Introduction
Cisplatin is a drug widely used in the treatment of
cancer and is often combined with radiotherapy. On the other hand,
whether cyclopentenylcytosine (CPEC) has potential in anticancer
treatment is currently under investigation (1–4). CPEC
is cytotoxic to various cell types, and it sensitizes human colon
carcinoma HT-29 cells to treatment with cisplatin (2). CPEC is a cytidine analogue, which, due
to its intracellular activation to its 5′-triphosphate form, is a
non-competitive inhibitor of cytidinetriphosphate synthetase. The
exposure of cancer cells to CPEC results in the depletion of
cellular CTP (cytidine 5′-triphosphate) and dCTP pools, leading to
inhibition of RNA and DNA synthesis, as well as S-phase
accumulation of mammalian cells (3,5,6). Since
CPEC induces depletion of CTP, one of the building blocks of DNA,
it may influence the proper repair of DNA after exposure to
ionizing radiation. Van Bree et al found that CPEC enhances
the radiosensitization effect of gemcitabine in human pancreatic
tumour cells; however, the radiosensitization effect of CPEC alone
was only modest (3).
Cisplatin treatment induces DNA damage via the
formation of interstrand and intrastrand crosslinks (7). Cisplatin crosslinks DNA in several
different ways inducing cell cycle arrest, inhibition of DNA
replication and transcription, and eventually apoptosis (8). The inhibition of DNA damage repair has
also been implicated to be involved in the cytotoxicity of
cisplatin (9). Therefore, cisplatin
is an effective radiosensitizer used in combination with
radiotherapy in a wide range of malignancies (10,11).
Cisplatin-induced radiosensitization occurs via the inhibition of
the non-homologous end-joining pathway (8,12).
Combination treatment of CPEC with cisplatin was
investigated by Gharehbaghi et al (1,2). A
synergistic cytotoxicity was found in HT-29 cells after treatment
of the cells, initially with 1 μM CPEC and subsequently with
cisplatin. Less synergy was found when cells were first incubated
with cisplatin and then treated with CPEC.
Although favourable results have been obtained with
the combination treatment of cisplatin and radiotherapy, relapses
still occur. Therefore, trimodality treatments have been
investigated in our laboratory. Bergs et al (11) observed that hyperthermia further
increased the effects of combined cisplatin and radiation treatment
in several human tumour cell lines. The present study investigated
whether CPEC enhances cisplatin-induced radiosensitizing effects in
human lung tumour cells.
Materials and methods
Cell culture
The human NSCLC cell line SWp (parental SW-1573
cells, squamous cell carcinoma) and its gemcitabine-resistant
variant, SWg, were grown at 37°C as monolayers in 75-cm2
tissue culture flasks (Costar/Corning) in Leibovitz-15 medium
(L-15; Gibco-BRL) supplemented with 10% fetal bovine serum, 2 mM
glutamine, 100 U/ml penicillin and 100 mg/ml streptomycin. The L-15
medium does not require CO2. The doubling time of the
two cell types during exponential growth is 24 h. In the SWg cell
line, which is derived from SWp, the dCK gene is disrupted
(13).
Irradiation
Irradiation was performed with γ-rays from a
137Cs source. At a dose rate of ~0.6 Gy/min, single
doses up to 8 Gy were applied.
Clonogenic cell survival
Cells were plated at the appropriate cell numbers.
After 2 h, the cells were attached to the bottom of the plate and
treated for 2 h with 0.1, 1 or 2 μM CPEC (NSC 375575). The medium
was then refreshed, and cells were treated for 2 h with 4 μM (1.2
g/ml) cisplatin (Platosin®, Pharmachemie, Haarlem, The
Netherlands). After this treatment, the medium was refreshed again,
and the cells were irradiated. In control experiments, cells were
treated with physiological salt solution, CPEC, cisplatin or
radiation only. Subsequently, cells were incubated for 10 days.
Surviving colonies were fixated and stained with
glutaraldehyde-crystal violet solution and counted (14). Following dose D, surviving fractions
S(D)/S(0) were corrected for toxicity of CPEC or cisplatin alone,
or a combination treatment of CPEC and cisplatin. Survival curves
were analyzed using SPSS (Chicago, IL, USA) statistical software by
means of fitting data by weighted linear regression, according to
the linear-quadratic formula: S(D)/S(0)=exp-(αD+βD2)
(15–19).
Results
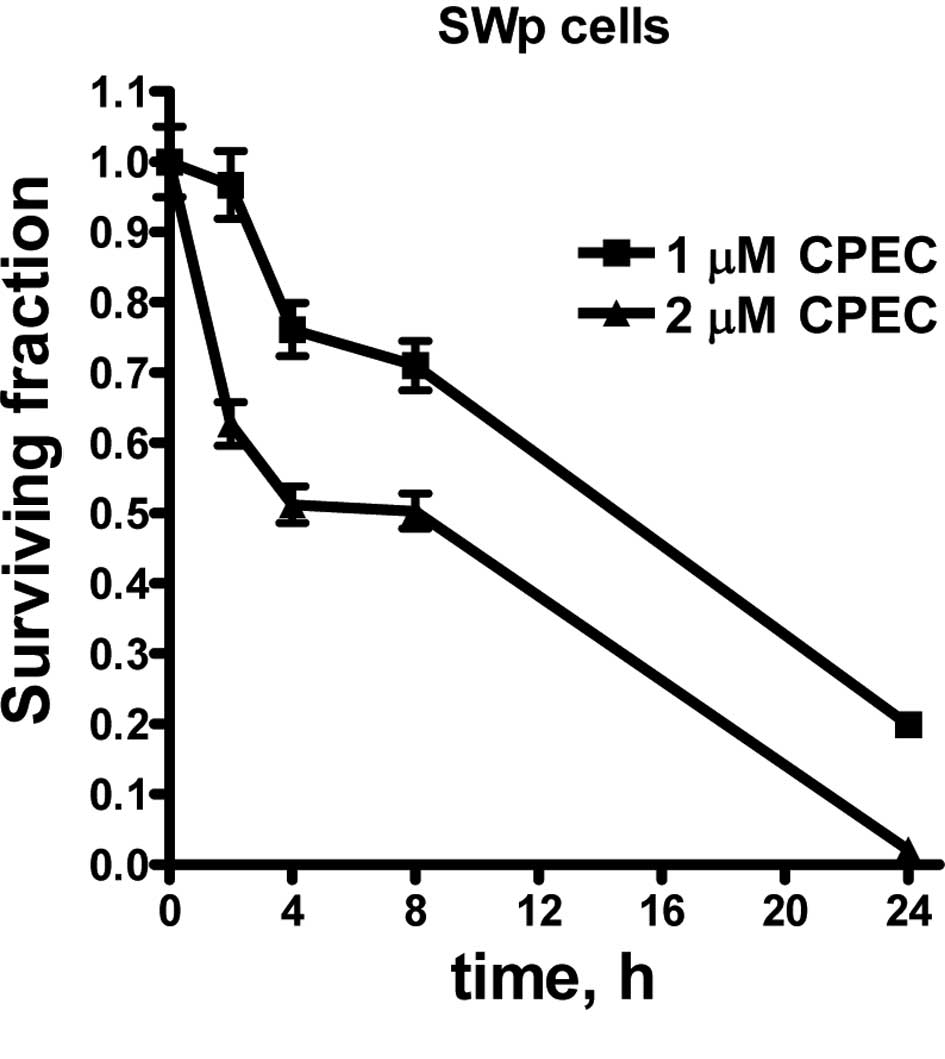
To study the influence of CPEC on cisplatin
radiosensitization, we initially determined the cytotoxicity of
CPEC alone. Fig. 1 shows the
toxicity of 1 and 2 μM CPEC on SWp cells after different incubation
times. A similar pattern was obtained for the SWg cells, indicating
that an intact dCK activity is not required for CPEC cytotoxicity
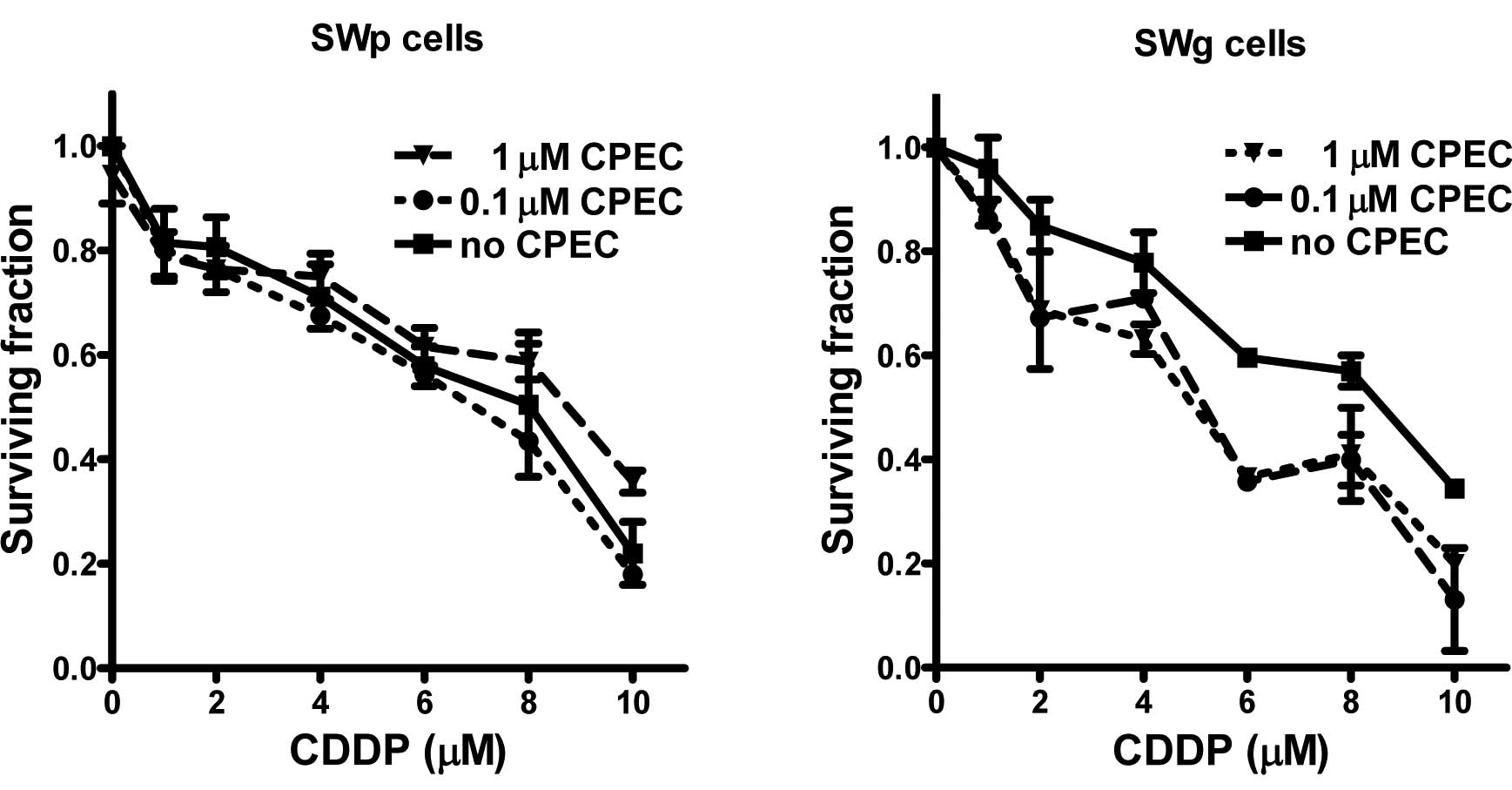
(data not shown). To investigate the cisplatin-sensitization by
CPEC, cells were incubated for 2 h with 0.1 or 1 μM CPEC. The
concentrations were selected to compare almost no (0.1 μM) and
moderate (1 μM) cytotoxicity of CPEC. In addition, the
concentration of 1 μM CPEC was described by Gharehbaghi et
al to sensitize the cisplatin toxicity of HT-29 cells (2). As shown in Fig. 2A, the cytotoxicity of cisplatin in
SWp cells was not increased by CPEC. However, in SWg cells the CPEC
treatment enhanced the cell killing effect of cisplatin (Fig. 2B).
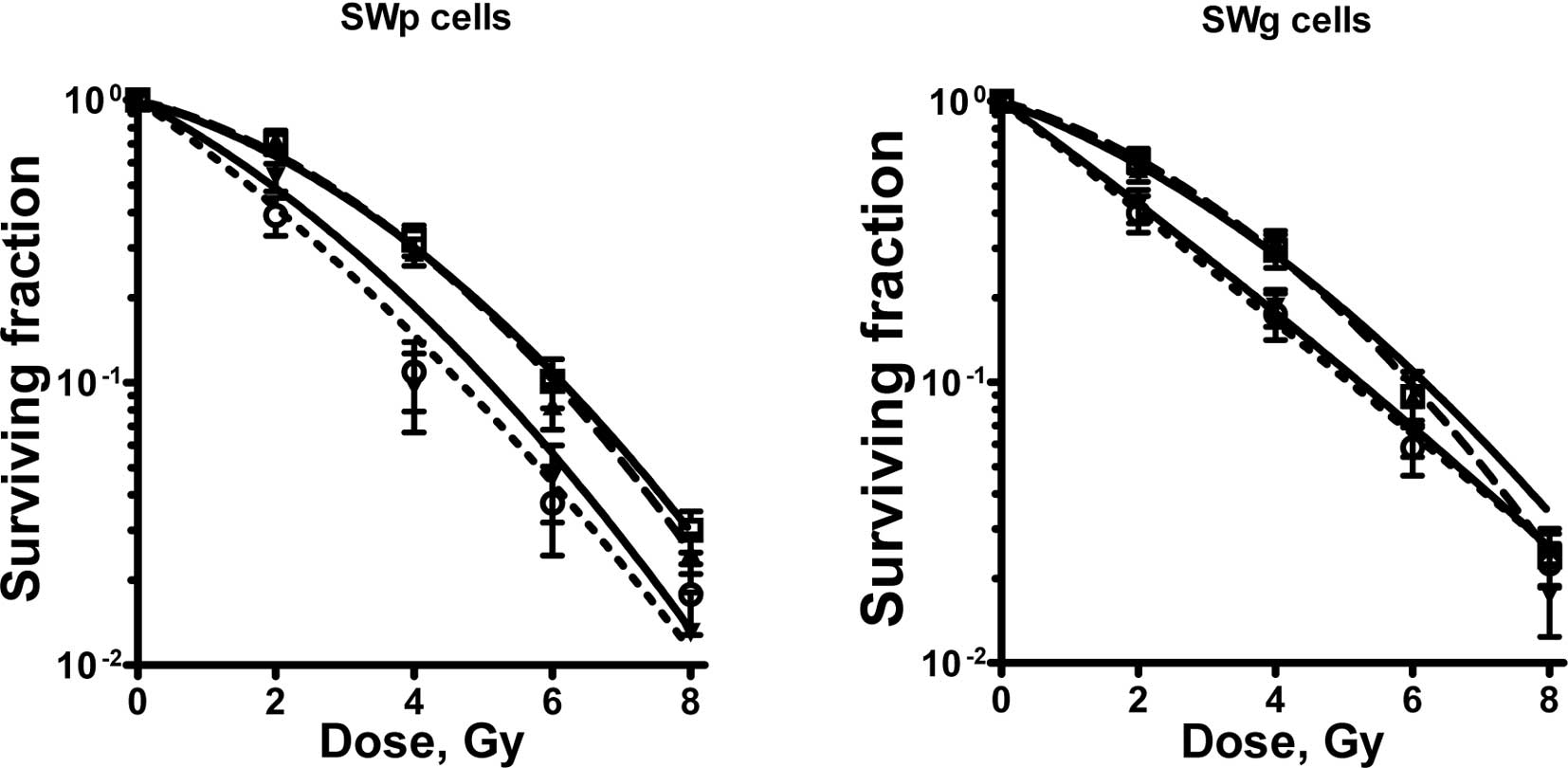
Fig. 3 shows the
radiosensitization curves. The linear-quadratic parameters of these
radiation-dose survival curves are provided in Table I. Fig.
3 shows that cisplatin treatment clearly radiosensitized the
lung tumour cells. This is evident from the value of the
sensitizing enhancement ratios of the α-parameter provided in
Table I. The increase in the α
value after cisplatin treatment was highly significant. However,
CPEC treatment did not radiosensitize these cells, nor did it
sensitize the cisplatin-induced radiosensitization. The slight
increase noted in the α value of the SWp cells after CPEC and
radiation was not significant.
 | Table ILinear-quadratic parameters and
sensitizing enhancement ratios of linear-quadratic parameter α. |
Table I
Linear-quadratic parameters and
sensitizing enhancement ratios of linear-quadratic parameter α.
| LQ parameter | α,
Gy−1 | β,
Gy−2 |
Sensitizer-enhancement ratio αa |
|---|
| SWp cells |
| Radiation only | 0.16±0.011 | 0.038±0.003 | 1.00 |
| Radiation + 1 μM
CPEC | 0.21±0.033 | 0.027±0.009 | 1.28±0.22 |
| Radiation + 4 μM
cisplatin | 0.41±0.014 | 0.006±0.004 | 2.52±0.19b |
| Radiation + 1 μM
CPEC + 4 μM cisplatin | 0.45±0.017 | 0.001±0.005 | 2.77±0.21b |
| SWg cells |
| Radiation only | 0.16±0.013 | 0.035±0.007 | 1.00 |
| Radiation + 1 μM
CPEC1 | 0.16±0.029 | 0.039±0.008 | 1.00±0.20 |
| Radiation + 4 μM
cisplatin | 0.30±0.016 | 0.030±0.010 | 1.88±0.18b |
| Radiation + 1 μM
CPEC + 4 μM cisplatin | 0.40±0.031 | 0.021±0.011 | 2.55±0.20b |
Discussion
Our results show that 4 μM of cisplatin with a 2-h
incubation sensitized SW-1573 cells to ionizing radiation. In
contrast to Akudugu and Slabbert (20), who did not observe any
radiosensitization of cisplatin in CHO cells after an <8-h
incubation, we clearly showed that a 2-h exposure to cisplatin
radiosensitized SW-1573 cells. The difference may be due to the
higher concentration of cisplatin used in our study (4 vs. 1.5 μM
used by Akudugu and Slabbert) or due to the different cell type.
Bergs et al (11,21) demonstrated that radiosensitization
with cisplatin was concentration-dependent. Incubation with 5 μM
radiosensitized SW1573 cells, but that with 1 μM cisplatin did not
(11). Cisplatin radiosensitization
has been shown for several different cell lines in a number of
studies, and usually higher doses than 1 μM were used (11,21–23).
Wilkins et al (22) studied
glioblastoma cells using higher concentrations (12 μM) of cisplatin
and a higher radiation dose (18 Gy). Begg et al (23) studied a RIF1 cell line and used
similar concentrations of cisplatin and radiation dose as those in
our study.
Our experimental design did not include the study of
potentially lethal damage repair (PLDR), since the cells were not
irradiated in the plateau phase, but were plated before
irradiation. However, the cisplatin-induced radiosensitization in
our study was likely due to an effect on PLDR, as shown by the
increase in the linear parameter, α. This is in agreement with the
results found by Wilkins et al who observed inhibition of
potentially lethal damage recovery by cisplatin (22). Bergs et al also demonstrated
that cisplatin-induced radiosensitization was due to the inhibition
of PLDR (11,21).
In the present study, CPEC sensitized cisplatin in
the SWg cell line, but did not increase the cisplatin cytoxicity in
the SWp cell line. The cell lines differ only in the fact that the
SWg line is deoxycytidine kinase (dCK)-deficient (13), although this deficiency has no
influence on the depletion of cellular CTP levels by CPEC (3). Therefore, it is difficult to explain
why CPEC sensitized cisplatin in the one cell line but not in the
other one. Gharehbaghi et al (2) clearly showed that pre-incubation with
1 μM of CPEC sensitizes HT-29 cells to cisplatin.
In this study, incubation with CPEC neither
sensitized these cells to ionizing radiation nor to
cisplatin-induced radiosensitization. The radiosensitization
properties of CPEC have been demonstrated in human pancreatic
carcinoma cells upon incubation with gemcitabine (3,4). In
these studies, it was observed that CPEC, at low, clinically
achievable and non-toxic doses, increased dFdC effectiveness; its
radiosensitizing effect in human pancreatic carcinoma cells was
also shown. However, CPEC alone did not radiosensitize these cells.
This latter finding is in agreement with our findings in lung
tumour cells.
In conclusion, cisplatin sensitized the human lung
tumour cells to ionizing radiation, but pre-treatment with CPEC
neither enhanced cisplatin cytotoxicity nor the cisplatin-induced
radiosensitizing effects.
Acknowledgements
We would like to thank Mrs. Arabella Burgers and Mr.
Daan van Abel for the technical assistance in the laboratory. The
Maurits and Anna de Kock, and the Nijbakker Morra foundations are
acknowledged for sponsoring the laboratory equipment.
References
|
1
|
Gharehbaghi K, Zhen W, Fritzer-Szekeres M,
Szekeres T and Jayaram HN: Studies on the antitumour activity and
biochemical actions of cyclopentenyl cytosine against human colon
carcinoma HT-29 in vitro and in vivo. Life Sci. 64:103–112. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Gharehbaghi K, Szekeres T, Yalowitz JA,
Fritzer-Szekeres M, Pommier YG and Jayaram HN: Sensitizing human
colon carcinoma HT-29 cells to cisplatin by cyclopentenylcytosine,
in vitro and in vivo. Life Sci. 68:1–11. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Van Bree C, Rodermond HM, Leen R, Medema J
and van Kuilenburg AB: Cyclopentenylcytosine increases gemcitabine
radiosensitisation in human pancreatic cancer cells. Br J Cancer.
98:1226–1233. 2008.PubMed/NCBI
|
|
4
|
Van Bree C, Barten-van Rijbroek AD, Leen
R, Rodermond HM, van Kuilenburg AB and Kal HB: Cyclopentenyl
cytosine has biological and anti-tumour activity, but does not
enhance the efficacy of gemcitabine and radiation in two animal
tumour models. Int J Oncol. 34:813–819. 2009.PubMed/NCBI
|
|
5
|
Kang GJ, Cooney DA, Moyer JD, Kelley JA,
Kim HY, Marquez VE and Johns DG: Cyclopentenylcytosine
triphosphate. Formation and inhibition of CTP synthetase. J Biol
Chem. 264:713–718. 1989.PubMed/NCBI
|
|
6
|
Bierau J, van Gennip AH, Leen R, Meinsma
R, Caron HN and van Kuilenburg AB: Cyclopentenyl cytosine-induced
activation of deoxycytidine kinase increases gemcitabine anabolism
and cytotoxicity in neuroblastoma. Cancer Chemother Pharmacol.
57:105–113. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Crul M, van Waardenburg RC, Beijnen JH and
Schellens JH: DNA-based drug interactions of cisplatin. Cancer
Treat Rev. 28:291–303. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Myint WK, Ng C and Raaphorst GP: Examining
the non-homologous repair process following cisplatin and radiation
treatments. Int J Radiat Biol. 78:417–424. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lawrence TS, Blackstock AW and McGinn C:
The mechanism of action of radiosensitization of conventional
chemotherapeutic agents. Sem Radiat Oncol. 13:13–21. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Rose PG, Bundy BN, Watkins EB, Thigpen JT,
Deppe G, Maiman MA, Clarke-Pearson DL and Insalaco S: Concurrent
cisplatin-based radiotherapy and chemotherapy for locally advanced
cervical cancer. N Engl J Med. 340:1144–1153. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bergs JW, Haveman J, ten Cate R, Medema
JP, Franken NA and van Bree C: Effect of 41ºC and 43ºC on cisplatin
radiosensitization in two human carcinoma cell lines with different
sensitivities for cisplatin. Oncol Rep. 18:219–226. 2007.
|
|
12
|
Haveman J, Castro Kreder N, Rodermond HM,
van Bree C, Franken NA, Stalpers LJ, Zdzienicka MZ and Peters GJ:
Cellular response of X-ray sensitive hamster mutant cell lines to
gemcitabine, cisplatin and 5-fluorouracil. Oncol Rep. 12:187–192.
2004.PubMed/NCBI
|
|
13
|
Van Bree C, Castro Kreder N, Loves WJ,
Franken NA, Peters GJ and Haveman J: Sensitivity to ionizing
radiation and chemotherapeutic agents in gemcitabine-resistant
human tumour cell lines. Int J Radiat Oncol Biol Phys. 54:237–244.
2002.PubMed/NCBI
|
|
14
|
Franken NA, Rodermond HM, Stap J, Haveman
J and van Bree C: Clonogenic assay of cells in vitro. Nat Protoc.
1:2315–2319. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Barendsen GW, van Bree C and Franken NA:
Importance of cell proliferative state and potentially lethal
damage repair on radiation effectiveness: Implications for combined
tumour treatments (review). Int J Oncol. 19:247–256. 2001.
|
|
16
|
Barendsen GW: Parameters of
linear-quadratic radiation dose-effect relationships: dependence on
LET and mechanisms of reproductive cell death. Int J Radiat Biol.
71:649–655. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Franken NA, van Bree C, Veltmaat MA,
Rodermond HM, Haveman J and Barendsen GW: Radiosensitization by
bromodeoxyuridine and hyperthermia: analysis of linear and
quadratic parameters of radiation survival curves of two human
tumour cell lines. J Radiat Res. 42:179–190. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Franken NA, van Bree C, Kipp JBA and
Barendsen GW: Modification of potentially lethal damage in
irradiated Chinese hamster V79 cells after incorporation of
halogenated pyrimidines. Int J Radiat Biol. 72:101–109. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Franken NA, van Bree C, Streefkerk JO,
Kuper IMJA, Rodermond HM, Kipp JBA, Haveman J and Barendsen GW:
Radiosensitization by iodo-deoxyuridine in cultured SW-1573 human
lung tumour cells: Effects on α and β of the linear-quadratic
model. Oncol Rep. 4:1073–1076. 1997.PubMed/NCBI
|
|
20
|
Akudugu JM and Slabbert JP: Modulation of
radiosensitivity in Chinese hamster lung fibroblasts by cisplatin.
Can J Physiol Pharmacol. 86:257–263. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Bergs JW, Franken NA, ten Cate R, van Bree
C and Haveman J: Effects of cisplatin and gamma-irradiation on cell
survival, the induction of chromosomal aberrations and apoptosis in
SW-1573 cells. Mutat Res. 594:148–154. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Wilkins DE, Heller DP and Raaphorst GP:
Inhibition of potentially lethal damage recovery by cisplatin in a
brain tumour cell line. Anticancer Res. 13:2137–2142.
1993.PubMed/NCBI
|
|
23
|
Begg AC, van Der Kolk PJ, Dewit L and
Bartelink H: Radiosensitization by cisplatin of RIF1 tumour cells
in vitro. Int J Radiat Biol. 50:871–884. 1986. View Article : Google Scholar : PubMed/NCBI
|