Introduction
Transvaginal sonography, hysteroscopy and magnetic
resonance (MR) imaging are diagnostic tools for intrauterine
abnormalities (1). Hysteroscopy
is a mainstay diagnostic method for women with an abnormal uterine
cavity and bleeding (2,3). Traditionally, hysteroscopy often
requires the use of mechanical or pharmaceutical dilatations of the
cervix before this procedure under local or general anesthesia in
the operating room (4). Although
this is considered a safe procedure, patients are at risk of
developing potential complications, such as bleeding, perforation,
infection, fluid overload, incomplete resection and intrauterine
adhesions (2). Therefore, very
few gynecologists perform hysteroscopy in an outpatient setting.
Recent advances in technology and improved techniques have turned
hysteroscopy into a common outpatient procedure which can be
performed in an office setting (outpatient hysteroscopy or office
hysteroscopy) (3). Outpatient
hysteroscopy is a minimally invasive procedure and offers a direct
visualization of the endometrial cavity (5). No anesthetic or local anesthesia
allows the use of outpatient settings, without taking the patient
to the operating room (6). The
number of outpatient hysteroscopy procedures is increasing
(6).
The authors have previously developed an ultrathin
fiberscopic imaging system for laser surgery that may be an
important instrument for clinical use during office-based
hysteroscopy (7). This device
consists of a custom 1.1 mm in diameter flexible fiberscope and
ytterbium laser-supported ablation system (composite-type optical
fiberscope) to achieve accurate laser irradiation for minimally
invasive procedures of intrauterine disease (7). In the present study, the authors
further developed an optical ultrathin hysterofiberscopic imaging
system with a flexible fiberscope (0.8 mm in diameter) for the
diagnosis of intrauterine abnormalities. The novelty of this method
concerns the development of the slimmest fiber hysteroscope. In
consequence, its use does not require cervical dilatation and
anesthesia which causes discomfort, and is a convenient and
patient-friendly technique. In addition, recent advances and the
widespread availability of smartphones render the utility of this
technology practical and promising in medicine. The smartphone
alone allows for image acquisition, image capture, video capture,
image storage and projection. A smartphone replaces the camera and
video receiver box, and no separate video receiver box is required.
This study provides an initial report of a novel docking system
that optimizes the coupling of a smartphone, the Apple iPhone 6S™,
with an office diagnostic, small-diameter hysterofiberscopy,
‘Hysmartscopy’ (a smart hysterofiberscopy).
The aim of this study was to evaluate the image
quality for the diagnosis of intrauterine abnormalities and to
assess the feasibility and safety of the Hysmartscopy system.
Materials and methods
System setup and design.
The authors of this study developed an optical
flexible fiberscope system for the diagnosis of intrauterine
abnormalities. The smartphone-based intrauterine imaging system was
a flexible fiberscope (0.8 mm in diameter) coupled with an Apple
iPhone 6S™ (Apple Inc.) in camera mode. The Hysmartscopy system
functions on the principles of a direct fiberscope and exploits the
autofocus capability of the iPhone camera. For maximal image
quality, this system provides a centered image on the iPhone camera
with an 8X optical zoom. It is an ultrathin and light weight,
simple system that turns a smartphone into a portable camera
capable of capturing and uploading high-quality images and videos
of the intrauterine pathologies via the Hysmartscopy system. An
overview of the whole system is illustrated in Fig. 1. The information of the
Hysmartscope is as follows: Optical system [field of view (90̊),
direction of view (0̊ forward viewing)], insertion portion [outer
diameter (0.8 mm), total length (210 mm)], and instrument channel
[minimum visible distance (3 mm)]. When Hysmartscopy with a 90̊
field of view was used at a focal distance of 5 mm, there was no
marked difference in resolution between Hysmartscopy and
conventional hysteroscopy. Fluid (saline) is instilled
transcervically into the uterine cavity to provide clear
visualization of uterine intracavitary pathologies. The examiners
can transmit the images to a remote endoscopic specialist through a
web application.
Image and color resolution.
The image resolution (line pairs/mm) of the
Hysmartscopy-coupled mobile device was evaluated by imaging a 1951
United States Air Force Contrast Resolution Chart Target (Edmund
Industrial Optics™). The Hysmartscope was held 5-10 mm above the
resolution target, and images were recorded. The color
resolution/quality was evaluated using the Munsell ColorChecker
Chart. The colors included the following: Red, orange, yellow,
green, blue, light purple and purple. The images were reviewed and
evaluated by expert endoscopists, residents and medical students. A
total of 34 evaluators (13 expert endoscopists, 10 residents and 11
medical students) were asked to rate the resolution, brightness,
color and overall image quality from 1 (very poor, inadequate for
any diagnostic purpose) to 5 (very good, ideal quality) on a
5-point Likert scale.
Proof of concept pilot study.
The study protocol was in agreement with the
Helsinki Declaration for Ethical Medical Research (no. 874).
Research was performed after obtaining approval from the Nara
Medical University Institutional Review Board (IRB). A written
informed consent was signed by each participant following a
detailed explanation of the objectives and protocol of the study.
This pilot study was conducted at the Department of Gynecology of
Nara Medical University Hospital from February, 2015 to February,
2019. Hysmartscopy was performed based on the following 4
indications: i) An abnormal uterine cavity, as suggested by
transvaginal ultrasonography and/or MR imaging; ii) subjects who
underwent pathological diagnosis; iii) prior to surgery; and iv)
not excluding cases with a diagnosis of a uterine malignancy. The
exclusion criteria were as follows: Virginity, cervical stenosis,
cervicovaginal infections, pelvic inflammatory disease and
pregnancy. Demographic records for each individual, including age
at diagnosis, parity, menopausal state, body mass index (BMI), past
medical history, histological diagnosis, grade and stage were all
retrospectively analyzed from the same database.
Diagnostic Hysmartscopy.
Prior to Hysmartscopy, the participants underwent
transvaginal sonography and/or MR imaging. The patient was examined
in the lithotomy position. A baseline transvaginal ultrasound
examination of the pelvis was performed using GE Healthcare Voluson
S6 (General Electric Co.). Hysmartscopy was performed in the early
to middle follicular phase of each menstrual cycle; in women who
experienced irregular cycles or menopause, it was performed at any
time point. The presence of free fluid in the cul-de-sac was
recorded prior to Hysmartscopy to calculate saline retrograde
regurgitation. At first, a flexible fiberscope (0.8 mm in diameter)
was assembled to relay the image onto the Apple iPhone 6S™ in
camera mode. Following preparation and draping, a sterile speculum
was inserted into the vagina, the cervix was visualized and cleaned
with an iodine solution, and the anterior lip was grasped with a
single-toothed tenaculum if required. The subjects underwent
Hysmartscopy without cervical dilatation. A catheter sheath with an
outer diameter of 2.2 mm was inserted transcervically into the
uterine cavity. The flexible fiberscope was inserted through a
catheter sheath and moved through the sheath to the uterine cavity.
Using a 10-ml syringe attached to the catheter, sterile saline
solution of 20 to 50 ml was slowly instilled, and the endometrial
cavity was then observed. The examiner was instructed to hold the
catheter sheath with one hand (with the thumb and second and third
digits) and worked from a comfortable position by aiming through
the screen of the iPhone.
Image evaluation.
Patients were imaged by 1 of 2 expert gynecological
endoscopists (K.I. and H.S.). The uterine cavity was systematically
examined and any observations were stored in electronic medical
records. Acquired images and videos can subsequently be saved in
the local memory and stored via secure server. The diagnostically
important frames were extracted from iPhone videos recorded in
full. The images collected from each patient were reviewed and
evaluated by 2 endoscopists. The evaluators were blinded to the
histological results.
In total, 22 patients requiring a diagnostic
Hysmartscopy for the investigation of intrauterine pathology were
included in this study. Following the Hysmartscopic procedures, all
the patients received surgery, including total hysterectomy (n=7)
or transcervical resection (n=15). As a preliminary evaluation from
February, 2015 to December, 2017 (the first cohort), Hysmartscopy
was performed in a conventional operating room under general
anesthesia on 17 patients (Propofol, n=15; and Sevoflurane, n=2).
The pathological results revealed endometrial benign polyp (n=4),
submucosal fibroids (n=6), endometrial cancer (n=5) and normal
endometrium (n=2). In the second cohort from January, 2018 to
February, 2019, Hysmartscopy was further validated in 5 additional
subjects with endometrial benign polyp (n=3) and submucosal
fibroids (n=2) without anesthesia and cervical dilatation. Finally,
a total of 22 cases were analyzed in this study and these were
divided into 4 groups. These included the endometrial benign polyp
(n=7), submucosal fibroid (n=8), endometrial cancer (n=5) and
normal endometrium (n=2) groups. The patients underwent an
outpatient evaluation. The results of Hysmartscopy and the
pathological reports of endometrial biopsy were compared, and the
diagnostic accuracy of Hysmartscopy for normal endometrium,
endometrial polyps, submucosal fibroids and endometrial cancer was
evaluated. The evaluators were asked to rate the resolution,
brightness, color and overall image quality on a 5-point Likert
scale.
Statistical analysis.
Statistical analyses were performed using SPSS
Statistics version 22 (International Business Machines Corp.). Data
distribution was verified by the Shapiro-Wilk test, presenting that
all cases exhibited normal distribution (data not shown). Age and
BMI among groups were analyzed by one-way ANOVA, followed by
Tukey's honestly significant difference test as a post-hoc test. To
assess nulliparous and premenopausal state among 4 groups, Fisher's
exact test was used. A P-value <0.05 was considered to indicate
a statistically significant difference.
Results
Ex vivo imaging.
Images of the Hysmartscopy system were recorded for
the iPhone camera by imaging the color target and the resolution
target. On average, the quality of the images taken by 13 expert
endoscopists (median, 4.0/5.0 on a 5-point Likert scale; mean,
3.4/5.0), 10 residents (median, 4.0/5.0; mean, 3.7/5.0) and 11
medical students (median, 3.0/5.0; mean, 3.5/5.0) was sufficient to
detect emergent findings, while it is somewhat difficult to detect
the subtle findings (data not shown). For 2 expert endoscopists
(K.I. and H.S.), the photographic quality on a 5-point scale was
ranked 4, ‘somewhat agree’ (data not shown). Thus, the endoscopic
image quality overall was within the diagnostically acceptable
range.
In vivo imaging.
The major clinical and pathological characteristics
are listed in Table I. The age of
the studied patients was 42.9±9.7 years (mean ± standard deviation;
range, 28 to 67 years). Age was higher in subjects with endometrial
cancer when compared to the other subjects, which was statistically
significantly different (P=0.036). In addition, in terms of BMI, no
statistically significant differences were observed between the
groups (P=0.841). In terms of the pre-menopausal state, a
statistically significant difference was found between the
endometrial cancer group and other groups (P=0.001). In total, 4 of
5 patients with endometrial cancer were in the post-menopausal
state. Four cases had a history of gynecological surgery (ovarian
cystectomy, n=3; and myomectomy, n=1). Two had suffered essential
hypertension. One had a history of diabetes (data not shown).
 | Table ICharacteristics of the study
subjects. |
Table I
Characteristics of the study
subjects.
| Baseline
characteristics of the 4 groups (no.) | Endometrial polyp
(n=7) | Submucosal fibroids
(n=8) | Endometrial cancer
(n=5) | Normal endometrium
(n=2) | P-value |
|---|
| | | | EC, G1 (n=3), | | |
| | | | EC, G2 (n=1), | | |
| | | | EC, G3 (n=1) | | |
| FIGO stage | | | IA (n=3) | | |
| | | | IB (n=1) | | |
| | | | IIIA (n=1) | | |
| Age at diagnosis | | | | | 0.036 |
|
Means ±
SD | 38.0±3.27 | 42.3±5.42 | 53.0±15.2 | 37.0±11.3 | |
|
Median
(range) | 37.0 (35-44) | 42.5 (35-52) | 54.0 (28-67) | 37.0 (29-45) | |
| Nulliparous | | | | | 1.000 |
|
Yes | 2 | 2 | 2 | 1 | |
|
No | 5 | 6 | 3 | 1 | |
| Pre-menopause | | | | | 0.001 |
|
Yes | 7 | 8 | 1 | 2 | |
|
No
(post-menopause) | 0 | 0 | 4 | 0 | |
| BMI | | | | | 0.841 |
|
Mean ±
SD | 22.7±3.00 | 21.5±2.80 | 22.8±4.43 | 23.8±7.00 | |
|
Median
(range) | 23.0 (18.6-26.5) | 21.4 (17.8-25.4) | 21.8 (17.9-28.6) | 23.8 (18.8-28.7) | |
Expert reviews of Hysmartscopic
images.
From the beginning of the procedure, the average
time required to capture a video was approximately 1 min. The
system benefits from a large field of view up to ~90 degrees for a
single image at a distance of 3-10 mm from the lesions. This field
aperture is comparable to the measured resolution associated with
the conventional hysteroscopes (Karl Storz SE & Co. KG). Images
are captured by an 8 megapixel camera with autofocus. The data
acquisition procedure is similar to that of conventional
hysteroscopy. Hysmartscopy has the advantages of flexibility for
allowing examiners to manipulate the scope in a hand-held manner.
Two examiners reported feeling somewhat too comfortable using a
smartphone (4.0/5.0 on a 5-point Likert scale). The images were
acceptable for diagnostic procedures.
Diagnostic accuracy of Hysmartscopy in
the detection of intrauterine abnormalities.
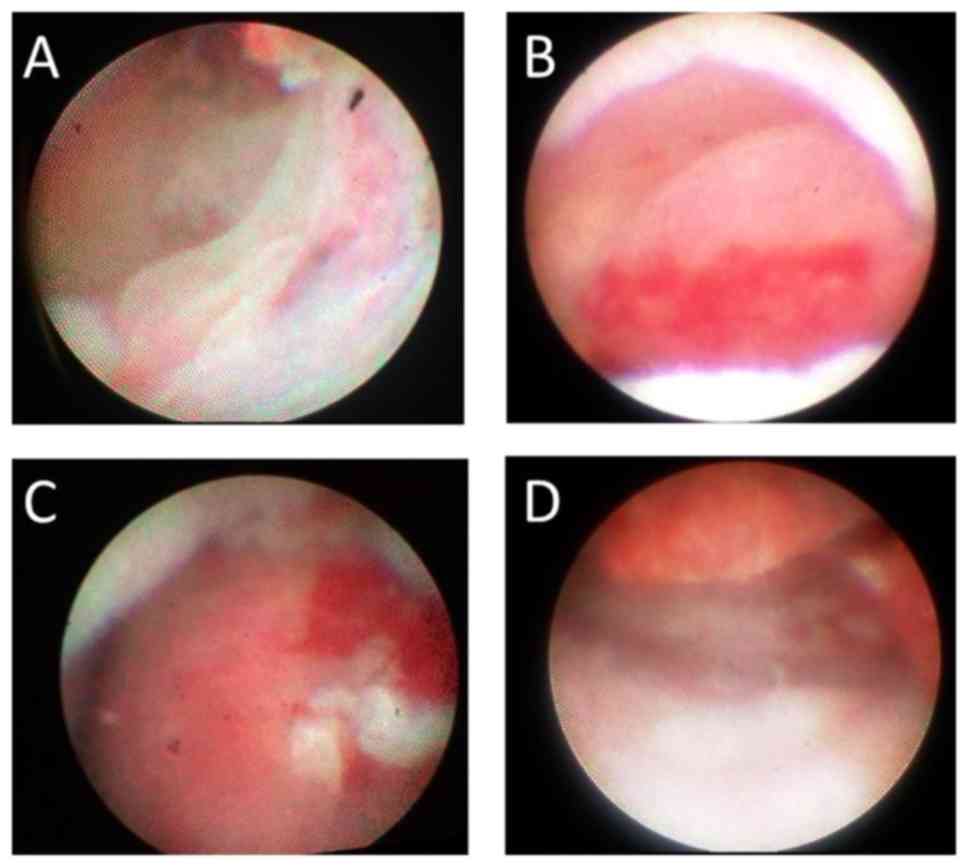
The diagnostically important frames extracted from
the Hysmartscopy iPhone videos are presented in Fig. 2. The pathological diagnosis of
intrauterine lesions in 22 women with abnormal uterine cavities was
as follows: Endometrial polyp (7 cases, 31.8%), submucosal fibroids
(8 cases, 36.4%), endometrial cancer (5 cases, 22.7%) and normal
endometrium (2 cases, 9.1%) (Table
I). This study evaluated whether Hysmartscopy provides an
accurate pathological diagnosis. Ultimately, the results of
Hysmartscopy and pathological reports of endometrial specimens were
compared, and the diagnostic accuracy of Hysmartscopy for normal
endometrium, endometrial polyps, submucosal fibroids and
endometrial cancer was evaluated. The diagnostic sensitivity of
Hysmartscopy was found to be 100% (2/2) for the normal endometrium,
71.4% (5/7) for endometrial polyps, 62.5% (5/8) for submucosal
fibroids and 100% (5/5) for endometrial cancer (Table II). The diagnostic accuracy of
Hysmartscopy in the detection of all intrauterine abnormalities was
77.3%.
 | Table IIThe diagnostic accuracy of
Hysmartscopy in the detection of intrauterine abnormalities. |
Table II
The diagnostic accuracy of
Hysmartscopy in the detection of intrauterine abnormalities.
| | | Hysmartscopy
diagnosis | |
|---|
| Pathological
reports | | Normal
endometrium | Endometrial
polyps | Submucosal
fibroids | EC | Diagnostic accuracy
(%) |
|---|
| Normal
endometrium | 2 | 2 | 0 | 0 | 0 | 100 |
| Endometrial
polyps | 7 | 1 | 5 | 1 | 0 | 71.4 |
| Submucosal
fibroids | 8 | 3 | 0 | 5 | 0 | 62.5 |
| Endometrial
cancer | 5 | 0 | 0 | 0 | 5 | 100 |
| | | | | | Total | 77.3 |
Adverse effects.
In the first cohort, there were no complications
during and after the diagnostic procedures. In the second cohort,
the Hysmartscopy system was successfully performed in all 5
subjects without anesthesia. All 5 patients tolerated the procedure
without analgesics or anesthesia in an office setting. None of the
cases had any complications during and after diagnostic
procedures.
Discussion
To the best of our knowledge, this is the first
proof of concept pilot study of a novel smartphone-based ultrathin
flexible fiberscope (currently known as Hysmartscopy). For this, a
flexible fiberscope (0.8 mm in diameter), its connector, iPhone 6S™
and portable LED light source are needed. The Hysmartscopy system
used in this study is the prototype for the device. The
feasibility, effectiveness, accuracy and performance of this system
for diagnosing intrauterine abnormalities were demonstrated in
ex vivo and clinical studies in the inpatient hospital
setting and outpatient office setting.
The aim of this study was to assess the feasibility
and safety of the Hysmartscopy system to diagnose intrauterine
abnormalities. In the first cohort, Hysmartscopy was performed in a
conventional operating room under general anesthesia in 17 patients
with an abnormal uterine cavity. In the second cohort, Hysmartscopy
was further validated in 5 additional subjects without anesthesia
and cervical dilatation in an office setting. In the proof of
concept pilot study, this system offers the advantage of direct
visualization of the uterine cavity without anesthesia in the
outpatient clinic. Endometrial polyps, submucosal fibroids and
endometrial cancer were correctly predicted in 5/7 (71.4%), 5/8
(62.5%) and 5/5 (100%) women, respectively. This study reports a
high diagnostic sensitivity (77.3%) and positive agreement between
the Hysmartscopy results and the histological findings. The
diagnostic accuracy of submucosal fibroids may depend on the degree
of the fibroid protruding towards the endometrial cavity, which
causes false endometrial thickening. The diagnostic sensitivity for
endometriotic cancer (n=5) was 100%. Bourdel et al reported
that the sensitivity and specificity of endometrial cancer were
86.6 and 87.3%, respectively, for experts with regarding to
evaluating the diagnostic accuracy of traditional hysteroscopy
(8). Hysmartscopy and
conventional hysteroscopy may be equally effective in diagnosing
intrauterine abnormalities.
In general, complications of surgical hysteroscopic
procedures may include simply, difficulty in entering the internal
os, bleeding, cervical laceration, uterine perforation, infection,
fluid overload, absorption of irrigation solutions, dilutional
hyponatremia, incomplete resection, intrauterine adhesions and,
rarely, gas or air embolism (2,9,10).
The reported incidence of complications is 1 to 3%, and the
majority of these occur during surgical procedures (11). The severe complication rate of
office hysteroscopy is rare, 0.05% (12). Hysmartscopy is diagnostic
hysteroscopy and is regarded as a safe and well-tolerated procedure
with rare complications. Due to the small diameter of the
instrument, flexibility and maneuverability, Hysmartscopy can be
used without anesthesia and cervical dilatation, and produces
minimal to no trauma to the cervical canal and thus markedly
diminishes any accidental bleeding.
This study also investigated the satisfaction of
gynecologists and the convenience of the smart device-based
Hysmartscopy. On average, the quality of the images and videos
taken by expert gynecologic endoscopists may be largely sufficient
to detect the emergent findings (4.0/5.0 on a 5-point Likert
scale). Image acquisition and spatial resolution would be
equivalent to an existing surgical camera system; the expert
reviewers found the overall image quality to be acceptable for
diagnostic purposes. Smartphone-based imaging can be an effective,
rapid and easy to learn procedure for medical trainees or residents
to capture intrauterine images in an office setting. This system is
lightweight, easy to use, has a low manufacturing cost,
field-portability and accessible design, together with the
connectivity of smartphones, which presents a promising platform
for diagnostic procedures in a variety of clinical settings.
Therefore, the Hysmartscopy system is considered to be an available
option for remote imaging via a network connection by an internet
web-based browser.
Furthermore, flexible hysteroscopes have been
developed for both diagnostic and therapeutic procedures. These
scopes provide specific advantages over rigid hysteroscopes in wide
120̊ field of view; however, the insertion tube outer diameter and
distal end outer diameter of the insertion portion are 4.5 and 4.9
mm, respectively (https://medical.olympusamerica.com/products). An
insertion tube diameter of the slimmest hysteroscope (HYF-XP from
Olympus Co., Ltd.) for office diagnostic hysteroscopy is 3.1 mm
(https://www.olympus-europa.com/medical/rmt/media/Content/Content-MSD/Documents/Brochures/hyf-xp__product-brochure_EN_20000101.pdf).
Continued technological advances will prompt the development of the
less complex and slimmer device, and allow its adaptation to a
minimally invasive hysteroscopic approach.
Guan et al (13) reported the advantages of robotic
techniques in hysteroscopic-assisted procedure to educate surgeons.
These advances could offer great value for surgeons by providing
visual, navigational, and mechanical computerized assistance. The
use of robotic-assisted hysteroscopy required for the intrauterine
operation is growing rapidly, driven by advances in technology,
which would make the difficult surgical techniques easier, safer,
more accessible and more efficient. Although robotic surgery has
great potential and may play an important role in surgical
settings, this procedure is still a pilot instrument that needs to
be improved through future studies.
The incidence of uterine cavity abnormalities
detected by Hysmartscopy in this study was only 77.3%. As shown in
Table II, 3 cases of women with
submucosal fibroids had completely normal intracavitary findings,
as they had submucosal fibroids with low fibroid protrusion ratio
into the uterine cavity. Not only Hysmartscopy, but also
conventional hysteroscopy could not confidently diagnose submucosal
fibroids with small intracavitary component, such as type II
fibroids (14).
In addition, this study was limited by the small
sample size (n=22), 2 expert gynecological endoscopists and by the
use of a subjective tool of a 5-step Likert scale. However, this is
a pilot proof of concept feasibility study and the 2 evaluators
were blinded to the pathological results, apart from the presence
of intrauterine abnormalities, which could sometimes compensate for
the small size. Another limitation is the lack of comparison with
an existing conventional hysteroscopy (15,16). Despite these limitations, it can
be considered that this new system is an accessible device,
comfortable to be used by examiners and patients, and may be useful
in the outpatient clinic for the direct visualization of the
uterine cavity. It may complement the less accurate methods, such
as blind endometrial cytology and curettage. These preliminary
results warrant further investigation to evaluate whether
Hysmartscopy affects therapeutic decision making and is considered
the gold standard for diagnosis of any intrauterine lesion.
In conclusion, this system may be a promising and
valuable alternative to the conventional hysteroscopy due to its
simplicity, accuracy, well-tolerability, portability, efficient
data collection and enhancing communication among physicians.
Acknowledgements
The authors would like to thank Mrs. Sachiko
Minakawa (CEO, OK Fiber Technology Co., Ltd., Kyoto, Japan.) and Dr
Takeshi Seki (Lecturer, Graduate School of Engineering Science,
Akita University, Akita, Japan.) for providing assistance with the
design, processing and assembly work accompanying the development
of prototypes for the Hysmartscopy system.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article or are available from the
corresponding author on reasonable request.
Authors' contributions
KO designed a novel smartphone-based ultrathin
flexible hysterofiberscopy system. KI and HS collected clinical
data.HK contributed to the conception, design and interpretation of
the data of this study. HK wrote the first draft. The final version
of the manuscript has been read and approved by all authors.
Ethics approval and consent to
participate
The study protocol was in agreement with the
Helsinki Declaration for Ethical Medical Research (no. 874).
Research was performed after obtaining approval from the Nara
Medical University Institutional Review Board (IRB). A written
informed consent was signed by each participant following a
detailed explanation of the objectives and protocol of the
study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Dueholm M, Lundorf E, Hansen ES, Ledertoug
S and Olesen F: Evaluation of the uterine cavity with magnetic
resonance imaging, transvaginal sonography, hysterosonographic
examination, and diagnostic hysteroscopy. Fertil Steril.
76:350–357. 2001.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Jansen FW, Vredevoogd CB, van Ulzen K,
Hermans J, Trimbos JB and Trimbos-Kemper TC: Complications of
hysteroscopy: A prospective, multicenter study. Obstet Gynecol.
96:266–270. 2000.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Gambadauro P, Martínez-Maestre MA and
Torrejón R: When is see-and-treat hysteroscopic polypectomy
successful? Eur J Obstet Gynecol Reprod Biol. 178:70–73.
2014.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Hauge K, Ekerhovd E and Granberg S:
Abnormal uterine bleeding refractory to medical therapy assessed by
saline infusion sonohysterography. Acta Obstet Gynecol Scand.
89:367–372. 2010.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Gambadauro P and Magos A: Pain control in
hysteroscopy. Finesse, not local anaesthesia. BMJ.
340(c2097)2010.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Campo R, Santangelo F, Gordts S, Di Cesare
C, Van Kerrebroeck H, De Angelis MC and Di Spiezio Sardo A:
Outpatient hysteroscopy. Facts Views Vis Obgyn. 10:115–122.
2018.PubMed/NCBI
|
|
7
|
Shigetomi H, Oka K, Seki T and Kobayashi
H: Design and preclinical validation of the composite-type optical
fiberscope for minimally invasive procedures of intrauterine
disease. J Minim Invasive Gynecol. 22:985–991. 2015. View Article : Google Scholar
|
|
8
|
Bourdel N, Modaffari P, Tognazza E,
Pertile R, Chauvet P, Botchorishivili R, Savary D, Pouly JL,
Rabischong B and Canis M: Does experience in hysteroscopy improve
accuracy and inter-observer agreement in the management of abnormal
uterine bleeding? Surg Endosc. 30:5558–5564. 2016.PubMed/NCBI View Article : Google Scholar
|
|
9
|
van Dongen H, de Kroon CD, Jacobi CE,
Trimbos JB and Jansen FW: Diagnostic hysteroscopy in abnormal
uterine bleeding: A systematic review and meta-analysis. BJOG.
114:664–675. 2007.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Aas-Eng MK, Langebrekke A and Hudelist G:
Complications in operative hysteroscopy-is prevention possible?
Acta Obstet Gynecol Scand. 96:1399–1403. 2017.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Sahu L, Tempe A and Gupta S: Hysteroscopic
evaluation in infertile patients: A prospective study. Int J Reprod
Contracept Obstet Gynecol. 1:37–41. 2012. View Article : Google Scholar
|
|
12
|
Capmas P, Pourcelot AG, Giral E, Fedida D
and Fernandez H: Office hysteroscopy: A report of 2402 cases. J
Gynecol Obstet Biol Reprod (Paris). 45:445–450. 2016.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Guan Z, Liu J, Bardawil E and Guan X:
Surgical management of cesarean scar defect: The
hysteroscopic-assisted robotic single-site technique. J Minim
Invasive Gynecol. Jun 17, 2019 (Epub ahead of print). PubMed/NCBI View Article : Google Scholar
|
|
14
|
Munro MG, Critchley HO and Fraser IS: FIGO
Menstrual Disorders Working Group: The FIGO classification of
causes of abnormal uterine bleeding in the reproductive years.
Fertil Steril. 95:2204–8, 2208.e1-3. 2011.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Marsh F and Duffy S: The technique and
overview of flexible hysteroscopy. Obstet Gynecol Clin North Am.
31:655–668. 2004.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Cicinelli E: Hysteroscopy without
anesthesia: Review of recent literature. J Minim Invasive Gynecol.
17:703–708. 2010.PubMed/NCBI View Article : Google Scholar
|