Introduction
Cerebral palsy is defined as a group of permanent
disorders of movement and posture development due to
non-progressive brain damage during the fetal period or early
childhood, thus causing limitations in activity. Motor disorders in
cerebral palsy are often accompanied by sensory, perceptual,
cognitive, communication, behavioral, epilepsy and secondary
musculoskeletal issues (1). The
global prevalence of cerebral palsy is 1.5-3/1,000 live births,
with spastic cerebral palsy being the most common type, accounting
for 72-80% of recorded cases (2-5).
In Vietnam, it is estimated that ~500,000 individuals live with
cerebral palsy, equivalent to 30-40% of the total disabilities in
children (6). Cerebral palsy is
the most common physical disability in children, often associated
with lifelong multiple disabilities, rendering it a significant
psychological and economic burden for families and societies
worldwide (5).
Due to multiple disabilities, children with cerebral
palsy require rehabilitation across various domains, although in
particular, they require physical therapy, occupational therapy and
speech therapy (5,7). Goal-oriented therapy methods designed
based on motor learning theory and neural plasticity, which train
tasks that are useful for daily life, have proven to be effective
for children with cerebral palsy. Evidence-based practice is
recommended for clinicians to use instead of traditional treatment
methods (8).
The Goal Attainment Scale (GAS), Gross Motor
Function Measure 66 (GMFM 66) and Pediatric Evaluation of
Disability Inventory (PEDI) are widely recognized tools for
assessing functional outcomes in pediatric populations,
particularly in children with motor impairments. GAS is a
patient-centered measure that evaluates individualized goal
achievement, offering a personalized perspective on therapy
outcomes (9-11).
The GMFM 66 quantitatively assesses changes in gross motor
function, particularly in children with cerebral palsy, providing a
reliable measure of motor performance improvements (7). The PEDI evaluates functional
capabilities and performance in daily activities, capturing a
comprehensive view of the independence of a child and caregiver
assistance needs (12,13). These tools collectively provide a
robust framework for assessing the multidimensional impact of
interventions.
Globally, a comprehensive intervention model for
children with cerebral palsy has been established. With a
family-centered approach, clinicians have collaborated to provide
evidence-based practices that meet the diverse treatment needs of
the children (14). In Vietnam,
early detection and early intervention for young children aged
<6 years with disabilities have been identified as key
components of rehabilitation and community-based rehabilitation in
recent years (15). Research has
demonstrated the effectiveness of interventions based on motor
learning theory and neuroplasticity for children with cerebral
palsy (16). During development,
the brains of children exhibit greater neuroplasticity potential
compared with more mature brains, providing enhanced opportunities
for therapeutic interventions (17). The Vietnam Ministry of Health has
incorporated the requirements of the comprehensive rehabilitation
model into the practice philosophy to guide the organization of the
model and improve rehabilitation services for children with
cerebral palsy (7,18-20).
However, early intervention and comprehensive intervention models
for young children with disabilities remain sporadically organized
(15). Studies on cerebral palsy
primarily focus on epidemiological and clinical characteristics or
report outcomes of single rehabilitation methods rather than
studying the effectiveness of a comprehensive goal-oriented and
family-centered rehabilitation model (6,21).
The successful implementation of a comprehensive, goal-directed,
family-centered rehabilitation model for children aged <6 years
with spastic cerebral palsy represents a significant advancement in
both the theory and clinical practice of rehabilitation in Vietnam.
This model has the potential for broad application across
rehabilitation centers nationwide. Therefore, the present study
aimed to fill the current gap by evaluating the simultaneous
effectiveness of interventions in the three main rehabilitation
areas: i) Physical therapy; ii) occupational therapy; and iii)
speech therapy.
Patients and methods
Study design
The present study was a prospective, non-randomized
cohort study using a comprehensive intervention model developed as
part of a rehabilitation training program provided by Humanity and
Inclusion at Hanoi Rehabilitation Hospital (Hanoi, Vietnam) from
January, 2019 to December, 2022.
Study subjects
Participants were children aged <6 years, who
were diagnosed with spastic cerebral palsy and who received
treatment at the Department of Pediatrics of Hanoi Rehabilitation
Hospital. The inclusion criteria for the present study included a
confirmed diagnosis of spastic cerebral palsy according to the
National Institute for Health and Care Excellence and the Vietnam
Ministry of Health guidelines, characterized by motor and postural
disorders due to non-progressive brain damage that occurred before,
during or after birth with increased muscle tone and tendon
reflexes in affected limbs or signs of pyramidal tract damage
(1,18,22,23).
Participants were also required to be in level II, III or IV of the
Gross Motor Function Classification System (GMFCS), level II, III
or IV of the Manual Ability Classification System (MACS; Mini MACS)
and level II, III or IV of the Communication Function
Classification System (CFCS). The GMFCS classifies gross motor
function, focusing on what children with cerebral palsy can achieve
within their living and activity environments (24). The MACS (for ages 4-18 years) and
Mini-MACS (for ages 1-4 years) classify the ability of children
with cerebral palsy to use their hands to manipulate objects in
daily activities (25). The CFCS
categorizes children with cerebral palsy into 5 levels based on
their daily communication abilities, considering 3 factors: i) The
ability to receive and send messages; ii) the pace of communication
with familiar or unfamiliar individuals; and iii) communication
methods such as speech, sound, eye gaze, facial expressions,
gestures, symbols, books, communication boards or assistive devices
(25). Children with hearing
impairment or vision loss and those who either discontinued or
failed to comply with treatment protocols were excluded from the
present study. Participation was voluntary and written informed
consent from the children's guardians was obtained.
Ethical considerations
The present study was approved by The Ethics
Committee of Hanoi Medical University (approval no: 60/HĐĐĐHYHN;
Hanoi, Vietnam). The present study was conducted with the voluntary
consent of the participants' guardians and research subjects could
withdraw from the present study at any stage. All information
obtained was used solely for research purposes.
Measurement of outcomes
GAS (9-11,18).
The GAS is a 5-level goal scale in which a score of -2 represents
the condition of the child at the start of the intervention and a
score of 0 corresponds to the expected outcome after the
intervention. The interpretation of each level is presented in
Table I.
 | Table IGAS scoring. |
Table I
GAS scoring.
| GAS score | Levels of
achievement |
|---|
| -2 | Much less than
expected outcome |
| -1 | Less than expected
outcome |
| 0 | Expected outcome
after intervention |
| +1 | More than expected
outcome |
| +2 | Much more than
expected outcome |
GMFM 66(7)
The GMFM 66 measures gross motor function in
children with cerebral palsy and includes 66 items covering five
domains: i) Lying and rolling (four items); ii) sitting (15 items);
iii) crawling and kneeling (10 items); iv) standing (13 items); and
v) walking, running and jumping (24 items). The GMFM 66 reference
percentile was analyzed from a normal sample of 650 children with
cerebral palsy (24). Higher GMFM
scores indicate greater motor abilities and improved functional
performance.
PEDI (12,13)
The PEDI measures the performance of a child in
everyday activities, administering two parts of the rating scale
including functional skills (FS) and caregiver assistance (CA), and
assessed the following 3 areas: i) Self-care; ii) mobility; and
iii) social function. The PEDI was completed by interviewing the
primary caregiver of the child. The raw score was calculated and
transformed into a scale score. Higher scores reflect greater
independence and reduced need for caregiver assistance, showing
improvement in daily living activities and overall functional
skills.
Comprehensive, goal-oriented and
family-centered rehabilitation model
The development of the model consisted of the
following four steps:
Step 1: Orienting goals based on the needs of the
family: Upon admitting a child with cerebral palsy to the hospital,
the family of the child was provided with information about
cerebral palsy, the treatment model and evidence-based practices
that were suitable for the child and available at the hospital.
Subsequently, the family underwent an in-depth interview with a
clinician, which focused on discussions between the clinician and
the family to understand their goals and expectations when bringing
the child to the hospital. Following the interview, the clinician
helped the family to prioritize these goals for the treatment plan.
After which, the clinician performed the PEDI and collaborated with
the family to establish the intervention goals.
Step 2: Setting GAS goals based on a consensus
between clinicians and the family: Clinicians carried out necessary
evaluations to support the establishment of specific GAS goals.
After these assessments, the clinicians formulated the GAS goals
and discussed the assessment results with the family. This step
involved an agreement with the family to ensure that the GAS goals
align with their expectations and the needs of the child.
Step 3: Planning and conducting the intervention: An
intervention plan detailing training activities, time allocated for
these activities and the roles of clinicians and family in the
intervention was developed. The clinicians performed therapy
sessions with the child at the hospital and guided the family on
conducting the exercises at home.
Step 4: Post-intervention evaluation: Following the
intervention, the clinicians and the family evaluated the
achievement of the GAS goals together. The clinicians then
reassessed the child and provided the family with detailed feedback
on the assessment results and progress.
Key members of the clinician team included a
rehabilitation doctor, physical therapist, occupational therapist
and speech therapist. Additional members, such as a pediatrician or
orthodontist, would be included depending on the condition of the
child. The rehabilitation doctor acted as the team leader,
overseeing all information related to the child, performing the
PEDI by interviewing the primary caregiver of the child, orienting
the intervention goals with the family and re-evaluating the
achievement of the GAS goals after the intervention. Team members
exchanged information on a weekly basis throughout the
implementation process.
Intervention
Children received therapy at the hospital 5
days/week, 3 weeks/month for 6 months. Each session lasted 1.5 h
and included physical therapy (30 min), occupational therapy (30
min) and speech therapy (30 min).
Physical therapy focused on improving gross motor
skills and mobility. Occupational therapy aimed to enhance fine
motor skills and self-care abilities. Speech therapy was targeted
at developing communication and social skills. Goal-directed
therapy techniques were applied, which involved practicing specific
activities based on goals co-designed with the patient. Based on
the principles of motor learning and neuroplasticity, this therapy
emphasizes active and repetitive practice of tasks in real-life
environments or similar simulated settings. Individualized speech
therapy complements this by focusing on developing early
communication skills and enhancing the ability to understand and
express language.
Caregivers carried out at-home exercises according
to the guidance of clinicians, and children were encouraged to
involve themselves in the targeted activities as much as possible.
The length of home exercises varied based on the number and content
of intervention goals. Physical therapy typically lasted 30-60
min/day as guided by the physical therapist. Occupational therapy
included simulated play activities with encouragement to engage in
targeted activities, and speech therapy focused on achieving
intervention goals during daily communication activities.
Data collection
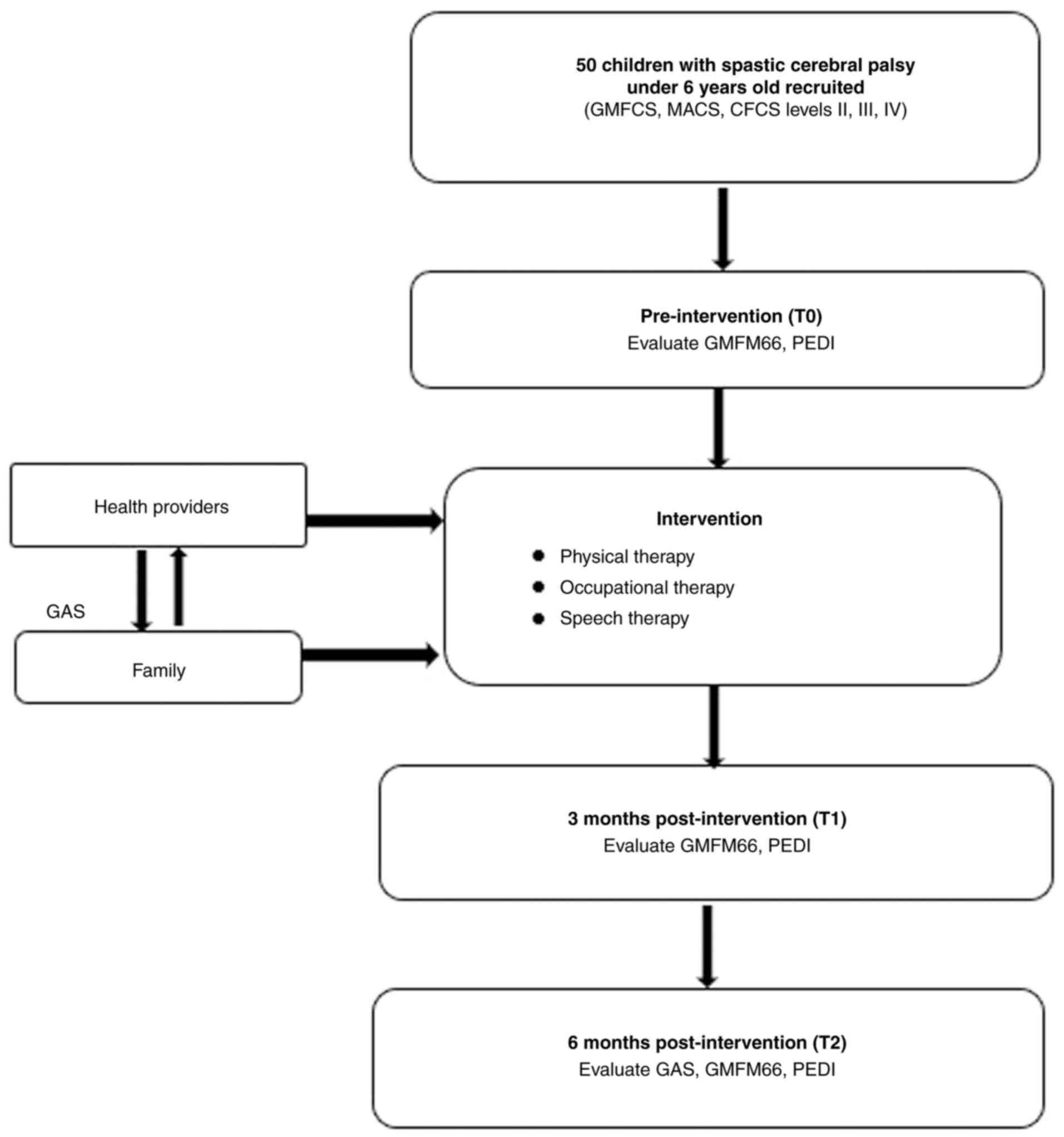
The research process is presented in Fig. 1. Children with cerebral palsy who
met the inclusion criteria underwent a comprehensive clinical
examination. This included interviewing their parents or primary
caregivers to gather information on the medical history and
condition of the child following the research case report template.
GMFCS, MACS/MiniMACS and CFCS levels were also assessed.
The PEDI and GMFM 66 scale were assessed at three
time points: i) Before the intervention (T0); ii) after 3 months
(T1); and iii) after 6 months (T2). The GAS scale criteria,
established by the clinicians, were evaluated after 6 months, with
the goal achievement results assessed in collaboration with the
families of the children with cerebral palsy (Fig. 1).
Statistical analysis
Data entry and analysis were performed using STATA
15.0 software (StataCorp LLC). The Shapiro-Wilk test was used to
test for normality. The Kruskal-Wallis test was used to compare the
differences in intervention results between T0, T1 and T2, followed
by Dunn's test with Bonferroni correction. Spearman's rank
correlation test was used to analyze the correlation between
variables. Linear regression was used to identify factors related
to treatment outcomes. P≤0.05 was considered to indicate a
statistically significant difference.
Results
The demographic and clinical characteristics of the
50 children participating in the present study are presented in
Table II. Among these children,
60% had spastic quadriplegia, 26% had spastic hemiplegia and 14%
had spastic diplegia. The boy-to-girl ratio was 1.94:1, with boys
accounting for 66% of the participants. The average age of the
participants was 39.34 months, with the highest percentage (50%)
being 24-47 months.
 | Table IICharacteristics of the study
participants (n=50). |
Table II
Characteristics of the study
participants (n=50).
| | Site of
paralysis | |
|---|
| Characteristics | Quadriplegia, n
(%) | Hemiplegia, n
(%) | Diplegia, n (%) | Total, n (%) |
|---|
| Sex | | | | |
|
Boys | 21 (70.0) | 7 (53.9) | 5 (71.4) | 33 (66.0) |
|
Girls | 9 (30.0) | 6 (46.2) | 2 (28.6) | 17 (34.0) |
| Age | | | | |
|
≤23
months | 7 (23.4) | 2 (15.4) | 0 | 9 (18.0) |
|
24-47
months | 13 (43.3) | 9 (69.2) | 3 (42.9) | 25 (50.0) |
|
48-71
months | 10 (33.3) | 2 (15.4) | 4 (57.1) | 16 (32.0) |
| GMFCS | | | | |
|
II | 4 (13.4) | 10 (76.9) | 3 (42.9) | 17 (34.0) |
|
III | 13 (43.3) | 3 (23.1) | 4 (57.1) | 20 (40.0) |
|
IV | 13 (43.3) | 0 | 0 | 13 (26.0) |
| Mini MACS | | | | |
|
II | 1 (3.3) | 8 (76.9) | 7 (100.0) | 16 (32.0) |
|
III | 18 (60.0) | 5 (23.1) | 0 | 23 (46.0) |
|
IV | 11 (36.7) | 0 | 0 | 11 (22.0) |
| CFCS | | | | |
|
II | 4 (13.3) | 4 (30.7) | 6 (86.7) | 14 (28.0) |
|
III | 11 (36.7) | 8 (61.5) | 1 (14.3) | 20 (40.0) |
|
IV | 15 (50.0) | 1 (7.7) | 0 | 16 (32.0) |
As regards gross motor function, 34% of the children
were classified as GMFCS level II, 40% as level III and 26% as
level IV. Notably, 43.3% of the children with quadriplegia were in
GMFCS level IV, while none of the children with spastic diplegia or
hemiplegia were at this level.
The MACS (Mini MACS) evaluation of hand use revealed
that 32% of the children were in level II, 46% in level III and 22%
in level IV. No children with hemiplegia were categorized in level
IV and 100% of those with diplegia were at MACS level II.
As regards communication function, 28% had CFCS
level II, 40% had level III and 32% had level IV. Among those with
quadriplegia, 50% were at CFCS level IV, while 61.5% of children
with hemiplegia were at level III and 86.7% of spastic diplegia
cases were at level II (Table
II).
A total of 522 GAS goals were established for
physical therapy and occupational therapy over the 6-month period
of rehabilitation. The achievement rate for physical therapy goals
(levels 0, 1 and 2) was 81.3%, while the achievement rate for
occupational therapy goals was 82.7%. The combined achievement rate
for physical and occupational therapy goals was 100%. As regards
speech therapy, 249 GAS goals were established and 74.7% of the
children achieved the goals (Table
III).
 | Table IIIResults of achieving GAS goals in
physical therapy and occupational therapy after 6 months of
rehabilitation. |
Table III
Results of achieving GAS goals in
physical therapy and occupational therapy after 6 months of
rehabilitation.
| | GAS score |
|---|
| Area | -2 n, (%) | -1 n, (%) | 0 n, (%) | 1 n, (%) | 2 n, (%) | Total, n (%) |
|---|
| Physical
therapy | 15 (5.6) | 35 (13.1) | 120 (44.9) | 61 (22.9) | 36 (13.5) | 267(100) |
| Occupational
therapy | 8 (3.3) | 34 (14.0) | 114 (46.9) | 51 (21.0) | 36 (14.8) | 243(100) |
| Physical and
occupational | 0 (0) | 0 (0) | 6(50) | 5 (41.7) | 1 (8.3) | 12(100) |
| Speech therapy | 18 (7.2) | 45 (18.1) | 95 (38.2) | 58 (23.3) | 33 (13.2) | 249(100) |
The treatment results after 3 months and 6 months of
intervention are presented in Table
IV. The GMFM 66 score increased by 4.9 points at T1 (P=0.09)
and 9.9 points at T2 (P<0.001). The GMFM 66 reference percentile
rose by 17.1 points and 31.1 points after 3 and 6 months,
respectively. Increases of 5.6 points (T1) and 11.0 points (T2)
were observed in the PEDI FS mobility. The PEDI CA mobility was
improved by 7.0 and 12.9 points at T1 and T2, respectively. The
PEDI FS self-care exhibited a gain of 4.7 points following 3 months
of rehabilitation and 8.8 points after 6 months. PEDI CA self-care
increased by 7.2 points at the 3-month assessment and 13.0 points
at 6 months. All differences observed were statistically
significant (P≤0.05). Similarly, the PEDI FS social function
increased by 5.7 points at T1 and 11.1 points at T2. These
improvements were statistically significant. The PEDI CA social
function also showed significant gains, increasing by 7.9 points
after 3 months and 14.8 points after 6 months (P≤0.01).
 | Table IVResults of the intervention
(n=50). |
Table IV
Results of the intervention
(n=50).
| | T0 (mean ± SD) | T1 (mean ± SD) | T2 (mean ± SD) | Pairwise
comparison | Mean
difference | 95% CI | P-value |
|---|
| GMFM 66 | 44.7±12.9 | 49.7±13.9 | 54.7±14.6 | T1-T0 | 4.9 | 4.5-5.3 | 0.09 |
| | | | | T2-T0 | 9.9 | 9.3-10.6 | <0.001 |
| GMFM 66 reference
percentile | 43.52±31.0 | 60.60±33.4 | 74.60±29.0 | T1-T0 | 17.1 | 14.5-19.7 | 0.008 |
| | | | | T2-T0 | 31.1 | 26.2-35.9 | <0.001 |
| PEDI FS
mobility | 41.4±11.7 | 47.1±12.4 | 52.5±13.0 | T1-T0 | 5.6 | 5.3-5.9 | 0.04 |
| | | | | T2-T0 | 11.0 | 10.5-11.6 | <0.001 |
| PEDI CA
mobility | 37.9±12.3 | 44.9±12.2 | 50.8 ±13.1 | T1-T0 | 7.0 | 6.4-7.5 | 0.01 |
| | | | | T2-T0 | 12.9 | 12.2-13.5 | <0.001 |
| PEDI FS
self-care | 39.2±10.4 | 43.9±11.0 | 48.0±11.8 | T1-T0 | 4.7 | 4.5-5.0 | 0.05 |
| | | | | T2-T0 | 8.8 | 8.0-9.6 | 0.03 |
| PEDI CA
self-care | 31.0±14.1 | 38.2±13.5 | 44.0±13.4 | T1-T0 | 7.2 | 6.7-7.7 | <0.001 |
| | | | | T2-T0 | 13.0 | 12.3-13.8 | <0.001 |
| PEDI FS social
function | 40.5±9.2 | 46.2±9.7 | 51.6±10.5 | T1-T0 | 5.7 | 5.4-6.0 | 0.01 |
| | | | | T2-T0 | 11.1 | 10.4-11.8 | <0.001 |
| PEDI CA social
function | 34.3±12.0 | 42.2±11.6 | 49.1±11.8 | T1-T0 | 7.9 | 7.3-8.4 | 0.006 |
| | | | | T2-T0 | 14.8 | 14.0-15.6 | <0.001 |
The results of the multivariable linear regression
model underscored that the site of paralysis and GMFCS levels are
significant predictors of GMFM 66 score improvements, whereas sex,
age and other classifications are insignificantly associated with
the outcome (Table V). Compared
with children with spastic quadriplegic cerebral palsy, those with
hemiplegia showed a significantly greater improvement in GMFM 66
scores (Coef.=1.45; P=0.03). GMFCS levels also significantly
affected GMFM 66 score improvement. In comparison with children
classified as GMFCS level II, those at GMFCS level III presented a
1.37-point lower improvement in GMFM 66 scores (P=0.01), while
children at GMFCS level IV had a 3.97-point lower improvement
(P<0.001).
 | Table VAssociation between age, sex, site of
paralysis, GMFCS level, MACS level and CFCS level, and the
improvement in GMFM 66 scores after six months of
rehabilitation. |
Table V
Association between age, sex, site of
paralysis, GMFCS level, MACS level and CFCS level, and the
improvement in GMFM 66 scores after six months of
rehabilitation.
| Parameters | Coef. | P-value | 95% CI | |
|---|
| Age, months | 0.02 | 0.28 | -0.01 | 0.05 |
| Sex (in reference
to boys) | | | | |
|
Girls | 0.04 | 0.91 | -0.77 | 0.86 |
| Site of paralysis
(in reference to quadriplegia) | | | | |
|
Hemiplegia | 1.45 | 0.03 | 0.18 | 2.72 |
|
Diplegia | 0.59 | 0.52 | -1.22 | 2.40 |
| GMFCS levels (in
reference to level II) | | | | |
|
Level
III | -1.37 | 0.01 | -2.35 | -0.39 |
|
Level
IV | -3.97 | <0.001 | -5.41 | -2.53 |
| MACS levels (in
reference to level II) | | | | |
|
Level
III | -0.47 | 0.47 | -1.75 | 0.82 |
|
Level
IV | -0.23 | 0.78 | -1.88 | 1.42 |
| CFCS levels (in
reference to level II) | | | | |
|
Level
III | 0.24 | 0.65 | -0.82 | 1.31 |
|
Level
IV | 0.44 | 0.50 | -0.88 | 1.76 |
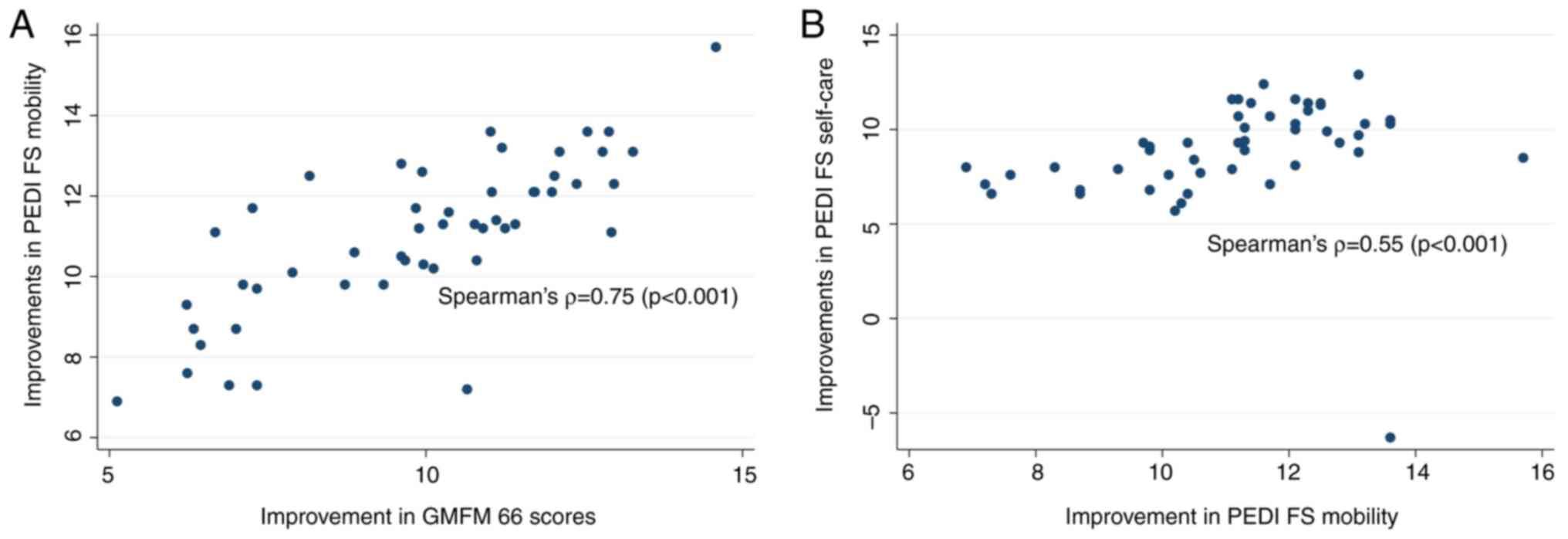
There was a strong positive correlation between the
improvement in GMFM 66 scores and the improvement in PEDI FS
mobility scores after 6 months of rehabilitation (P<0.001),
suggesting the improvement of PEDI FS mobility scores as GMFM 66
scores increased. Additionally, there was a moderate positive
correlation (r=0.55) between the improvement in PEDI FS mobility
scores and PEDI FS self-care scores (P<0.001), implying that
improvements in mobility skills are associated with enhancements in
self-care abilities (Fig. 2).
Discussion
As regards physical therapy and occupational
therapy, the results of achieving GAS goals in the present study
were similar to the results presented in the study by Storvold and
Jahnsen (27) (82.86%) and Lowing
et al (26) (84.55%) in
terms of mobility and self-care goals. In the present study,
several goals of coordination between physical therapy and
occupational therapy were established. The role of teamwork in the
rehabilitation process for children with cerebral palsy has been
promoted to achieve the desired goals of the child and family. To
ensure the validity and reliability of the GAS, all healthcare
staff who directly interacted with the children had >1 year of
experience and were trained in a GAS goal setting. Therapists
worked with families to establish GAS goals, while rehabilitation
doctors evaluated standard scales and collaborated with families to
assess the achievement of these goals.
An intensive intervention program (>3
sessions/week), including goal-directed therapy, has been shown to
effectively improve gross motor function in children with cerebral
palsy (27-31).
The GMFM 66 results from the present study are lower than the study
by Storvold and Jahnsen (27)
where a 6-week, 5 days/week and 10 h/week, intervention at the
rehabilitation center combined with home and school exercises
increased GMFM 66 scores by 10.79 points for children with GMFCS
levels I and II (27). Similarly,
Sorsdahl et al (32)
reported a 4.5-point increase after a 3-week, 5 days/week and 3
h/day intervention for children with GMFCS levels I-IV (32). These differences may be attributed
to variations in participant selection and intervention intensity,
as the present study selected children with more severe GMFCS
(levels II, III and IV) and possibly lower intervention dosage
compared with the other studies. By contrast, Lowing et al
(26) reported an increase of 5.02
points after 3 months of intervention for 22 children with GMFCS
levels I-IV, and are higher compared with the study by Ahl et
al (30) who found a
3.13-point increase after 5 months of goal-directed therapy for 14
children with GMFCS levels II-V (26,30).
In both studies, children exercised at the center once/week and the
remainder of the time at home.
Overall, studies on goal-directed therapy show that
children with cerebral palsy were all actively engaged in treatment
>3 times/week. The specific intervention dosage and whether the
intervention is conducted by healthcare professionals or the
primary caregivers of the child with cerebral palsy may vary
depending on the study. The results of these studies demonstrate
that children with cerebral palsy exhibit improvements following
intervention. However, the level of progress appears to be
influenced by the treatment dosage. Higher dosage treatments, such
as in the studies by Storvold and Jahnsen (27) and Sorsdahl et al (32) are more likely to record improved
progress. Additionally, the GMFCS level may also be related to
treatment effectiveness.
In studies on the effectiveness of goal-directed
therapy and comparing GMFM 66 scores, studies without control
groups also use the GMFM 66 reference percentile. The GMFM 66
reference percentile helps to assess the relative motor ability of
the study subjects compared with children with cerebral palsy of
the same age and GMFCS level. An increase in the GMFM 66 reference
percentile score following intervention indicates that the child
has made significant progress in gross motor function following the
intervention, as their progress surpasses that of the standard
sample. In the present study, at T1 and T2, all children showed an
increase in the GMFM 66 reference percentile scores compared with
T0. Additionally, after 3 months of intervention, the reference
percentile scores increased by an average of 17.1 points, and after
6 months, they increased by 31.1 points. The present study results
are consistent with Lowing et al (26) where the GMFM 66 reference
percentile score increased by 18 points after 3 months, and
Storvold and Jahnsen (27) in
which the GMFM 66 reference percentile scores increased from 15 to
37 points after 6 weeks.
The results of the present study are similar to
those of the study by Sorsdahl et al (32) who found that the GMFM 66 score of
children with cerebral palsy GMFCS levels I and II improved more
than levels III, IV and V after 3 weeks of intervention. However,
the current results are different from Lowing et al
(26) which reported that after 3
months of rehabilitation, the gross motor ability of children with
cerebral palsy improved but did not correlate to the level of
GMFCS. Considering the site of paralysis, the present findings are
also similar to the research results of Storvold and Jahnsen
(27) where children with spastic
quadriplegia showed less improvement in GMFM 66 scores compared
with children with spastic hemiparesis.
The improvement of the PEDI FS mobility scores in
the present study is similar to the results of the study by Lowing
et al (26), which reported
an increase of 5.85 points in PEDI FS mobility after 3 months of
intervention. However, the improvement in PEDI CA mobility was 9.4
points, higher than the results of the present study.
The improvement of the PEDI FS self-care of children
with cerebral palsy in the present study is similar to the research
results of Ahl et al (30)
and Lowing et al (26)
after 3 months, however, they reported a higher level of
improvement in the PEDI level of assistance in self-care skills, at
10.99 points. These differences may be because in Vietnam, families
typically help children with cerebral palsy more in mobility and
self-care activities.
While the GMFM 66 measures gross motor function, it
does not capture how these abilities translate into functional
mobility in daily life, such as moving on a bed, using a
wheelchair, navigating indoors or moving outdoors (28). Therefore, to evaluate the
effectiveness of goal-directed therapy, where goals are tied to
specific and practical daily activities, researchers often combine
the GMFM 66, PEDI mobility domain and the GAS scores (27,32).
By combining different assessment tools, a comprehensive
understanding of the motor and mobility capabilities of the child
in the therapy room, at home and in the community can be assessed,
thus providing a holistic evaluation of the effectiveness of
goal-directed therapy for children with cerebral palsy.
Han et al (33) found a strong correlation (r=0.83)
between the GMFM 66 and PEDI FS mobility scores in children with
spastic cerebral palsy aged 1-6 years, which aligns with the
findings of the present study (33). In the present study, a greater
improvement in GMFM-66 scores was associated with higher
improvement in PEDI FS mobility.
Improvements in PEDI FS mobility and PEDI FS
self-care are positively correlated (r=0.55; P<0.001). This
result indicates that in a rehabilitation model combining physical
and occupational therapy, children with cerebral palsy tend to make
simultaneous progress in both mobility and self-care skills.
As regards speech therapy, 249 GAS goals were
established and 74.7% of the children achieved the goals. The PEDI
FS social function and PEDI CA social function in the present study
at the 3-month mark improved more than the research results of
Sorsdahl et al (32),
Lowing et al (26) and Ahl
et al (30). This may be
because the participants in the present study received
goal-directed physiotherapy, occupational therapy and speech
therapy simultaneously.
The findings of the present study have some
implications for clinical practice and future research.
Rehabilitation centers should implement a comprehensive,
goal-directed and family-centered rehabilitation model for children
with cerebral palsy. Additionally, further research is required to
assess how family training programs affect the knowledge, attitudes
and practices of guardians. Based on these evaluations, treatment
programs can be developed to enhance the duration of home-based
practice while reducing the time spent in hospital-based
therapy.
The results of the present study should be
considered in light of several limitations. First, a control group
or pre-intervention follow-up were not included, which means that
the natural progression of functional development over time could
not be entirely ruled out as a factor influencing the observed
improvements in children with cerebral palsy. In addition, the
study did not comprehensively assess co-existing health issues,
such as intellectual disabilities and speech difficulties, which
could affect the ability of children to learn motor skills and
communicate effectively. Another limitation is that the present
study mainly evaluated the functional improvement of children with
cerebral palsy after intervention in each area, and thus the
association between the effectiveness of intervention methods in
the comprehensive intervention model has not been analyzed
in-depth. It should also be noted that implementing a comprehensive
intervention model requires time and resources, such as developing
an information system on cerebral palsy to provide to families and
creating tools to simulate real-life activities. Rehabilitation
centers in Vietnam are still facing a shortage of personnel,
especially in the areas of occupational therapy and speech therapy
(19,20). Therefore, it is essential to
strengthen workforce training, conduct workshops and expand the
model.
In conclusion, the comprehensive, goal-directed and
family-centered rehabilitation model is effective for children
<6 years old with spastic cerebral palsy.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
KCH and VMP conceived and designed the study,
performed statistical analysis and interpretation of the data, were
involved in the investigative aspects of the study, and wrote,
reviewed and edited the manuscript. Both authors read and approved
the final version of the manuscript. KCH and VMP confirm the
authenticity of all the raw data.
Ethics approval and consent to
participate
The present study was approved by The Ethics
Committee of Hanoi Medical University (approval no.: 60/HĐĐĐHYHN;
Hanoi, Vietnam). The research was conducted with the voluntary
consent of the participants' guardians. Research subjects could
withdraw from the study at any stage and all information obtained
was used solely for research purposes.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Rosenbaum P, Paneth N, Leviton A,
Goldstein M, Bax M, Damiano D, Dan B and Jacobsson B: A report: The
definition and classification of cerebral palsy April 2006. Dev Med
Child Neurol Suppl. 109:8–14. 2007.PubMed/NCBI
|
|
2
|
Chauhan A and Singh M, Jaiswal N, Agarwal
A, Sahu JK and Singh M: Prevalence of cerebral palsy in Indian
Children: A systematic review and Meta-analysis. Indian J Pediatr.
86:1124–1130. 2019.PubMed/NCBI View Article : Google Scholar
|
|
3
|
McManus V, Guillem P, Surman G and Cans C:
SCPE work, standardization and definition-an overview of the
activities of SCPE: A collaboration of european CP registers.
Zhongguo Dang Dai Er Ke Za Zhi. 8:261–265. 2006.PubMed/NCBI
|
|
4
|
Sellier E, Platt MJ, Andersen GL,
Krägeloh-Mann I, De La Cruz J and Cans C: Surveillance of Cerebral
Palsy Network. Decreasing prevalence in cerebral palsy: A
Multi-site European population-based study, 1980 to 2003. Dev Med
Child Neurol. 58:85–92. 2016.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Liptak GS and Accardo PJ: Health and
social outcomes of children with cerebral palsy. J Pediatr. 145 (2
Suppl):S36–S41. 2004.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Khandaker G, Van Bang N, Dung TQ, Giang
NTH, Chau CM, Van Anh NT, Van Thuong N, Badawi N and Elliott EJ:
Protocol for hospital based-surveillance of cerebral palsy (CP) in
Hanoi using the paediatric active enhanced disease surveillance
mechanism (PAEDS-Vietnam): A study towards developing
Hospital-based disease surveillance in Vietnam. BMJ Open.
7(e017742)2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Department of Medical Service
Administration: Guidelines for Diagnosis, Treatment, and Functional
Rehabilitation for Children with Cerebral Palsy-Guidelines on
Physical Therapy. J 2018.
|
|
8
|
Novak I, McIntyre S, Morgan C, Campbell L,
Dark L, Morton N, Stumbles E, Wilson SA and Goldsmith S: A
systematic review of interventions for children with cerebral
palsy: State of the evidence. Dev Med Child Neurol. 55:885–910.
2013.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Goal Attainment Scaling: Applications,
Theory, and Measurement. Psychology Press, New York, 2014.
|
|
10
|
Hurn J, Kneebone I and Cropley M: Goal
setting as an outcome measure: A systematic review. Clin Rehabil.
20:756–772. 2006.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Turner-Stokes L: Goal attainment scaling
(GAS) in rehabilitation: A practical guide. Clin Rehabil.
23:362–370. 2009.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Berg M, Jahnsen R, Froslie KF and Hussain
A: Reliability of the pediatric evaluation of disability inventory
(PEDI). Phys Occup Ther Pediatr. 24:61–77. 2004.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Berg MM, Dolva AS, Kleiven J and
Krumlinde-Sundholm L: Normative scores for the pediatric evaluation
of disability inventory in norway. Phys Occup Ther Pediatr.
36:131–143. 2016.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Schwabe AL: Comprehensive care in cerebral
palsy. Phys Med Rehabil Clin N Am. 31:1–13. 2020.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Department of Medical Service
Administration: Guidelines for Early Detection-Early Intervention
for Children's Disabilities. J 2023.
|
|
16
|
Novak I, Morgan C, Fahey M,
Finch-Edmondson M, Galea C, Hines A, Langdon K, Namara MM, Paton
MC, Popat H, et al: State of the evidence traffic lights 2019:
systematic review of interventions for preventing and treating
children with cerebral palsy. Curr Neurol Neurosci Rep.
20(3)2020.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Johnston MV: Plasticity in the developing
brain: Implications for rehabilitation. Dev Disabil Res Rev.
15:94–101. 2009.PubMed/NCBI View
Article : Google Scholar
|
|
18
|
Department of Medical Service
Administration: Guidelines for Diagnosis, Treatment, and Functional
Rehabilitation for Children with Cerebral Palsy. General
Guidelines. J 2018.
|
|
19
|
Department of Medical Service
Administration: Guidelines for Diagnosis, Treatment, and Functional
Rehabilitation for Children with Cerebral Palsy. Guidelines on
Occupational Therapy. J 2018.
|
|
20
|
Department of Medical Service
Administration: Guidelines for Diagnosis, Treatment, and Functional
Rehabilitation for Children with Cerebral Palsy. Guidelines on
Speech Therapy. J 2020.
|
|
21
|
Pham VM, Hoang TL, Hoang KC, Nguyen NM,
DeLuca SC and Coker-Bolt P: The effect of constraint-induced
movement therapy for children with hemiplegic cerebral palsy in
Vietnam. Disabil Rehabil. 47:912–918. 2025.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Wallace SJ: Epilepsy in cerebral palsy.
Dev Med Child Neurol. 43:713–717. 2001.PubMed/NCBI View Article : Google Scholar
|
|
23
|
National Institute for Health and Care
Excellence: Cerebral palsy in under 25s: Assessment and management
(NG62). https://www.nice.org.uk/guidance/ng62.
|
|
24
|
Hanna SE, Bartlett DJ, Rivard LM and
Russell DJ: Reference curves for the Gross Motor Function Measure:
Percentiles for clinical description and tracking over time among
children with cerebral palsy. Phys Ther. 88:596–607.
2008.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Eliasson AC, Krumlinde-Sundholm L, Rösblad
B, Beckung E, Arner M, Ohrvall AM and Rosenbaum P: The manual
ability classification system (MACS) for children with cerebral
palsy: Scale development and evidence of validity and reliability.
Dev Med Child Neurol. 48:549–554. 2006.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Lowing K, Bexelius A and Brogren Carlberg
E: Activity focused and goal directed therapy for children with
cerebral palsy-do goals make a difference? Disabil Rehabil.
31:1808–1816. 2009.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Storvold GV and Jahnsen R: Intensive motor
skills training program combining group and individual sessions for
children with cerebral palsy. Pediatr Phys Ther. 22:150–159.
2010.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Rahlin M, Duncan B, Howe CL and Pottinger
HL: How does the intensity of physical therapy affect the Gross
Motor Function Measure (GMFM-66) total score in children with
cerebral palsy? A systematic review protocol. BMJ Open.
10(e036630)2020.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Arpino C, Vescio MF, De Luca A and
Curatolo P: Efficacy of intensive versus nonintensive physiotherapy
in children with cerebral palsy: A meta-analysis. Int J Rehabil
Res. 33:165–171. 2010.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Ahl LE, Johansson E, Granat T and Carlberg
EB: Functional therapy for children with cerebral palsy: An
ecological approach. Dev Med Child Neurol. 47:613–619.
2005.PubMed/NCBI
|
|
31
|
Bower E and McLellan DL: Effect of
increased exposure to physiotherapy on skill acquisition of
children with cerebral palsy. Dev Med Child Neurol. 34:25–39.
1992.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Sorsdahl AB, Moe-Nilssen R, Kaale HK,
Rieber J and Strand LI: Change in basic motor abilities, quality of
movement and everyday activities following intensive,
goal-directed, activity-focused physiotherapy in a group setting
for children with cerebral palsy. BMC Pediatr.
10(26)2010.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Han T, Gray N, Vasquez MM, Zou LP, Shen K
and Duncan B: Comparison of the GMFM-66 and the PEDI Functional
Skills Mobility domain in a group of Chinese children with cerebral
palsy. Child Care Health Dev. 37:398–403. 2011.PubMed/NCBI View Article : Google Scholar
|