Introduction
Abnormal mechanical loading is a main external
factor affecting the development of osteoarthritis (OA).
Physiological loading plays a critical role in the maintenance of
the cartilage matrix. However, excessive loading causes an
imbalance between the degradation and synthesis of matrix
macromolecules, thus resulting in OA (1,2).
Obesity and a heavy physical workload influence the occurrence of
hip OA (3,4). Acetabular dysplasia is an anatomical
factor that increases the mechanical stress on the articular
surface of the hip joint (5,6).
However, the incidence of OA with concurrent acetabular dysplasia
is lower in patients of an advanced age (7,8).
Age-related spinal degenerative change commonly
results in spinal kyphosis in older individuals. Patients with
spinal kyphosis develop posterior pelvic inclination to compensate
for their sagittal spinal imbalance (9-11).
Excessive posterior pelvic inclination may uncover the anterior
acetabulum (12). The decrease in
the loading area of the femoral head presumably increases
mechanical stress to the articular surface, resulting in OA. To
date, only a limited number of studies have described such a
mechanism in the etiology of hip OA (13,14).
Kitamura et al (15)
recently analyzed the equivalent stress of the acetabular surface
at three pelvic tilt positions relative to the functional pelvic
plane (10° anterior tilt, no tilt, and 10°
posterior tilt). They demonstrated that the mean contact area was
smaller and that the mean maximum contact pressure and median
maximum equivalent stress were larger in anteriorly than
posteriorly tilted pelvises. However, exactly how much posterior
pelvic inclination produces an excessive load on the articular
surface and is a risk factor for OA onset remains unknown.
The present study was thus performed to determine
the amount of posterior pelvic inclination required to reproduce
the loading condition of the dysplastic hip joints using finite
element (FE) analysis. To this end, the mechanical stress of the
articular surface of the hip was analyzed while posterior pelvic
inclination was serially increased in five-degree increments. In
addition, the mechanical stress was compared between normal hips
and hips with acetabular dysplasia with or without posterior pelvic
inclination.
Patients and methods
Patients
Patients treated for coxalgia at Kagoshima
University Medical Hospital from January, 2011 to December, 2016
were retrospectively evaluated. The criteria for enrollment in the
present study were as follows: A hip joint space of >2.0 mm, no
radiographic evidence of formation of osteophytes or cysts or
severe sclerotic change, deformity of the femoral head to eliminate
secondary changes in osteoarthritic progression, and no previous
operation on the hip joint. The present study finally included 27
hips of 19 women [unilateral (right or left) hip joints of 11 women
and bilateral (right and left) hip joints of 8 women were
analyzed]. All data were retrospectively collected from medical
records (Table I). The research
protocol of the present study was approved by the Institutional
Ethics Committee on Clinical Research of Kagoshima University, and
the study was performed in compliance with the Declaration of
Helsinki. Patient consent was waived by the committee as this study
was a retrospective observational study.
 | Table IBaseline characteristics of the
patients in the present study. |
Table I
Baseline characteristics of the
patients in the present study.
| | Normal (n=16
hips) | Acetabular dysplasia
(n=11 hips) | P-value |
|---|
| Age, years | 59.0±19.7 | 46.0±13.5 | 0.98 |
| Sharp's angle of the
hip | 39.3±3.3 | 47.6±2.1 |
<0.001a |
| Pelvic
inclination | 22.4±5.7 | 19.6±5.0 | 0.20 |
Radiographic measurements
The Sharp's angle of the hip and pelvic inclination
were measured on frontal X-ray images of the bilateral hip joints.
A Sharp's angle of ≥45 degrees was defined as acetabular dysplasia
in the present study. The pelvic inclination was calculated based
on measurements from anteroposterior pelvic radiographs according
to a previous report (16). In
summary, the pelvic inclination was calculated using the following
equation: A=-69.0° x L/T + 61.6° in women,
where L/T is the longitudinal/transverse axis length ratio of the
pelvic cavity on the anteroposterior pelvic radiograph. The
equation was produced by comparing the pelvic inclination with the
L/T ratio using Japanese pelvic bones. According to an original
study using anteroposterior pelvic radiographs of normal hip
joints, the standard pelvic inclination was 19.97±5.93°
in women (16).
FE analysis
Femoral and pelvic models were created based on
computed tomography (CT) scans with a slice thickness of 3 mm. CT
imaging was performed in the supine position. This position was
defined as the original position.
FE models of the femur and pelvis were generated
from the CT data using Mechanical Finder version 9.0 software
(Research Centre for Computational Mechanics Inc.). This software
constructs FE models demonstrating the shape of the individual bone
and the distribution of its density; it also implements the FE
method for solving linear algebraic equations using the
displacement method (17). FE mesh
models were produced using ANSYS ICEM CFD version 18.0 (ANSYS Inc.)
with this software. FE models of the femur were produced using the
methods described in the study by Bessho et al (17) and their methods were applied to the
pelvis. Image processing was performed using Mechanical Finder
version 10.0 (Research Centre for Computational Mechanics Inc.,
Tokyo, Japan).
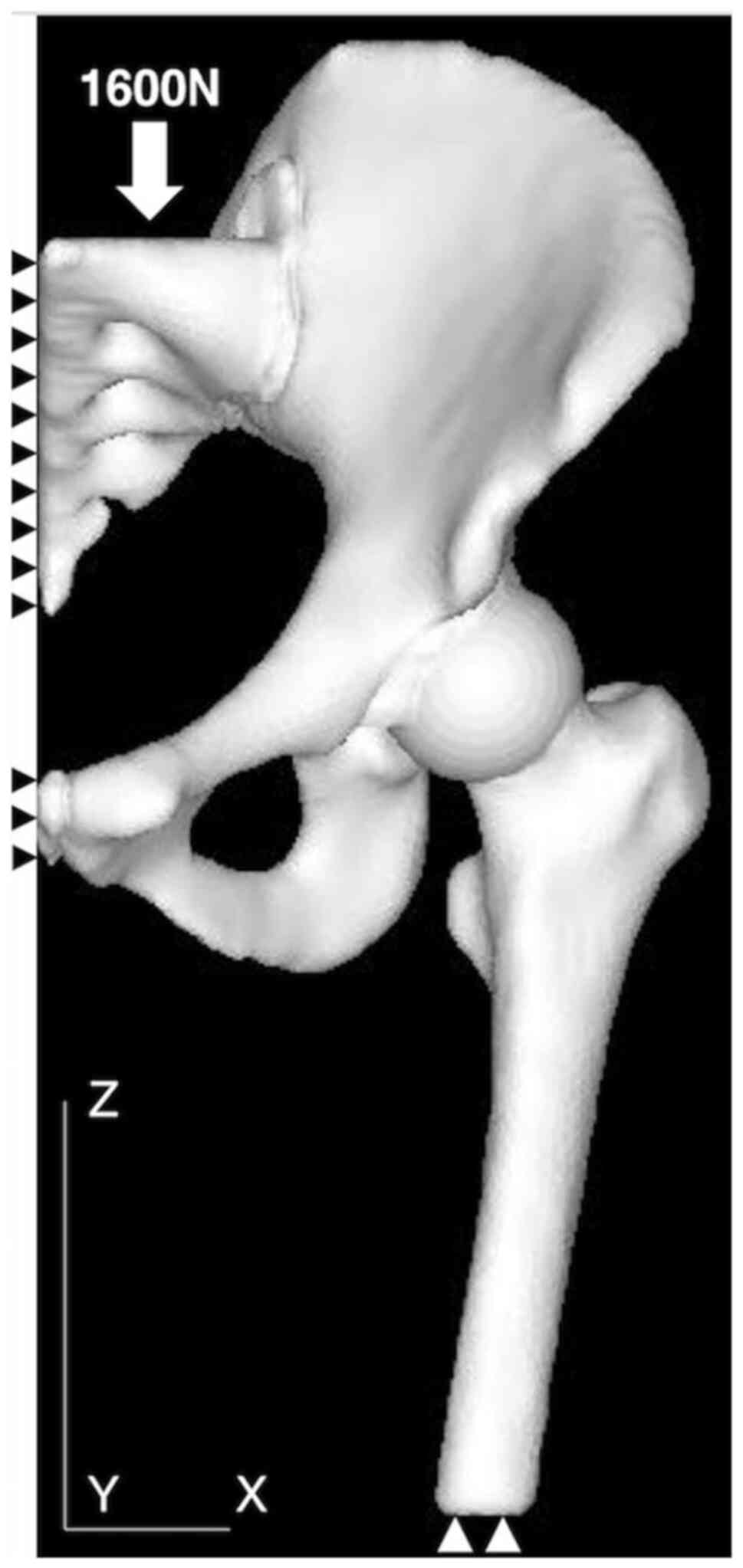
Subsequently, three-dimensional FE models were
constructed for each patient (Fig.
1). A mesh size of <2 mm could not be solved due to the
limited capacity of the computer used. A total of five models of
different mesh sizes were created to perform the mesh sensitivity
test: 2.0 to 4.0 mm, 2.5 to 5.0 mm, 3.0 to 6.0 mm, 3.5 to 7.0 mm
and 4.0 to 8.0 mm. The mesh convergence test used in the present
study calculated the equivalent stress. The percentage change of
the equivalent stress between the 2.0- to 4.0-mm model and the 2.5-
to 5.0-mm model was 0.70%. The percentage changes between the 2.0-
to 4.0-mm and 3.0- to 6.0-mm models, 2.0- to 4.0-mm and 3.5- to
7.0-mm models, and 2.0- to 4.0-mm and 4.0- to 8.0-mm models were
1.13, 3.70 and 5.02%, respectively. Therefore, the 2.0- to 4.0-mm
mesh size was used. These models had 2.0- to 4.0-mm tetrahedral
elements for the inner cortical and cancellous bone and three-nodal
point shell elements with a thickness of 0.4 mm for the outer
cortical bone. Articular cartilage was modeled as a homogeneous
isotropic material (18). The
articular cartilage of the femoral head was presumed to be
spherical and to have a mean thickness of 2.0 mm (19). The models of articular cartilage
had 0.5- to 1.0-mm tetrahedral elements. FE models of the pelvis
were constructed with ~300,000 elements, and those of the femur
were constructed with ~130,000 elements. The elastic modulus of the
cortical and cancellous bone was determined from CT density values
using the equations proposed in the study by Keyak et al
(20) (Table II). Poisson's ratio of the
cortical and cancellous bone was 0.40 (20,21).
Articular cartilage had an elastic modulus of 10.35 MPa and a
Poisson's ratio of 0.40(18). The
models presumed completely bonded interfaces between cartilage and
bone, while the coefficient of friction between cartilages was
presumed to be 0 (Fig. 1). The
applied loading condition was based on the study by Ike et
al (18). A load of 1,600 N
was applied vertically to the sacral spine. The models were
presumed to represent the patient standing on one leg. Pauwels
(22) previously reported that the
contact force of the femoral head was three times the body weight
when standing on one leg. The mean body weight of Japanese women
was ~53 kg in 2015. Therefore, the load was defined as 1,600 N. Of
note, two boundary conditions were used in the present study: The
distal parts of the femoral shafts were fully restrained, and the
median line of the pelvis was fully restrained except for Z-axial
displacement (Fig. 2). In each
model, three-dimensional FE models were also constructed by
changing the pelvic inclination from the original position to +30
degrees in five-degree increments.
 | Table IIEquations used to calculate the
elastic modulus of bone. |
Table II
Equations used to calculate the
elastic modulus of bone.
| Bone density | Elastic modulus |
|---|
| ρ=0 | 0.001 |
| 0<ρ≤0.27 |
33,900p2.20 |
| 0.27<ρ<0.6 | 5307p + 469 |
| 0.6≤ρ |
10,200p2.01 |
The Drucker-Prager yield criterion was used. The
mean equivalent stress in the subchondral bone was used. The mean
equivalent stress in the part of the femoral head covered by the
acetabular roof was measured.
Statistical analysis
Age, Sharp's angle of the hip and pelvic inclination
values are expressed as the mean ± standard deviation. The
equivalent stress is expressed as the median and interquartile
range. The Kolmogorov-Smirnov and Shapiro-Wilk tests were used to
evaluate the data. The equivalent stress did not follow a normal
distribution; therefore, the Mann-Whitney U test was used to
compare the equivalent stress of the femoral head between normal
hip joints and hips affected by acetabular dysplasia. A value of
P<0.05 was considered to indicate a statistically significant
difference. The equivalent stress measured for each pelvic
inclination was compared. The Kruskal-Wallis test was used to
compare the equivalent stress among the different pelvic
inclinations. If the difference was significant, the Bonferroni
correction was used. All statistical analyses were performed using
EZR version 1.35 (Saitama Medical Center, Jichi Medical University,
Saitama, Japan), which is a graphical user interface for R (The R
Foundation for Statistical Computing). More precisely, it is a
modified version of R commander designed to add statistical
functions frequently used in biostatistics (23).
Results
FE analysis was used to compare normal hips with
hips affected by acetabular dysplasia, changing the pelvic
inclination from the original position to 30 degrees. The
equivalent stress for the femoral head at the original position was
0.97 MPa (0.91-1.01) in normal hip joints and 1.18 MPa (1.00-1.28)
in hips affected by acetabular dysplasia (P=0.023; Fig. 3).
The distribution and volume of the equivalent stress
to the femoral head at the original position and with 30 degrees of
posterior inclination is presented in Fig. 3. In hips with acetabular dysplasia,
the equivalent stress one-sidedly increased at the anterior portion
of the femoral head compared with the normal hip (Fig. 4A and C). In both normal hips and hips with
acetabular dysplasia, the equivalent stress was markedly increased
at 30 degrees of posterior inclination (Fig. 4B and D).
The equivalent stress of the femoral heads under
various conditions in which the pelvic inclination was changed from
the original position to 30 degrees in 5-degree increments is shown
in Table III. In both normal
hips and hips with acetabular dysplasia, the equivalent stress
increased in a stepwise manner. In the normal hips, when the pelvic
posterior inclination was increased by 25 and 30 degrees, the
equivalent stress was 1.21 (1.11=1.35) and 1.24 (1.20=1.47) MPa,
respectively (P=0.029 and 0.010, respectively). In the hips
affected by acetabular dysplasia, when the posterior pelvic
inclination was increased by 30 degrees, the equivalent stress was
1.61 (1.33-1.85) (P=0.016; Table
III).
 | Table IIIEquivalent stress in the femoral head
in the patients in the present study. |
Table III
Equivalent stress in the femoral head
in the patients in the present study.
| A, Normal hip |
|---|
| Pelvic inclination
angle | Median | Interquartile
range | P-value (vs. original
position) |
|---|
| Original
position | 0.97 | 0.91-1.01 | |
| +5° | 1.00 | 0.93-1.05 | 1.0 |
| +10° | 1.02 | 0.93-1.10 | 1.0 |
| +15° | 1.10 | 0.99-1.16 | 0.97 |
| +20° | 1.16 | 1.05-1.24 | 0.11 |
| +25° | 1.21 | 1.11-1.35 | 0.029a |
| +30° | 1.24 | 1.20-1.47 | 0.010a |
| B, Acetabular
dysplasia |
| Pelvic inclination
angle | Median | Interquartile
range | P-value (vs.
original position) |
| Original
position | 1.18 | 1.00-1.28 | 1.0 |
| +5° | 1.19 | 1.05-1.31 | 1.0 |
|
+10° | 1.23 | 1.08-1.37 | 1.0 |
|
+15° | 1.30 | 1.12-1.40 | 1.0 |
|
+20° | 1.39 | 1.20-1.48 | 1.0 |
|
+25° | 1.51 | 1.26-1.67 | 0.18 |
|
+30° | 1.61 | 1.33-1.85 | 0.016a |
The equivalent stress of the femoral heads in
patients with acetabular dysplasia was 1.22-fold greater than that
in patients with normal hip joints. The equivalent stress of the
normal hip joint with 25 degrees of posterior pelvic inclination
was 1.25-fold greater than that of the original position. This
overloading of the normal hip joint in patients with posterior
pelvic inclination was the same as that in patients with acetabular
dysplasia in the original position. Furthermore, the equivalent
stress of the hip affected by acetabular dysplasia with 25 degrees
of posterior pelvic inclination was 1.55-fold greater than that of
the normal hip at the original position (Fig. 5).
Discussion
The present study investigated the mechanical stress
of hip joints with or without acetabular dysplasia by FE analysis.
The mechanical stress when the posterior pelvic inclination changed
from 0 to 30 degrees was also investigated.
A previous epidemiological study demonstrated that
the population with acetabular dysplasia had a 4.3-fold higher risk
of developing radiographic OA of the hip than the population
without acetabular dysplasia (6).
Excessive contact stress of the articular surface of the hip in
patients with acetabular dysplasia predicts the onset of OA;
therefore, various osteotomies have been designed to reduce the
mechanical stress and risk of OA development (24).
Patient-specific FE analysis has revealed that
rotational acetabular osteotomy reduces the mechanical stress in
the hip joint. The equivalent stress in the femoral head has been
shown to decrease from 3.4 MPa (1.2-6.0) to 2.9 MPa (1.7-4.0)
(18). Therefore, the
post-operative equivalent stress in the femoral heads with
acetabular dysplasia was 0.85-fold greater than that in the
pre-operative hips (18).
Hip-spine syndrome is a widely accepted morbid
association between lumbar spine arthrosis and hip arthrosis
(25). In patients of an advanced
age, posterior pelvic inclination commonly increases due to various
factors, including spinal kyphosis, paravertebral muscle weakness
and failure of the pelvic support mechanism (26). Posterior pelvic inclination in
patients with decreased lumbar lordosis reduces the femoral head
area covered by the acetabulum (12). The present study demonstrated that
normal hip joints without acetabular dysplasia had a mechanical
stress almost equivalent to that in hip joints with acetabular
dysplasia when posterior pelvic inclination was increased to 25
degrees (Fig. 5). Yoshimoto et
al (27) analyzed several
hip-spine alignment parameters, including pelvic tilt in patients
with or without hip dysplasia. They found that patients who had hip
OA without acetabular dysplasia tended to have decreased lumbar
lordosis and increased posterior pelvic tilt, which was frequently
observed in the older patients (27). With aging, posterior pelvic tilt
increases as lumbar spinal degeneration decreases lumbar lordosis,
resulting in secondary hip OA (spine-hip syndrome). Based on these
current findings, posterior pelvic inclination of >25 degrees
may be a risk factor for onset of OA secondary to pelvic
malalignment, including hip-spine (spine-hip) syndrome.
The present study has several limitations. First,
the stress was analyzed for a single-legged stance. The stress of
the hip joint during some activities (walking, running and stair
climbing) could not be evaluated. Second, the bone models were
created based on the CT images of each patient, but with the same
loading conditions. Therefore, the results of the present study
were subject to minor differences. Finally, the main limitation of
the present study was the lack of direct epidemiological data
showing that posterior pelvic inclination is a risk factor for OA.
Such an epidemiological study may demonstrate the actual critical
degree of posterior pelvic inclination that leads to hip OA.
In conclusion, the present study demonstrated that
the mechanical stress of normal hip joints serially increased as
posterior pelvic inclination increased, reaching a level almost
equivalent to that of hip joints with acetabular dysplasia at 25
degrees of posterior pelvic inclination. The data presented herein
suggest that posterior pelvic inclination may be a mechanical
factor that affects the development of OA in patients without
acetabular dysplasia, particularly when the posterior pelvic
inclination exceeds 25 degrees.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
DS and YI designed the study. DS, YF, SNak and TI
performed data collection. DS, YI, SNag and NT analyzed the data
and wrote the manuscript. SNak and NT revised the manuscript
critically for important intellectual content. DS and SNag confirm
the authenticity of all the raw data. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee on Clinical Research at Kagoshima University (no. 29-37),
and the study was performed in compliance with the Declaration of
Helsinki. Patient consent was waived by the committee as this study
was a retrospective observational study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Sun HB: Mechanical loading, cartilage
degradation, and arthritis. Ann N Y Acad Sci. 1211:37–50.
2010.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Chen C, Tambe DT, Deng L and Yang L:
Biomechanical properties and mechanobiology of the articular
chondrocyte. Am J Physiol Cell Physiol. 305:1202–1208.
2013.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Lievense AM, Bierma-Zeinstra SM, Verhagen
AP, van Baar M, Verhaar JA and Koes BW: Influence of obesity on the
development of osteoarthritis of the hip: A systematic review.
Rheumatology (Oxford). 41:1155–1162. 2002.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Lievense A, Bierma-Zeinstra S, Verhagen A,
Verhaar J and Koes B: Influence of work on the development of
osteoarthritis of the hip: A systematic review. J Rheumatol.
28:2520–2528. 2001.PubMed/NCBI
|
|
5
|
Weinstein SL: Natural history of
congenital hip dislocation (CDH) and hip dysplasia. Clin Orthop
Relat Res. 62–76. 1987.PubMed/NCBI
|
|
6
|
Reijman M, Hazes JM, Pols HA, Koes BW and
Bierma-Zeinstra SM: Acetabular dysplasia predicts incident
osteoarthritis of the hip: The Rotterdam study. Arthritis Rheum.
52:787–793. 2005.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Ishidou Y, Matsuyama K, Sakuma D,
Setoguchi T, Nagano S, Kawamura I, Maeda S and Komiya S:
Osteoarthritis of the hip joint in elderly patients is most
commonly atrophic, with low parameters of acetabular dysplasia and
possible involvement of osteoporosis. Arch Osteoporos.
12(30)2017.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Lane NE, Nevitt MC, Cooper C, Pressman A,
Gore R and Hochberg M: Acetabular dysplasia and osteoarthritis of
the hip in elderly white women. Ann Rheum Dis. 56:627–630.
1997.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Ailon T, Shaffrey CI, Lenke LG, Harrop JS
and Smith JS: Progressive spinal kyphosis in the aging population.
Neurosurgery. 77 (Suppl 4):S164–S172. 2015.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Kasukawa Y, Miyakoshi N, Hongo M, Ishikawa
Y, Kudo D, Suzuki M, Mizutani T, Kimura R, Ono Y and Shimada Y:
Age-related changes in muscle strength and spinal kyphosis angles
in an elderly Japanese population. Clin Interv Aging. 12:413–420.
2017.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Barrey C, Roussouly P, Le Huec JC,
D'Acunzi G and Perrin G: Compensatory mechanisms contributing to
keep the sagittal balance of the spine. Eur Spine J. 22 (Suppl
6):S834–S841. 2013.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Watanabe W, Sato K, Itoi E, Yang K and
Watanabe H: Posterior pelvic tilt in patients with decreased lumbar
lordosis decreases acetabular femoral head covering. Orthopedics.
25:321–324. 2002.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Russell ME, Shivanna KH, Grosland NM and
Pedersen DR: Cartilage contact pressure elevations in dysplastic
hips: A chronic overload model. J Orthop Surg Res.
1(6)2006.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Chegini S, Beck M and Ferguson SJ: The
effects of impingement and dysplasia on stress distributions in the
hip joint during sitting and walking: A finite element analysis. J
Orthop Res. 27:295–201. 2009.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Kitamura K, Fujii M, Utsunomiya T, Iwamoto
M, Ikemura S, Hamai S, Motomura G, Todo M and Nakashima Y: Effect
of sagittal pelvic tilt on joint stress distribution in hip
dysplasia: A finite element analysis. Clin Biomech (Bristol, Avon).
74:34–41. 2020.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Doiguchi Y, Iwasaki K and Yamada K:
Correlation between pelvic inclination and radiological shape of
the pelvic cavity. Orthop Traumatol. 41:641–645. 1992.
|
|
17
|
Bessho M, Ohnishi I, Matsuyama J,
Matsumoto T, Imai K and Nakamura K: Prediction of strength and
strain of the proximal femur by a CT-based finite element method. J
Biomech. 40:1745–1753. 2007.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Ike H, Inaba Y, Kobayashi N, Yukizawa Y,
Hirat Y, Tomioka M and Saito T: Effects of rotational acetabular
osteotomy on the mechanical stress within the hip joint in patients
with developmental dysplasia of the hip: A Subject-Specific finite
element analysis. Bone Joint J. 97-B:492–497. 2015.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Zhao X, Chosa E, Totoribe K and Deng G:
Effect of periacetabular osteotomy for acetabular dysplasia
clarified by three-dimensional finite element analysis. J Orthop
Sci. 15:632–640. 2010.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Keyak JH, Rossi SA, Jones KA and Skinner
HB: Prediction of femoral fracture load using automated finite
element modeling. J Biomech. 31:125–133. 1998.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Reilly DT and Burstein AH: The elastic and
ultimate properties of compact bone tissue. J Biomech. 8:393–405.
1975.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Pauwels F: Biomechanics of the Normal and
Diseased Hip. Theoretical Foundation, Technique and Results of
Treatment. An Atlas. Springer-Verlag, 1976.
|
|
23
|
Kanda Y: Investigation of the freely
available easy-to-use software ‘EZR’ for medical statistics. Bone
Marrow Transplant. 48:452–458. 2013.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Mavčič B, Iglič A, Kralj-Iglič V, Brand RA
and Vengust R: Cumulative hip contact stress predicts
osteoarthritis in DDH. Clin Orthop Relat Res. 466:884–891.
2008.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Offierski CM and Macnab I: Hip-spine
syndrome. Spine (Phila Pa 1976). 8:316–321. 1983.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Sasaki K, Hongo M, Miyakoshi N, Matsunaga
T, Yamada S, Kijima H and Shimada Y: Evaluation of sagittal
spine-pelvis-lower limb alignment in elderly women with pelvic
retroversion while standing and walking using a three-dimensional
musculoskeletal modelw. Asian Spine J. 11:562–569. 2017.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Yoshimoto H, Sato S, Masuda T, Kanno T,
Shundo M, Hyakumachi T and Yanagibashi Y: Spinopelvic alignment in
patients with osteoarthrosis of the hip: A radiographic comparison
to patients with low back pain. Spine (Phila Pa 1976).
30:1650–1657. 2005.PubMed/NCBI View Article : Google Scholar
|