Worldwide, colorectal cancer (CRC) has become the
third-most common type of malignancy and fourth-most frequent cause
of cancer-related mortality. The CRC metastasis rate has increased
steadily to 20–25% (1–4), and 70–80% of these cases occur in the
liver (5). Almost half of all
patients who undergo resection for primary CRC will eventually
develop metachronous liver metastases (6), the leading cause of death in this
population with a median overall survival (OS) duration of 6–12
months if left untreated (7).
Surgical resection is the mainstay of treatment for colorectal
liver metastasis (CRCLM); however, liver metastases are deemed
resectable in only 10–20% of cases (8) with disappointing results and high
recurrence rate. One multi-center study of 1669 patients found that
more than half developed recurrences, with median disease-free
survival duration of 16.3 months (9).
Therefore, various alternative options for CRCLM
management have been extensively studied. However, definition
debates add serious strain in designing management plan.
Particularly in resection for cure was very low in synchronous
compared to metachronous, however, new chemotherapy agent has a
role to improve resection rate up to 30–40% (5). Definition of synchronous metastases is
still debated, although it has been highly suspected in those
detected up to 3 (10), 4 (11), or 6 months (12,13)
after the primary diagnosis.
Noteworthy, multidisciplinary team decision-making
and evolving chemotherapy agents and patient care are contributed
to improve 5-year OS rates from <8% to 25–40% (14,15).
Neoadjuvant treatment, which is used for local tumor amelioration,
has a high response rate (>50%) and can increase the rate of
resectability from 10 to 30% (16,17),
although the recurrence rate still remains high, with OS not
exceeding 3 years (18). Therefore,
alternative treatment strategies are essential. We reviewed current
data and analyzed existing treatment modalities. We hope this
review will generate prospective insights into ongoing
controversies regarding the management of liver metastases of
CRC.
Generally, liver metastasis cas manifest in both
synchronous or metachronous forms. These presentations raise
questions regarding the ability to resect the primary tumor, liver
metastasis, or both and when to consider different forms of
radiotherapy with or without chemotherapy. In the following
section, management of synchronous CRCLM will be elaborated in
details.
In addition, addressing management of extra-hepatic
metastasis (EHM) along with CRCLM is challenging and may end with
dismal outcome; however, surgical intervention can improve OS in
resectable cases. What to do and when to consider resection? We
could estimate the current inquiry from the results of an
international multi-institutional analysis (27) involving 1629 patients who underwent
resection of CRCLM found that most patients had solitary EHM, and
the 5-year survival rates were 26 and 58% for those with and
without EHM, respectively (P<0.01). In addition, EHM
characteristics such as R1 margin positivity, multiple sites, and
location were associated with worse survival. Accordingly, EHM
resection is possible in selected patients without presence of
extensive disease.
The selection criteria for liver resection are
essential in order to avoid an inadequate FLR, a major cause of
surgery-related death. Normally, patients can survive with only 20%
of a healthy normal liver. However, for patients whose livers are
affected by chemotherapy or who expect to receive postoperative
chemotherapy, 30–40% of the liver should be preserved (28,29).
Liver resection is planned if a complete R0 resection is feasible,
at least 2 liver segments with independent inflow and outflow are
spared, and appropriate biliary drainage is maintained.
The choice to administer initial surgical or
chemotherapeutic treatment remains a subject of debate. However,
upfront liver metastasis resection is the primary treatment
modality for resectable CRCLM (rCRCLM) (30–32),
however, most of such cases presented with a higher recurrence rate
(33). Therefore, the National
Comprehensive Cancer Network (NCCN) recommends 6 months of
perioperative systemic chemotherapy. However, standard policy and
treatment strategy are poorly defined (34). Currently, alternative treatment has
been tried and introduced radiofrequency ablation (RFA) in
resectable CRCLM, which has failed to generate good results. A
recent meta-analysis (35) agreed
with this fact, they investigated the role of RFA vs. resection for
rCRCLM and found that the former was associated with poorer OS
(hazard ratio (HR): 1.85, 95% confidence interval (CI): 1.48–2.32,
P<0.00001) and DFS (HR: 1.68, 95% CI: 1.14–2.48, P=0.009).
Thereafter, neoadjuvant chemotherapy has been
proposed to assess tumor biology, at which chemotherapy could be
prolonged and surgery would be delayed in poor responders until
good response was shown (36,37).
Adam et al (38), enrolled
131 patients with rCRCLM found worse 5-year survival in poor
responders compared to stable or responsive disease (8% vs. 30%,
37%; P=0.0001), respectively. Moreover, Ruenberger et al
(39) conducted a prospective trial
to assess the efficacy of 6 cycles of neoadjuvant XELOX or FOLFOX4
in 50 patients with rCRCLM demonstrating recurrence-free survival
rates correlated with tumor responses (24.7, 8.2, and 3.0 months)
in responsive, stable, and progressive disease, respectively. Based
on these results, perioperative chemotherapy upfront could be an
essential partto assess tumor response, which is supported by EORTC
40983 studies (16). However, these
studies reported chemotherapy-associated liver damage and a
significantly higher rate of postoperative complications with
chemotherapy than with surgery alone (25% vs. 16%). Therefore,
chemotherapy may cause liver injury and poor short-term prognosis
consequently (40). Other studies
including those of EORTC 40983 found an association between high
morbidity rate and the number of chemotherapy cycles (17,41,42),
suggested that a period of 3 months preoperative FOLFOX-4
chemotherapy should not br exceed in order to avoid
chemotherapy-related liver toxicity (39).
Several liver resection techniques exist.
Previously, two-stage hepatectomy (TSH) was recommended to reduce
surgical trauma (45). However,
most cancer centers, including our institution, supported a
single-stage approach after finding insignificant morbidity during
perioperative management (46,47).
However, no existing protocol favor simultaneous resection over a
staged approach. The approach depends on the surgeon's experience
and patient's physical status. The only possible advantage of
single stage over two-stage procedure is the earlier initiation of
adjuvant chemotherapy (48).
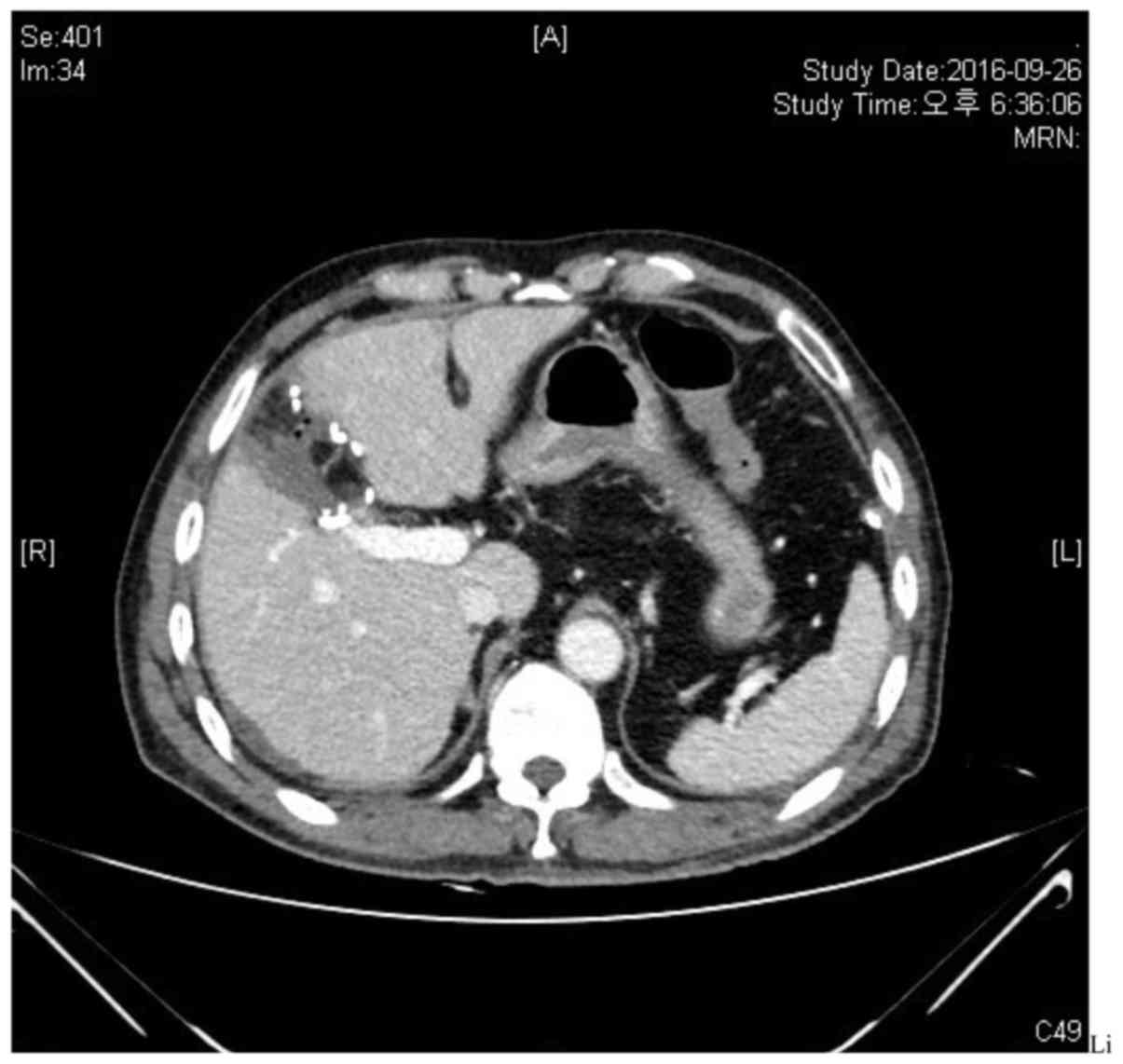
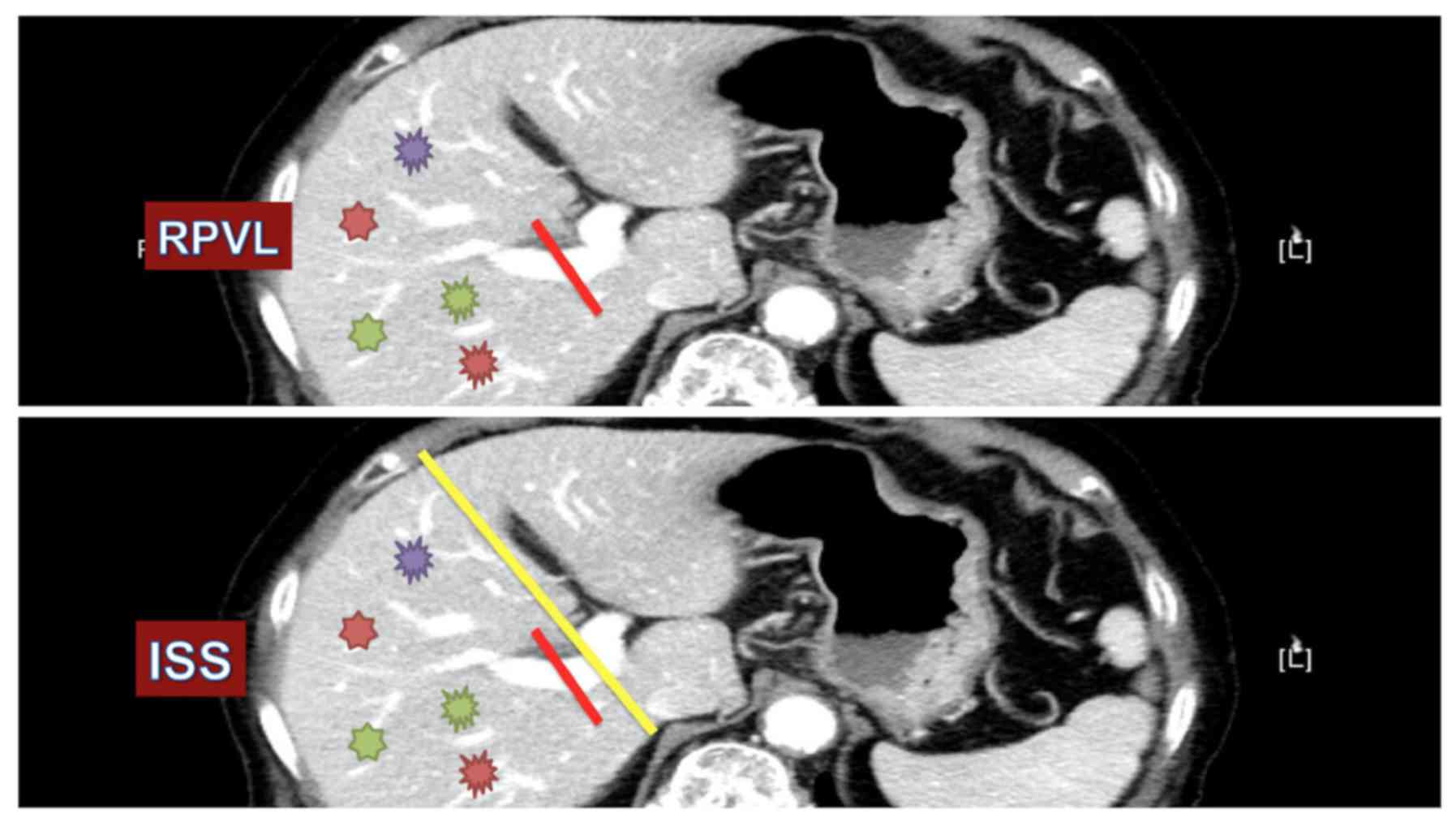
Silberhumer et al (49)
studied 429 patients subjected to operative treatment for CRC with
simultaneous liver metastases; 75 and 25% underwent simultaneous
and staged resection, respectively. The 1-year survival rates were
90.5% in the simultaneous group and 92.6% in the staged group, and
the corresponding 5-year survival rates were 38.5 and 38.9%,
respectively. Simultaneous liver resection and staged procedures
are associated with similar long-term cancer outcomes. We encourage
single-stage liver resection together with primary lesion resection
whenever possible, as shown in Fig.
1.
Moreover, radical extended lymph node dissection
should be considered for suspected lymph nodes in the hepatic
pedicle or in patients with >3 poorly differentiated metastatic
lesions in segments (IV and V) (50). Currently, TSH is considered only if
an adequate liver remnant cannot be preserved after HR; TSH and HR;
In this case, certain groups of liver tumors are resected first,
followed by resection of the remaining tumors in a second procedure
after a liver regeneration period (4–12 months) (51). The two-stage procedure is largely
used for unresectable liver metastasis or to render unresectable
lesions resectable, especially when combined with alternative
treatments such as portal vain embolization or RFA (discussed in
detail later on).
This common scenario presents a real challenge in
the medical field. Whether primary mass resected first to debulk
tumor-related complications or upfront chemotherapy should be
administered first to downstage the tumor. Numerous treatment
procedures are tailored according to the patient's presentation and
tumor criteria as follows:
Upfront chemotherapy is the treatment modality of
choice for uCRCLM. Appropriate chemotherapy regimens promote tumor
downstaging and can subsequently render unresectable tumors into
resectable (i.e., conversion chemotherapy) (52,53).
Previously, single-agent chemotherapy with 5FU and folinic acid
(5FU/LV) yielded a response of 20%. A randomized trial (54), allocated 40 patients to receive
5FU/LV or placebo, marked improved OS was observed with
chemotherapy, compared with placebo (11 months vs. 5 months).
Consequently, combined therapy composed of 5FU and oxaliplatin or
irinotecan treatment has increased response rates to 40–50%, with
estimated median OS durations of 12–20 months (55,56).
Several recent publications have described
well-designed phase III trials that evaluated the benefits of
oxaliplatin-based chemotherapy particularly in improving
pathological response rates (57–61).
This conclusion was investigated in a recent meta-analysis by An
et al (62), and it
confirmed the benefits of oxaliplatin for local and distant
metastasis. Furthermore, Zakaria et al (52) examined the application of three
chemotherapy agents and tumor responses in 42 patients with uCRCLM;
60% achieved tumor reduction, 40% underwent surgery, and the median
survival duration was 26 months. However, a high postoperative
recurrence rate was observed (73%). Overall, a combined approach
with resection yielded higher resectability rates and higher
negative margins for uCRCLM (63,64).
Molecular target agents specific for vascular
endothelial growth factor (VEGF) have been developed, including
bevacizumab and cetuximab. Saltz et al (67), evaluated the efficacy of adding
bevacizumab to oxaliplatin-based chemotherapy [capecitabine plus
oxaliplatin (XELOX) or (FOLFOX-4)] in 1401 patients with CRCLM. The
median PFS durations were 9.4 months in the bevacizumab group and
8.0 months in the placebo group (P=0.0023); the groups had similar
OS and response rates. In another randomized trial conducted by
Bokemeyer et al (68), to
evaluate the addition of cetuximab to FOLFOX-4 vs. FOLFOX-4 only,
cetuximab was associated with a clinically significant increase in
overall response (61% vs. 37%; P=0.011) and reduced risk of disease
progression (hazard ratio=0.57; P=0.0163) when compared with
FOLFOX-4 alone, particularly in KRAS wild-type tumors.
Based on these data, we encourage the FOLFOX
regimen, in addition to target agents, as a first-line treatment of
choice at our institute. Our recent report by Kim et al
(69) reviewed 50 patients with
locally advanced rectal cancer and borderline-resectable liver
metastases. Patients were treated by short-course radiotherapy
(SCRT) and upfront chemotherapy (FOLFOX, FOLFIRI, +/− target
agent), with delayed surgery. Tumor downstaging and R0 resection
were achieved in 35 (70%) patients. The median PFS was 16 months,
and the 2-year PFS rate was 34.8%. Furthermore, chemotherapy can be
administered via hepatic arterial infusion (HAI), which yields
higher response rates to both first and second-line therapies
particularly in oxaliplatin or irinotecan infusion (70,71).
Nevertheless, HAI is a technically demanding procedure that should
be handled by experts. HAI-based treatment strategies are
controversial with regard to procedure-related morbidities such as
sclerosing cholangitis and limited experience (72).
Systemic chemotherapy has been widely studied;
however, the oncologic outcomes are inconclusive in CRCLM (73). Therefore, current questions are
raised whether the radiotherapy dose or pathway could contribute to
achieving better results is controversial. A phase II trial
(69) evaluated a 12-week FOLFOX
regimen with pelvic CRT in 26 patients with symptomatic advanced
rectal cancer and metastatic disease. 18F-fluorodeoxyglucose
positron emission tomography (FDG-PET) revealed metabolic response
rates of 96% for primary rectal cancer and 60% for metastatic
disease; evidence of good pathological responses was also observed
in resected specimens. Of note, the authors of that study invented
a new approach at which RT therapy was divided into 2 courses to
reduce toxicity. Accordingly, 92% of the 26 patients reached
treatment week 11 without deviation, suggesting positive outcomes
of this treatment strategy. The RT formats and strategies will be
discussed in the following sections.
Application of radiotherapy has widely been used in
the field of CRC. In CRCLM, however, SCRT has been proposed along
with chemotherapy and delayed surgery, which has yielded a great
improvement in controlling the tumor locally. Technique and
procedure of SCRT has been previously described in our study
(74). Besides, combined approaches
of SCRT along with FOLFOX have been validated in several recent
studies.
Liver metastases are best eradicated by excision;
however, if resection is unsuitable, consensus suggests that
combination ablative therapy should be considered to prevent liver
failure after major resection. RFA, cryotherapy, or high intensity
focused ultrasound, can be used in combination to offer curative
treatment in patients with unresectable tumors (77,78).
Currently, a phase II randomized extension of the EORTC intergroup
randomized study 40004 (CLOCC) (10) has enrolled 119 patients with uCRCLM
to investigate the benefit of FOLFOX plus RFA vs. FOLFOX alone. The
inclusion criterion was a maximum of 9 liver lesions without
extrahepatic involvement. The 30-month OS rates were 61.7% in the
combination group vs. 57.6% in the control group. The median OS
durations were 45.6 vs. 40.5 months (P<0.01), thus favoring
combination treatment over FOLFOX alone. Abdalla et al
(79) reported their experience
with RFA vs. chemotherapy alone for CRCLM; the authors observed
significant improvements with RFA relative to chemotherapy
alone.
Furthermore, combined therapy (resection+RFA) help
to achieve a R0 status while maintaining an adequate FLR to avoid
postoperative hepatic failure (80). However, surgical decision for RFA
should be crucial and tailored accordingly, otherwise may end with
unwanted consensus in particular of higher local recurrence rate.
Qui et al (81) enrolled 112
patients diagnosed with unresectable liver metastasis from
different primary tumors. The ablation success rates were 93.3% for
hepatocellular carcinoma (HCC) and 96.7% for secondary liver
metastasis. The corresponding 5-year overall recurrence rates of
these diseases were 80 and 77.8%, respectively. Park et al
(82) predicted factors associated
with high recurrence rates after RFA in patients with hepatic
metastases. Lesions with ablative margins of ≥5 mm were associated
with longer disease-free interval than lesions of <5 mm. These
finding are on line with our experience. Hur et al (83) conducted comparative study between HR
and RFA in 67 consecutive patients with solitary CRCLM. Forty-two
patients underwent HR and 25 patients underwent RFA. The 5-year
overall and local recurrence-free survival rates (LRFS) were in
favor of HR (50.1 and 89.7%, respectively) and (25.5 and 69.7%,
respectively) than RFA, particularly in patients with tumor >3
cm. However, LRFS was likewise to resection with tumor size <3
cm (95.7% vs. 85.6%, P=0.304). Thus, we recommend selecting
appropriate patients and tumor character ahead of planning RFA
procedure.
The goal of portal vein embolization (PVE) is to
achieve complete portal occlusion of the targeted segments and
generate adequate liver hypertrophy prior to a proposed surgery.
Preoperative PVE was first described by Elias et al
(90) in 14 patients with hilar
cholangiocarcinoma, in whom successful results were achieved
without major consequences. The Cardiovascular and Interventional
Radiological Society of Europe (CIRSE) reported minor and major
complications of PVE at 25 and 5%, respectively (91). However, PVE contraindications should
be noted; these include extensive ipsilateral tumor thrombus and
clinically evident portal hypertension. However, PVE may be an
important component of two-stage hepatectomy, thus rendering
unresectable bilateral CRCLM resectable (92,93).
Narita et al (94) studied
the outcomes of PVE in 80 patients with liver metastasis, among
whom 61 had completed two-stage hepatectomy. The 5-year OS rate was
32%, and the median OS duration was 39.6 months.
A major drawback of PVE is the risk of tumor growth
after embolization, as observed in a previous large observational
study. The authors assessed the effects of PVE and bevacizumab on
liver hypertrophy and tumor growth to control group (bevacizumab
without PVE). Among 119 study patients, significant increases in
total tumor volume were observed in the PVE group, whereas
decreases were observed in the control arm (0.07 vs. 0.06
cm3/day, P<0.01) (95). An animal study by Maggiori et
al (96) found that PVE
increased tumor growth in the non-occluded liver while decreasing
growth in the occluded liver. This tumor growth after PVE was
poorly understood, but might be attributable to post-PVE
proliferative activity involving increased levels of cytokines and
inflammatory mediators (97).
Therefore, does PVE jeopardize the downstaging effect of
chemotherapy on CRCLM? This debate has not been defined yet.
Noteworthy, hepatocyte growth factor (HGF) has been suggested as
the major liver and tumor stimulus, as reported by Zou et al
(98). Thereafter using of
anti-inflammatory medication to ameliorate PVE proliferative
activity is a topic of debates.
Emerging of Selective internal radiotherapy (SIRT)
contributed to develop the PVE technique. In a meta-analysis
(99), SIRT exhibited appropriate
usefulness in 90% of uCRCLM cases. Therefore, a combination of PVE
and SIRT could provide a surrogate for major hepatectomy (SIRT will
be explained later in this review). However, this combination has
not yet been established (100).
Remaining controversies surrounding challenges and treatment
options suggest that considerable effort will be required in the
future to validate the PVE treatment.
ALPPS has enabled to rescue patients with uCRCLM who
have failed to achieve adequate FLR after PVE. Nevertheless, this
procedure is technically demanding and associated with a high
comorbidity rate (40%) (107). To
date, a systemic review and meta-analysis (108) has evaluated three procedures for
the treatment of liver tumors: ALPPS, PVE, and PVL. The authors
found no significant difference between PVE and PVL in terms of
tumor progression or resection rate, whereas ALPPS was associated
with a significant increase in FLR. In a 2015 meta-analysis, Sun
et al (109) reported a
higher morbidity rate with ALPPS compared with 2-stage hepatectomy
(56.3% vs. 36.1%, P<0.01), and a higher resection rate with
ALPPS (100% vs. 79.1%). Schadde et al (106) conducted a multicenter study of 320
patients at 55 centers. The reported 75% mortality rate was
attributed to liver failure. Accordingly, appropriate selection for
ALPPS is crucial.
Surprisingly, authors argue about the true volume of
the FLR following the ALPPS procedure. Tissue edema and
inflammatory reactions could affect the post-ALPPS liver size,
leading to an over measurement relative to the actual total volume
of the FLR (110). The recent
technique of hepatobiliary scintigraphy can be used to assess total
and regional liver function (111,112). Finally, the ALPPS procedure is in
an early milestone stage and is associated with a higher morbidity
rate than other treatment modalities; however the results remain
controversial (113). Notably, the
mortality rate associated with ALPPS was 9%, but this decreased to
5% in a sub-analysis of patients aged <60 years who were
diagnosed with CRCLM (106). We
conclude that ALPPS surgery should be strongly considered, as it
yields good outcomes in a subset of patients; however, further
evaluation through well-organized trials is required in the
future.
Currently, the new modality for targeting liver
lesions emerged in a form of selective internal radiotherapy (SIRT)
technique in order to target distal tumor vasculature.
Yttrium-microspheres are used for radiotherapy embolization with
high energy and parenchyma penetration of >11 mm, which make it
effective in liver metastasis trapped at the distal end of tumor
vasculature. SIRT, has been previously shown to yield early
successes in patients with HCC (114). Since then, other authors have
investigated the applications of SIRT for liver metastasis,
regardless of primary tumor, and have obtained good results
(115,116). Accordingly, SIRT has been assigned
as the treatment of choice for 90% of uCRCLMs that achieved success
after a chemotherapy failure (99,115).
Van Hazel et al (117)
conducted a randomized clinical trial evaluating the utility of
SIRT plus chemotherapy (FU/LV) vs. chemotherapy alone in 11
patients with uCRCLM. The time to disease progression analysis
favored the SIRT arm (18.6 months vs. 3.6 months, P<0.0005).
Additionally, the median survival duration was significantly longer
in the SIRT arm (29.4 months vs. 12.8 months, P=0.02).
Therefore, SIRT is technically demanding, and
certain levels of skill and experience are warranted before
planning treatment with this procedure. Therefore, SIRT remains in
an early milestone stage, and more effort is needed to validate its
safety and feasibility in CRCLM. The results of recent trials are
listed in Table III.
Although considerable effort has been expended to
improve the outcomes of CRCLM, treatment policies are poorly
defined. For resectable CRCLM, systemic chemotherapy regimens,
together with liver resection, appear to improve DFS when compared
with surgery alone. The OS outcomes, however, have not previously
been well illustrated. For uCRCLM, several techniques intended to
increase the rate of liver resection have emerged. Still,
contradictory data and variable results have contributed to an
inability to determine an appropriate conclusion. Furthermore, SIRT
and ALPPS procedures are demanding in terms of technical skill and
resources, but have yielded promising initial results. Much effort
remains with regard to achieving satisfactory treatment strategies
in CRCLM.
|
1
|
Lykoudis PM, O'Reilly D, Nastos K and
Fusai G: Systematic review of surgical management of synchronous
colorectal liver metastases. Br J Surg. 101:605–612. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Nordlinger B, Van Cutsem E, Gruenberger T,
Glimelius B, Poston G, Rougier P, Sobrero A and Ychou M: European
Colorectal Metastases Treatment Group; Sixth International
Colorectal Liver Metastases Workshop: Combination of surgery and
chemotherapy and the role of targeted agents in the treatment of
patients with colorectal liver metastases: Recommendations from an
expert panel. Ann Oncol. 20:985–992. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Simmonds PC, Primrose JN, Colquitt JL,
Garden OJ, Poston GJ and Rees M: Surgical resection of hepatic
metastases from colorectal cancer: A systematic review of published
studies. Br J Cancer. 94:982–999. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
van Dijk TH, Tamas K, Beukema JC, Beets
GL, Gelderblom AJ, de Jong KP, Nagtegaal ID, Rutten HJ, van de
Velde CJ, Wiggers T, et al: Evaluation of short-course radiotherapy
followed by neoadjuvant bevacizumab, capecitabine, and oxaliplatin
and subsequent radical surgical treatment in primary stage IV
rectal cancer. Ann Oncol. 24:1762–1769. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Manfredi S, Lepage C, Hatem C, Coatmeur O,
Faivre J and Bouvier AM: Epidemiology and management of liver
metastases from colorectal cancer. Ann Surg. 244:254–259. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Bozzetti F, Doci R, Bignami P, Morabito A
and Gennari L: Patterns of failure following surgical resection of
colorectal cancer liver metastases. Rationale for a multimodal
approach. Ann Surg. 205:264–270. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Konopke R, Roth J, Volk A, Pistorius S,
Folprecht G, Zöphel K, Schuetze C, Laniado M, Saeger HD and
Kersting S: Colorectal liver metastases: An update on palliative
treatment options. J Gastrointestin Liver Dis. 21:83–91.
2012.PubMed/NCBI
|
|
8
|
Cummings LC, Payes JD and Cooper GS:
Survival after hepatic resection in metastatic colorectal cancer: A
population-based study. Cancer. 109:718–726. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
de Jong MC, Pulitano C, Ribero D, Strub J,
Mentha G, Schulick RD, Choti MA, Aldrighetti L, Capussotti L and
Pawlik TM: Rates and patterns of recurrence following curative
intent surgery for colorectal liver metastasis: An international
multi-institutional analysis of 1669 patients. Ann Surg.
250:440–448. 2009.PubMed/NCBI
|
|
10
|
Ruers T, Punt C, Van Coevorden F, Pierie
JP, Borel-Rinkes I, Ledermann JA, Poston G, Bechstein W, Lentz MA,
Mauer M, et al: Radiofrequency ablation combined with systemic
treatment versus systemic treatment alone in patients with
non-resectable colorectal liver metastases: a randomized EORTC
Intergroup phase II study (EORTC 40004). Ann Oncol. 23:2619–2626.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Edge SB and Compton CC: The American Joint
Committee on Cancer: The 7th edition of the AJCC cancer staging
manual and the future of TNM. Ann Surg Oncol. 17:1471–1474. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Mekenkamp LJ, Koopman M, Teerenstra S, van
Krieken JH, Mol L, Nagtegaal ID and Punt CJ: Clinicopathological
features and outcome in advanced colorectal cancer patients with
synchronous vs. metachronous metastases. Br J Cancer. 103:159–164.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Siriwardena AK, Mason JM, Mullamitha S,
Hancock HC and Jegatheeswaran S: Management of colorectal cancer
presenting with synchronous liver metastases. Nat Rev Clin Oncol.
11:446–459. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Adam R: Chemotherapy and surgery: new
perspectives on the treatment of unresectable liver metastases. Ann
Oncol. 14:(Suppl 2). ii13–ii16. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Nordlinger B, Van Cutsem E, Rougier P,
Köhne CH, Ychou M, Sobrero A, Adam R, Arvidsson D, Carrato A,
Georgoulias V, et al: Does chemotherapy prior to liver resection
increase the potential for cure in patients with metastatic
colorectal cancer? A report from the European Colorectal Metastases
Treatment Group. Eur J Cancer. 43:2037–2045. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Nordlinger B, Sorbye H, Glimelius B,
Poston GJ, Schlag PM, Rougier P, Bechstein WO, Primrose JN, Walpole
ET, Finch-Jones M, et al: EORTC Gastro-Intestinal Tract Cancer
Group; Cancer Research UK; Arbeitsgruppe Lebermetastasen
und-tumoren in der Chirurgischen Arbeitsgemeinschaft Onkologie
(ALM-CAO); Australasian Gastro-Intestinal Trials Group (AGITG);
Fédération Francophone de Cancérologie Digestive (FFCD):
Perioperative chemotherapy with FOLFOX4 and surgery versus surgery
alone for resectable liver metastases from colorectal cancer (EORTC
Intergroup trial 40983): A randomised controlled trial. Lancet.
371:1007–1016. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Cunningham D, Humblet Y, Siena S, Khayat
D, Bleiberg H, Santoro A, Bets D, Mueser M, Harstrick A, Verslype
C, et al: Cetuximab monotherapy and cetuximab plus irinotecan in
irinotecan-refractory metastatic colorectal cancer. N Engl J Med.
351:337–345. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Bramhall SR, Gur U, Coldham C, Gunson BK,
Mayer AD, McMaster P, Candinas D, Buckels JA and Mirza DF: Liver
resection for colorectal metastases. Ann R Coll Surg Engl.
85:334–339. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Clavien PA, Petrowsky H, DeOliveira ML and
Graf R: Strategies for safer liver surgery and partial liver
transplantation. N Engl J Med. 356:1545–1559. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hou W and Zhu X: Extra vascular
interventional treatment of liver cancer, present and future. Drug
Discov Ther. 9:335–341. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
van Dam RM, Lodewick TM, van den Broek MA,
de Jong MC, Greve JW, Jansen RL, Bemelmans MH, Neumann UP, Damink
Olde SW and Dejong CH: Outcomes of extended versus limited
indications for patients undergoing a liver resection for
colorectal cancer liver metastases. HPB (Oxford). 16:550–559. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Vauthey JN, Pawlik TM, Abdalla EK, Arens
JF, Nemr RA, Wei SH, Kennamer DL, Ellis LM and Curley SA: Is
extended hepatectomy for hepatobiliary malignancy justified? Ann
Surg. 239:722–730; discussion 730–732. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Tsoulfas G, Pramateftakis MG and Kanellos
I: Surgical treatment of hepatic metastases from colorectal cancer.
World J Gastrointest Oncol. 3:1–9. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Pawlik TM, Abdalla EK, Ellis LM, Vauthey
JN and Curley SA: Debunking dogma: Surgery for four or more
colorectal liver metastases is justified. J Gastrointest Surg.
10:240–248. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Altendorf-Hofmann A and Scheele J: A
critical review of the major indicators of prognosis after
resection of hepatic metastases from colorectal carcinoma. Surg
Oncol Clin N Am. 12:165–192, xi. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Pulitanò C, Bodingbauer M, Aldrighetti L,
de Jong MC, Castillo F, Schulick RD, Parks RW, Choti MA, Wigmore
SJ, Gruenberger T, et al: Liver resection for colorectal metastases
in presence of extrahepatic disease: Results from an international
multi-institutional analysis. Ann Surg Oncol. 18:1380–1388. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Mattar RE, Al-Alem F, Simoneau E and
Hassanain M: Preoperative selection of patients with colorectal
cancer liver metastasis for hepatic resection. World J
Gastroenterol. 22:567–581. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Abdalla EK, Denys A, Chevalier P, Nemr RA
and Vauthey JN: Total and segmental liver volume variations:
Implications for liver surgery. Surgery. 135:404–410. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Chang GJ: Challenge of primary tumor
management in patients with stage IV colorectal cancer. J Clin
Oncol. 30:3165–3166. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Choti MA, Sitzmann JV, Tiburi MF,
Sumetchotimetha W, Rangsin R, Schulick RD, Lillemoe KD, Yeo CJ and
Cameron JL: Trends in long-term survival following liver resection
for hepatic colorectal metastases. Ann Surg. 235:759–766. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Fong Y, Fortner J, Sun RL, Brennan MF and
Blumgart LH: Clinical score for predicting recurrence after hepatic
resection for metastatic colorectal cancer: Analysis of 1001
consecutive cases. Ann Surg. 230:309–318; discussion 318–321. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Kemeny N, Kemeny MM and Lawrence TS: Liver
metastasesClinical Oncology. Abeloff MD, Armitage JO, Lichter AS
and Niederhuber JE: Churchill Livingstone; New York: pp. 886–921.
2000
|
|
34
|
National Comprehensive Cancer Network:
Colon cancer guidelines version 3. 2012.(28/9/2014). http://www.nccn.org/professionals/physician_gls/pdf/colorectal_screening.pdf
|
|
35
|
Bai H, Huangz X, Jing L, Zeng Q and Han L:
The effect of radiofrequency ablation vs. liver resection on
survival outcome of colorectal liver metastases (CRLM): A
meta-analysis. Hepatogastroenterology. 62:373–377. 2015.PubMed/NCBI
|
|
36
|
Gruenberger Th, Gruenberger B, Becherer A,
Kettenbach J, Dieckmann K and Schima W: Interdisciplinary
management of colorectal cancer liver metastases. Eur Surg.
38:107–111. 2006. View Article : Google Scholar
|
|
37
|
Viganò L, Capussotti L, De Rosa G, De
Saussure WO, Mentha G and Rubbia-Brandt L: Liver resection for
colorectal metastases after chemotherapy: Impact of
chemotherapy-related liver injuries, pathological tumor response,
and micrometastases on long-term survival. Ann Surg. 258:731–742.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Adam R, Pascal G, Castaing D, Azoulay D,
Delvart V, Paule B, Levi F and Bismuth H: Tumor progression while
on chemotherapy: A contraindication to liver resection for multiple
colorectal metastases? Ann Surg. 240:1052–1064. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Gruenberger B, Scheithauer W, Punzengruber
R, Zielinski C, Tamandl D and Gruenberger T: Importance of response
to neoadjuvant chemotherapy in potentially curable colorectal
cancer liver metastases. BMC Cancer. 8:1202008. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Khan AZ, Morris-Stiff G and Makuuchi M:
Patterns of chemotherapy-induced hepatic injury and their
implications for patients undergoing liver resection for colorectal
liver metastases. J Hepatobiliary Pancreat Surg. 16:137–144. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Aloia T, Sebagh M, Plasse M, Karam V, Lévi
F, Giacchetti S, Azoulay D, Bismuth H, Castaing D and Adam R: Liver
histology and surgical outcomes after preoperative chemotherapy
with fluorouracil plus oxaliplatin in colorectal cancer liver
metastases. J Clin Oncol. 24:4983–4990. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Pulitanò C, Aldrighetti L, Arru M, Vitali
G, Ronzoni M, Catena M, Finazzi R, Villa E and Ferla G: Influence
of preoperative chemotherapy on the risk of major hepatectomy for
colorectal liver metastases. Ann Surg. 244:833–835; author reply
835. 2006. View Article : Google Scholar
|
|
43
|
Khoo E, O'Neill S, Brown E, Wigmore SJ and
Harrison EM: Systematic review of systemic adjuvant, neoadjuvant
and perioperative chemotherapy for resectable colorectal-liver
metastases. HPB (Oxford). 18:485–493. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Primrose J, Falk S, Finch-Jones M, Valle
J, O'Reilly D, Siriwardena A, Hornbuckle J, Peterson M, Rees M,
Iveson T, et al: Systemic chemotherapy with or without cetuximab in
patients with resectable colorectal liver metastasis: The New EPOC
randomised controlled trial. Lancet Oncol. 15:601–611. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Fujita S, Akasu T and Moriya Y: Resection
of synchronous liver metastases from colorectal cancer. Jpn J Clin
Oncol. 30:7–11. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Tanaka K, Shimada H, Matsuo K, Nagano Y,
Endo I, Sekido H and Togo S: Outcome after simultaneous colorectal
and hepatic resection for colorectal cancer with synchronous
metastases. Surgery. 136:650–659. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Martin R, Paty P, Fong Y, Grace A, Cohen
A, DeMatteo R, Jarnagin W and Blumgart L: Simultaneous liver and
colorectal resections are safe for synchronous colorectal liver
metastasis. J Am Coll Surg. 197:233–241; discussion 241. –242.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Chua HK, Sondenaa K, Tsiotos GG, Larson
DR, Wolff BG and Nagorney DM: Concurrent vs. staged colectomy and
hepatectomy for primary colorectal cancer with synchronous hepatic
metastases. Dis Colon Rectum. 47:1310–1316. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Silberhumer GR, Paty PB, Denton B, Guillem
J, Gonen M, Araujo RL, Nash GM, Temple LK, Allen PJ, DeMatteo RP,
et al: Long-term oncologic outcomes for simultaneous resection of
synchronous metastatic liver and primary colorectal cancer.
Surgery. 160:67–73. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Jaeck D and Pessaux P: Bilobar colorectal
liver metastases: Treatment options. Surg Oncol Clin N Am.
17:553–568, ix. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Sharma S, Camci C and Jabbour N:
Management of hepatic metastasis from colorectal cancers: An
update. J Hepatobiliary Pancreat Surg. 15:570–580. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Zakaria S, Donohue JH, Que FG, Farnell MB,
Schleck CD, Ilstrup DM and Nagorney DM: Hepatic resection for
colorectal metastases: Value for risk scoring systems? Ann Surg.
246:183–191. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Leonard GD, Brenner B and Kemeny NE:
Neoadjuvant chemotherapy before liver resection for patients with
unresectable liver metastases from colorectal carcinoma. J Clin
Oncol. 23:2038–2048. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Scheithauer W, Rosen H, Kornek GV, Sebesta
C and Depisch D: Randomised comparison of combination chemotherapy
plus supportive care with supportive care alone in patients with
metastatic colorectal cancer. BMJ. 306:752–755. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Saltz LB, Cox JV, Blanke C, Rosen LS,
Fehrenbacher L, Moore MJ, Maroun JA, Ackland SP, Locker PK, Pirotta
N, et al: Irinotecan Study Group: Irinotecan plus fluorouracil and
leucovorin for metastatic colorectal cancer. N Engl J Med.
343:905–914. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
de Gramont A, Figer A, Seymour M, Homerin
M, Hmissi A, Cassidy J, Boni C, Cortes-Funes H, Cervantes A, Freyer
G, et al: Leucovorin and fluorouracil with or without oxaliplatin
as first-line treatment in advanced colorectal cancer. J Clin
Oncol. 18:2938–2947. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Aschele C, Cionini L, Lonardi S, Pinto C,
Cordio S, Rosati G, Artale S, Tagliagambe A, Ambrosini G, Rosetti
P, et al: Primary tumor response to preoperative chemoradiation
with or without oxaliplatin in locally advanced rectal cancer:
Pathologic results of the STAR-01 randomized phase III trial. J
Clin Oncol. 29:2773–2780. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Rödel C, Liersch T, Becker H, Fietkau R,
Hohenberger W, Hothorn T, Graeven U, Arnold D, Lang-Welzenbach M,
Raab HR, et al: German Rectal Cancer Study Group: Preoperative
chemoradiotherapy and postoperative chemotherapy with fluorouracil
and oxaliplatin versus fluorouracil alone in locally advanced
rectal cancer: Initial results of the German CAO/ARO/AIO-04
randomised phase 3 trial. Lancet Oncol. 13:679–687. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Allegra CJ, Yothers G, O'Connell MJ, Beart
RW, Wozniak TF, Pitot HC, Shields AF, Landry JC, Ryan DP, Arora A,
et al: Neoadjuvant 5-FU or capecitabine plus radiation with or
without oxaliplatin in rectal cancer patients: A phase III
randomized clinical trial. J Natl Cancer Inst. 107:pii: djv248.
2015. View Article : Google Scholar :
|
|
60
|
Schmoll H-J, Haustermans K, Price TJ,
Nordlinger B, Hofheinz R, Daisne J-F, Janssens J, Brenner B,
Schmidt P, Reinel H, et al: Preoperative chemoradiotherapy and
postoperative chemotherapy with capecitabine and oxaliplatin versus
capecitabine alone in locally advanced rectal cancer: First results
of the PETACC-6 randomized phase III trial. J Clin Oncol.
31:(Suppl). 35312013.PubMed/NCBI
|
|
61
|
Gérard JP, Azria D, Gourgou-Bourgade S,
Martel-Laffay I, Hennequin C, Etienne PL, Vendrely V, François E,
de La Roche G, Bouché O, et al: Comparison of two neoadjuvant
chemoradiotherapy regimens for locally advanced rectal cancer:
Results of the phase III trial ACCORD 12/0405-Prodige 2. J Clin
Oncol. 28:1638–1644. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
An X, Lin X, Wang FH, Goodman K, Cai PQ,
Kong LH, Fang YJ, Gao YH, Lin JZ, Wan DS, et al: Short term results
of neoadjuvant chemoradiotherapy with fluoropyrimidine alone or in
combination with oxaliplatin in locally advanced rectal cancer: A
meta analysis. Eur J Cancer. 49:843–851. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Razafindratsira T, Isambert M and Evrard
S: Complications of intraoperative radiofrequency ablation of liver
metastases. HPB (Oxford). 13:15–23. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Evrard S, Rivoire M, Arnaud J, Lermite E,
Bellera C, Fonck M, Becouarn Y, Lalet C, Puildo M and
Mathoulin-Pelissier S: Unresectable colorectal cancer liver
metastases treated by intraoperative radiofrequency ablation with
or without resection. Br J Surg. 99:558–565. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Tournigand C, André T, Achille E, Lledo G,
Flesh M, Mery-Mignard D, Quinaux E, Couteau C, Buyse M, Ganem G, et
al: FOLFIRI followed by FOLFOX6 or the reverse sequence in advanced
colorectal cancer: A randomized GERCOR study. J Clin Oncol.
22:229–237. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Falcone A, Ricci S, Brunetti I, Pfanner E,
Allegrini G, Barbara C, Crinò L, Benedetti G, Evangelista W,
Fanchini L, et al: Gruppo Oncologico Nord Ovest: Phase III trial of
infusional fluorouracil, leucovorin, oxaliplatin, and irinotecan
(FOLFOXIRI) compared with infusional fluorouracil, leucovorin, and
irinotecan (FOLFIRI) as first-line treatment for metastatic
colorectal cancer: The Gruppo Oncologico Nord Ovest. J Clin Oncol.
25:1670–1676. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Saltz LB, Clarke S, Díaz-Rubio E,
Scheithauer W, Figer A, Wong R, Koski S, Lichinitser M, Yang TS,
Rivera F, et al: Bevacizumab in combination with oxaliplatin-based
chemotherapy as first-line therapy in metastatic colorectal cancer:
A randomized phase III study. J Clin Oncol. 26:2013–2019. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Bokemeyer C, Bondarenko I, Makhson A,
Hartmann JT, Aparicio J, de Braud F, Donea S, Ludwig H, Schuch G,
Stroh C, et al: Fluorouracil, leucovorin, and oxaliplatin with and
without cetuximab in the first-line treatment of metastatic
colorectal cancer. J Clin Oncol. 27:663–671. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Kim KH, Shin SJ, Cho MS, Ahn JB, Jung M,
Kim TI, Park YS, Kim H, Kim NK and Koom WS: A phase II study of
preoperative mFOLFOX6 with short-course radiotherapy in patients
with locally advanced rectal cancer and liver-only metastasis.
Radiother Oncol. 118:369–374. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Grothey A, Jordan K, Kellner O, Constantin
C, Dietrich G, Kroening H, Mantovani L, Schlichting C, Forstbauer H
and Schmoll H-J: Capecitabine/irinotecan (Capiri) and
capecitabine/oxaliplatin (CapOx) are active second-line protocols
in patients with advanced colorectal cancer (ACRC) after failure of
first-line combination therapy: results of a randomized phase II
study. J Clin Oncol. 22:(Suppl 14). 35342004. View Article : Google Scholar
|
|
71
|
Shimonov M, Hayat H, Chaitchik S, Brener
J, Schachter P and Czerniak A: Combined systemic chronotherapy and
hepatic artery infusion for the treatment of metastatic colorectal
cancer confined to the liver. Chemotherapy. 51:111–115. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Kelly RJ, Kemeny NE and Leonard GD:
Current strategies using hepatic arterial infusion chemotherapy for
the treatment of colorectal cancer. Clin Colorectal Cancer.
5:166–174. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Lévi F, Giacchetti S, Adam R, Zidani R,
Metzger G and Misset JL: Chronomodulation of chemotherapy against
metastatic colorectal cancer. Eur J Cancer. 31A:1264–1270. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Shin SJ, Yoon HI, Kim NK, Lee KY, Min BS,
Ahn JB, Keum KC and Koom WS: Upfront systemic chemotherapy and
preoperative short-course radiotherapy with delayed surgery for
locally advanced rectal cancer with distant metastases. Radiat
Oncol. 6:992011. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Radu C, Berglund A, Påhlman L and
Glimelius B: Short-course preoperative radiotherapy with delayed
surgery in rectal cancer - a retrospective study. Radiother Oncol.
87:343–349. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Yoon HI, Koom WS, Kim TH, Ahn JB, Jung M,
Kim TI, Kim H, Shin SJ and Kim NK: Upfront systemic chemotherapy
and short-course radiotherapy with delayed surgery for locally
advanced rectal cancer with distant metastases: Outcomes,
compliance, and favorable prognostic factors. PLoS One.
11:e01614752016. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Brooks AJ, Wang F, Alfredson M, Yan TD and
Morris DL: Synchronous liver resection and cryotherapy for
colorectal metastases: survival analysis. Surgeon. 3:265–268. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Kennedy JE, Wu F, ter Haar GR, Gleeson FV,
Phillips RR, Middleton MR and Cranston D: High-intensity focused
ultrasound for the treatment of liver tumours. Ultrasonics.
42:931–935. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Abdalla EK, Vauthey JN, Ellis LM, Ellis V,
Pollock R, Broglio KR, Hess K and Curley SA: Recurrence and
outcomes following hepatic resection, radiofrequency ablation, and
combined resection/ablation for colorectal liver metastases. Ann
Surg. 239:818–827. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Khatri VP, Chee KG and Petrelli NJ: Modern
multimodality approach to hepatic colorectal metastases: Solutions
and controversies. Surg Oncol. 16:71–83. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Qiu J, Chen S and Wu H: Long-term outcomes
after hepatic resection combined with radiofrequency ablation for
initially unresectable multiple and bilobar liver malignancies. J
Surg Res. 188:14–20. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Park MJ, Kim TH, Lee KM, Cheong JY and Kim
JK: Radiofrequency ablation of metastatic liver masses: Recurrence
patterns and prognostic factors based on radiologic features.
Hepatogastroenterology. 60:563–567. 2013.PubMed/NCBI
|
|
83
|
Hur H, Ko YT, Min BS, Kim KS, Choi JS,
Sohn SK, Cho CH, Ko HK, Lee JT and Kim NK: Comparative study of
resection and radiofrequency ablation in the treatment of solitary
colorectal liver metastases. Am J Surg. 197:728–736. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Mima K, Beppu T, Chikamoto A, Miyamoto Y,
Nakagawa S, Kuroki H, Okabe H, Hayashi H, Sakamoto Y, Watanabe M,
et al: Hepatic resection combined with radiofrequency ablation for
initially unresectable colorectal liver metastases after effective
chemotherapy is a safe procedure with a low incidence of local
recurrence. Int J Clin Oncol. 18:847–855. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Berber E, Pelley R and Siperstein AE:
Predictors of survival after radiofrequency thermal ablation of
colorectal cancer metastases to the liver: A prospective study. J
Clin Oncol. 23:1358–1364. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Solbiati L, Livraghi T, Goldberg SN,
Ierace T, Meloni F, Dellanoce M, Cova L, Halpern EF and Gazelle GS:
Percutaneous radio-frequency ablation of hepatic metastases from
colorectal cancer: Long-term results in 117 patients. Radiology.
221:159–166. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Mulier S, Ni Y, Jamart J, Ruers T, Marchal
G and Michel L: Local recurrence after hepatic radiofrequency
coagulation: Multivariate meta-analysis and review of contributing
factors. Ann Surg. 242:158–171. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Cirocchi R, Trastulli S, Boselli C,
Montedori A, Cavaliere D, Parisi A, Noya G and Abraha I:
Radiofrequency ablation in the treatment of liver metastases from
colorectal cancer. Cochrane Database Syst Rev. 6:CD0063172012.
|
|
89
|
Bipat S, van Leeuwen MS, Comans EF, Pijl
ME, Bossuyt PM, Zwinderman AH and Stoker J: Colorectal liver
metastases: CT, MR imaging, and PET for diagnosis - meta-analysis.
Radiology. 237:123–131. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Elias D, De Baere T, Roche A, Mducreux
Leclere J and Lasser P: During liver regeneration following right
portal embolization the growth rate of liver metastases is more
rapid than that of the liver parenchyma. Br J Surg. 86:784–788.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Denys A, Bize P, Demartines N, Deschamps F
and De Baere T: Cardiovascular and Interventional Radiological
Society of Europe: Quality improvement for portal vein
embolization. Cardiovasc Intervent Radiol. 33:452–456. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Abdalla EK, Bauer TW, Chun YS, D'Angelica
M, Kooby DA and Jarnagin WR: Locoregional surgical and
interventional therapies for advanced colorectal cancer liver
metastases: expert consensus statements. HPB (Oxford). 15:119–130.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Brouquet A, Abdalla EK, Kopetz S, Garrett
CR, Overman MJ, Eng C, Andreou A, Loyer EM, Madoff DC, Curley SA,
et al: High survival rate after two-stage resection of advanced
colorectal liver metastases: Response-based selection and complete
resection define outcome. J Clin Oncol. 29:1083–1090. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Narita M, Oussoultzoglou E, Jaeck D,
Fuchschuber P, Rosso E, Pessaux P, Marzano E and Bachellier P:
Two-stage hepatectomy for multiple bilobar colorectal liver
metastases. Br J Surg. 98:1463–1475. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Simoneau E, Aljiffry M, Salman A,
Abualhassan N, Cabrera T, Valenti D, El Baage A, Jamal M, Kavan P,
Al-Abbad S, et al: Portal vein embolization stimulates tumour
growth in patients with colorectal cancer liver metastases. HPB
(Oxford). 14:461–468. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Maggiori L, Bretagnol F, Sibert A, Paradis
V, Vilgrain V and Panis Y: Selective portal vein ligation and
embolization induce different tumoral responses in the rat liver.
Surgery. 149:496–503. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Pamecha V, Levene A, Grillo F, Woodward N,
Dhillon A and Davidson BR: Effect of portal vein embolisation on
the growth rate of colorectal liver metastases. Br J Cancer.
100:617–622. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Zou RH, Li AH, Han F, Hong J, Li BK, Huang
W, Huang L and Yuan YF: Liver hypertrophy and accelerated growth of
implanted tumors in nonembolized liver of rabbit after left portal
vein embolization. J Surg Res. 178:255–263. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Vente MA, Wondergem M, van der Tweel I,
van den Bosch MA, Zonnenberg BA, Lam MG, van Het Schip AD and
Nijsen JF: Yttrium-90 microsphere radioembolization for the
treatment of liver malignancies: A structured meta-analysis. Eur
Radiol. 19:951–959. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
de Graaf W, van den Esschert JW, van
Lienden KP and van Gulik TM: Induction of tumor growth after
preoperative portal vein embolization: Is it a real problem? Ann
Surg Oncol. 16:423–430. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Schnitzbauer AA, Lang SA, Goessmann H,
Nadalin S, Baumgart J, Farkas SA, Fichtner-Feigl S, Lorf T,
Goralcyk A, Hörbelt R, et al: Right portal vein ligation combined
with in situ splitting induces rapid left lateral liver lobe
hypertrophy enabling 2-staged extended right hepatic resection in
small-for-size settings. Ann Surg. 255:405–414. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Gauzolino R, Castagnet M, Blanleuil ML and
Richer JP: The ALPPS technique for bilateral colorectal metastases:
Three ‘variations on a theme’. Updates Surg. 65:141–148. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Honjo I, Suzuki T, Ozawa K, Takasan H,
Kitamura O and Ishikawa T: Ligation of a branch of the portal vein
for carcinoma of the liver. Am J Surg. 130:296–302. 1975.
View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Aussilhou B, Lesurtel M, Sauvanet A,
Farges O, Dokmak S, Goasguen N, Sibert A, Vilgrain V and Belghiti
J: Right portal vein ligation is as efficient as portal vein
embolization to induce hypertrophy of the left liver remnant. J
Gastrointest Surg. 12:297–303. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Robles R, Marín C, Lopez-Conesa A, Capel
A, Perez-Flores D and Parrilla P: Comparative study of right portal
vein ligation versus embolisation for induction of hypertrophy in
two-stage hepatectomy for multiple bilateral colorectal liver
metastases. Eur J Surg Oncol. 38:586–593. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Schadde E, Raptis DA, Schnitzbauer AA,
Ardiles V, Tschuor C, Lesurtel M, Abdalla EK, Hernandez-Alejandro
R, Jovine E, Machado M, et al: Prediction of mortality after ALPPS
Stage-1: An analysis of 320 patients from the International ALPPS
Registry. Ann Surg. 262:780–786. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Shindoh J, Vauthey JN, Zimmitti G, Curley
SA, Huang SY, Mahvash A, Gupta S, Wallace MJ and Aloia TA: Analysis
of the efficacy of portal vein embolization for patients with
extensive liver malignancy and very low future liver remnant
volume, including a comparison with the associating liver partition
with portal vein ligation for staged hepatectomy approach. J Am
Coll Surg. 217:126–134. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Pandanaboyana S, Bell R, Hidalgo E,
Toogood G, Prasad KR, Bartlett A and Lodge JP: A systematic review
and meta-analysis of portal vein ligation versus portal vein
embolization for elective liver resection. Surgery. 157:690–698.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Sun Z, Tang W, Sakamoto Y, Hasegawa K and
Kokudo N: A systematic review and meta-analysis of feasibility,
safety and efficacy of associating liver partition and portal vein
ligation for staged hepatectomy (ALPPS) versus two-stage
hepatectomy (TSH). Biosci Trends. 9:284–288. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Shteyer E, Liao Y, Muglia LJ, Hruz PW and
Rudnick DA: Disruption of hepatic adipogenesis is associated with
impaired liver regeneration in mice. Hepatology. 40:1322–1332.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Hoekstra LT, de Graaf W, Nibourg GA, Heger
M, Bennink RJ, Stieger B and van Gulik TM: Physiological and
biochemical basis of clinical liver function tests: A review. Ann
Surg. 257:27–36. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Guiu B, Bize P, Gunthern D, Demartines N,
Halkic N and Denys A: Portal vein embolization before right
hepatectomy: Improved results using n-butyl-cyanoacrylate compared
to microparticles plus coils. Cardiovasc Intervent Radiol.
36:1306–1312. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Eshmuminov D, Raptis DA, Linecker M,
Wirsching A, Lesurtel M and Clavien PA: Meta-analysis of
associating liver partition with portal vein ligation and portal
vein occlusion for two-stage hepatectomy. Br J Surg. 103:1768–1782.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Lau WY, Ho S, Leung TW, Chan M, Ho R,
Johnson PJ and Li AK: Selective internal radiation therapy for
nonresectable hepatocellular carcinoma with intraarterial infusion
of 90yttrium microspheres. Int J Radiat Oncol Biol Phys.
40:583–592. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Murthy R, Xiong H, Nunez R, Cohen AC,
Barron B, Szklaruk J, Madoff DC, Gupta S, Wallace MJ, Ahrar K, et
al: Yttrium 90 resin microspheres for the treatment of unresectable
colorectal hepatic metastases after failure of multiple
chemotherapy regimens: Preliminary results. J Vasc Interv Radiol.
16:937–945. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Welsh JS, Kennedy AS and Thomadsen B:
Selective Internal Radiation Therapy (SIRT) for liver metastases
secondary to colorectal adenocarcinoma. Int J Radiat Oncol Biol
Phys. 66:(Suppl). S62–S73. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Van Hazel G, Blackwell A, Anderson J,
Price D, Moroz P, Bower G, Cardaci G and Gray B: Randomised phase 2
trial of SIR-Spheres plus fluorouracil/leucovorin chemotherapy
versus fluorouracil/leucovorin chemotherapy alone in advanced
colorectal cancer. J Surg Oncol. 88:78–85. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Van Hazel GA, Heinemann V, Sharma NK,
Findlay MP, Ricke J, Peeters M, Perez D, Robinson BA, Strickland
AH, Ferguson T, et al: SIRFLOX: Randomized phase III trial
comparing first-line mFOLFOX6 (plus or minus bevacizumab) versus
mFOLFOX6 (plus or minus bevacizumab) plus selective internal
radiation therapy in patients with metastatic colorectal cancer. J
Clin Oncol. 34:1723–1731. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Bokemeyer C, Van Cutsem E, Rougier P,
Ciardiello F, Heeger S, Schlichting M, Celik I and Köhne CH:
Addition of cetuximab to chemotherapy as first-line treatment for
KRAS wild-type metastatic colorectal cancer: Pooled analysis of the
CRYSTAL and OPUS randomised clinical trials. Eur J Cancer.
48:1466–1475. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Sharma RA, Van Hazel GA, Morgan B, Berry
DP, Blanshard K, Price D, Bower G, Shannon JA, Gibbs P and Steward
WP: Radioembolization of liver metastases from colorectal cancer
using yttrium-90 microspheres with concomitant systemic
oxaliplatin, fluorouracil, and leucovorin chemotherapy. J Clin
Oncol. 25:1099–1106. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Stubbs RS and Wickremesekera SK: Selective
internal radiation therapy (SIRT): A new modality for treating
patients with colorectal liver metastases. HPB (Oxford). 6:133–139.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Nordlinger B, Sorbye H, Glimelius B,
Poston GJ, Schlag PM, Rougier P, Bechstein WO, Primrose JN, Walpole
ET, Finch-Jones M, et al: EORTC Gastro-Intestinal Tract Cancer
Group; Cancer Research UK; Arbeitsgruppe Lebermetastasen
und-tumoren in der Chirurgischen Arbeitsgemeinschaft Onkologie
(ALM-CAO); Australasian Gastro-Intestinal Trials Group (AGITG);
Fédération Francophone de Cancérologie Digestive (FFCD):
Perioperative FOLFOX4 chemotherapy and surgery versus surgery alone
for resectable liver metastases from colorectal cancer (EORTC
40983): Long-term results of a randomised, controlled, phase 3
trial. Lancet Oncol. 14:1208–1215. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Ychou M, Hohenberger W, Thezenas S,
Navarro M, Maurel J, Bokemeyer C, Shacham-Shmueli E, Rivera F, Choi
Kwok-Keung C and Santoro A: A randomized phase III study comparing
adjuvant 5-fluorouracil/folinic acid with FOLFIRI in patients
following complete resection of liver metastases from colorectal
cancer. Ann Oncol. 20:1964–1970. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Portier G, Elias D, Bouche O, Rougier P,
Bosset JF, Saric J, Belghiti J, Piedbois P, Guimbaud R, Nordlinger
B, et al: Multicenter randomized trial of adjuvant fluorouracil and
folinic acid compared with surgery alone after resection of
colorectal liver metastases: FFCD ACHBTH AURC 9002 trial. J Clin
Oncol. 24:4976–4982. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Hatfield P, Hingorani M, Radhakrishna G,
Cooper R, Melcher A, Crellin A, Kwok-Williams M and
Sebag-Montefiore D: Short-course radiotherapy, with elective delay
prior to surgery, in patients with unresectable rectal cancer who
have poor performance status or significant co-morbidity. Radiother
Oncol. 92:210–214. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Pettersson D, Holm T, Iversen H, Blomqvist
L, Glimelius B and Martling A: Preoperative short-course
radiotherapy with delayed surgery in primary rectal cancer. Br J
Surg. 99:577–583. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Turkmen C, Ucar A, Poyanli A, Vatankulu B,
Ozkan G, Basaran M, Serin K, Sanli Y and Adalet I: Initial outcome
after selective intraarterial radionuclide therapy with yttrium-90
microspheres as salvage therapy for unresectable metastatic liver
disease. Cancer Biother Radiopharm. 28:534–540. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Kucuk ON, Soydal C, Lacin S, Ozkan E and
Bilgic S: Selective intraarterial radionuclide therapy with
Yttrium-90 (Y-90) microspheres for unresectable primary and
metastatic liver tumors. World J Surg Oncol. 9:862011. View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Björnsson B, Sparrelid E, Røsok B,
Pomianowska E, Hasselgren K, Gasslander T, Bjørnbeth BA, Isaksson B
and Sandström P: Associating liver partition and portal vein
ligation for staged hepatectomy in patients with colorectal liver
metastases - Intermediate oncological results. Eur J Surg Oncol.
42:531–537. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Kremer M, Manzini G, Hristov B,
Polychronidis G, Mokry T, Sommer CM, Mehrabi A, Weitz J, Büchler MW
and Schemmer P: Impact of neoadjuvant chemotherapy on hypertrophy
of the future liver remnant after associating liver partition and
portal vein ligation for staged hepatectomy. J Am Coll Surg.
221:717–728.e1. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Torres OJ, Fernandes ES, Oliveira CV, Lima
CX, Waechter FL, Moraes-Junior JM, Linhares MM, Pinto RD, Herman P
and Machado MA: Associating liver partition and portal vein
ligation for staged hepatectomy (ALPPS): The Brazilian experience.
Arq Bras Cir Dig. 26:40–43. 2013. View Article : Google Scholar : PubMed/NCBI
|