Introduction
Gastric cancer (GC) is the third most common cause
of cancer-related death worldwide (1), with approximately one million new
cases diagnosed each year (2). Even
though the incidence of GC has declined in most endemic countries,
and despite considerable therapeutic improvements in surgical
techniques, innovations in clinical diagnosis and the development
of new chemotherapy regimens, it still remains a global challenge,
since the prognosis for patients with GC is generally poor,
particularly in advanced stages of the disease (3).
Several lines of evidence indicate that immune cells
in the tumor microenvironment have an important role in regulating
tumor progression, which may determine the clinical parameters and
prognosis of GC (4). Therefore, a
better comprehension of the immune mechanisms that govern tumor
surveillance and tumor evasion strategies is essential to
investigate new therapeutic tools to treat this disease.
Among the innate immune effectors that participate
in the early control of transformed cells are the natural killer
cells (5), which directly lyse
tumor cells without prior sensitization (6). The recognition of target cells by NK
cells is mediated by activating receptors that detect
self-molecules induced in conditions of cellular stress (7). This is the case for NKG2D, a type II
C-type lectin-like transmembrane activating receptor expressed on
NK cells, some cytolytic CD8+ αβ T cells, γδ T cells and
NKT cells (8,9). Its functional outcome is the release
of granules containing perforin and granzyme, which consequently
triggers cell-mediated cytotoxicity (10). The target cell ligands recognized by
the NKG2D receptor are the MHC class I chain-related molecules A
and B (MICA and MICB) and UL16-binding proteins (ULBP) 1–6
(11), which are cell surface
glycoproteins expressed at low levels in most tissues, but
upregulated under cellular transformation (12). Since NK cells can efficiently
recognize and kill tumors bearing NKG2D ligands (NKG2DLs) (13), the presence of these molecules on
the cell surface potentially serves as 'danger signals' to alert
the innate immune system to the existence of transformed cells,
thus contributing to their elimination (14).
Nevertheless, several types of tumors have evolved
mechanisms to evade immune surveillance mediated by cytolytic
cells. Among these strategies, the shedding of NKG2DLs from the
surface of tumor cells results in the release of soluble MICA,
which dampens NK cell and CD8+ T lymphocyte cytotoxicity
due to downregulation of NKG2D receptor and leads to impairment of
NKG2D-dependent cell activation (15–17).
In addition, the expression of low levels of NKG2DLs on the cell
surface as a result of intracellular deposits of immature forms of
these ligands also prevents NK cell-mediated lysis and favors tumor
development (18).
On the contrary, tumors that secrete MICA still
express significant amounts of this NKG2DL on their cell surface
(19,20). Several reports have demonstrated
that sustained surface tumor expression of NKG2DLs can also elicit
NKG2D receptor downregulation (21). Therefore, chronic exposure of NK
cells to tumor-associated cell surface or soluble NKG2DLs may lead
to disease progression and poor prognosis in cancer as a result of
the impairment of NKG2D receptor-dependent activation, which
contributes to tumor escape (19,22,23).
In GC patients, systemic and local immune defects
have been demonstrated, which correlate with disease progression
and prognosis. For instance, tumor-infiltrating and systemic NK
cells, cytotoxic CD8+ T cells and γδ T cells in GC
patients express low levels of NKG2D receptor, resulting in
compromised cytotoxic activity and contributing to disease severity
(24–26). Serum levels of soluble MICA and MICB
in patients with GC are increased compared to healthy donors
(27). In addition, MICA and MICB
mRNA levels in the gastric tumor tissue are higher compared to
patient gastric mucosa (28).
Although MICA and MICB have been detected in gastric adenocarcinoma
tissue (29) and gastric mucosa of
healthy donors (30), both, tumor
and gastric mucosa-associated MICA and MICB expression in GC and
its clinical significance still remain to be established.
In the present study, we sought to determine tissue
expression of MICA and MICB in GC patients and examine the clinical
relevance of these NKG2DLs in this disease. The expression of MICA
and MICB in the primary tumor and the adjacent non-tumor gastric
mucosa from GC patients who received radical surgery was evaluated
by immunohistochemistry (IHC) and flow cytometry. MICA mRNA levels
were determined by real-time quantitative PCR (RT-qPCR).
Additionally, we evaluated the relationship between MICA and MICB
expression in the tumor and clinicopathological features of the
disease, including tumor size, differentiation, depth of invasion,
status of lymph node metastasis and TNM staging, as well as their
prognostic value to post-resection survival of GC patients.
Materials and methods
Patients and samples
During 2010 and 2012, a total of 29 patients (7
female, 22 male) aged 64±12 years (range, 41–90 years) treated at
the Department of Gastrointestinal Surgery, Hospital del Salvador
(Santiago, Chile), and pathologically diagnosed with gastric
adenocarcinoma, were enrolled in this study. None of the patients
received chemotherapy, radiotherapy, or other medical interventions
for GC treatment before surgery. Primary gastric tumor and their
matched adjacent nonmalignant gastric mucosa samples were collected
immediately after surgical resection of the stomach. Patient
characteristics and clinicopathological features of tumors
(Table I) were determined according
to the disease staging system of the American Joint Committee on
Cancer (AJCC) (7th Edition) (31).
Tumor size was given as the maximum tumor diameter measured on the
freshly resected stomach. Histopathological diagnosis was carried
out by the team of pathologists from Hospital del Salvador
(Santiago, Chile). The patient survival was assessed for 36 months
after potentially curative surgery or until death due to
tumor-specific disease. Written informed consent for tissue
donation was obtained from all the patients. This study was
approved by the Committee on Human Ethics Investigation of the
Faculty of Medicine, University of Chile, and the Committee on
Scientific Ethics of the Metropolitan Health Service of the Chilean
Government.
 | Table IClinicopathological characteristics
of gastric cancer patients. |
Table I
Clinicopathological characteristics
of gastric cancer patients.
| Variables | N (%) |
|---|
| Gender |
| Male | 22 (76) |
| Female | 7 (24) |
| Age at surgery
(years) |
| Mean (range) | 64 (41–90) |
| Tumor size
(cm) |
| ≤5 | 10 (34.5) |
| >5 | 19 (65.5) |
| Tumor
differentiation |
| High/medium | 12 (41.4) |
| Low/none | 17 (58.6) |
| Invasion
statusa |
| T1, T2 | 7 (24.1) |
| T3, T4 | 22 (75.9) |
| Lymph node
metastasis (N) |
| No (N0) | 8 (27.6) |
| Yes (N1,2,3) | 21 (72.4) |
| TNM stageb |
| I, II | 12 (41.4) |
| III, IV | 17 (58.6) |
Isolation of single cells from
dissociated gastric tissues
Fresh tumor and their matched mucosal tissue samples
from 23 GC patients were transported to the laboratory in Hank's
balanced salt solution (HBSS) medium (Gibco, Invitrogen, Waltham,
MA, USA) supplemented with 100 U/ml penicillin and 100 µg/ml
streptomycin (GE Healthcare Hyclone, Inc., South Logan, UT, USA).
Tissues were cut into small pieces using sterile scalpel blades and
minced in RPMI-1640 medium (GE Healthcare-HyClone Laboratories)
supplemented with penicillin/streptomycin and 3% fetal bovine serum
(FBS) with the help of syringe needles and plungers. To obtain
single-cell suspensions, the resultant dissociated tissues were
passed through 70-µm cell strainers (BD Biosciences, San
Jose, CA, USA) to remove tissue fragments. Cells were then
centrifuged at 2,000 rpm for 10 min at 4°C, and the pellet was
incubated with erythrocyte lysis buffer for 10 min at room
temperature (RT). Cells were washed with RPMI-supplemented medium,
centrifuged and counted. Cell viability was assessed by an
exclusion method using Trypan blue staining (Merck KGaA, Darmstadt,
Germany). Cell suspensions were then used for flow cytometric
analysis.
Flow cytometric analysis
Cells derived from the primary tumors and their
matched non-tumor gastric mucosa were resuspended with 1%
paraformaldehyde (PFA) in 1% FBS/phosphate-buffered saline (PBS)
and incubated on ice for 30 min. Cells were then transferred to
V-bottomed 96-well plates (Thermo Fisher Scientific, Waltham, MA,
USA) and centrifuged at 2,000 rpm for 3 min at 4°C. At least
2×105 cells were stained with purified mouse anti-human
MICA or MICB monoclonal antibodies (both from R&D Systems,
Inc., Minneapolis, MN, USA) (1:25 dilution in 1% FBS/PBS). Purified
mouse IgG2b (Santa Cruz Biotechnology, Inc., Santa Cruz, CA, USA)
was used as the isotype control to exclude non-specific
fluorescence. Cells were then incubated overnight at 4°C. After
three washes with 1% FBS/PBS, a secondary fluorescein
isothiocyanate (FITC)-conjugated goat anti-mouse antibody (KPL,
Inc., Gaithersburg, MD, USA) was added (1:50 dilution in 1%
FBS/PBS), and cells were incubated for 30 min at 4°C. Further
washing steps were carried out, and cells were finally fixed in 2%
PFA before flow cytometric analysis. An average of 20,000 events
was collected per sample. MICA and MICB staining was detected as
median fluorescence intensity (MFI). Flow cytometry was performed
using a FACSCalibur flow cytometer, acquired with the CellQuest
program (both from BD Biosciences), and analyzed using FlowJo
vX.0.7 software (Tree Star, Inc., Ashland, OR, USA).
IHC
Formalin-fixed, paraffin-embedded tumor samples from
13 GC patients enrolled in this study were obtained from the
Department of Pathology from Hospital del Salvador (Santiago,
Chile). In 7 paired cases, non-neoplastic gastric mucosa was
available for comparative analysis. Only specimens fixed and
included in optimal conditions for quantitative immunohistochemical
studies were selected. Serial sections (4 µm thick) of
tissue samples were plated on silanized glass slides,
deparaffinized and rehydrated. Antigen retrieval was performed by
heating the tissue sections in a steam bath at 90–95°C for 30 min
in 10 mM citrate buffer (pH 6.0). The slides were rinsed in cool
running water and immersed in 3% hydrogen peroxide for 10 min at RT
to block the endogenous peroxidase activity. To reduce non-specific
binding, slides were incubated with 2% bovine serum albumin (BSA)
in PBS for 10 min at RT. The sections were then incubated with
mouse anti-human MICA/B polyclonal antibody generated as previously
described (32,33) (1:50 dilution in 2% BSA/PBS) for 1 h
at 37°C in a humid chamber. The specificity of the reaction was
tested by omission of the primary antibody. Slides were further
incubated with a secondary antibody, a biotinylated goat anti-mouse
IgG (Sigma-Aldrich, St. Louis, MO, USA) (1:200 dilution in 2%
BSA/PBS), for 30 min at RT. Next, sections were incubated with
streptavidin-horseradish peroxidase (HRP)-conjugate (Dako/Agilent
Technologies, Glostrup, Denmark) in 2% BSA/PBS for 20 min at RT. As
a peroxidase substrate, liquid 3,3-diaminobenzidine
tetrahydrochloride (DAB Chromogen; Dako/Agilent Technologies) was
used. Each step was followed by extensive slide washes with PBS (pH
7.4). The sections were then counterstained with hematoxylin,
dehydrated in ethanol, cleared in xylene, coverslipped and
evaluated in a Leica DM2500 microscope. Photographs were digitally
processed using a Leica Application Suite V3.6.0 (Leica
Microsystems, Wetzlar, German). Peroxidase staining intensity was
assessed in 10 randomly-selected microscopic fields per tissue
section, and the immune-reactive areas were quantified in
pixels/µm2 using ImageJ software (National
Institutes of Health, Bethesda, MD, USA). Coloring cytoplasm and
membrane of cells present in the tumor and mucosal tissues was
considered as positive reaction for MICA/B.
Quantitative real-time PCR (qRT-PCR)
qRT-PCR was performed to determine the mRNA level of
MICA. After stomach surgical resection, the fresh tissue samples
were immediately immersed in RNAlater RNA stabilization reagent
(Qiagen, KJ Venlo, The Netherlands) and stored at −20°C until RNA
extraction. Total RNA was extracted from 9 pairs of matched gastric
tumor and adjacent non-tumor gastric mucosa of GC patients using
E.Z.N.A® Total RNA kit I (Omega Bio-Tek, Inc., Norcross,
GA, USA), according to the manufacturer's instructions. After
treatment with DNase I (Thermo Fisher Scientific), total RNA
concentration and purity were assessed using the Synergy HT
Multi-detection microplate reader (Bio-Tek Instruments, Inc.,
Winooski, VT, USA). cDNA synthesis was carried out using the
Affinity Script Multi-Temp RT & RT-PCR kit (Agilent
Technologies, Inc., Santa Clara, CA, USA), using 2 µg of
total RNA as the template. The resulting cDNA was amplified by
qRT-PCR using the Stratagene Mx3000P QPCR System (Agilent
Technologies), which measures the binding of SYBR® Green
(Brilliant III Ultra-Fast SYBR-Green QPCR Master Mix; Agilent
Technologies) to the double stranded DNA. The housekeeping gene
HPRT was used as an internal control. Gene-specific primers were
designed using the Amplifx 1.7 software (University of Marseille,
Marseille, France). Primers for MICA were 5′-GAGACTTGACAGGG
AACGGAAA-3′ (sense) and 5′-GAAGACAACAGCACC AGGAG-3′ (antisense).
Primers for HPRT were CAAGCTTGCTGGTGAAAAGGAC (sense) and
GTCAAGGGCATATCCTACAACAAA (antisense). PCR reactions were performed
in triplicate in a final volume of 20 µl as follows: 95°C
for 5 min, followed by 40 cycles of 95°C for 5 sec and 60°C for 20
sec. Regression curves were calculated for each sample, and the
threshold cycles were obtained using the instrument's software
(MxPro QPCR software; Agilent Technologies) and calculated using
the 2−ΔΔCT method, were determined relative to the mean
values of each gastric mucosa sample.
Statistical analysis
Data were expressed as mean ± standard error of the
mean (SEM) for each group. Normal distribution was tested by
Kolmogorov-Smirnov test. Normally distributed data were analyzed
using Student's t-tests, while non-parametric data were evaluated
using Wilcoxon or Mann-Whitney U tests to compare results between
groups. For survival analysis, groups of patients were
distinguished according to positive or negative MICA and MICB
expression on tumor tissue (observed by flow cytometry). Survival
rates, which were defined as the period from surgery until
GC-related death or survival for 36 months after surgery, were
analyzed by the Kaplan-Meier method, and the log-rank test was
performed to assess survival differences. Data were evaluated with
GraphPad Prism v6.01 software (GraphPad Software, Inc., La Jolla,
CA, USA). All statistical tests were two-tailed, and P-values
<0.05 were considered statistically significant.
Results
MICA and MICB are expressed on gastric
tumor and mucosal tissues of GC patients
NKG2DLs are frequently expressed by tumor cells, and
their presence on the surface of target cells may determine the NK
cell-mediated immune response against the tumor (12). The levels of MICA mRNA in 9 pairs of
gastric tumor and adjacent non-tumor gastric mucosa from GC
patients were estimated by qRT-PCR. The MICA levels were
significantly increased in the tumor tissue as compared with the
gastric mucosa (P=0.039) (Fig. 1),
in accordance with results previously described by others using
Multiplex RT-PCR (28).
Nevertheless, since the levels of mRNA do not
usually predict its protein abundance (34), we decided to perform
immunohistochemical staining of MICA/B in paraffin-embedded gastric
tumor and mucosal tissue sections of histopathologically confirmed
gastric adenocarcinoma. Representative photomicrographs are shown
in Fig. 2A. The analysis of 13
gastric tumors and 7 non-neoplasic gastric mucosa from GC patients
showed that MICA/B immunoreactivity in the tumor tissue was
significantly higher than in the gastric mucosa (P=0.0009)
(Fig. 2B).
MICA/B expression associates with
clinicopathological characteristics of gastric adenocarcinoma
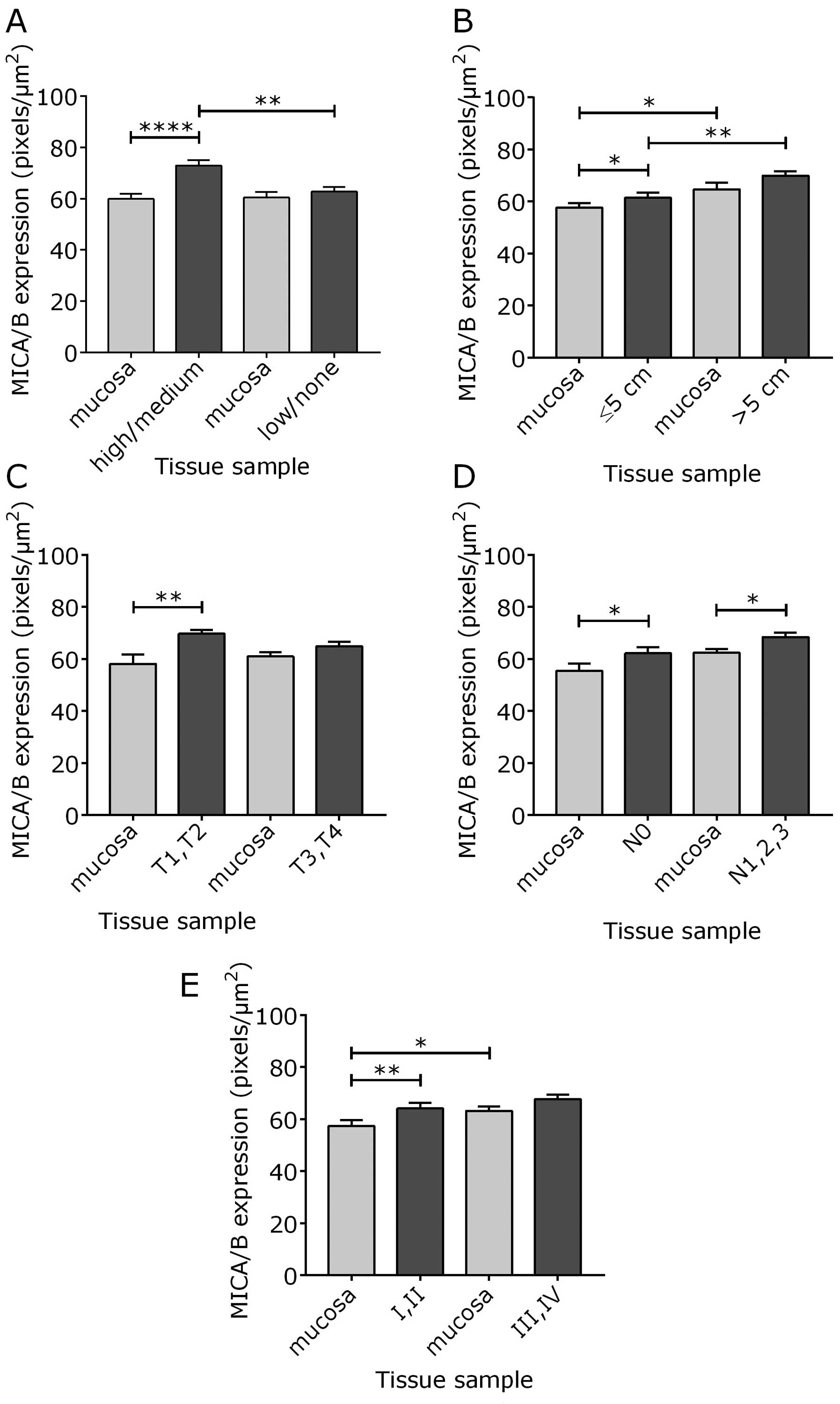
We further asked whether our immunohistochemical
analysis of MICA/B expression in human GC presented an association
with clinicopathological parameters of the disease. MICA/B
expression in the tumor was found to be significantly increased
when compared to the gastric mucosa in patients with well
differentiated tumors (P<0.0001) (Fig. 3A), in tumors of small size (≤5 cm)
(P=0.0359) (Fig. 3B), tumors with
lower invasion status (T1 and T2) (P=0.0015) (Fig. 3C), tumors with no lymphatic invasion
(N0) (P=0.0269) (Fig. 3D), and
tumors at TNM stages I and II (P=0.0056) (Fig. 3E). However, MICA/B immunoreactivity
in the tumor did not differ significantly from that of the
corresponding gastric mucosa in patients diagnosed with poorly or
non-differentiated tumors (Fig.
3A), with tumors >5 cm (Fig.
3B), tumors with deeper invasion status (T3 and T4) (Fig. 3C), and tumors at TNM stages III and
IV (Fig. 3E), although patients
presenting with lymph node metastasis (N1, N2 and N3) showed higher
MICA/B expression in the tumor than in the gastric mucosa
(P=0.0115) (Fig. 3D). Notably,
while well differentiated tumors displayed higher MICA/B expression
than non-differentiated tumors (P=0.0049) (Fig. 3A), tumors ≤5 cm showed significantly
lower MICA/B immunoreactivity than tumors >5 cm (P=0.0024)
(Fig. 3B). Accordingly, the
non-neoplasic gastric mucosa of tumors ≤5 cm presented decreased
MICA/B expression compared to the gastric mucosa of tumors >5 cm
(P=0.0205) (Fig. 3B), which was
also observed in tumors at stages I and II of the disease
(P=0.0477) (Fig. 3E).
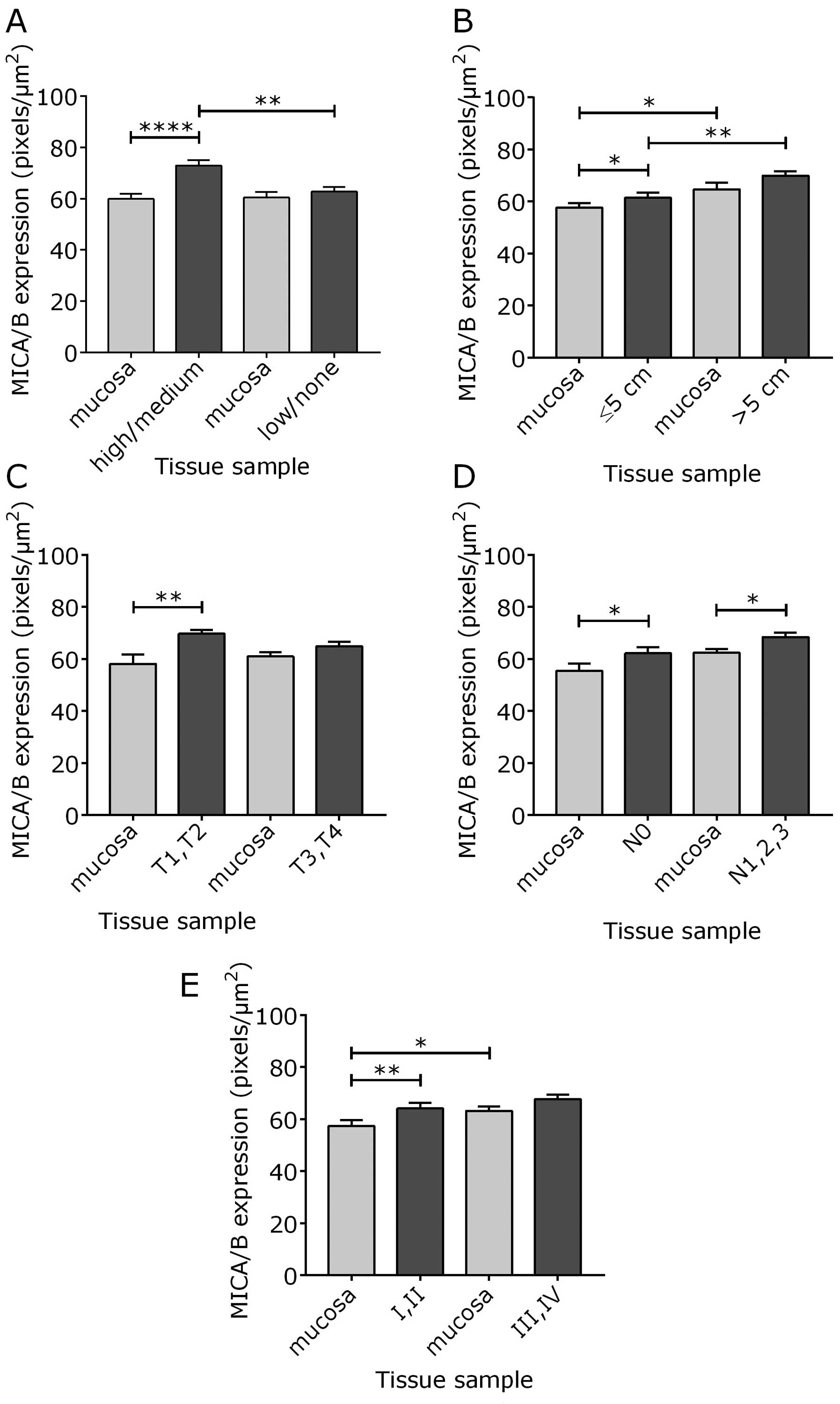 | Figure 3MICA/B expression in gastric
adenocarcinoma associates with clinicopathological parameters of
the disease. Quantification, in pixels/µm2, of
IHC staining of 13 tumors and 7 non-neoplasic gastric mucosal
samples of GC patients. Tumor tissue and mucosa were classified
according to disease parameters: (A) tumor differentiation
(high/medium and low/none), (B) tumor size (≤5 and >5 cm), (C)
invasion status (T1,T2 and T3,T4), (D) lymph node metastasis (N0
and N1,2,3), and (E) TNM stage (I,II and III,IV). Mean values ± SEM
are shown. The Mann-Whitney U test or unpaired t-test was used for
statistical analysis. *P<0.05;
**P<0.01; ****P<0.0001. |
Next, we performed flow cytometry to evaluate MICA
expression on cells derived from 23 pairs of gastric tumor and
mucosa of GC patients. MICB expression was also analyzed on 20
pairs of tumor and mucosal tissues. Contour plots of freshly
isolated gastric tumor and mucosal cells of a representative
patient are shown in Fig. 4A.
Expression intensity of MICA and MICB, shown in the corresponding
histograms, was assessed on the selected contour plot gates and
compared to the isotype control (Fig.
4A). The median fluorescence intensity (MFI) values of MICA and
MICB present in the tumor and mucosa, for all patients analyzed,
are shown in Fig. 4B and C,
respectively. MFI values >10 were established as positive ligand
expression. MICA expression was observed in 57% of tumors (13 out
of 23 samples) (Fig. 4B), while
MICB was detected in 50% of tumors (10 out of 20 samples) (Fig. 4C). Although the presence of MICA and
MICB was observed in 10 (44%) and 9 (45%) non-neoplasic gastric
mucosal samples, respectively, paired tissue analysis showed no
significant difference between tumor and gastric mucosa expression
of either ligand (Fig. 4B and
C).
We then evaluated whether gastric tumor and mucosa
expression of MICA and MICB, observed by flow cytometry, associates
with clinicopathological features of the disease. We found that, as
observed by IHC (Fig. 3B), tumors
≤5 cm presented lower expression of MICA (P=0.0045) and MICB
(P=0.0461) than tumors >5 cm (Fig.
5A and B). Although MICA and MICB expression in the gastric
mucosa of tumors >5 cm did not differ significantly from that of
the mucosa of tumors ≤5 cm, no difference in the expression of
either ligand was observed between the tumor and gastric mucosa
when tumors were ≤5 or >5 cm (Fig.
5).
GC patients presenting large tumors that
express MICA and MICB show lower overall survival rate
It has been reported that tumor size is an
independent prognostic indicator in GC patients, and that patients
bearing tumors >5 cm present more aggressive clinicopathological
characteristics than patients with tumors ≤5 cm (35). The 3-year overall survival rate in
our cohort, after gastrectomy, was 30.4%, with a median survival of
12.6 months (range, 2–36 months). We observed no statistically
significant difference in the survival rate between patients with
tumors ≤5 cm and tumors >5 cm (data not shown). Nevertheless, in
patients presenting tumors ≤5 cm, the 3-year survival rate when
tumors expressed MICA and MICB was 100%, whereas in patients whose
small tumors did not express MICA and MICB, the survival rate was
17% (P=0.0404) (Fig. 6A). On the
contrary, all the patients with tumors >5 cm that expressed MICA
and MICB succumbed within 16.4 months after gastrectomy, while in
patients whose large tumors did not express MICA and MICB, the
3-year survival rate reached 50% (P=0.0157) (Fig. 6B). These results suggest that
tumor-associated expression of MICA and MICB may not guarantee a
survival benefit for GC patients with tumors >5 cm.
Discussion
NK cells participate in the immune surveillance of
several types of tumors, including gastrointestinal malignancies
(29,36). Nevertheless, in GC patients, the
downregulation of NKG2D receptor on tumor-infiltrating and systemic
NK cells, cytotoxic CD8+ T cells and γδ T lymphocytes
has been associated with impaired function of these cells and also
with tumor progression and poor disease prognosis (24–26).
Low surface expression of NKG2D receptor has been attributed to the
effects of soluble NKG2DLs that are shed from solid tumors by
metalloproteinases, compromising the NKG2D-dependent NK cell
activation and favoring tumor escape (19,37).
Indeed, we have detected higher levels of soluble MICA and MICB in
the serum of GC patients compared with healthy individuals (data
not shown), as previously described by others (27). Conversely, persistent cell surface
expression of NKG2DLs by tumors and other cells can also elicit
NKG2D receptor downregulation, promoting an impairment of NK and
CD8+ T cell cytotoxicity (21). Tumor-associated or soluble NKG2DLs
have been related with disease progression and poor prognosis in
several types of cancer, such as pancreatic and prostate cancer
(MICA/B) (15,22), ovarian cancer (ULBP2 and ULBP4)
(38), melanoma (ULBP2) (39) and multiple myeloma (MICA) (40). In GC patients, MICA and MICB mRNA
levels have been described in the tumor and non-neoplasic gastric
mucosal tissue (28). Accordingly,
MICA/B has been detected, at the protein level, in the primary
tumor of these patients (29).
However, to date, the levels of MICA and MICB expression in both
gastric tumor and mucosal tissues of GC patients have not been
addressed.
In the present study, we evaluated the presence of
MICA and MICB in the tumor tissue and gastric mucosa obtained from
GC patients who underwent potentially curative surgery to treat the
disease. We observed that MICA mRNA levels, estimated by qRT-PCR,
were detected in both, gastric tumor and mucosal tissues, and that
MICA mRNA levels are higher in the tumor as compared with the
gastric mucosa. These results are in agreement with Park et
al (28), who reported, using
Multiplex PCR, that the mRNA levels of MICA and other NKG2DLs
(MICB, ULBP-2 and ULBP-3) are significantly increased in the
primary tumor of GC patients compared to the adjacent non-neoplasic
gastric mucosa.
Here, we also observed that MICA and MICB are
expressed in 57 and 50% of tumors, respectively. Conversely, 44 and
45% of patients presented MICA and MICB, respectively, in their
non-neoplasic gastric mucosa, as evidenced by flow cytometry. Our
IHC data showed that the immunoreactivity for MICA/B in the tumor
was increased in relation to the gastric mucosa, although we did
not detect such significant differential tumor and mucosal tissue
expression of MICA and MICB by flow cytometry. The use of different
antibodies and techniques to detect these NKG2DLs in gastric
tissues might have contributed to this result. Nevertheless, we can
conclude that MICA and MICB are expressed in both, the primary
tumor and gastric mucosa of patients with gastric cancer.
The prognostic value of MICA/B expression in gastric
adenocarcinoma has been studied. A recent report by Mimura et
al (29) demonstrated, using a
large cohort of GC patients, that 40% of these patients express
MICA/B in the tumor, which correlated with clinicopathological
parameters that characterized early disease stages and better
overall survival. These authors also observed that most patients at
advanced stages of GC do not express MICA/B (29). In this study, we related MICA/B
expression, by IHC, in both, gastric tumor and mucosal tissues, to
clinicopathological characteristics of the disease. MICA/B
expression in the tumor was significantly increased compared to the
gastric mucosa in patients with well differentiated tumors, in
tumors of small size (≤5 cm), tumors with lower invasion status (T1
and T2), tumors with no lymphatic invasion (N0), and tumors at
early TNM stages (I and II). In contrast, MICA/B expression in the
tumor was similar to the gastric mucosa in patients with poorly or
non-differentiated tumors, with tumors >5 cm, tumors with deeper
invasion status (T3 and T4), and tumors at advanced TNM stages (III
and IV), although GC patients presenting with lymph node metastasis
(N1, N2 and N3) showed higher MICA/B expression in the tumor than
in the gastric mucosa. Notably, the non-neoplasic gastric mucosa of
patients bearing large tumors and tumors at stages III and IV
presented higher levels of MICA/B than the gastric mucosa of small
tumors and tumors at earlier disease stages, respectively.
Altogether, these results suggest that both, the equivalent
expression of MICA/B in the tumor and non-neoplasic gastric mucosa
and the increased expression of MICA/B in the gastric mucosa of GC
patients presenting advanced features of the disease reflects a
persistent cell-associated expression of these NKG2DLs. Whether
patient tumor and gastric mucosal expression of MICA/B favors NKG2D
receptor downregulation in cytotoxic lymphocytes at advanced stages
of GC needs further investigation.
In the present study, we also observed that, by IHC,
well differentiated tumors presented higher levels of MICA/B than
non-differentiated tumors. These results are in agreement with
Mimura et al (29), who
demonstrated that MICA/B-positive tumors were more prevalent in
patients presenting well-differentiated tumors. It has been well
established that the prognosis of patients with GC is determined by
tumor extension and lymph node involvement (41,42).
Although tumor differentiation may influence patient survival
(43), its value as an independent
prognostic indicator in GC is still controversial (44). On the contrary, several reports have
identified gastric tumor size as an independent prognostic factor
in gastric cancer. For instance, Zu et al (35), in a study using a large cohort of
patients and adopting a 5-cm cut-off value for tumor size, clearly
demonstrated that GC patients bearing tumors >5 cm presented
more aggressive clinicopathological characteristics than patients
with tumors ≤5 cm, which was also correlated to worse patient
survival, regardless of tumor stage and lymph node metastasis,
supporting that tumor size may be considered an independent
prognostic indicator in patients with gastric cancer.
By IHC, we demonstrated that tumors ≤5 cm had
significantly lower MICA/B expression than tumors >5 cm, which
was confirmed by flow cytometry. Even though the overall survival
rate between GC patients with tumors ≤5 cm and tumors >5 cm did
not differ in our cohort, the 3-year survival percentage of
patients whose tumors were ≤5 cm and that presented both, MICA and
MICB, was significantly higher than in patients with small tumors
that did not express these NKG2DLs. In contrast, GC patients with
tumors >5 cm that expressed MICA and MICB had significant lower
survival rates than patients presenting large tumors that did not
express either of the ligands. Therefore, these results indicate
that tumor-associated expression of MICA and MICB may be protective
for patients bearing tumors of small size, while MICA and MICB
expression in large tumors may contribute to tumor progression.
The association between MICA/B expression and tumor
stage has been previously studied for other types of cancer. In
colorectal and pancreatic cancers, MICA was detected as an
independent marker of favorable prognosis for stages I and II, but
not later stages of the disease (15,45).
These data, along with those obtained by Mimura et al
(29) for GC, suggest a protective
role for NKG2DL expression at early, but not advanced stages of
tumors. Accordingly, here we provide evidence that MICA/B
expression in small gastric tumors, which has been associated with
better patient survival (35), may
contribute to a better prognosis of the disease, but that
persistent expression of MICA/B in large tumors may not be
beneficial for GC patients.
It is intriguing that the high expression of a
molecule involved in the alertness of the immune response may
conversely be associated with a tumor immune evasion strategy. It
is well established that cell transformation results in increased
NKG2DL expression in relation to their basal levels, thus
converting these cells in a specific target for NK cell-mediated
cytotoxicity, which may determine their elimination (8,9).
However, high MICA and MICB expression in the primary tumor tissue
may provide a selective advantage for tumor cells that sustain MICA
and MICB expression and, instead of immune activation, this
prevalent expression would promote immune suppression, since
persistent NKG2DL expression may desensitize NK cells and render
them dysfunctional, which is a determinant of tumor aggressiveness
(21,46,47).
However, it is worth mentioning that other factors, such as soluble
NKG2DLs (19) and TGF-β released
from tumors (48), may more
strongly impair NK cell and other lymphocytes cytotoxicity,
compromising their function and favoring malignant progression.
It is becoming clear that the delineation of
alternative pathways for antagonizing the deleterious effects of
NKG2DL overexpression in cancer patients remains an important issue
for further investigation. Defining the contributory role of
persistent NKG2D receptor ligands on tumor progression could help
the development of novel treatment strategies or improve the
efficacy of standard therapy for GC. Our findings suggest that
MICA/B expression within large tumors can serve as a prognostic
indicator for GC and a potential target for immunotherapy.
Acknowledgments
This project was financially supported by grants
from the following Chilean Research Foundations: FONDECYT (grants
3100151 and 11110456 to C.H.R., 1130330 to M.C.M., and 1151214 to
H.R.C.), FONDEF (CAl2i10023 to M.C.M.), and ENLACE (ENL2010/2012 to
M.C.M.). We would like to thank Ms. Juana Orellana, Ms. Ruth Mora,
Ms. Graciela Caroca and Mr. Álvaro Rojas for their invaluable
expert technical assistance. We are also grateful to Dr Juan
Justiniano, Dr Jorge Bravo, Dr Claudio Heine, Dr Angela Castillo,
Dr Loreto Tapia, Dr Pablo Villegas, Ms. Paula Pino, Ms. Patricia
Acevedo, Ms. Yanet Vergara, Ms. Erika Abello, and members of the
Hospital del Salvador, Santiago, Chile, for providing assistance
with patients' tissue samples and clinical information. We also
thank Dr Arturo Ferreira, Dr Norberto Zwirner, Dr Mercedes López
and Dr Flávio Salazar-Onfray for their critical review of the
manuscript, as well as Dr Bárbara Pesce and Dr Leandro Carreño for
their helpful assistance on flow cytometry data analysis.
References
|
1
|
International Agency for Research on
Cancer and World Health Organization: World Cancer Report 2014.
Stewart BW and Wild C: IARC Press; Lyon: 2014
|
|
2
|
Torre LA, Bray F, Siegel RL, Ferlay J,
Lortet-Tieulent J and Jemal A: Global cancer statistics, 2012. CA
Cancer J Clin. 65:87–108. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Arkenau HT: Gastric cancer in the era of
molecularly targeted agents: Current drug development strategies. J
Cancer Res Clin Oncol. 135:855–866. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ogino S, Galon J, Fuchs CS and Dranoff G:
Cancer immunology–analysis of host and tumor factors for
personalized medicine. Nat Rev Clin Oncol. 8:711–719. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Trinchieri G: Natural killer cells wear
different hats: Effector cells of innate resistance and regulatory
cells of adaptive immunity and of hematopoiesis. Semin Immunol.
7:83–88. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Gasser S and Raulet DH: Activation and
self-tolerance of natural killer cells. Immunol Rev. 214:130–142.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Anfossi N, André P, Guia S, Falk CS,
Roetynck S, Stewart CA, Breso V, Frassati C, Reviron D, Middleton
D, et al: Human NK cell education by inhibitory receptors for MHC
class I. Immunity. 25:331–342. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Raulet DH and Guerra N: Oncogenic stress
sensed by the immune system: Role of natural killer cell receptors.
Nat Rev Immunol. 9:568–580. 2009. View
Article : Google Scholar : PubMed/NCBI
|
|
9
|
Nausch N and Cerwenka A: NKG2D ligands in
tumor immunity. Oncogene. 27:5944–5958. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Burgess SJ, Maasho K, Masilamani M,
Narayanan S, Borrego F and Coligan JE: The NKG2D receptor:
Immunobiology and clinical implications. Immunol Res. 40:18–34.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Champsaur M and Lanier LL: Effect of NKG2D
ligand expression on host immune responses. Immunol Rev.
235:267–285. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Fernandez NC, Treiner E, Vance RE,
Jamieson AM, Lemieux S and Raulet DH: A subset of natural killer
cells achieves self-tolerance without expressing inhibitory
receptors specific for self-MHC molecules. Blood. 105:4416–4423.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ogasawara K and Lanier LL: NKG2D in NK and
T cell-mediated immunity. J Clin Immunol. 25:534–540. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Diefenbach A, Jamieson AM, Liu SD, Shastri
N and Raulet DH: Ligands for the murine NKG2D receptor: Expression
by tumor cells and activation of NK cells and macrophages. Nat
Immunol. 1:119–126. 2000. View
Article : Google Scholar
|
|
15
|
Duan X, Deng L, Chen X, Lu Y, Zhang Q,
Zhang K, Hu Y, Zeng J and Sun W: Clinical significance of the
immunostimulatory MHC class I chain-related molecule A and NKG2D
receptor on NK cells in pancreatic cancer. Med Oncol. 28:466–474.
2011. View Article : Google Scholar
|
|
16
|
Kohga K, Takehara T, Tatsumi T, Miyagi T,
Ishida H, Ohkawa K, Kanto T, Hiramatsu N and Hayashi N: Anticancer
chemotherapy inhibits MHC class I-related chain a ectodomain
shedding by downregulating ADAM10 expression in hepatocellular
carcinoma. Cancer Res. 69:8050–8057. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Tamaki S, Sanefuzi N, Kawakami M, Aoki K,
Imai Y, Yamanaka Y, Yamamoto K, Ishitani A, Hatake K and Kirita T:
Association between soluble MICA levels and disease stage IV oral
squamous cell carcinoma in Japanese patients. Hum Immunol.
69:88–93. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Fuertes MB, Girart MV, Molinero LL,
Domaica CI, Rossi LE, Barrio MM, Mordoh J, Rabinovich GA and
Zwirner NW: Intracellular retention of the NKG2D ligand MHC class I
chain-related gene A in human melanomas confers immune privilege
and prevents NK cell-mediated cytotoxicity. J Immunol.
180:4606–4614. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Groh V, Wu J, Yee C and Spies T:
Tumour-derived soluble MIC ligands impair expression of NKG2D and
T-cell activation. Nature. 419:734–738. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Salih HR, Rammensee HG and Steinle A:
Cutting edge: Down-regulation of MICA on human tumors by
proteolytic shedding. J Immunol. 169:4098–4102. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Oppenheim DE, Roberts SJ, Clarke SL,
Filler R, Lewis JM, Tigelaar RE, Girardi M and Hayday AC: Sustained
localized expression of ligand for the activating NKG2D receptor
impairs natural cytotoxicity in vivo and reduces tumor
immunosurveillance. Nat Immunol. 6:928–937. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Wu JD, Higgins LM, Steinle A, Cosman D,
Haugk K and Plymate SR: Prevalent expression of the
immunostimulatory MHC class I chain-related molecule is
counteracted by shedding in prostate cancer. J Clin Invest.
114:560–568. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
McGilvray RW, Eagle RA, Rolland P,
Jafferji I, Trowsdale J and Durrant LG: ULBP2 and RAET1E NKG2D
ligands are independent predictors of poor prognosis in ovarian
cancer patients. Int J Cancer. 127:1412–1420. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Osaki T, Saito H, Yoshikawa T, Matsumoto
S, Tatebe S, Tsujitani S and Ikeguchi M: Decreased NKG2D expression
on CD8+ T cell is involved in immune evasion in patients
with gastric cancer. Clin Cancer Res. 13:382–387. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Saito H, Osaki T and Ikeguchi M: Decreased
NKG2D expression on NK cells correlates with impaired NK cell
function in patients with gastric cancer. Gastric Cancer. 15:27–33.
2012. View Article : Google Scholar
|
|
26
|
Kuroda H, Saito H and Ikeguchi M:
Decreased number and reduced NKG2D expression of Vdelta1 gammadelta
T cells are involved in the impaired function of Vdelta1 gammadelta
T cells in the tissue of gastric cancer. Gastric Cancer.
15:433–439. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Zhao S, Wang H, Nie Y, Mi Q, Chen X and
Hou Y: Midkine upregulates MICA/B expression in human gastric
cancer cells and decreases natural killer cell cytotoxicity. Cancer
Immunol Immunother. 61:1745–1753. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Park SW, Bae JH, Kim SD, Son YO, Kim JY,
Park HJ, Lee CH, Park DY, Kim JY, Lee MK, et al: Comparison of
level of NKG2D ligands between normal and tumor tissue using
multiplex RT-PCR. Cancer Invest. 25:299–307. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Mimura K, Kamiya T, Shiraishi K, Kua LF,
Shabbir A, So J, Yong WP, Suzuki Y, Yoshimoto Y, Nakano T, et al:
Therapeutic potential of highly cytotoxic natural killer cells for
gastric cancer. Int J Cancer. 135:1390–1398. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Groh V, Bahram S, Bauer S, Herman A,
Beauchamp M and Spies T: Cell stress-regulated human major
histocompatibility complex class I gene expressed in
gastrointestinal epithelium. Proc Natl Acad Sci USA.
93:12445–12450. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Washington K: 7th edition of the AJCC
cancer staging manual: stomach. Ann Surg Oncol. 17:3077–3079. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Bethke J, Rojas V, Berendsen J, Cárdenas
C, Guzmán F, Gallardo JA and Mercado L: Development of a new
antibody for detecting natural killer enhancing factor (NKEF)-like
protein in infected salmonids. J Fish Dis. 35:379–388. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Santana PA, Álvarez CA, Guzmán F and
Mercado L: Development of a sandwich ELISA for quantifying hepcidin
in Rainbow trout. Fish Shellfish Immunol. 35:748–755. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Vogel C and Marcotte EM: Insights into the
regulation of protein abundance from proteomic and transcriptomic
analyses. Nat Rev Genet. 13:227–232. 2012.PubMed/NCBI
|
|
35
|
Zu H, Wang F, Ma Y and Xue Y:
Stage-stratified analysis of prognostic significance of tumor size
in patients with gastric cancer. PLoS One. 8:e545022013. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Waldhauer I and Steinle A: NK cells and
cancer immunosurveillance. Oncogene. 27:5932–5943. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Raulet DH: Missing self recognition and
self tolerance of natural killer (NK) cells. Semin Immunol.
18:145–150. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Li K, Mandai M, Hamanishi J, Matsumura N,
Suzuki A, Yagi H, Yamaguchi K, Baba T, Fujii S and Konishi I:
Clinical significance of the NKG2D ligands, MICA/B and ULBP2 in
ovarian cancer: High expression of ULBP2 is an indicator of poor
prognosis. Cancer Immunol Immunother. 58:641–652. 2009. View Article : Google Scholar
|
|
39
|
Paschen A1, Sucker A, Hill B, Moll I,
Zapatka M, Nguyen XD, Sim GC, Gutmann I, Hassel J, Becker JC, et
al: Differential clinical significance of individual NKG2D ligands
in melanoma: soluble ULBP2 as an indicator of poor prognosis
superior to S100B. Clin Cancer Res. 15:5208–5215. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Rebmann V, Schütt P, Brandhorst D, Opalka
B, Moritz T, Nowrousian MR and Grosse-Wilde H: Soluble MICA as an
independent prognostic factor for the overall survival and
progression-free survival of multiple myeloma patients. Clin
Immunol. 123:114–120. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Nakamura K, Ueyama T, Yao T, Xuan ZX, Ambe
K, Adachi Y, Yakeishi Y, Matsukuma A and Enjoji M: Pathology and
prognosis of gastric carcinoma. Findings in 10,000 patients who
underwent primary gastrectomy. Cancer. 70:1030–1037. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Siewert JR, Böttcher K, Stein HJ and Roder
JD: Relevant prognostic factors in gastric cancer: Ten-year results
of the German Gastric Cancer Study. Ann Surg. 228:449–461. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Adachi Y, Yasuda K, Inomata M, Sato K,
Shiraishi N and Kitano S: Pathology and prognosis of gastric
carcinoma: Well versus poorly differentiated type. Cancer.
89:1418–1424. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Dicken BJ, Bigam DL, Cass C, Mackey JR,
Joy AA and Hamilton SM: Gastric adenocarcinoma: Review and
considerations for future directions. Ann Surg. 241:27–39.
2005.
|
|
45
|
McGilvray RW, Eagle RA, Watson NF,
Al-Attar A, Ball G, Jafferji I, Trowsdale J and Durrant LG: NKG2D
ligand expression in human colorectal cancer reveals associations
with prognosis and evidence for immunoediting. Clin Cancer Res.
15:6993–7002. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Wang C, Zhou XJ, Li YY, Wan J, Yang LY and
Li GH: Effect of vasoactive intestinal peptide (VIP) on NKG2D
signal pathway and its contribution to immune escape of MKN45
cells. Sci World J. 2013:4295452013.
|
|
47
|
El-Gazzar A, Groh V and Spies T:
Immunobiology and conflicting roles of the human NKG2D lymphocyte
receptor and its ligands in cancer. J Immunol. 191:1509–1515. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Lee JC, Lee KM, Kim DW and Heo DS:
Elevated TGF-beta1 secretion and down-modulation of NKG2D underlies
impaired NK cytotoxicity in cancer patients. J Immunol.
172:7335–7340. 2004. View Article : Google Scholar : PubMed/NCBI
|