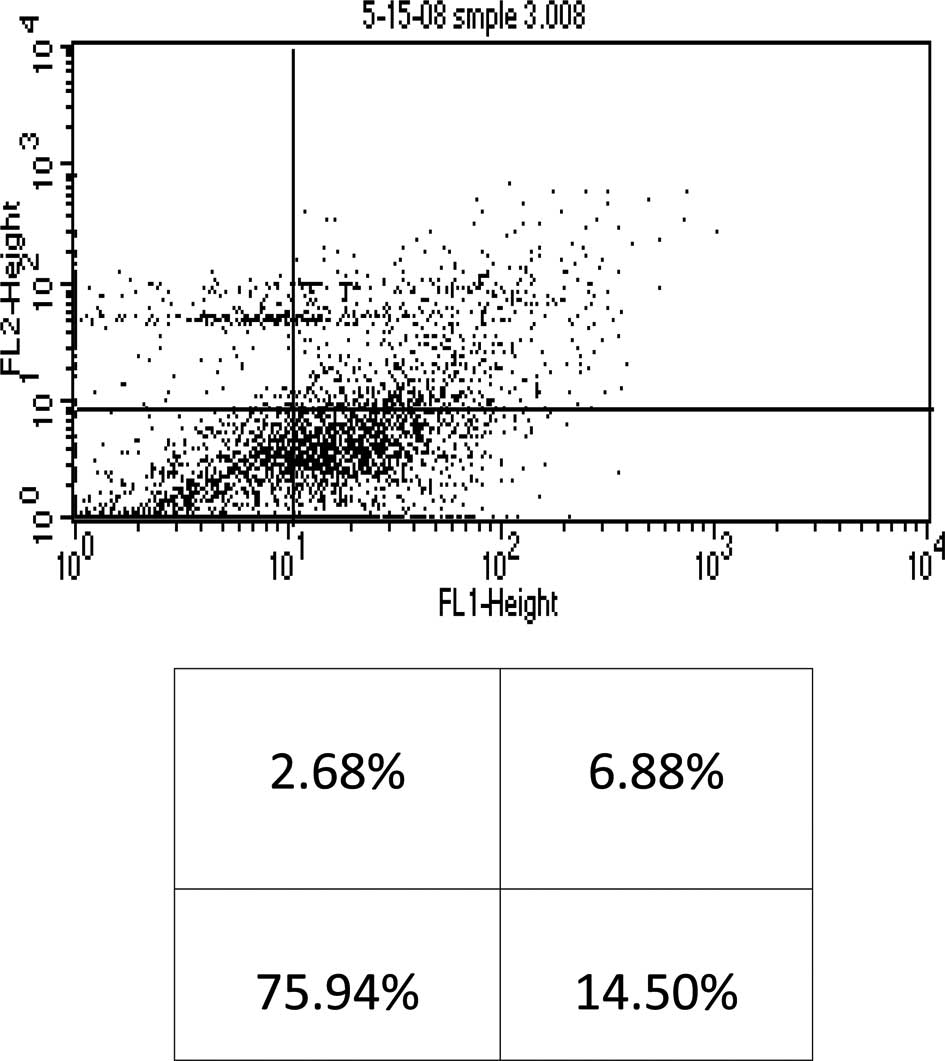
First flow cytometry study
This study was mainly designed to determine whether
AA enhances As2O3-induced cytotoxicity in the
KG-1a human AML cell line. When the KG-1a cells were incubated with
the chemotherapeutic agents for 48 h, results obtained indicated
that 2 μM of As2O3 alone resulted in early
and late apoptosis, and necrosis (14.5%, 6.88% and 2.68%,
respectively) of the total cell population (Fig. 1). Moreover, 2 μM of
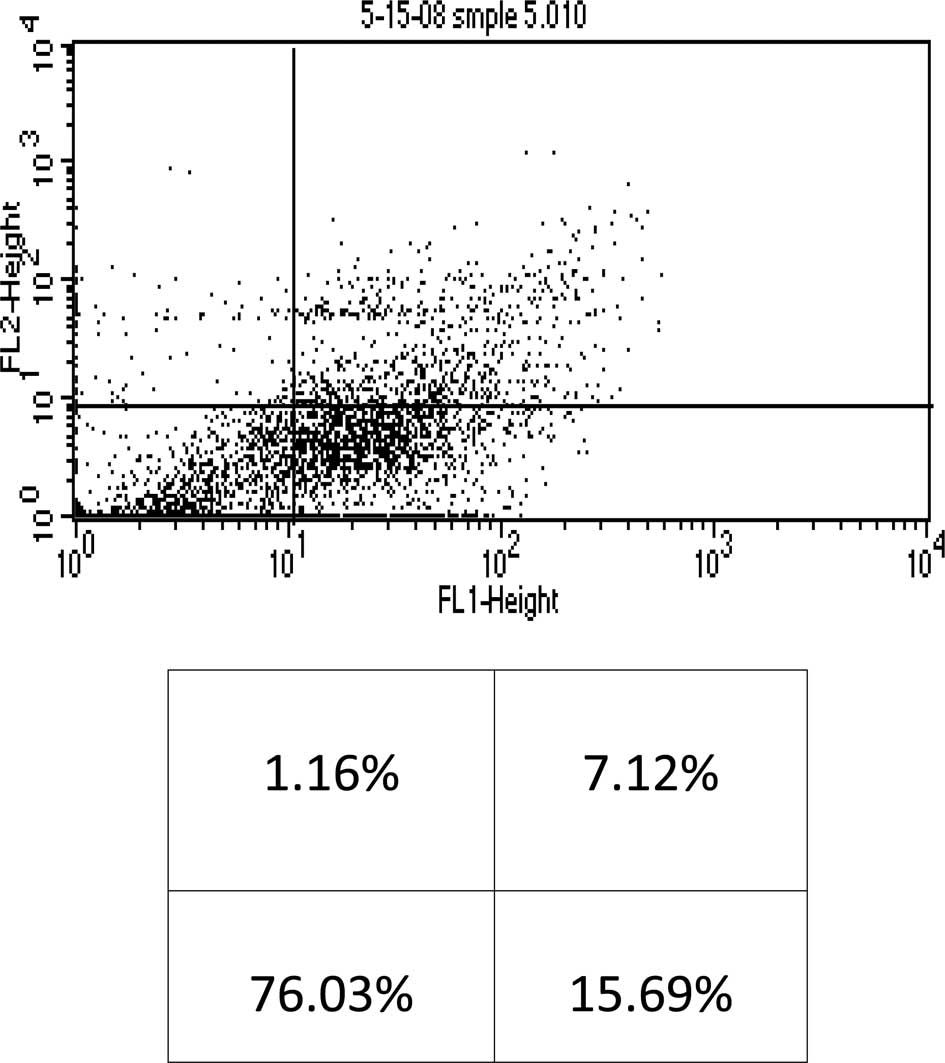
As2O3 in the presence of 100 μM of AA
resulted in 15.69% early apoptosis, 7.12% late apoptosis and 1.16%
necrosis of the total cell population (Fig. 2).
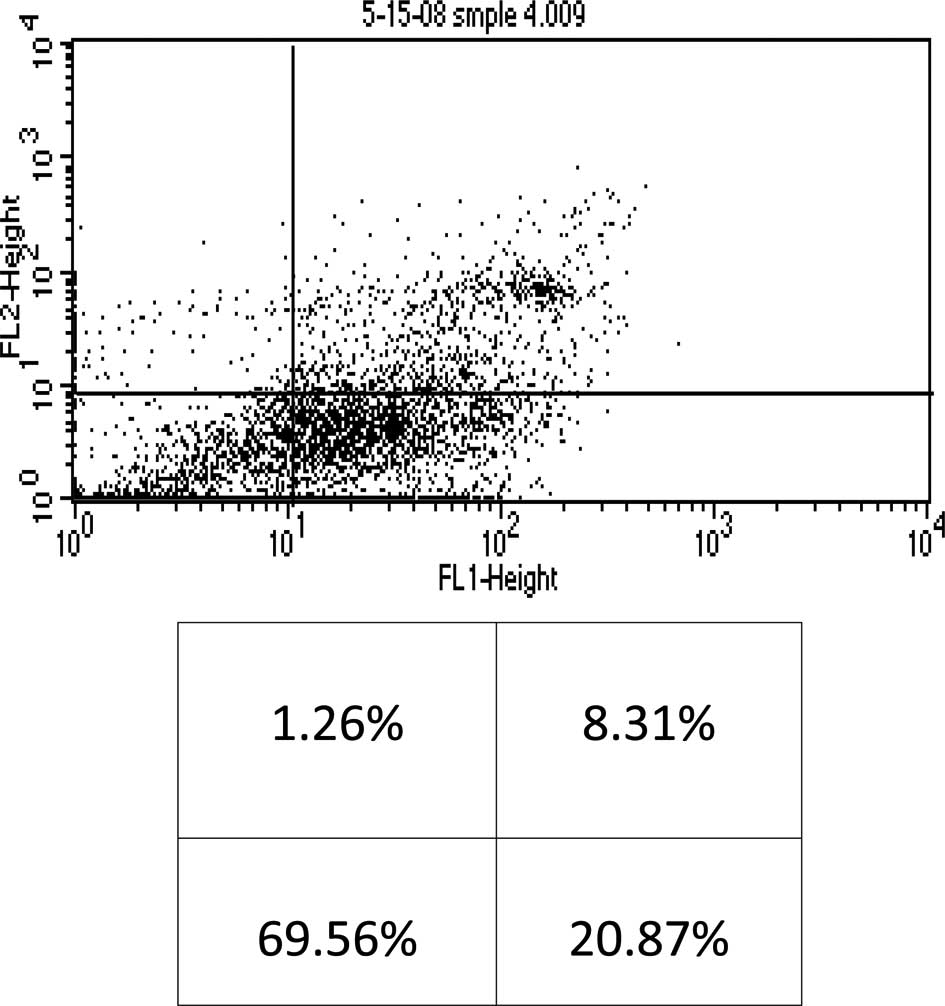
When the cells were incubated with 4 μM of
As2O3 alone, early and late apoptosis, as
well as necrosis (20.87%, 8.31% and 1.26%, respectively) of the
total cell population were observed (Fig. 3). Conversely, when 4 μM of
As2O3 was used in the presence of 100 μM of
AA, 21.84% early apoptosis, 8.14% late apoptosis and 0.77% necrosis
of the total cell population were noted (Fig. 4). These findings indicate that AA
did not significantly enhance the cytotoxicity of
As2O3, and as a result our study utilized the
higher dose of As2O3 (4 μM) without the
addition of AA.
Cytotoxic effects of thalidomide, arsenic
trioxide and interleukin-2 alone or in combination in KG-1a
leukemia cells
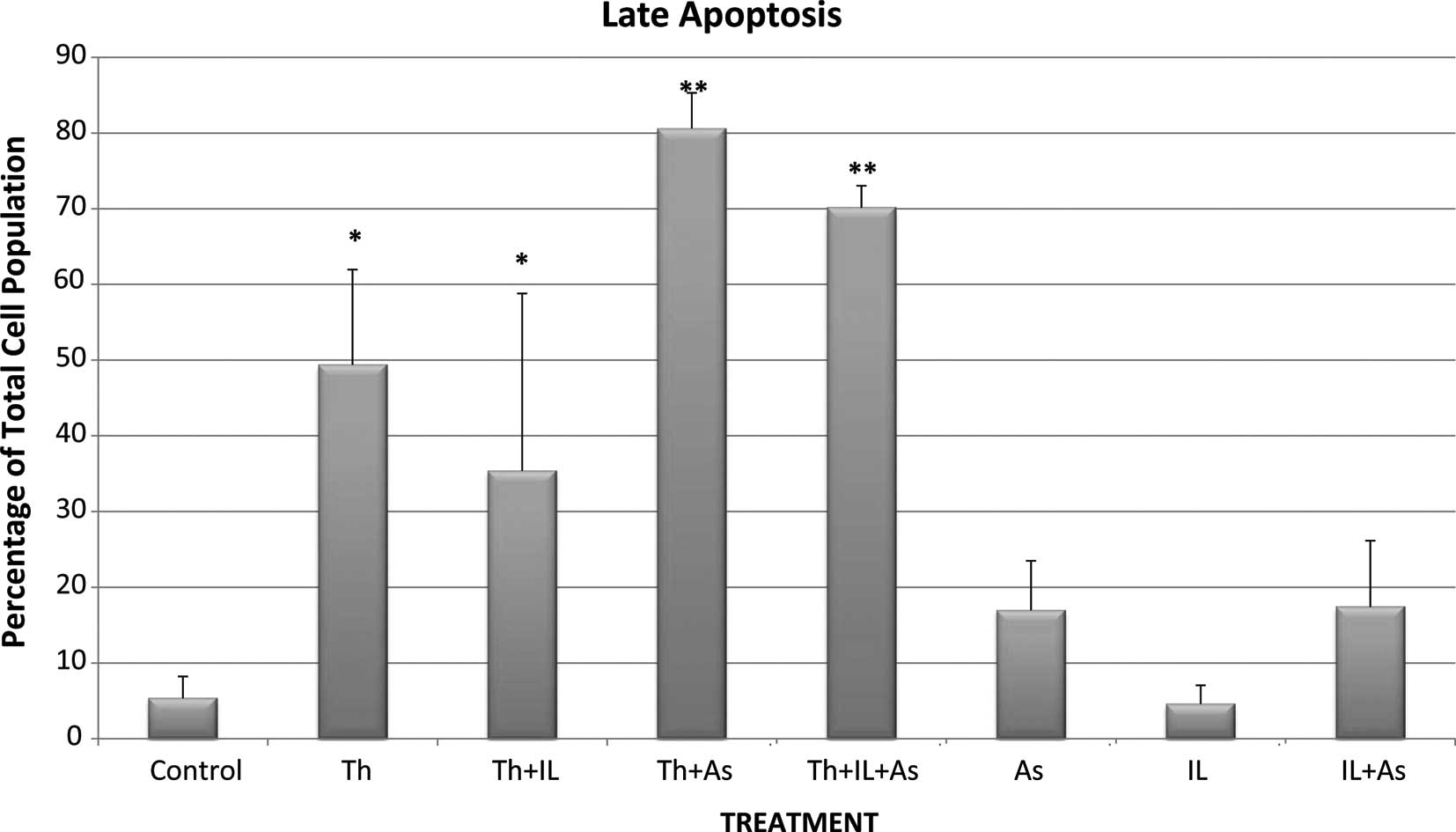
Subsequent flow cytometry studies were conducted to
test the cytotoxicity of chemotherapeutic agents both individually
and in combination in KG-1a human leukemia cells in order to
evaluate whether thalidomide cytotoxicity was enhanced by either
IL-2 and/or As2O3.
Control KG-1a cells that were incubated for 48 h
showed 0.775% necrosis, 9.89% early apoptosis and 5.345% late
apoptosis in the total cell population (Figs. 5-7).
When the cells were incubated with thalidomide only in a
concentration of 5 mg/l, the percentages noted were: necrosis.
1.155%; early apoptosis, 7.92% and late apoptosis, 49.385% in the
total cell population (Figs.
5-7). These results indicate
that thalidomide exerted significant cytotoxicity in the KG-1a
cells, and this cytotoxicity was mainly due to late apoptosis.
When the cells were incubated with 4 μM of
As2O3 the percentages of total cell
population noted were: necrosis, 0.59%; early apoptosis, 10.095%
and late apoptosis, 16.965% (Figs.
5-7). These results indicate
that As2O3 alone had a modest cytotoxic
effect since the percentages of cells in early and late apoptosis
as well as necrosis were not statistically significantly different
from values noted in the control cells. A similar conclusion was
drawn with regard to cytotoxicity resulting from incubation of the
KG-1a cells with 200 IU/ml of IL-2 alone. IL-2 alone resulted in
0.325% necrosis, 8.54% early apoptosis and 4.585% late apoptosis
(Figs. 5-7). These values are not significantly
different from those observed in the control KG-1a cells incubated
under the same conditions.
However, when thalidomide and
As2O3 were combined, the percentages observed
were: necrosis, 0.87%; early apoptosis, 3.455% and late apoptosis,
80.6% (Figs. 5-7). These findings indicate that
As2O3 enhanced the cytotoxicity induced by
thalidomide since the percentage of cells in late apoptosis was
49.385% when the cells were incubated with thalidomide alone, but
increased to 80.6% when thalidomide was combined with
As2O3.
When IL-2 was combined with thalidomide no
enhancement of cytotoxicity was noted as the percentages of total
cell population showing necrosis, early apoptosis and late
apoptosis were: 1.155, 7.92 and 49.385%, respectively, with
thalidomide alone and 1.47, 6.58 and 35.385%, respectively, when a
combination of thalidomide and IL-2 were used (Figs. 5-7).
IL-2 was also unable to enhance the cytotoxicity of
the combination of thalidomide and As2O3 when
the chemotherapeutic agents were used together since the
percentages of total cell population showing necrosis, early and
late apoptosis were 1.69, 5.655 and 70.135%, respectively. These
values were not statistically significantly different from those
observed with thalidomide and As2O3.
Discussion
This study was conducted to evaluate the efficacy of
thalidomide in the management of AML, as well as to examine the
possibility of increasing its cytotoxicity by combining it with
other chemotherapeutic agents, such as IL-2 and
As2O3. The variant subline KG-1a of the human
acute myelogenous leukemia cell line KG-1 (11) was used as a test model.
The present study investigated the effect of AA on
As2O3 cytotoxic activity. Glutathione (GSH)
was shown to be an inhibitor of As2O3-induced
cell death either by conjugating As2O3 or by
sequestering reactive oxygen induced by
As2O3. Consistent with this possibility,
increasing GSH levels with N-acetylcysteine attenuated
As2O3 cytotoxicity (12). Decreases in GSH levels were
associated with AA metabolism. Clinically relevant doses of AA
decreased GSH levels and potentiated the
As2O3-mediated cell death of the four
multiple myeloma cell lines. Similar results were obtained in
freshly isolated human multiple myeloma cells (12). AA is widely heralded as an
antioxidant (13). However, it was
shown that AA acts as an oxidizing agent, particularly in the
presence of compounds that increase the production of reactive
oxygen species (14). The
pro-oxidant effects of AA and potentiation of cell death induced by
free radicals appear to involve the production of hydrogen peroxide
(H2O2) (14,15).
However, AA alone had no effect on cell viability suggesting that
AA does not produce a sufficient level of
H2O2 to initiate oxidative damage. Instead,
AA treatment increases basal levels of cellular
H2O2 (12).
Grad et al showed that clinically-relevant doses of AA
decreased GSH levels and potentiated the
As2O3-mediated cell death of four types of
multiple myeloma cell lines (12).
Accordingly, the likelihood that AA increases the
cytotoxicity of As2O3 in the KG-1a human
leukemia cell line was investigated. Two doses of
As2O3, 2 and 4 μM, were tested in the
presence or absence of AA in a concentration of 100 μM. The results
obtained indicate that 2 μM of As2O3 alone
resulted in 6.88% late apoptosis compared to 7.12% of late
apoptosis in the presence of AA. In addition, late apoptosis
induced by 4 μM of As2O3 alone was 8.31
compared to 8.14% in the presence of AA. These findings indicate
that in our protocol, AA did not enhance the cytotoxicity of
As2O3. Therefore, subsequent studies were
conducted without adding AA to As2O3.
Thalidomide (Thalomid®),
α-(N-phthalimido) glutarimide, is an immunomodulatory agent.
Thalidomide has numerous characteristics that may contribute to its
role as a potential agent in the treatment of malignant and
immunological diseases. The drug inhibits angiogenesis by blocking
basic fibroblast growth factor (bFGF) and vascular endothelial
growth factor (VEGF) (16),
modulates various cytokines (17),
enhances cell-mediated immunity by directly co-stimulating T-cells
(18) and alters adhesion molecule
expression (19).
Thalidomide at 5 mg/l (19 μM) resulted in 49.385%
late apoptosis compared to 5.345% of the control. These results
were consistent with Du et al (20), who stated that thalidomide inhibited
tumor growth in a concentration-dependent manner in MCF-7 and HL-60
cell lines. Moreover, 1C50S (inhibitory concentration of 50%) for
the cell lines were 18.36±2.34 and 22.14±2.15 μM, respectively
(20).
Efforts were made in our study to increase the
cytotoxicity of thalidomide by combining it with other
chemotherapeutic agents. The first agent used was IL-2. IL-2
(Proleukin, Aldesleuken for injection), currently being used to
treat adults with metastatic melanoma and renal cell carcinoma, was
also examined in this study to see whether it was able to enhance
thalidomide cytotoxicity. IL-2 alone resulted in 4.59% late
apoptosis compared to 5.35% late apoptosis in the control. The
combination of thalidomide and IL-2 resulted in 35.39% late
apoptosis compared to 49.39% late apoptosis for thalidomide alone.
Thus, it was shown that IL-2 neither enhanced thalidomide toxicity
nor was cytotoxic itself when used as a single therapeutic
modality.
The reason that IL-2 was not cytotoxic to the
leukemic cell line in this setting may be due to an unfavorable
microenvironment since this was an in vitro study. Other
studies investigated the development of an approach aimed at
preventing relapse after autologous hemopoietic cell
transplantation (AHCT). Post-transplant relapse is due to minimal
residual disease in the body of the patient that persists after the
conditioning regimen and/or presence of leukemic cells in the auto
graft (21). Following an
allogeneic transplant, the rate of leukemic relapse is lower for
two reasons: the graft is free of leukemic cells and, more
importantly, the graft vs. leukemia (GVL) effect associated with
the transfer of donor T-and natural killer-cells is able to
immunologically eradicate host leukemic cells (22). Therefore, efforts have been made to
lower leukemic relapse after AHCT by either purging the leukemic
cells in the auto graft (23) or
inducing an autologous GVL effect by immunotherapy (24). Since the results of the two
approaches were not always satisfactory, other approaches which
actively eradicated the residual disease from the patient’s body,
as opposed to those that only eliminated the contaminating leukemic
cells in the graft, were adopted to ensure long-term disease-free
survival (25). Reported
immunotherapeutic approaches are diverse but the majority include
the use of in vivo IL-2 with or without adoptively
transferred lymphokine-activated killer (LAK) cells. However, this
approach is limited by the fact that the doses of IL-2 required to
maintain LAK activity in vivo cause undesirable side effects
(26). Alternatively, several other
cytokines including IL-1 (27),
IL-4 (28), IL-7 (29), IL-12 (29) and granulocyte-macrophage
colony-stimulating factor (GM-CSF) (30) have shown to be able to induce LAK
activity themselves or in combination with IL-2. Rojas et al
(31) demonstrated that
immunotherapy with IL-2 + GM-CSF after total body irradiation
results in a net improvement in survival in BALB/C mice injected
with LSTRA leukemic cells (31).
Other investigators reported the in vitro and in vivo
generation of LAK activity by the synergistic effects of IL-2 and
GM-CSF (30,32). However, the ability of this approach
to cure leukemia or reduce the post-transplant relapse rate has yet
to be conclusively demonstrated. Thus, IL-2 would be more effective
if combined with a cytokine such as GM-CSF.
As2O3 is a chemotherapeutic
agent used in the current study to enhance the cytotoxicity of
thalidomide. As2O3 (Trisenox®) is
currently used in the treatment of the first relapse of acute
promyelocytic leukemia. The detailed mechanisms of
As2O3 cytotoxicity are not completely known,
but various preclinical studies have provided insight into the
processes involved. The mechanisms include cellular
differentiation, induction of apoptosis, and degradation of
specific acute promyelocytic leukemia (APL) transcripts,
antiproliferation, and inhibition of angiogenesis (33). Numerous studies examining the
activity of arsenic utilized the prototype APL cell line NB4, which
carries the t(15;17) translocation involving the RAR-α and PML
genes (34). This activity
generates a PML/RAR-α fusion protein between RAR-α, a nuclear
receptor for retinoic acid and PML, a growth suppressor localized
on nuclear-matrix-associated bodies. In APL studies,
As2O3 induced a differential effect that was
shown to be dose-dependent in that it induced partial
differentiation at low concentrations (0.1–0.5 mmol/l) and induced
apoptosis at relatively high concentrations (0.5–2.0 mmol/l)
(35). Apoptosis in APL patients
was shown to be, in part, secondary to the down-regulation of bcl-2
gene expression at the protein and mRNA levels as well as through
modulation of PML-RAR-α and PML (36,37).
The down-regulation of bcl-2 protein is independent of PML and
PML/RAR-α expression (38). Davison
et al showed that the apoptotic effect of
As2O3 in APL is partially dependent on JNK
activation (39). The antileukemic
effects of all-trans retinoic acid and As2O3
target RAR-α and PML, respectively, while both induce the
degradation of PML/RAR-α fusion proteins in NB4 cells (35,40).
As2O3 induces the degradation of PML/RAR-α
(as well as the wild-type PML) over a wide range of concentrations
(0.5–2.0 mmol/l) (35). Moreover,
As2O3 was shown to induce the degradation of
the PML/RAR-α fusion protein in retinoic acid-resistant cells
(35,41).
In related hematologic malignancies, such as
multiple myeloma and lymphoma, preclinical studies of
As2O3 have demonstrated similar apoptotic
effects (15,36,42,43).
Park et al demonstrated that
As2O3-induced G1 and/or G2M phase arrest in
myeloma cells (36). Simultaneous
induction of cyclin-dependent kinase inhibitor, p21 was also noted.
Liu et al showed that As2O3 induced
apoptosis in resistant cell lines and fresh myeloma cells through
p53-dependent cell cycle arrest and activation of extrinsic and
intrinsic caspase pathways (43).
Evidence exists of an immune mechanism with
As2O3 in myeloma cells with elevated LAK and
other immune cells (44). A similar
immune mechanism has yet to be demonstrated in
As2O3-treated APL.
The anti-leukemic effect of
As2O3 may partially be related to the
inhibition of angiogenesis due to interruption of the reciprocal
stimulant loop between endothelial cells releasing cytokines which
stimulate leukemic cells to release growth factors such as VEGF
(through apoptosis of the two cell types) (45). Another mechanism of
As2O3-induced apoptosis is through the
activation of caspases. As2O3 activates these
proteases, which play an important role in the degradation phase of
apoptosis, in NB4 cell lines (43,46,47).
As2O3 is able to lead to potential changes in
the membrane and increased membrane permeability with the resultant
degradation phase of apoptosis. Furthermore, the ability of
As2O3 to induce apoptosis is dependent on the
generation of reactive oxygen species (46,48).
This suggests that the effect of As2O3 is
potentiated through modulation of the glutathione redox system.
As2O3 was used in the current
study to test its efficacy in the enhancement of the cytotoxicity
of thalidomide in an acute myelogenous human leukemia cell line. It
was noted that As2O3 alone resulted in 16.97%
late apoptosis compared to 5.35% late apoptosis in the control.
When As2O3 was used concurrently with
thalidomide it resulted in 80.6% late apoptosis compared to 49.39%
late apoptosis of thalidomide alone. The combination of
thalidomide, As2O3 and IL-2 resulted in
70.14% of late apoptosis. Thus, in our study
As2O3 enhancesd the cytotoxic effect of
thalidomide in contrast to IL-2 which did not manifest any
noticeable cytotoxicity. Further studies are warranted to prove or
disprove the potential role of IL-2 to enhance the cytotoxicity of
thalidomide.
In conclusion, this study showed that the cytotoxic
effect of thalidomide is significantly enhanced when combined with
As2O3 in the KG-1a human AML cell line. These
findings point to the potential use of As2O3
in combination with thalidomide for a more efficient management of
AML by increasing the rate of complete remission for AML patients
and the least chance of relapse. Further studies are needed to
confirm the current findings. However, the results obtained are
promising since thalidomide effectiveness in the therapy of AML may
be significantly enhanced by the concurrent use of
As2O3. This may aid patients who suffer from
this disease.
Acknowledgements
This study was supported in part by NIH grant
RR03020.
References
|
1
|
Godwin JE and Smith SE: Acute myeloid
leukemia in the older patient. Crit Rev Oncol Hematol. 48:S17–S26.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Harousseuau JL: Acute myeloid leukemia in
the elderly. Blood Rev. 12:145–153. 1988. View Article : Google Scholar
|
|
3
|
Cortes JE and Kantarjian HM: Acute
lymphocytic leukemia: A comprehensive review with emphasis on
biology and therapy. Cancer. 76:2393–2417. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Estey EH, Kantarjian H and Keating MJ:
Therapy for acute myeloid leukemia. Hematology: Basic Principles
and Practice. 2nd edition. Hoffman R, Benz E Jr, Shattil S, Cohen H
and Silberstein L: Churchill Livingstone; New York: pp. 1014–1028.
1994
|
|
5
|
Thomas DA, Kantarjian H and Smith TL:
Primary refractory and relapsed adult acute lymphoblastic leukemia:
characteristics, treatment results, and prognosis with salvage
therapy. Cancer. 86:1216–1230. 1999. View Article : Google Scholar
|
|
6
|
Beran M, Estey E and O’Brien S: Topotecan
and cytarabine is an active combination regimen in myelodysplastic
syndromes and chronic myelomonocytic leukemia. J Clin Oncol.
17:2819–2830. 1999.PubMed/NCBI
|
|
7
|
Estey EH, Kantarjian HM and O’Brien S:
High remission rate, short remission duration in patients with
refractory anemia with excess blasts (RAEB) in transformation
(RAEB-t) given acute myelogenous leukemia (AML)-type chemotherapy
in combination with granulocyte-CSF (G-CSF). Cytokines Mol Ther.
1:21–28. 1995.PubMed/NCBI
|
|
8
|
Thomas D: Pilot studies of thalidomide in
acute myelogenous leukemia, myelodysplastic syndromes, and
myeloproliferative disorders. Semin Oncol. 37(Suppl 3): 26–34.
2000.
|
|
9
|
Lu C and Hassan HT: Human stem cell
factor-antibody (anti-SCF) enhances chemotherapy cytotoxicity in
human CD34+ resistant myeloid leukemia cells. Leuk Res. 30:296–302.
2006.PubMed/NCBI
|
|
10
|
Yang H, Hoshino K, Sanchez-Gonzalez B,
Kantarjian H and Garcia-Manero G: Antileukemia activity of the
combination of 5-aza-2′-deoxycytidine with valproic acid. Leuk Res.
29:739–748. 2005.PubMed/NCBI
|
|
11
|
Koeffler HP, Billing R, Lusis AJ, Sparkes
R and Golde DW: An undifferentiated variant derived from the human
acute myelogenous leukemia cell line (KG-1). Blood. 56:265–273.
1980.PubMed/NCBI
|
|
12
|
Grad JM, Bahlis NJ, Reis I, Oshiro MM,
Dalton WS and Boise LH: Ascorbic acid enhances arsenic
trioxide-induced cytotoxicity in multiple myeloma cells. Blood.
98:805–813. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Block G and Levine M: Vitamin C: a new
look. Ann Intern Med. 114:909–910. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Sakagami H and Satoh K: Modulating factors
of radical intensity and cytotoxic activity of ascorbate [review].
Anticancer Res. 17:3513–3520. 1997.PubMed/NCBI
|
|
15
|
Dai J, Weinberg RS, Waxman S and Jing Y:
Malignant cells can be sensitized to undergo growth inhibition and
apoptosis by arsenic trioxide through modulation of the glutathione
redox system. Blood. 93:268–277. 1999.PubMed/NCBI
|
|
16
|
Kruse FF, Joussen AM, Rohrschneider K,
Becker MD and Volcker HE: Thalidomide inhibits corneal angiogenesis
induced by vascular endothelial growth factor. Graefes Arch Clin
Exp Ophthalmol. 236:461–466. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Corral LG, Haslett PAJ, Muller GW, et al:
Differential cytokine modulation and T-cell activation by two
distinct classes of thalidomide analogues that are potent
inhibitors of TNF-alpha. J Immunol. 163:380–386. 1999.PubMed/NCBI
|
|
18
|
Haslett PAJ, Corral LG, Albert M and
Kaplan G: Thalidomide costimulates primary human T lymphocytes,
preferentially inducing proliferation, cytokine production, and
cytotoxic responses in the CD8+ subset. J Exp Med.
187:1885–1892. 1998. View Article : Google Scholar
|
|
19
|
Geitz H, Handt S and Zwingenberger K:
Thalidomide selectively modulates the density of cell surface
molecules involved in the adhesion cascade. Immunopharmacology.
31:213–221. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Du GJ, Lin HH, Xu QT and Wang MW:
Thalidomide inhibits growth of tumors through COX-2 degradation
independent of antiangiogenesis. Vascul Pharmacol. 43:112–119.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Heslop HE, Rooney CM and Brenner MK:
Gene-marking and hemopoietic stem cell transplantation. Blood Rev.
4:220–224. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Barret AJ: Mechanisms of the
graft-versus-leukemia reactivity. Bone Marrow Transplant. 1:61–68.
1997.
|
|
23
|
Ball ED, Mills LE, Cornwell GG Jr, Davis
BH, Coughlin CT and Howell AL: Autologous bone marrow
transplantation for acute myeloid leukemia using monoclonal
antibody-purged bone marrow. Blood. 75:1199–1206. 1990.PubMed/NCBI
|
|
24
|
Sznol M and Parkinson DR: Interleukin-2 in
therapy of hematologic malignancies. Blood. 83:2020–2222.
1994.PubMed/NCBI
|
|
25
|
Uckun FM, Kersey JH, Vallera DA, Ledbetter
JA, Weisdorf D and Myers DE: Autologous bone marrow transplantation
in high risk remission T-lineage acute lymphoblastic leukemia using
immunotoxins plus 4-hydroperoxycyclophosphamide for marrow purging.
Blood. 76:1723–1733. 1990.PubMed/NCBI
|
|
26
|
Kalland T, Belfrage H, Bhiladvala P and
Hedlund G: Analysis of the murine lymphokine-activated killer (LAK)
phenomenon: dissection of effectors and progenitors into NK-and
T-like cells. J Immunol. 38:3640–3645. 1987.PubMed/NCBI
|
|
27
|
Ochoa AC, Gromo G, Alter BJ, Sondel PM and
Bach FH: Long-term growth of lymphokine-activated killer
(LAK)-cells: role of anti CD-3, beta-IL 1, interferon-gamma and
-beta. J Immunol. 138:2728–2733. 1987.PubMed/NCBI
|
|
28
|
Peace DJ, Kern DE, Schultz KR, Greenberg
PD and Cheever MA: IL-4-induced lymphokine-activated killer cells.
Lytic activity is mediated by phenotypically distinct natural
killer-like and T-cell-like large granular lymphocytes. J Immunol.
140:3679–3685. 1988.
|
|
29
|
Naume B and Espevik T: Effects of IL-7 and
IL-12 on highly enriched CD56+ natural killer cells: a
comparative study. J Immunol. 147:2208–2214. 1991.PubMed/NCBI
|
|
30
|
Stewart-Akers AM, Cairns JS, Tweardy DJ
and McCarthy SA: Effect of granulocyte macrophage-colony
stimulating factor on lymphokine-activated killer cell induction.
Blood. 81:2672–2678. 1993.PubMed/NCBI
|
|
31
|
Rojas R, Roman J, Herrera C, Alvarez MA,
Ramirez R and Torres A: BALB/C mice injected with LSTRA leukemic
cell line are cured by in vivo treatment with IL-2 + GM-CSF. Leuk
Res. 27:351–357. 2003.PubMed/NCBI
|
|
32
|
Herrera C, Garcia-Perez MJ, Ramirez R,
Martin C, Alvarez MA and Martinez F: Lymphokine-activated killer
(LAK)-cell generation from peripheral blood stem cells by in vitro
incubation with low dose interleukin-2 plus granulocyte
macrophage-colony stimulating factor. Bone Marrow Transplant.
19:545–551. 1997. View Article : Google Scholar
|
|
33
|
Evens AM, Tallman MS and Gartenhaus RB:
The potential of arsenic trioxide in the treatment of malignant
disease: past, present, and future. Leuk Res. 28:891–900. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Lanotte M, Martin-Thouvenin V, Najman S,
Balerini P, Valensi F and Berger R: NB4, a maturation inducible
cell line with t(15;17) marker isolated from a human acute
promyelocytic leukemia (M3). Blood. 77:1080–1086. 1991.PubMed/NCBI
|
|
35
|
Chen GQ, Shi XG, Tang W, et al: Use of
arsenic trioxide in the treatment of acute promyelocytic leukemia
(APL): I. Arsenic trioxide exerts dose-dependent dual effects on
APL cells. Blood. 89:3345–3353. 1997.PubMed/NCBI
|
|
36
|
Park WH, Seol JG, Kim ES, Hyun JM, Jung CW
and Lee CC: Arsenic trioxide-mediated growth inhibition in MC/CAR
myeloma cells via cell cycle arrest in association with induction
of cyclin-dependent kinase inhibitor, p21, and apoptosis. Cancer
Res. 60:3065–3071. 2000.PubMed/NCBI
|
|
37
|
Perkins C, Kim CN, Fang G and Bhalla KN:
Arsenic induces apoptosis of multidrug-resistant human myeloid
leukemia cells that express Bcr-Abl or overexpress MDR, MRP, Bcl-2,
or Bcl-x(L). Blood. 95:1014–1022. 2000.PubMed/NCBI
|
|
38
|
Schor NF, Rudin CM, Hartman AR, Thompson
CB, Tyurina YY and Kagan VE: Cell line dependence of Bcl-2-induced
alteration of glutathione handling. Oncogene. 19:472–476. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Davison K, Mann KK, Waxman S and Miller
WH: JNK activation is a mediator of arsenic trioxide-induced
apoptosis in acute promyelocytic leukemia cells. Blood.
103:3496–3502. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Shao W, Fanelli M, Ferrara FF, Riccioni R,
Rosenauer A and Davison K: Arsenic trioxide as an inducer of
apoptosis and loss of PML/RAR alpha protein in acute promyelocytic
leukemia cells. J Natl Cancer Inst. 90:124–133. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Kinjo K, Kizaki M, Muto A, Fukuchi Y,
Umezawa A and Yamato K: Arsenic trioxide-induced apoptosis and
differentiation in retinoic acid resistant acute promyelocytic
leukemia model in hGM-CSF-producing transgenic SCID mice. Leukemia.
14:431–438. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Rousselot P, Labaume S, Marolleau JP,
Larghero J, Noguera MH and Brouet JC: Arsenic trioxide and
Melarsoprol induce apoptosis in plasma cell lines and in plasma
cells from myeloma patients. Cancer Res. 59:1041–1048.
1999.PubMed/NCBI
|
|
43
|
Liu Q, Hilsenbeck S and Gazitt Y: Arsenic
trioxide-induced apoptosis in myeloma cells: p53-dependent G1 or
G2/M cell cycle arrest, activation of caspase-8 or caspase-9, and
synergy with APO2/TRAIL. Blood. 101:4078–4087. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Deaglio S, Canella D, Baj G, Arnulfo A,
Waxman S and Malavasi F: Evidence of an immunologic mechanism
behind the therapeutical effects of arsenic trioxide on myeloma
cells. Leuk Res. 25:227–235. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Roboz GJ, Dias S, Lam G, Lane WJ, Soignet
SL and Warrell RP Jr: Arsenic trioxide induces dose-and
time-dependent apoptosis of endothelium and may exert an
antileukemic effect via inhibition of angiogenesis. Blood.
96:1525–1530. 2000.PubMed/NCBI
|
|
46
|
Gartenhaus RB, Prachand SN, Paniaqua M, Li
Y and Gordon LI: Arsenic trioxide cytotoxicity in steroid and
chemotherapy-resistant myeloma cell lines: enhancement of apoptosis
by manipulation of cellular redox state. Clin Cancer Res.
8:666–672. 2002.PubMed/NCBI
|
|
47
|
Kitamura K, Minami Y, Yamamoto K, et al:
Involvement of CD95-independent caspase 8 activation in arsenic
trioxide-induced apoptosis. Leukemia. 14:1743–1750. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Gupta S, Yel L, Kim D, Kim C, Chiplunkar S
and Gollapudi S: Arsenic trioxide induces apoptosis in peripheral
blood T lymphocytes subsets by inducing oxidative stress: a role of
Bcl-2. Mol Cancer Ther. 2:711–719. 2003.PubMed/NCBI
|