Introduction
Prostate adenocarcinoma is one of the most commonly
diagnosed carcinomas in the Western world and a leading cause of
cancer-related death (1). Localized
prostate cancer can be cured by various treatment modalities,
whereas in advanced stages hormonal ablation represents the most
effective systemic treatment option. However, androgen
insensitivity invariably develops and is responsible for prostate
cancer lethality. Although established, the use of doxetacel
chemotherapy is only associated with a 3-month gain in overall
survival. Thus, alternative effective systemic therapies are
required. An improved insight into the molecular mechanisms of
prostate cancer progression, which may result in novel therapeutic
options, is therefore crucial.
BRAF, a member of the RAF family of serine/threonine
kinases, can be activated by a somatic mutation in many human
cancers. BRAF mutations are reported to occur at high frequencies
in malignant melanomas and thyroid papillary carcinomas and at
lower frequencies in a variety of other human types of cancer
(2). Several BRAF inhibitors are
clinically available, including the VEGFR/PDGFR/KIT/RAF-inhibitor
sorafenib (BAY43-9006) which has been shown to exhibit significant
anti-BRAF activity in vitro, suggesting a therapeutic option
for tumors carrying BRAF mutations (3,4).
Oncogenic activating BRAF mutations were recently
reported in approximately 10% of a series of 204 non-pretreated
prostate cancer cases (5). This
raises the possibility that BRAF inhibitors are a promising
therapeutic option for androgen-independent prostate cancer
patients in whom all current treatments have only limited efficacy.
Studies involving BRAF mutations in hormone refractory prostate
cancer patients are lacking. Therefore, 43 hormone refractory
prostate cancer tissue samples were analyzed for BRAF
mutations.
Materials and methods
Tissue samples
Paraffin-embedded tissue samples from 43 patients
with hormone refractory prostate cancer were collected between 1999
and 2007 at the Institute of Pathology of the University Medical
Center Hamburg-Eppendorf. Hormone refractory disease was defined as
an increased prostate-specific agent (PSA) during anti-androgen
therapy on three consecutive measurements. Tissue samples were
obtained by palliative transurethral resections. All patients had
high-grade cancer (Table I).
 | Table ITumor characteristics and the BRAF
mutation status in 43 cases of hormone refractory prostate
cancer. |
Table I
Tumor characteristics and the BRAF
mutation status in 43 cases of hormone refractory prostate
cancer.
| Sample no. | BRAF-11 | BRAF-15 | Age (years) | Gleason score |
|---|
| Ha 1 | wt | wt | 80 | 4+5 |
| Ha 2 | wt | wt | 79 | 4+5 |
| Ha 3 | wt | wt | 55 | 5+4 |
| Ha 4 | wt | wt | 79 | 5+4 |
| Ha 5 | wt | wt | 84 | 4+4 |
| Ha 6 | wt | wt | 84 | 5+4 |
| Ha 7 | wt | wt | 70 | 4+4 |
| Ha 8 | wt | wt | 76 | 4+5 |
| Ha 9 | wt | wt | 86 | 4+5 |
| Ha 10 | wt | wt | 59 | 4+5 |
| Ha 11 | wt | wt | 77 | 4+5 |
| Ha 12 | wt | wt | 76 | 4+3 |
| Ha 13 | wt | wt | 85 | 4+5 |
| Ha 14 | wt | wt | 83 | 4+5 |
| Ha 15 | wt | wt | 70 | 4+5 |
| Ha 16 | wt | wt | 65 | 4+5 |
| Ha 17 | wt | wt | 79 | 5+5 |
| Ha 18 | wt | wt | 85 | 4+5 |
| Ha 19 | wt | wt | 73 | 5+5 |
| Ha 20 | wt | wt | 78 | 4+5 |
| Ha 21 | wt | wt | 61 | 4+5 |
| Ha 22 | wt | wt | 61 | 4+4 |
| Ha 23 | wt | wt | 64 | 4+3 |
| Ha 24 | wt | wt | 75 | 4+5 |
| Ha 25 | wt | wt | 74 | 5+4 |
| Ha 26 | wt | wt | 80 | 4+5 |
| Ha 27 | wt | wt | 86 | 3+4 |
| Ha 28 | wt | wt | 64 | 5+4 |
| Ha 29 | wt | wt | 87 | 4+5 |
| Ha 30 | wt | wt | 73 | 4+5 |
| Ha 31 | wt | wt | 83 | 4+5 |
| Ha 32 | wt | wt | 88 | 4+5 |
| Ha 33 | wt | wt | 84 | 4+5 |
| Ha 34 | wt | wt | 63 | 4+5 |
| Ha 35 | wt | wt | 80 | 4+4 |
| Ha 36 | wt | wt | 86 | 4+5 |
| Ha 37 | wt | wt | 77 | 5+4 |
| Ha 38 | wt | wt | 70 | 4+5 |
| Ha 39 | wt | wt | 67 | 4+5 |
| Ha 40 | wt | wt | 76 | 4+5 |
| Ha 41 | wt | wt | 89 | 3+4 |
| Ha 42 | wt | wt | 72 | 4+5 |
| Ha 43 | wt | wt | 67 | 5+5 |
| Control | wt | V600E | | |
BRAF mutation analysis
Representative tumor areas of the paraffin tissue
block containing at least 70% tumor cells were selected. Two tissue
cylinders (0.6 mm in diameter, ~5-mm long) were punched from each
block using a hollow needle and were subjected to DNA isolation
using a commercial kit (QIAmp DNA mini kit; Qiagen, Hilden,
Germany). Isolated DNA (70 ng) was used for PCR to generate BRAF
exons 11- and 15-specific DNA fragments. Primers were: BRAF-11:
forward, 5′-tccctctcaggcataaggtaa-3′ and reverse 5′-cgaacagtg
aatatttcctttgat-3′; and BRAF-15, forward 5′-tcataatgcttgctctg
atagga-3′ and reverse 5′-ggccaaaaatttaatcagtgga-3′. PCR was
performed on a thermal cycler with the following steps: i) initial
template DNA denaturation at 95˚C for 10 min; ii) 34 cycles of 30
sec at 95˚C, 120 sec at 58˚C and 75 sec at 72˚C and iii) a 7-min
extension at 72˚C. For sequencing, 5 μl of the BRAF exons 11- and
15-specific PCR product were treated with 2 μl ExoSAP (USB Europe
GmbH, Staufen, Germany) for 15 min at 37˚C and 15 min at 80˚C to
remove unincorporated primers. The treated PCR products were
subjected to sequencing using the primers outlined above. The
sequencing reaction was performed on a thermal cycler with the
following steps: i) 10 min at 95˚C (polymerase activation); ii) 10
sec at 95˚C (denaturation) and iii) 35 cycles of 10 sec at 55˚C
followed by 2 min at 60˚C. The sequencing products were
ethanol-precipitated to remove excess primers and analyzed on an
ABI PRISM 3100 genetic analyzer. The samples were processed in
duplicate starting from the PCR. Forward and reverse sequences were
compared manually to the BRAF reference sequence (NG_007873.1). A
mutation was assumed only when it was detected in both analyses. A
case of serrated adenoma of the caecum with a known V600E mutation
was analyzed in parallel as a positive control.
Results and Discussion
BRAF is a member of the RAF family of protein
kinases that includes the members ARAF, BRAF and CRAF (6). BRAF is the only RAF protein to be
mutated in approximately 8% of human tumors, resulting in the
intensive study of this gene (7).
In our study, the BRAF mutation status and tumor characteristics of
the patients are shown in Table I.
Mutations of BRAF were reported in approximately 66% of melanomas
and in smaller percentages in other types of cancer, including
thyroid, colonic and ovarian, as well as in some sarcomas (2,7,8). In
patients with germ cell tumors, the BRAF mutation appears to
indicate resistance against cisplatin treatment (9). However, over 30 different mutations in
BRAF have been identified (10,11), a
single base-pair substitution in exon 15 at codon 600 (V600E) is
found in over 80% of cases. The majority of mutations identified
cause constitutive kinase activation with the V600E mutation
demonstrating approximately 500-fold greater kinase activity than
wild-type BRAF. Supporting its classification as an oncogene, V600E
BRAF stimulates ERK signaling, induces proliferation and in model
systems is capable of promoting transformation. As suggested by
pre-clinical studies, tumors with a V600E BRAF mutation remain
dependent upon BRAF for proliferation and survival (12,13).
Given its frequent occurrence in human cancer, efforts are underway
to develop targeted inhibitors of BRAF and its downstream effectors
(14).
Cho et al (5)
suggested that BRAF mutations may be found in a significant
proportion of prostate cancers. In a series of 206 prostate
cancers, these authors reported a BRAF mutation rate of
approximately 10%. The BRAF-mutated tumors in this study tended to
have a higher Gleason score, a higher pre-operative serum PSA
level, as well as a more advanced tumor stage [median PSA, 10.3
ng/ml (5.5–98); Gleason score, ≥7b in 14/21 (67%) patients; stage,
≥pT3a in 12/21 (57.1%) patients]. A role of BRAF activation in
prostate cancer development and progression is also consistent with
data from Gao et al (15),
who demonstrated activation of the Akt and BRAF/Erk MAP kinase
signaling pathway in an androgen-independent prostate cancer model
established in mice.
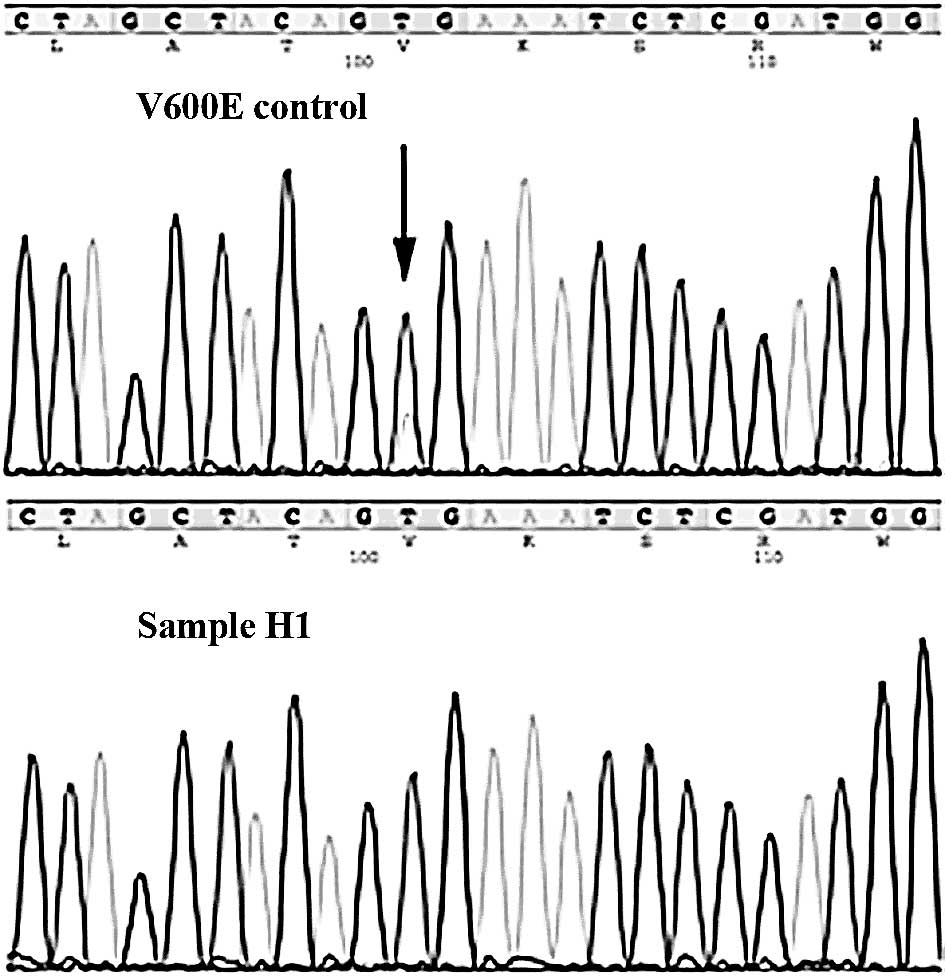
However, in our cohort of 43 hormone refractory
prostate cancer specimens no BRAF mutations were found, while the
control case (serrated adenoma of the caecum) showed the known
mutation, V600E (Fig. 1). Since the
204 cancer cases analyzed by Cho et al (5) were untreated primary tumors, one
explanation for the different results observed may be that BRAF
mutations are involved only in the early stages of prostate cancer
development and that tumor maintenance and progression towards
advanced and/or hormone-insensitive cancers are independent of the
BRAF pathway, in order that BRAF wild-type cells eventually
overgrow the BRAF-mutated cells. This assumption is consistent with
experimental findings from Jeong et al (16). These authors developed a genetically
engineered mouse (GEM) model of invasive prostate cancers, whereby
an activating mutation of BRAF V600E was targeted to the epithelial
compartment of the prostate gland on the background of Ink4a/Arf
deficiency. These GEM mice developed prostate gland hyperplasia
with progression to rapidly growing invasive adenocarcinoma without
evidence of AKT activation, providing genetic proof that the
activation of MAP kinase signaling is sufficient to drive prostate
tumorigenesis. Notably, the genetic extinction of BRAF V600E in
established prostate tumors did not lead to tumor regression,
indicating that, while sufficient to initiate development of
invasive prostate adenocarcinoma, BRAF V600E is not required for
its maintenance. Based on these findings it can be speculated that
BRAF-positive tumor cell clones are eliminated by other tumor cell
clones during tumor progression towards hormone resistance, which
could explain the lack of BRAF mutations in our series of
hormone-resistant prostate cancers.
However, other groups studying less advanced
prostate cancers failed to show BRAF mutations. For example, Liu
et al did not find any BRAF mutations in 93 non-pretreated
prostate cancer tissues (17). The
same holds true for a smaller study by Cohen et al who also
failed to show mutations in a small set of 17 untreated prostate
cancer samples (2). An ethnic bias
towards the prevalence of prostate BRAF mutations may represent an
alternative explanation for the difference in results. In contrast
to Cho et al (5) who
exclusively analyzed Korean patients, our study as well as the
aforementioned studies by Liu et al (17) and Cohen et al (2) examined Caucasian patients. The
prevalence for an ethnic relationship between tumor molecular
abnormalities and ethnic variations is well documented from the
study of epidermal growth factor receptor mutations in non-small
cell lung cancer. Patients from Asian descent are more likely to
have non-small cell lung cancer with epidermal growth factor
receptor-activating mutations than patients from the US (18). Moreover, HER2 amplification is more
frequent in breast cancers of Korean and Saudi Arabian patients
than in those of Caucasian patients (19,20).
Technical errors are another possible explanation
for conflicting results in molecular analyses. The majority of BRAF
mutations reported by Cho et al (5) were V600A or V600M. These mutations are
transitions uncommon in cancers in Caucasian individuals (21). It is known that such transitions can
be artificially incorporated into DNA which has been fixed in
formalin (22). However, even in
the event that all V600A or V600M mutations were caused by
technical errors in the study of Cho et al (5), the BRAF mutation rate would not have
dropped to zero. The large scale of their study at least allowed
for the detection of 2 of 206 cases with V600E mutations, which is
not a typical technical artifact.
In conclusion, BRAF mutations are rare in early- and
late-stage prostate cancer. Collectively, approximately 1% of
prostate cancers harbor BRAF mutations. Since more than 11,000 men
die from hormone refractory prostate cancer in Germany alone,
testing a cohort of prostate cancers for BRAF mutations must be
considered in a clinical trial when potent BRAF-inhibiting drugs
become available.
Acknowledgements
A grant support was obtained from the German
Federation Ministry of Education and Science in the framework of
the program for medical genome research (FKZ:01GS08189).
References
|
1
|
Jemal A, Murray T, Ward E, et al: Cancer
statistics, 2005. CA Cancer J Clin. 1:10–30. 2005. View Article : Google Scholar
|
|
2
|
Cohen Y, Xing M, Mambo E, et al: BRAF
mutation in papillary thyroid carcinoma. J Natl Cancer Inst.
8:625–627. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wilhelm SM, Carter C, Tang L, et al: BAY
43-9006 exhibits broad spectrum oral antitumor activity and targets
the RAF/MEK/ERK pathway and receptor tyrosine kinases involved in
tumor progression and angiogenesis. Cancer Res. 19:7099–7109. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Preto A, Goncalves J, Rebocho AP, et al:
Proliferation and survival molecules implicated in the inhibition
of BRAF pathway in thyroid cancer cells harbouring different
genetic mutations. BMC Cancer. 1:3872009. View Article : Google Scholar
|
|
5
|
Cho NY, Choi M, Kim BH, Cho YM, Moon KC
and Kang GH: BRAF and KRAS mutations in prostatic adenocarcinoma.
Int J Cancer. 8:1858–1862. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Chong H, Vikis HG and Guan KL: Mechanisms
of regulating the Raf kinase family. Cell Signal. 5:463–469. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Davies H, Dicks E, Stephens P, et al: High
throughput DNA sequence variant detection by conformation sensitive
capillary electrophoresis and automated peak comparison. Genomics.
3:427–432. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kimura ET, Nikiforova MN, Zhu Z, Knauf JA,
Nikiforov YE and Fagin JA: High prevalence of BRAF mutations in
thyroid cancer: genetic evidence for constitutive activation of the
RET/PTC-RAS-BRAF signaling pathway in papillary thyroid carcinoma.
Cancer Res. 7:1454–1457. 2003.PubMed/NCBI
|
|
9
|
Honecker F, Wermann H, Mayer F, et al:
Microsatellite instability, mismatch repair deficiency, and BRAF
mutation in treatment-resistant germ cell tumors. J Clin Oncol.
13:2129–2136. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Bamford S, Dawson E, Forbes S, Clements J,
Pettett R, Dogan A, Flanagan A, Teague J, Futreal PA, Stratton MR
and Wooster R: The COSMIC (Catalogue of Somatic Mutations in
Cancer) database and website. Br J Cancer. 91:355–358.
2004.PubMed/NCBI
|
|
11
|
Wan PT, Garnett MJ, Roe SM, Lee S,
Niculescu-Duvaz D, Good VM, Jones CM, Marshall CJ, Springer CJ,
Barford D and Marais R: Mechanism of activation of the RAF-ERK
signaling pathway by oncogenic mutations of B-RAF. Cell.
116:855–867. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hoeflich KP, Gray DC, Eby MT, et al:
Oncogenic BRAF is required for tumor growth and maintenance in
melanoma models. Cancer Res. 2:999–1006. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sumimoto H, Miyagishi M, Miyoshi H, et al:
Inhibition of growth and invasive ability of melanoma by
inactivation of mutated BRAF with lentivirus-mediated RNA
interference. Oncogene. 36:6031–6039. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Pratilas CA and Solit DB: Therapeutic
strategies for targeting BRAF in human cancer. Rev Recent Clin
Trials. 2:121–134. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Gao H, Ouyang X, Banach-Petrosky WA,
Gerald WL, Shen MM and Abate-Shen C: Combinatorial activities of
Akt and B-Raf/Erk signaling in a mouse model of
androgen-independent prostate cancer. Proc Natl Acad Sci USA.
39:14477–14482. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Jeong JH, Wang Z, Guimaraes AS, et al:
BRAF activation initiates but does not maintain invasive prostate
adenocarcinoma. PLoS One. 12:e39492008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Liu T, Willmore-Payne C, Layfield LJ and
Holden JA: Lack of BRAF activating mutations in prostate
adenocarcinoma: a study of 93 cases. Appl Immunohistochem Mol
Morphol. 2:121–125. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Riely GJ, Politi KA, Miller VA and Pao W:
Update on epidermal growth factor receptor mutations in non-small
cell lung cancer. Clin Cancer Res. 24:7232–7241. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Al-Kuraya K, Schraml P, Sheikh S, et al:
Predominance of high-grade pathway in breast cancer development of
Middle East women. Mod Pathol. 7:891–897. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Choi DH, Shin DB, Lee MH, et al: A
comparison of five immunohistochemical biomarkers and HER-2/neu
gene amplification by fluorescence in situ hybridization in white
and Korean patients with early-onset breast carcinoma. Cancer.
8:1587–1595. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Michaloglou C, Vredeveld LC, Mooi WJ and
Peeper DS: BRAF(E600) in benign and malignant human tumours.
Oncogene. 7:877–895. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Marchetti A, Felicioni L and Buttitta F:
Assessing EGFR mutations. N Engl J Med. 5:526–528. 2006.PubMed/NCBI
|