Introduction
Bladder cancer is one of the most frequent
malignancies in the urinary tract, with an estimated 429,800 new
cases and 165,100 deaths occurring each year worldwide (1). The most common histologic type of
bladder cancer in China, America and Europe is urothelial carcinoma
(2). Although ~70% of urothelial
carcinoma is diagnosed as non-muscle invasive with a favourable
prognosis, ~40% of these patients will progress to muscle invasive
with a median survival of 15 months when metastatic disease
develops (3). Metastatic disease is
resistant to conventional cancer therapy, and the low cure rate in
large part is due to development of multidrug resistance (4). Novel approaches such as immunotherapy
are currently under investigation (5).
Human epidermal growth factor receptor (HER)1/EGFR
and HER2 are implicated in the carcinogenesis of several
malignancies (6,7). They play critical roles in
angiogenesis, cell growth, and survival signalling in bladder
cancer, and their alterations are usually associated with poor
prognosis (8,9). Therapeutic antibodies and inhibitors
of the EGFR or HER2 signalling pathway have shown encouraging
results in the treatment of breast and colorectal cancer (10,11).
The success of anti-HER therapy in other cancers has led to its
attempt in bladder cancer clinical trials; however, the benefits
have not been fully achieved (12–15).
Therefore, an alternative approach to improve the current strategy
for bladder cancer is urgently needed.
One advancement is the use of bispecific antibodies
(Bi-Abs), redirecting immune cells to tumour cells by having two
different antigen binding sites, with one recognizing the tumour
cells and the other recognizing the immune cells, usually T and NK
cells. Researchers have engaged in taking advantage of immune cells
to kill tumours for decades. Treatment of non-muscle-invasive
bladder cancer with Bacillus Calmette-Guerin (BCG) demonstrated a
remarkable reduction in recurrence by activating both the innate
and adaptive immune systems (16).
In 2016, and 2017, immunotherapy with programmed cell death 1/PD-1
ligand (PD-1/PD-L) immune checkpoint blockade to recover T-cell
potency made a significant leap forward for patients with advanced
or metastatic bladder cancer (17–19).
Administration of Bi-Abs is also a strategy for enduring T-cell
antitumour potency. Recently, phase I clinical trials with
HER2Bi-Ab armed activated T cells (ATCs) have shown encouraging
results in women with metastatic breast cancer and in men with
metastatic castrate-resistant prostate cancer (20,21).
In the present study, ATCs were armed with Bi-Abs to
target bladder cancer cells and their chemotherapeutic
drug-resistant counterparts. Human bladder urothelial carcinoma
cells were demonstrated to express high levels of EGFR and HER2
protein. A clinically approved anti-CD3 antibody was chemically
conjugated with either an anti-EGFR or anti-HER2 antibodies. The
anti-CD3×anti-EGFR bispecific antibody (EGFRBi-Ab) or
anti-CD3×anti-HER2 bispecific antibody (HER2Bi-Ab) was then used to
direct the ATCs to kill bladder cancer cells and their
chemotherapeutic drug-resistant counterparts.
Materials and methods
Cell culture
The human bladder cancer cell line T24 was provided
by the Chinese Academy of Sciences Culture Collection (Beijing).
The drug-resistant bladder cancer cell line T24/DDP was established
by stepwise exposure of T24 cells to escalating concentrations of
cisplatin (Sigma-Aldrich, St. Louis, MO, USA), ranging from 0.01 to
0.60 µg/ml for >6 months (22,23).
The human bladder cancer cell line Pumc-91 was provided by the Cell
Laboratory of Peking Union Medical College Hospital (Beijing). The
drug-resistant cell line was Pumc-91/ADM, which was established by
increasing the dosage of adriamycin gradually, and the final
concentration of adriamycin was 1.0 µg/ml (23–26).
The parental cell lines were cultured in RPMI-1640 medium
supplemented with 10% heat-inactivated foetal bovine serum (FBS),
while drug-resistant cell lines were cultured in the
above-mentioned medium with 18% FBS. Cells were incubated at 37°C
in a standard 5% CO2 cell incubator under a humidified
atmosphere of 95% air. All agents for cell culture were purchased
from Gibco Company (Gaithersburg, MD, USA).
Preparation of activated T cells from
peripheral blood lymphocytes (PBMCs)
PBMCs were separated by Ficoll density gradient
centrifugation from healthy donors supplied by Beijing Blood Bank.
PBMCs were cultured at 1×106/ml in RPMI-1640 medium
supplemented with 10% FBS and 300 ng/ml anti-CD3 monoclonal
antibody (mAb) combined with 600 ng/ml anti-CD28 mAb (both from
eBioscience, San Diego, CA, USA) in the presence of 100 IU/ml
recombinant human IL-2 (PeproTech, Rocky Hill, NJ, USA). Fresh
medium containing fresh interleukin-2 was added every 2 or 3 days,
and cells were cultured for 14 days and then cryopreserved. The
study was performed according to the protocols approved by the
Biomedical Research Ethics Committee of Beijing Shijitan Hospital
of Capital Medical University.
Synthesis of anti-CD3×anti-EGFR
(EGFRBi-Ab) and anti-CD3×anti-HER2 (HER2Bi-Ab) bispecific
antibodies and arming of ATCs
Anti-EGFR (Erbitux®; Merck Serono,
Darmstadt, Germany) or anti-HER2 (Herceptin®; Roche,
Indianapolis, IN, USA) was reacted with sulfo-SMCC, and anti-CD3
mAb (OKT3; eBioscience) was reacted with Traut's reagents using a
previously described method (27–29).
Cryopreserved ATCs were thawed, armed with EGFRBi-Ab or HER2Bi-Ab
at a concentration of 50 ng/106 cells at room
temperature for 30 min, and washed to eliminate unbound antibodies.
ATCs preincubated with the combination of Erbitux® (50
ng/106 cells), Herceptin® (50
ng/106 cells), and OKT3 (50 ng/106 cells)
were used as control unarmed ATCs.
FlowJo cytometric analysis
To detect the expression of EGFR or HER2 on the cell
surface, bladder cancer cells (1×106) were incubated for
30 min on ice with Erbitux® or Herceptin®,
followed by staining with anti-human-IgG-PE (BioLegend, San Diego,
CA, USA). To detect EGFRBi-Ab or HER2Bi-Ab bound to bladder cancer
cells, T24 cells were first incubated with EGFRBi-Ab or HER2Bi-Ab
for 30 min. The combination of Erbitux®,
Herceptin® with OKT3 was used as the negative control.
Then, FITC-labelled goat anti-mouse IgG2a was used to detect the
anti-CD3 moiety of the Bi-Ab. To examine the population of effector
cells, ATCs were incubated with anti-human CD3-FITC, anti-human
CD4-PE, anti-human CD8-APC and anti-human CD56-APC. To detect CD69
expression on ATCs, floating cells from T24 and ATC co-cultures
were incubated with anti-human CD69-PE and anti-human CD3-FITC. The
anti-human CD3-FITC, anti-human CD69-PE, anti-human CD4-PE,
anti-human CD8-APC, anti-human CD56-APC, and anti-mouse IgG2a-PE
secondary antibodies were from eBioscience. The cells were assayed
with a Guava EasyCyte flow cytometer (Guava Technologies, Hayward,
CA, USA), and data analysis was carried out with FlowJo Software
Version 7.6.1 (Tree Star, Inc., Ashland, OR, USA).
In vitro cytotoxicity assay
Cytotoxicity assays were performed using a lactate
dehydrogenase (LDH) activity assay kit (Sigma-Aldrich) according to
the manufacturer's instructions, and real-time images were captured
at a magnification of ×200 with an optical microscope (Olympus,
Tokyo, Japan). Target cells were seeded in triplicate in 96-well
microplates at 1×104/well before the addition of
EGFRBi-Ab-armed, HER2Bi-Ab-armed or unarmed ATCs at the indicated
effector-to-target ratio (E/T). Effector cells and tumour cells
were allowed to interact at 37°C for 18 h. Then, supernatants were
collected, and LDH activity assays were performed to evaluate the
death of target tumour cells at E/T ratios of 5:1 and 10:1.
ELISA assay
Target cells were seeded in triplicate in 96-well
microplates at 1×104/well before the addition of
EGFRBi-Ab-armed, HER2Bi-Ab-armed, or unarmed ATCs at E/T of 10:1.
Effector cells and tumour cells were allowed to interact at 37°C
for 18 h. Then, supernatants were collected, and the production of
IFN-γ, TNF-α and IL-2 was quantified with a human cytokine ELISA
kit (eBioscience) according to the manufacturer's instructions.
Statistical analyses and
reproducibility
All experiments were repeated three times. Data were
analysed using GraphPad Prism 5 software and are presented as the
mean ± SD. Unpaired Student's t-test (two-tailed) or the
Mann-Whitney test was used for comparison of two groups where
appropriate. One-way analysis of variance (ANOVA) followed by
Dunnett's post hoc test was used for multiple comparisons.
P<0.05 was considered statistically significant. Numbers with a
significant difference from a control are denoted by an asterisk in
the figures.
Results
Confirmation of EGFR and HER2
expression on human bladder cancer cells
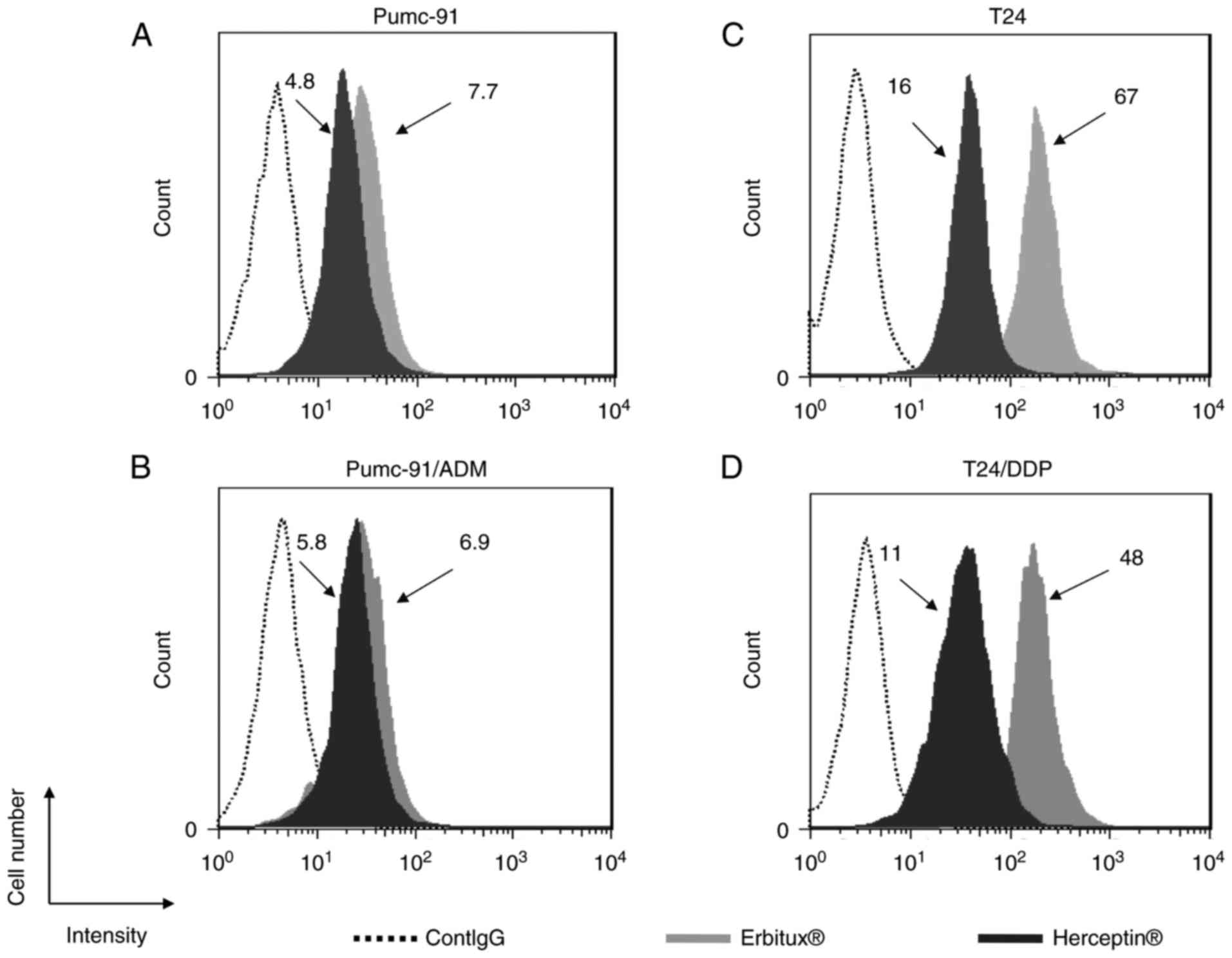
The surface expression of EGFR and HER2 on human
muscle-invasive bladder cancer cells, including Pumc-91 and T24
cells, and their chemotherapeutic drug-resistant counterparts,
Pumc-91/ADM and T24/DDP, were assessed by flow cytometry. The
drug-resistant characteristics of Pumc-91/ADM and T24/DDP were
confirmed by MTT assay, reverse transcription polymerase chain
reaction and flow cytometry in our previous studies (22–25).
As shown in Fig. 1, mean
fluorescence intensity (MFI) values obtained from humanized
anti-human EGFR Ab (Erbitux®) or anti-human HER2Ab
(Herceptin®) staining divided by control antibody
staining are indicated, and high expression of EGFR and HER2 was
detected in all human bladder cancer cells.
Preparation and characterization of
EGFRBi-Ab, HER2Bi-Ab and ATCs
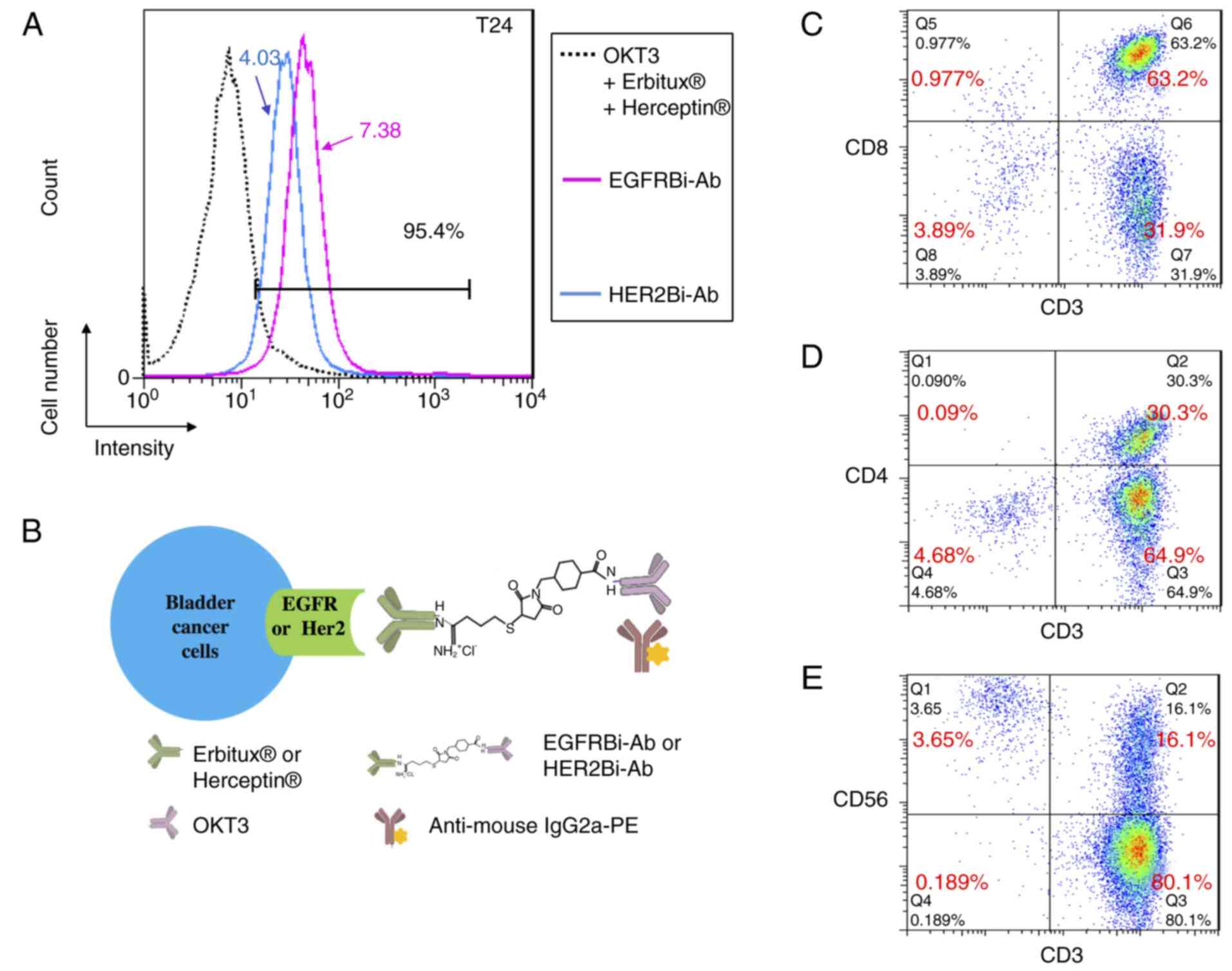
We next constructed two types of bispecific
antibodies that recognized both CD3 on T cells and EGFR or HER2 on
bladder cancer cells. Erbitux® or Herceptin®
antibody was chemically hetero-conjugated to OKT3 and named
EGFRBi-Ab or HER2Bi-Ab (27–29).
The binding specificity of EGFRBi-Ab and HER2Bi-Ab was tested
against EGFR and HER2, respectively. T24 bladder cancer cells were
stained with EGFRBi-Ab or HER2Bi-Ab, and then an
anti-mouse-IgG2a-FITC was added to detect the CD3 moiety of the
Bi-Abs. Only functional bispecific antibody was able to bind to T24
cells and be detected through mouse origin OKT3 by anti-mouse IgG2a
secondary antibody. In the control where Erbitux®,
Herceptin® and OKT3 were used without conjugation,
Erbitux® and Herceptin® were able to bind to
T24 cells but could not be recognized by the anti-mouse IgG2a
secondary antibody. As shown in Fig.
2A, positively stained cells were detected in >95% of the
T24 population with a MFI of 7.38 or 4.03 for EGFRBi-Ab or
HER2Bi-Ab staining, respectively. The scheme for flow
cytometry-based binding assays for EGFRBi-Ab and HER2Bi-Ab is
demonstrated in Fig. 2B. Moreover,
evaluation of the binding of Bi-Ab to CD3+ cells has
been previously shown by a similar method (27–29).
To produce a sufficient number of effector cells,
PBMCs from buffy coat were stimulated by the combination of ant-CD3
mAb with anti-CD28 mAb in the presence of IL-2 for 14 days as
described in Materials and methods, then the effector cells were
quantitatively analysed by FACS. As shown in Fig. 2C-E, the cell population contained
almost 95–96% CD3+ cells among which there were ~63.2%
CD3+CD8+ (Fig.
2C) and 30.3% CD3+CD4+ cells (Fig. 2D). Regarding the CD3−
population, most of them were CD56-positive (Fig. 2E). Overall, these data suggested
that the effector cells were mainly composed of ATCs and a small
population of NK cells.
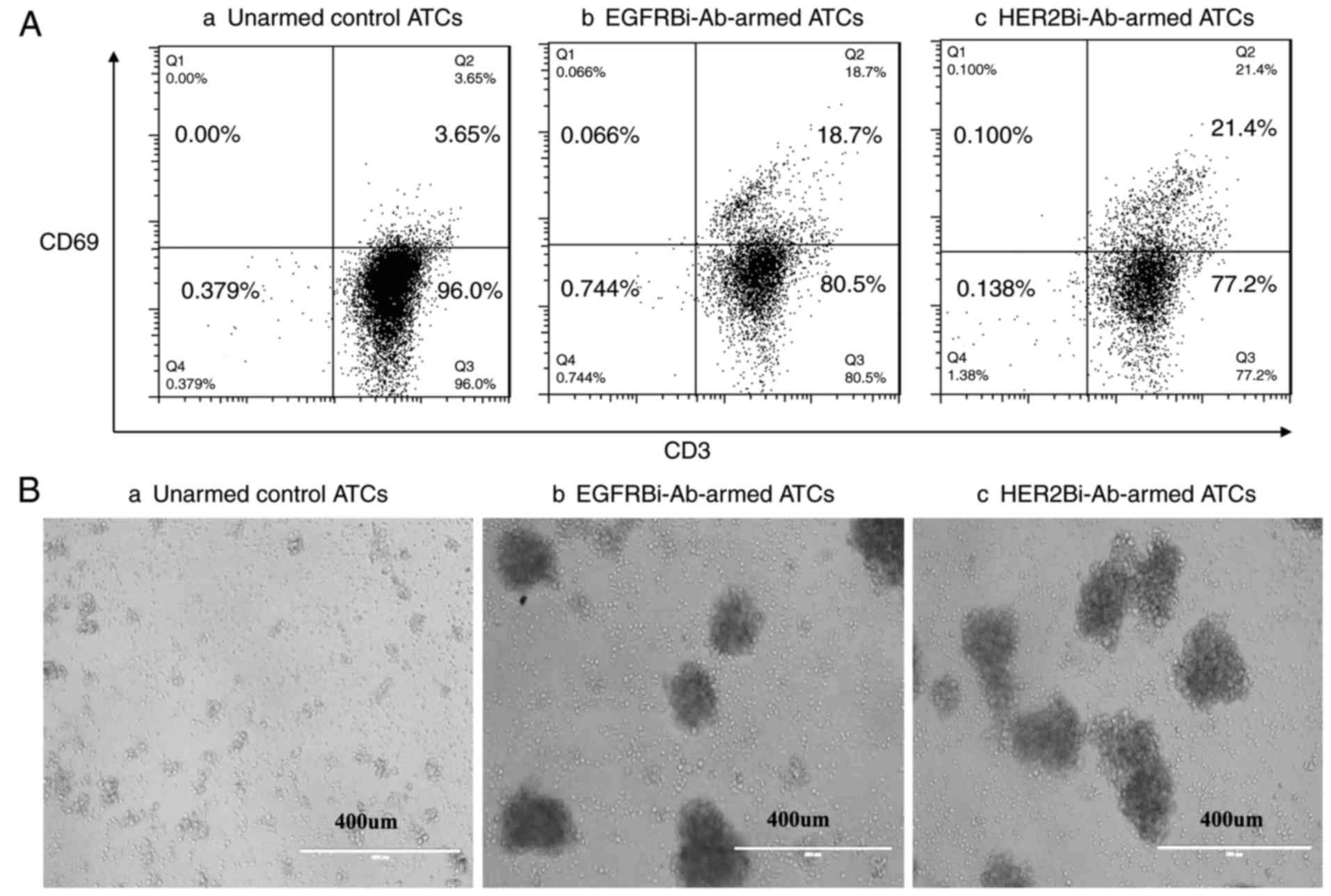
Activation of EGFRBi-Ab- or
HER2Bi-Ab-armed ATCs by human bladder cancer cells
Based on our previous experiments (27–29),
we chose 50 ng/106 cells as the concentration of
EGFRBi-Ab or HER2Bi-Ab with which to arm ATCs for all subsequent
experiments, and ATCs mixed with individual OKT3,
Erbitux® and Herceptin® were used as unarmed
control ATCs. The antitumour effects of EGFRBi-Ab- or
HER2Bi-Ab-armed ATCs on T24 cells were tested at an effector/target
(E/T) ratio of 10:1. After 18 h of incubation of T24 cells with
EGFRBi-Ab-armed ATCs or HER2Bi-Ab-armed ATCs, FACS analysis showed
increased expression of CD69, an activation marker for T cells, in
Bi-Ab-armed ATCs compared with that in their unarmed-ATC
counterparts (Fig. 3A). As shown in
Fig. 3B, real-time images
demonstrated that both EGFRBi-Ab-armed ATCs and HER2Bi-Ab-armed
ATCs, but not unarmed control ATCs aggregated with T24 cells in
culture, clustering around the edge of target cell bulk, which
showed specific activation of EGFRBi-Ab- or HER2Bi-Ab-armed
ATCs.
Cytotoxic effects of EGFRBi-Ab- or
HER2Bi-Ab-armed ATCs on human bladder cancer cells
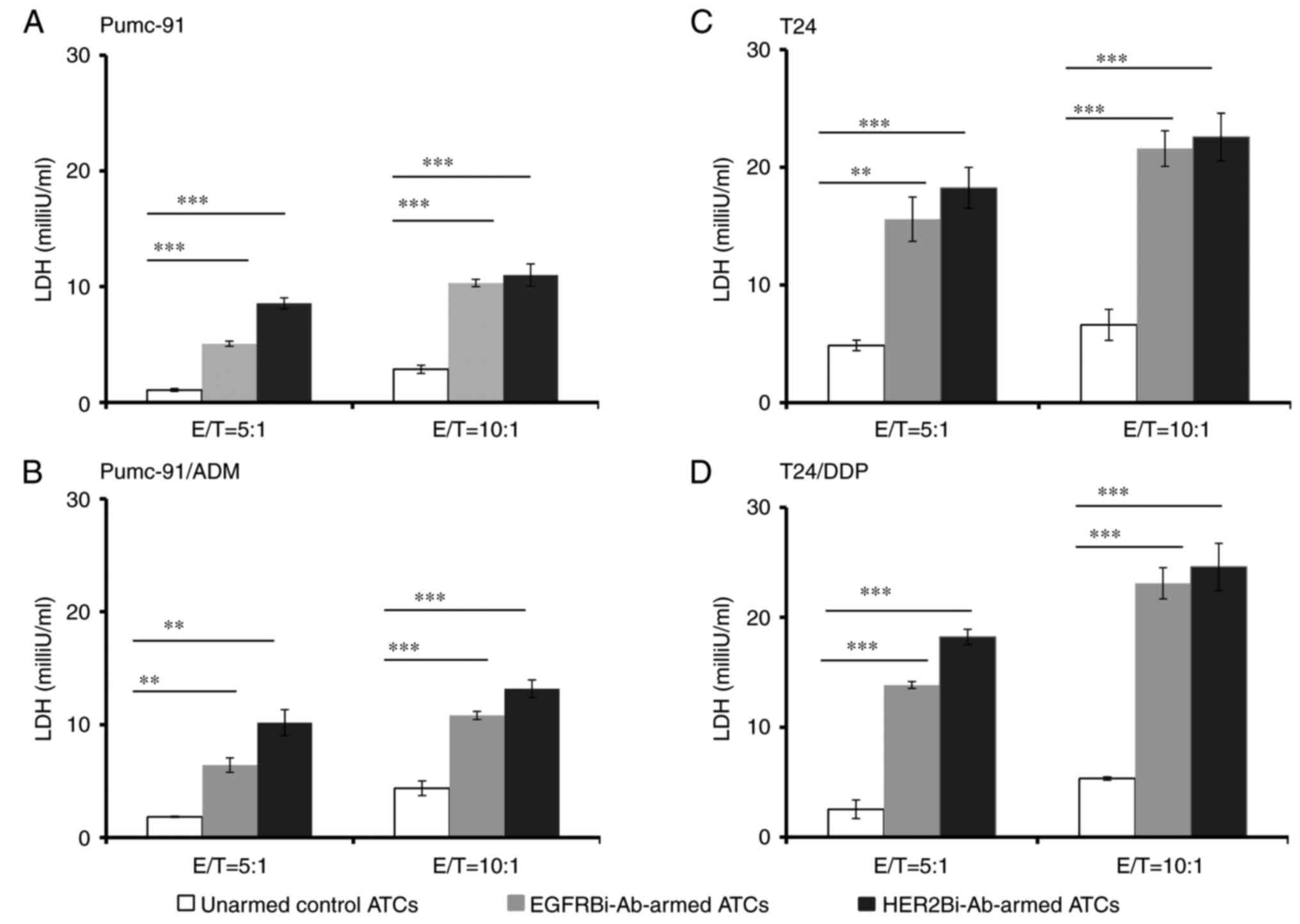
EGFRBi-Ab- or HER2Bi-Ab-armed ATCs were tested for
cytotoxicity on Pumc-91, T24, Pumc-91/ADM and T24/DDP human bladder
cancer cells. Lactate dehydrogenase (LDH) activity assays were
performed to evaluate the death of target bladder cancer cells at
E/T ratios of 5:1 and 10:1. As shown in Fig. 4, after an 18-h incubation with
EGFRBi-Ab-armed ATCs or HER2Bi-Ab-armed ATCs, the concentration of
LDH with armed effectors was significantly greater than that with
unarmed effectors in all the bladder cancer cells, indicating the
specific cytotoxicity of EGFRBi-Ab- or HER2Bi-Ab-armed ATCs on
these cells.
Cytotoxic effects of EGFRBi-Ab- or
HER2Bi-Ab-armed ATCs on human bladder cancer cells with cytokine
production
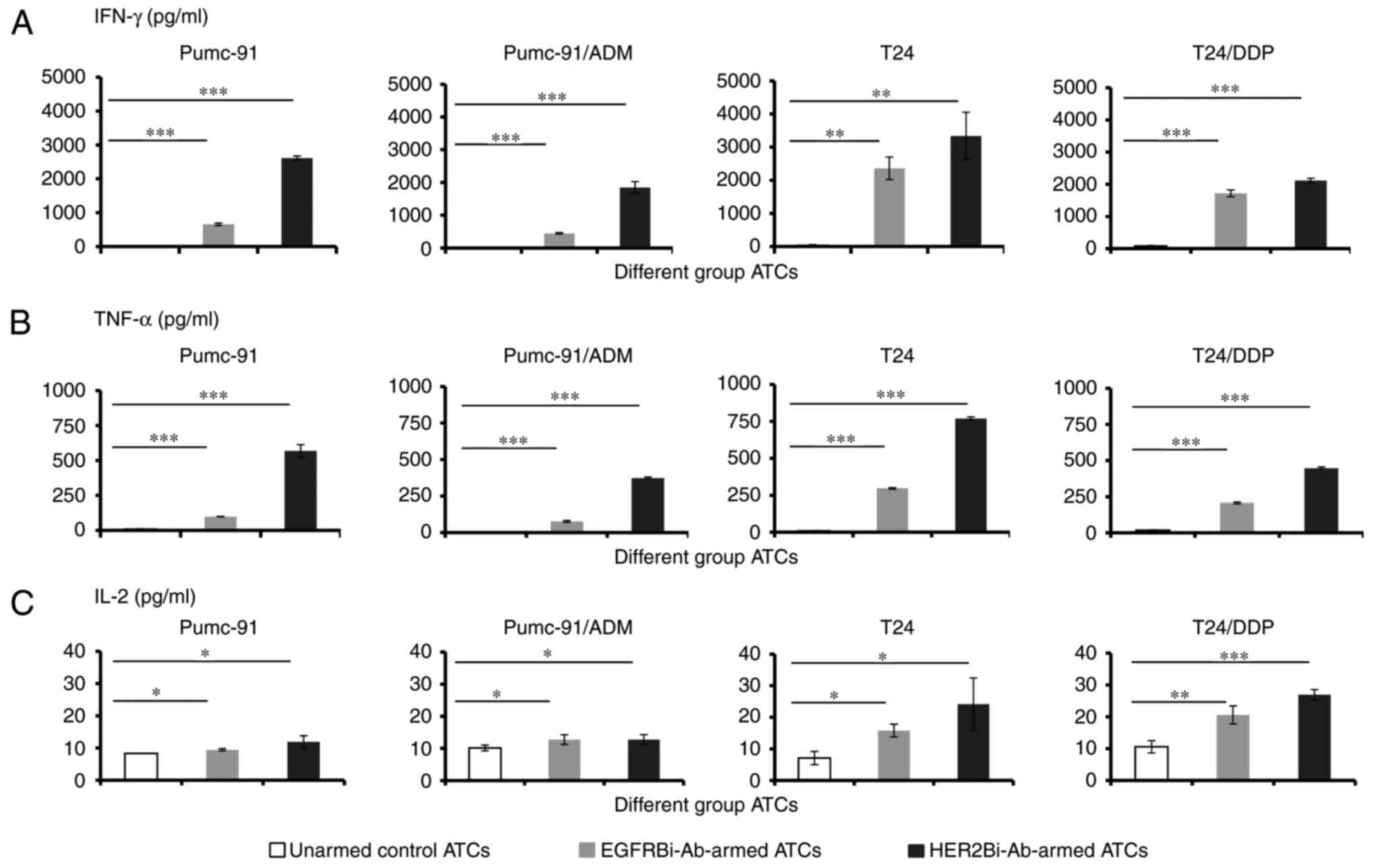
To analyse the levels of T cell-derived cytokines
involved in cytotoxicity, cell supernatants were analysed for
IFN-γ, TNF-α and IL-2 production at E/T ratio of 10:1. As shown in
Fig. 5, significantly more IFN-γ
(Fig. 5A), TNF-α (Fig. 5B) and IL-2 (Fig. 5C) secretion was observed from
EGFRBi-Ab- or HER2Bi-Ab-armed ATCs than from their unarmed control
ATC counterparts when ATCs were co-cultured with Pumc-91, T24,
Pumc-91/ADM or T24/DDP.
Discussion
Due to development of multidrug resistance,
metastases of bladder cancer are resistant to conventional cancer
therapy. As large numbers of activated T cells can be produced
ex vivo, and as mAbs specific for a tumour surface protein
have become available, Bi-Abs have shown encouraging antitumour
effects in both experimental and clinical studies in recent years
(20,21,27–32).
Bi-Abs, usually comprising an anti-CD3 mAb hetero-conjugated to a
different mAb specific to a selected tumour-associated antigen
(TAA), will empower each TAA-specific T cell to retarget tumour
cells. HER2 and EGFR are ideal targets in antibody-based
therapeutic strategies for tumours especially breast and colorectal
cancer (10,11). Therefore, targeting HER2 or EGFR
appears to be a reasonable way to treat bladder cancer.
In the present study, we examined the expression of
EGFR and HER2 on human muscle-invasive bladder cancer cells and
their chemotherapeutic drug-resistant counterparts. Co-expression
of HER2 and EFGR, which suggests activation of both the
AKT/PTEN/mTOR and RAS/MEK/ERK pathways, has been reported with
worse prognosis in several types of cancer, including bladder
cancer (8,33). Synergy among different signaling
pathways is essential for more aggressive disease and therefore
deserves further consideration. We further tested whether EGFR or
HER2 is a useful target for the development of a Bi-Ab therapy in
bladder cancer, and evaluated the antitumour effects of Bi-Ab-armed
ATCs. In vitro cytotoxicity assays demonstrated that
EGFRBi-Ab-armed or HER2Bi-Ab-armed ATCs displayed significant
cytotoxic activity against bladder cancer cells, whereas neither
the anti-EGFR antibody nor the anti-HER2 antibody alone had an
inhibitory effect on them (data not shown). Moreover, our
investigation showed that Bi-Ab-armed ATCs expressed higher levels
of activating marker CD69 and secreted more IFN-γ, TNF-α and IL-2
than did unarmed ATCs.
The present study demonstrated that compared with
control unarmed ATCs, those armed with either EGFRBi-Ab or
HER2Bi-Ab released high levels of LDH, indicating that armed ATCs
mediated specific cytotoxicity against bladder cancer cells. These
results showed that T-cell cytotoxicity was dependent upon the
engagement of EGFR or HER2 via Bi-Ab linkage. Indeed, at the E/T
ratio of 10:1, 50 ng Bi-Ab per 106 ATCs showed
remarkable LDH release against tumour cells after an 18-h
incubation, whereas anti-EGFR/anti-HER2 antibody had no inhibitory
effect at the concentration of 10 µg/ml after a 72-h incubation
(data not shown). Moreover, the present study supported that arming
ATCs with Bi-Abs circumvented the requirement for major
histocompatibility complex antigen recognition by ATCs.
HER2Bi-Ab-armed ATCs could not kill CD3−HER2−
K562 cells, demonstrating the specificity of the HER2Bi-Ab
(28,29). Moreover, effector cells armed with
EGFRBi-Ab, but not with HER2Bi-Ab could kill
EGFR+HER2− U87-MG cells (27).
Our results showed that ATCs armed with either
EGFRBi-Ab or HER2Bi-Ab released high levels of IFN-γ, TNF-α and
IL-2 upon incubation with bladder cancer cells. The increased
cytokine secretion indicated that the ATCs were reactivated when
encountering tumour cells. IFN-γ and TNF-α secreted by Bi-Ab-armed
ATCs are directly tumouricidal and can also activate endogenous
immune cells in vivo, counteracting tumour-derived
suppression. Moreover, based on flow cytometry assays, both
HER2Bi-Ab-armed ATCs and EGFRBi-Ab-armed ATCs expressed higher
levels of CD69 than unarmed-ATC counterparts. CD69, a marker of
early T-cell activation, acts as a costimulatory molecule enhancing
T-cell responses following TCR-ligand interaction (34). Our real-time images also revealed
that armed ATCs but not unarmed control ATCs aggregated with
bladder cancer cells in culture, clustering around the edge of the
target cell bulk, indicating the specific activation of EGFRBi-Ab-
or HER2Bi-Ab-armed ATCs. In several phase I clinical trials,
patients infused with HER2Bi-Ab-armed ATCs exhibited elevated
levels of cytokines in their serum, suggesting that armed ATC
administration stimulated the endogenous immunity to develop
antitumour activity (20,21).
In conclusion, both EGFR and HER2 appear to be
suitable targets for T cell-mediated immunotherapy against bladder
cancer including chemotherapeutic drug-resistant bladder cancer.
EGFRBi-Ab- or HER2Bi-Ab-armed ATCs may provide a promising approach
for bladder cancer in the future.
Acknowledgements
The present study was funded by grants from the
National Nature Science Foundation of China (no. 31400754), Beijing
Key Laboratory of Urinary Cellular Molecular Diagnostics
(Z151100001615060), Beijing Natural Science Foundation (no.
7172106), Beijing Municipal Administration of Hospitals' Ascent
Plan (DFL20150701) and Beijing Shijitan Hospital Foundation
(2015C-12).
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Torre LA, Bray F, Siegel RL, Ferlay J,
Lortet-Tieulent J and Jemal A: Global cancer statistics, 2012. CA
Cancer J Clin. 65:87–108. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Pang C, Guan Y, Li H, Chen W and Zhu G:
Urologic cancer in China. Jpn J Clin Oncol. 46:497–501. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Von der Maase H, Sengelov L, Roberts JT,
Ricci S, Dogliotti L, Oliver T, Moore MJ, Zimmermann A and Arning
M: Long-term survival results of a randomized trial comparing
gemcitabine plus cisplatin, with methotrexate, vinblastine,
doxorubicin, plus cisplatin in patients with bladder cancer. J Clin
Oncol. 23:4602–4608. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Krishna R and Mayer LD: Multidrug
resistance (MDR) in cancer. Mechanisms, reversal using modulators
of MDR and the role of MDR modulators in influencing the
pharmacokinetics of anticancer drugs. Eur J Pharm Sci. 11:265–283.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Carneiro BA, Meeks JJ, Kuzel TM, Scaranti
M, Abdulkadir SA and Giles FJ: Emerging therapeutic targets in
bladder cancer. Cancer Treat Rev. 41:170–178. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Appert-Collin A, Hubert P, Crémel G and
Bennasroune A: Role of ErbB receptor in cancer cell migration and
invasion. Front Pharmacolo. 6:2832015.
|
|
7
|
Smolensky D, Rathore K and Cekanova M:
Molecular targets in urothelialcancer: Detection, treatment, and
animal models ofbladder cancer. Drug Des Devel Ther. 10:3305–3322.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Koletsas N, Koletsa T, Choidas S,
Anaqnostopoulos K, Touloupidis S, Zaramboukas T, Raptou G,
Papadopoulos N and Lambropoulou M: Immunohistochemical
investigation of HER/AKT/mTOR pathway and cellular adhesion
molecules in urothelial carcinomas. Patholog Res Int.
2017:67941502017.PubMed/NCBI
|
|
9
|
Zhao J, Xu W, Zhang Z, Song R, Zeng S, Sun
Y and Xu C: Prognostic role of HER2 expression in bladder cancer: A
systematic review and meta-analysis. Int Urol Nephrol. 47:87–94.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ross JS, Slodkowska EA, Symmans WF,
Pusztai L, Ravdin PM and Hortobagyi GN: The HER-2 receptor and
breast cancer: Ten years of targeted anti-HER-2 therapy and
personalized medicine. Oncologist. 14:320–368. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lo Nigro C, Ricci V, Vivenza D, Granetto
C, Fabozzi T, Miraqlio E and Merlano MC: Prognostic and predictive
biomarkers in metastatic colorectal canceranti-EGFR therapy. World
J Gastroenterol. 22:6944–6954. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hussain M, Daignault S, Agarwal N, Grivas
PD, Siefker-Radtke AO, Puzanov I, MacVicar GR, Levine EG, Srinivas
S, Twardowski P, et al: A randomized phase 2 trial of
gemcitabine/cisplatin with or without cetuximab in patients with
advanced urothelial carcinoma. Cancer. 120:2684–2693. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Philips GK, Halabi S, Sanford BL, Bajorin
D and Small EJ; Cancer and Leukaemia Group B, : A phase II trial of
cisplatin, fixed dose-rate gemcitabine and gefitinib for advanced
urothelial tract carcinoma: Results of the Cancer and Leukaemia
Group B 90102. BJU Int. 101:20–25. 2008.PubMed/NCBI
|
|
14
|
Oudard S, Culine S, Vano Y, Goldwasser F,
Théodore C, Nguyen T, Voog E, Banu E, Vieillefond A, Priou F, et
al: Multicentre randomized phase II trial of gemcitabine +
platinum, with or without trastuzumab, in advanced or metastatic
urothelial carcinoma overexpressing Her2. Eur J Cancer. 51:45–54.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Powles T, Huddart RA, Elliott T, Sarker
SJ, Ackerman C, Jones R, Hussain S, Crabb S, Jagdev S, Chester J,
et al: Phase III, doubled-blind, randomized trial that compared
maintenance lapatinib versus placebo after first-line chemotherapy
in patients with human epidermal growth factor receptor
1/2-positive metastatic bladder cancer. J Clin Oncol. 35:48–55.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Wu Y, Enting D, Rudman S and Chowdhury S:
Immunotherapy for urothelial cancer: From BCG to checkpoint
inhibitors and beyond. Expert Rev Anticancer Ther. 15:509–523.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Rosenberg JE, Hoffman-Censits J, Powles T,
van der Heijden MS, Balar AV, Necchi A, Dawson N, O'Donnell PH,
Balmanoukian A, Loriot Y, et al: Atezolizumab in patients with
locally advanced and metastatic urothelial carcinoma who have
progressed following treatment with platinum-based chemotherapy: A
single-arm, multicentre, phase 2 trial. Lancet. 387:1909–1920.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Sharma P, Callahan MK, Bono P, Kim J,
Spiliopoulou P, Calvo E, Pillai RN, Ott PA, de Braud F, Morse M, et
al: Nivolumab monotherapy in recurrent metastatic urothelial
carcinoma (CheckMate 032): A multicentre, open-label, two-stage,
multi-arm, phase 1/2 trial. Lancet Oncol. 17:1590–1598. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Bellmunt J, De Wit R, Vaughn DJ, Fradet Y,
Lee JL, Fong L, Vogelzang NJ, Climent MA, Petrylak DP, Choueiri TK,
et al: Pembrolizumab as second-line therapy for advanced urothelial
carcioma. N Eng J Med. 376:1015–1026. 2017. View Article : Google Scholar
|
|
20
|
Lum LG, Thakur A, Al-Kadhimi Z, Colvin GA,
Cummings FJ, Legare RD, Dizon DS, Kouttab N, Maizei A, Colaiace W,
et al: Targeted T-cell therapy in stage IV breast cancer: A phase I
clinical trial. Clin Cancer Res. 21:2305–2314. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Vaishampayan U, Thakur A, Rathore R,
Kouttab N and Lum LG: Phase I study of anti-CD3 × anti-Her2
bispecific antibody in metastatic castrate resistant prostate
cancer patients. Prostate Cancer. 2015:2851932015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Zhao M, Zhang M and Ma P: Establishment of
cisplatin-multi drug resistance cell line of human bladder cancer
T24 and its biological characteristics. Immun Clin Med. 22:338–341.
2015.(In Chinese).
|
|
23
|
Wang S, Lei T and Zhang M: The reversal
effect and its mechanisms of tetramethylpyrazine on multidrug
resistance in human bladder cancer. PLoS One. 11:e01577592016.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Zhang M, Jin S and Zhang M: The
establishment and biological characteristics evaluation of human
multidrug-resistant bladder cancer Pumc-91/ADM cell line. J Med
Res. 38:70–72. 2009.(In Chinese).
|
|
25
|
Wang S, Meng Q, Xie Qi and Zhang M: Effect
and mechanism of resveratrol on drug resistance in human bladder
cancer cells. Mol Med Rep. 15:1179–1187. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Xiu W, Ma J, Lei T, Zhang M and Zhou S:
Immunosuppressive effect of bladder cancer on function of dendritic
cells involving of Jak2/STAT3 pathway. Oncotarget. 7:63204–63214.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Ma P, He Q, Li W, Li X, Han H, Jin M, Liu
C, Tao H, Ma J and Gao B: Anti-CD3 × EGFR bispecific antibody
redirects cytokine-induced killer cells to glioblastoma in vitro
and in vivo. Oncol Rep. 34:2567–2575. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Han H, Ma J, Zhang K, Li W, Liu C, Zhang
Y, Zhang G, Ma P, Wang L, Zhang G, et al: Bispecific anti-CD3 ×
anti-HER2 antibody mediates T cell cytolytic activity to
HER2-positive colorectal cancer in vitro and in vivo. Int J Oncol.
45:2446–2454. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Ma J, Han H, Liu D, Li W, Feng H, Xue X,
Wu X, Niu G, Zhang G, Zhao Y, et al: HER2 as a promising target for
cytotoxicity T cells in human melanoma therapy. PLoS One.
8:e732612013. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Ma J, Ma P, Zhao C, Xue X, Han H, Liu C,
Tao H, Xiu W, Cai J and Zhang M: B7-H3 as a promising target for
cytotoxicity T cell in human cancer therapy. Oncotarget.
7:29480–29491. 2016.PubMed/NCBI
|
|
31
|
Lum LG and Thakur A: Targeting T cells
with bispecific antibodies for cancer therapy. BioDrugs.
25:365–379. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Bhutani D and Lum LG: Activated T cells
armed with bispecific antibodies killtumor targets. Curr Opin
Hematol. 22:476–483. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Friedman M, Lindström S, Ekerljumg L,
Andersson-Svahn H, Carlsson J, Brismar H, Gedda L, Frejd FY and
Ståhl S: Engineering and characterization of a bispecific HER2 ×
EGFR-binding affibody molecule. Biotechnol Appl. Biochem.
54:121–131. 2009.
|
|
34
|
Sathaliyawala T, Kubota M, Yudanin N,
Turner D, Camp P, Thome JJ, Bickham KL, Lerner H, Goldstein M,
Sykes M, et al: Distribution and compartmentalization of human
circulating and tissue-resident memory T cell subsets. Immunity.
38:187–197. 2013. View Article : Google Scholar : PubMed/NCBI
|