Introduction
Periodontal abscesses have a high prevalence rate
and are thus considered to be the third most prevalent infection
which demands emergency treatment (1,2).
Clinically, periodontal abscess usually presents as an ovoid
swelling in the gingiva along the lateral side of the root
(3,4). It is usually associated with a
periodontal pocket, the presence of bleeding upon probing and
suppuration, and the involved tooth may exhibit increased tooth
mobility and tenderness upon percussion (1,5).
Periodontal abscesses are treated with oral rinses, mechanical
debridement and drainage; antibiotic therapy is only administered
in certain conditions, such as endo-perio lesions, phoenix abscess,
etc (2).
Based on the etiology, periodontal abscesses can be
either periodontitis-related or non-periodontitis-related. Occlusal
trauma has been shown to be linked to periodontal abscesses
(4,5). Occlusal trauma is the damage
inflicted to teeth when excessive force acts upon the tooth. It is
basically the injury resulting in tissue changes within the
attachment apparatus as a result of occlusal force. Excessive
occlusal forces applied to a tooth with normal periodontal support
is termed as primary occlusal trauma, and when the injury results
from excessive forces on tooth/teeth with reduced periodontal
support, this is considered as secondary occlusal trauma (6).
Occlusal trauma is considered to elicit an
inflammatory response in the periodontal apparatus, as well as in
the dental pulp, which can lead to pulpal death, and the
derangement in periodontal structures and alveolar bone (7).
Both periodontal and endodontic disorders can
advance at different rates, depending on a variety of factors, such
as injuries, trauma, etc (4,6).
These elements may also have an impact on the effectiveness of any
given treatment. The additional impact of treating one tissue on
the companion tissue should be taken into account when treating
teeth with concurrent endodontic and periodontal disorders. The
timing of endodontic therapy is a crucial factor to consider when
scheduling treatment for concurrent periodontal and endodontic
disorders. Furthermore, since cross-seeding through the apical or
lateral foramina is a possibility, the result of endodontic therapy
may be affected if the root canal filling is inserted, while a
periodontal infection that interacts with the root canal system is
still present. Fortunately, utilizing an antibacterial medication
inside the canals during periodontal therapy helps keep the
environment within the root canal system in a state that is
unfavorable for bacterial colonization, particularly if the
dressing is changed on a frequent basis. Utilizing a biocompatible
medication is crucial for encouraging periodontal recuperation and
for improving the general outlook of the tooth (7).
The present study describes the inter-disciplinary
management involving endodontic and periodontal treatment of the
tooth of a patient with periodontal abscess due to occlusal
trauma.
Case report
A 42-year-old male patient reported to the
Department of Conservative Dentistry and Endodontics (Manipal
College of Dental Sciences Mangalore, Manipal Academy of Higher
Education, Manipal, India) with the chief complaint of a fractured
cusp with respect to the lower left back tooth, 1 week prior. The
medical history of the patient was non-contributory and the
biochemical parameters were not evaluated. No extraoral changes
were noted, and an intraoral examination revealed a bilateral
fractured cusp on tooth no. 36, which was found to be due to
excessive masticatory load. Pulp sensibility tests revealed that
the tooth was vital. No periapical changes were noted on intraoral
periapical radiograph. Taking into consideration the clinical and
radiographic findings, a composite restoration was performed to
build up the fractured cusp after relieving the tooth from
occlusion.
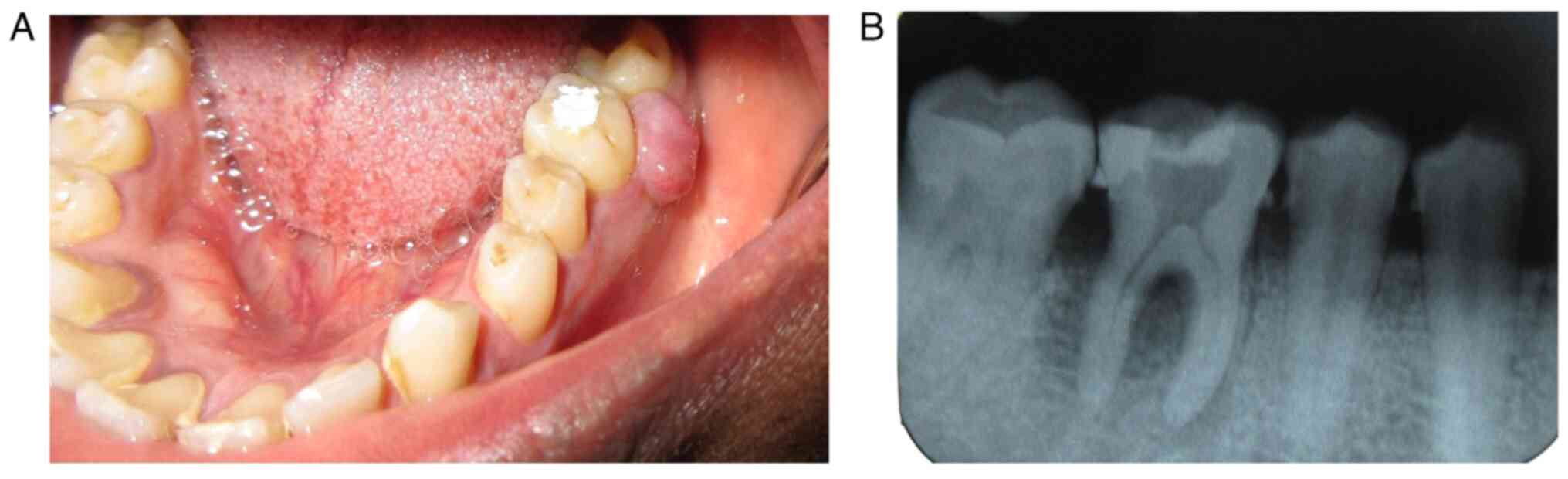
Following this episode, the patient returned to the
aforementioned department after 2 months, with the complaint of a
swelling in the lower back tooth. Upon an intraoral examination, a
localized swelling (1 cm in diameter) was found on tooth no. 36. A
periodontal pocket measuring 5 mm was found on the distal aspect of
tooth no. 36. The tooth developed grade II mobility and was
rendered non-vital due to the lack of a response on the pulp
vitality test. An intra oral periapical radiograph with respect to
tooth no. 36 revealed diffuse radiolucency involving the distal
root, the loss of lamina dura in that area and radiolucency in the
furcation area, suggestive of furcation involvement. Horizontal
bone loss was also noted. Noting the aforementioned results, the
treatment strategy was planned accordingly.
Treatment of the periodontal
abscess
For the treatment of the periodontal abscess, the
patient was referred to the Department of Periodontology in the
same institution. As there was a periodontal pocket and drainage
was feasible via the sulcus, surgical drainage and incision did not
constitute the recommended course of treatment. After administering
local anesthesia, gracey curettes 11-12 and 13-14 were used to
drain the abscess through the sulcus. Following the drainage,
antibiotics (C. Amox LB, 500 mg, 1-1-1 for 5 days) were prescribed
over the course of 5 days. Additionally, urgent endodontic therapy
was initiated. Rubber dam isolation was difficult, since the tooth
was grade II mobile (Fig. 1).
By the next visit, the resolution of the swelling
was noted and the mobility had reduced from grade II to grade I. A
reduction in the depth of the periodontal pocket was observed. The
endodontic treatment was then completed using Protaper files
(Dentsply Inc., Maillefer, Dentsply India) with the crown down
technique till F2 file size. Copious irrigation was performed using
normal saline 0.9 and 5% sodium hypochlorite (Vishal Dentocare Pvt.
Ltd.). In addition, three rounds of calcium hydroxide were
administered as an intracanal medicament in the form of Calcicur
(Voco) at every 15-day intervals. After 45 days, tooth no. 36 was
obturated with an F2 protaper gutta percha cone (Dentsply Inc.,
Maillefer, Dentsply India) along with AH Plus sealer (Dentsply
Inc., Sirona, Dentsply India).
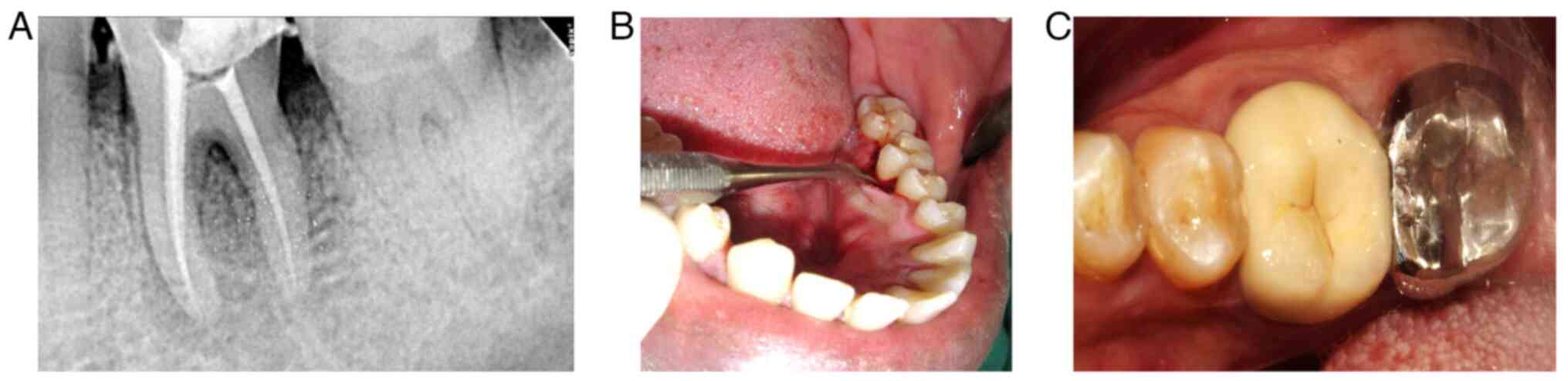
To receive the core build up, the existing
restoration was removed. Limited access to the tooth surface was
noted on the lingual side, and hence, an access flap was planned.
After administering local anesthesia, sulcular incisions was placed
around tooth no. 36, the flap was reflected using periosteal
elevator and access was achieved for the restoration. Lingually,
the access flap was reflected below the gingival margin, and the
tooth surface was smoothened using polishing bur and the entire
cavity was sealed using glass ionomer (GC Glass Ionomer Universal
Restorative) restoration (Fig.
2A). Simple interrupted sutures were placed and post-operative
instructions were provided. The patient was recalled after 1 week,
and suture removal followed by the reduction of glass ionomer
restoration and the composite core build up (Filtek Z 350 XT, 3M
ESPE) were performed. The patient was recalled after 1 month and
porcelain fused to metal crown was administered as the
post-endodontic restoration (Fig.
2B and C).
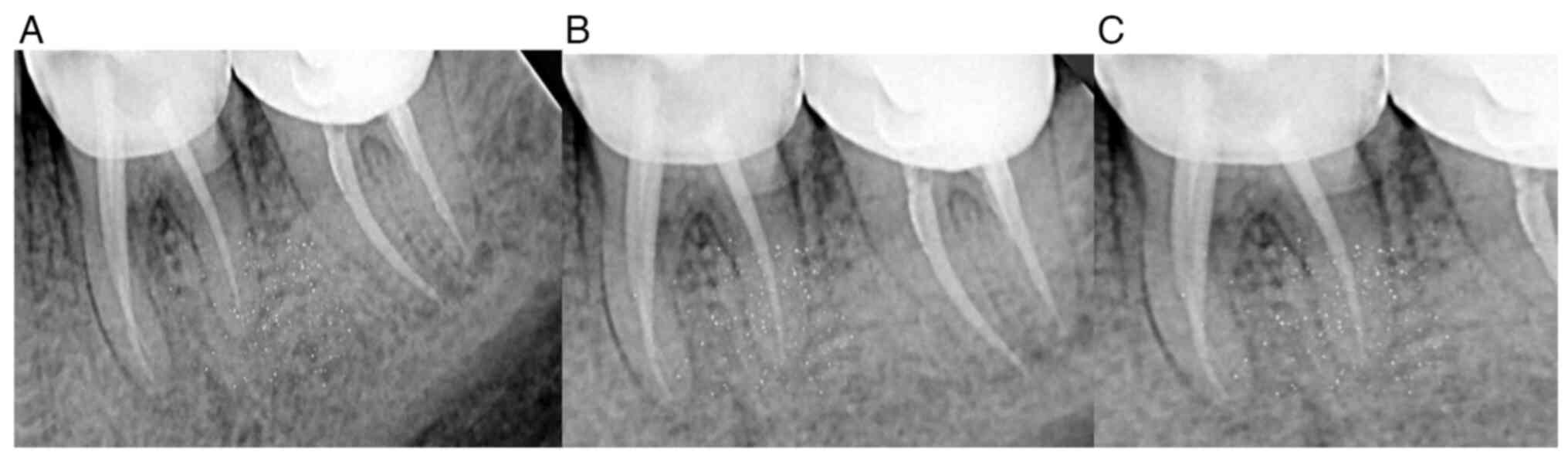
Follow-up visits were scheduled for clinical and
radiographic examinations. During the follow-up clinical
examinations, healthy gingival and periodontal health was noted
with the reduced mobility of tooth no. 36. Upon a radiographic
examination, the dissolution of periapical changes and bone fill
were noted. The patient was followed-up for 3 months, 6 months, 1
year and 2 years post-treatment (Fig.
3).
Discussion
The present study highlights the need of an
interdisciplinary approach in the management of endodontic and
periodontal lesions. The endo-periodontal conditions require the
assistance of experts from the fields of endodontic and
periodontics, as the need for periodontal therapy and endodontic
treatment cannot be accomplished by general dentists.
There are several potential causes of dental
infections, including gingival infections, trauma, surgery,
pericoronitis and pulp necrosis. Depending on the etiology of the
infection, odontogenic or dental abscesses are classified as
endodontic or periapical, periodontal, or pericoronal (3). In emergency dentistry clinics, the
frequency of periodontal abscesses has been investigated (8,9).
Periodontal abscesses are frequently linked to areas where there
was no previous periodontal pocket or directly to periodontitis.
While such occurrences can sometimes occur in the absence of an
abscess, a periodontal abscess in periodontitis indicates an
interval of ongoing bone deterioration (exacerbation). Abscesses
can emerge more easily in convoluted areas with cul-de-sacs that
ultimately become sequestered. Through the course of illness, a
periodontal abscess can arise at numerous stages: As an acute
aggravation of unresolved periodontitis during periodontal therapy,
in cases of resistant periodontitis, or while performing
periodontal management. In the absence of periodontitis,
periodontal abscesses may originate from the following causes: i)
Effects of foreign bodies; ii) an endodontic tool creating a hole
in the tooth wall; iii) the involvement of the lateral cysts; and
iv) local elements influencing the shape of the root may make a
periodontal abscess more likely to develop (3,9).
The periodontal abscess may have commenced as a
result of germs entering the soft tissue pocket wall. Chemotactic
proteins secreted by the bacteria subsequently draw in
pro-inflammatory cells, and the ensuing inflammatory response
causes the connective tissues to be destroyed, the bacterial
encapsulation and pus generation. Histologically, a core region of
damaged leukocytes and soft tissue debris is surrounded by intact
neutrophils (9).
At a later stage, neutrophils and macrophages
assemble to form a pyogenic membrane. Since a highly acidic
atmosphere will encourage the action of lysosomal enzymes, the
degree of breakdown in the abscess will be dependent on the
pathogenicity and development of the bacteria inside the foci as
well as the local pH (3).
In the case in the present study, the initial
representation was of a fractured cusp, which was found to be the
result of occlusal trauma. Occlusal trauma has long been known to
cause damage to the underlying periodontium. The injury that thus
results in the periodontium is known as trauma from occlusion. This
trauma from occlusion, when it occurs on a healthy periodontium due
to excessive occlusal forces, is known as primary trauma from
occlusion. This is known to occur when a person bites onto a hard
food substance or as a result of a faulty restoration. Secondary
trauma from occlusion on the other hand occurs in situations where
the periodontium is weak and unable to bear the normal forces of
occlusion (10). In the present
case, the periodontium was healthy and hence, the fractured cusp
may have been due to primary trauma from occlusion. Thus, occlusal
correction followed by the restoration of the cusp was
performed.
Persistent trauma has been known to cause changes in
the periapical region, causing pulp necrosis and leading to acute
periapical abscess or phoenix abscess. In the case presented
herein, the tooth was found to be mobile and an isolated deep
periodontal pocket was found to be associated with the tooth
(7,11). The pulpal infection could have
spread via the lateral canals into the periodontal pocket and lead
to a periodontal abscess (12).
Taking the clinical course and manifestations into consideration,
the case was diagnosed as an endodontic periodontal lesion.
Periodontal abscess drainage followed by endodontic treatment and
the restoration of the involved tooth were carried out.
Therefore, it is critical for a dentist to
recognize, evaluate and treat endodontic periodontal diseases in
this manner. A periodontal abscess is diagnosed according to the
symptoms experienced by the individual, as well as the signs
discovered during the oral examination. In order to improve the
prognosis of patients, the management of periodontal abscess
requires the use of therapeutic modalities carried out under expert
supervision. In the case this condition is left untreated, bacteria
will then accumulate due to the periodontal pocket closure
preventing the gingival crevicular fluid from being cleared.
However, the expulsion of the lysosomal enzymes from hosts
neutrophils is mostly responsible for tissue destruction in
periodontal abscesses. Long standing untreated cases of periodontal
abscess affects the prognosis of the condition, resulting in damage
to the periodontal architecture and osseous framework, resulting in
the exfoliation of teeth.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
RM and SP conceptualized the study. SH substantially
contributed to data interpretation, and RM, SP wrote and prepared
the draft of the manuscript. RM, SP and SH confirm the authenticity
of the raw data. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
The present study was approved by the Institutional
Ethics Committee Manipal College of Dental Sciences (18115),
Mangalore, India. The patient provided consent for his
participation in the study.
Patient consent for publication
The patient provided consent for the publication of
the present case report and any accompanying images.
Competing interests
The authors declare that they have no competing
interests.
Authors’ information
The ORCID IDs of the authors are as follows: RM
(0000-0003-3407-8685), SP (0000-0003-4512-0252) and SH
(0000-0003-0730-0914).
References
|
1
|
Corbet EF: Diagnosis of acute periodontal
lesions. Periodontol 2000. 34:204–216. 2004.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Jaramillo A, Arce RM, Herrera D,
Betancourth M, Botero JE and Contreras A: Clinical and
microbiological characterization of periodontal abscesses. J Clin
Periodontol. 32:1213–1218. 2005.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Herrera D, Roldan S and Sanz M: The
periodontal abscess: A review. J Clin Periodontol. 27:377–386.
2000.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Herrera D, Roldán S, González I and Sanz
M: The periodontal abscess (I). Clinical and microbiological
findings. J Clin Periodontol. 27:387–394. 2000.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Carranza FJ (ed): Carranza's Clinical
Periodontology. 9th edition. Saunders, Philadelphia, PH, pp448-451,
2002.
|
|
6
|
Neff P: Trauma from occlusion: Restorative
concerns. Dent Clin North Am. 39:335–354. 1995.PubMed/NCBI
|
|
7
|
Hallmon WW: Occlusal trauma: Effect and
impact on the periodontium. Ann Periodontol. 4:102–108.
1999.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Herrera D, Alonso B, de Arriba L, Santa
Cruz I, Serrano C and Sanz M: Acute periodontal lesions.
Periodontol 2000. 65:149–177. 2014.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Vályi P and Gorzó I: Periodontal abscess:
Etiology, diagnosis and treatment. Fogorv Sz. 97:151–155.
2004.PubMed/NCBI(In Hungarian).
|
|
10
|
Davies SJ, Gray RJ, Linden GJ and James
JA: Occlusal consideration in periodontics. Br Dent J. 191:597–604.
2001.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Yegin Z, Ileri Z, Tosun G and Sener Y:
Treatment of periodontal abscess caused by occlusal trauma: A case
report. J Pediatr Dent. 1:50–52. 2013.
|
|
12
|
Serio FG and Hawley CE: Periodontal trauma
and mobility. Diagnosis and treatment planning. Dent Clin North Am.
43:37–44. 1999.PubMed/NCBI
|