Introduction
Shock wave lithotripsy (SWL), trauma and renal
angiographic procedures are all known to cause renal hematoma
(1). However, a renal hematoma may
also occur spontaneously in patients with a malignancy or in
patients receiving anticoagulation therapy. Although the incidence
is rare, the occurrence of a renal hematoma can be fatal (2). Ureteroscopic lithotripsy (URSL) as a
transurethral, minimally invasive and efficient procedure has
become a regular operation for treatment of ureteral calculi. For
example, the ureteroscopic holmium laser lithotripsy is the current
technique of choice for the treatment of ureteric stones (3). The postoperative complication rate of
URSL is low, with the most frequent complication being a fever
(4,5). Therefore, it is easy for urological
surgeons to neglect or be unaware of a subcapsular renal hematoma
(SRH) as a rare complication following URSL therapy.
With a kidney fracture or spontaneous renal
hemorrhage, SRH will occur. It can cause hemorrhagic shock when the
active bleeding fails to be prevented. Even when the active
bleeding is controlled, the SRH will lead to high blood pressure
and subsequent renal failure since the active subcapsular bleeding
will accumulate around the kidney and compressed it for a
substantial amount of time. Engel and Page (6) first reported a clinical case of
hypertension caused by subcapsular renal hematoma and it improved
following nephrectomy. The present study reports such a case, in
which a young male patient suffered from a SRH two days after
undergoing failed URSL therapy with a holmium laser (UHL).
Case report
Written informed consent was obtained from the
patient, a 24-year-old male patient, complaining of distending pain
in the left lumber region for 10 days and diagnosed with moderate
dilatation of the upper ureter, left hydronephrosis and left kidney
stones by ultrasonography, who was admitted to Zhongnan Hospital
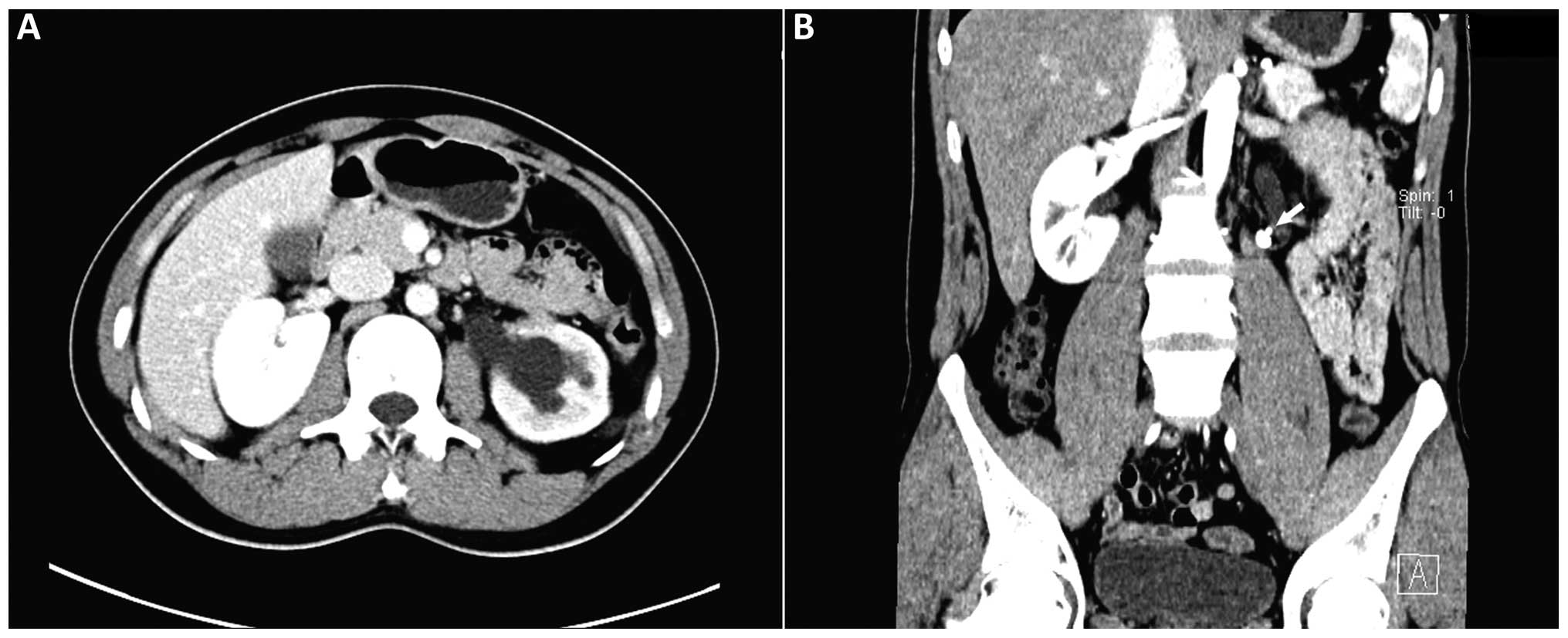
(Wuhan, China). A contrast-enhanced computerized tomography (CT)
scan confirmed two calculi in the left proximal ureter, which
measured 1×0.8×0.5 cm and 0.5×0.5×0.8 cm, and moderate left
hydronephrosis (Fig. 1). In
addition, the contrast-enhanced CT scan revealed good renal
parenchyma and function. The patient had undergone a successful UHL
due to the identification of a left ureteral calculus three years
previously; however, the patient had no other disease.
Holmium laser lithotripsy (PowerSuite 60 W; Lumenis,
Inc., San Jose, CA, USA) under a rigid ureteroscope was recommended
for treatment. Following the administration of intravenous
anesthesia (remifentanil, 2 µg/kg; Rui Jie Ren Fu Inc., Yi Chang,
China and propofol, 1.0 mg/kg; De Pu Li Ma; AstraZeneca, Shanghai,
China), the patient was placed in the lithotomy position. A super
lubricious guide wire (ureteral safety wire guide introducer set;
Cook Urological Inc; Spencer, IN, USA) was inserted into the left
ureter though the ureteral orifice, after which a 6.5-F rigid
tapered ureteroscope (Richard Wolf Medical Instruments Corporation,
Vernon Hills, IL, USA) was advanced forward slowly and carefully
until the stones were located. However, the treatment failed to
fragment the stones completely even when the repetition rate of the
laser energy was increased from 35 to 40 Hz. In addition, the
bigger stone moved to the pelvis, while the smaller calculus was
crushed. To force the stone to move out from the renal pelvis,
intravenous administration of 20 mg furosemide (Luo Fu Shang Zhu
She Ye, Luo Fu Shang Guo Yao Inc., Guangzhou, China) was applied,
and a lower hip position and a high flushing pressure of the
irrigation system were responded empirically. However, the stone
was ultimately lost in the endoscopic view. A 5 FR-26-cm Double J
stent (ureteral stents 7F; Bard International Inc., Karlsruhe,
Germany) was placed routinely and the procedure was terminated.
At 22:30 on the following day, the patient
complained of pain in the left lumber region; thus, diclofenac
sodium suppositories were applied as a symptomatic treatment. After
2 h, the pain returned and a somatoscopy indicated abdominal
tenderness and rebound pain. Considering the diagnosis of an acute
abdomen initially, an emergency examination was conducted. The
routine blood tests revealed a blood leukocyte count of
13.30×109/l and a hemoglobin level of 90 g/l. The
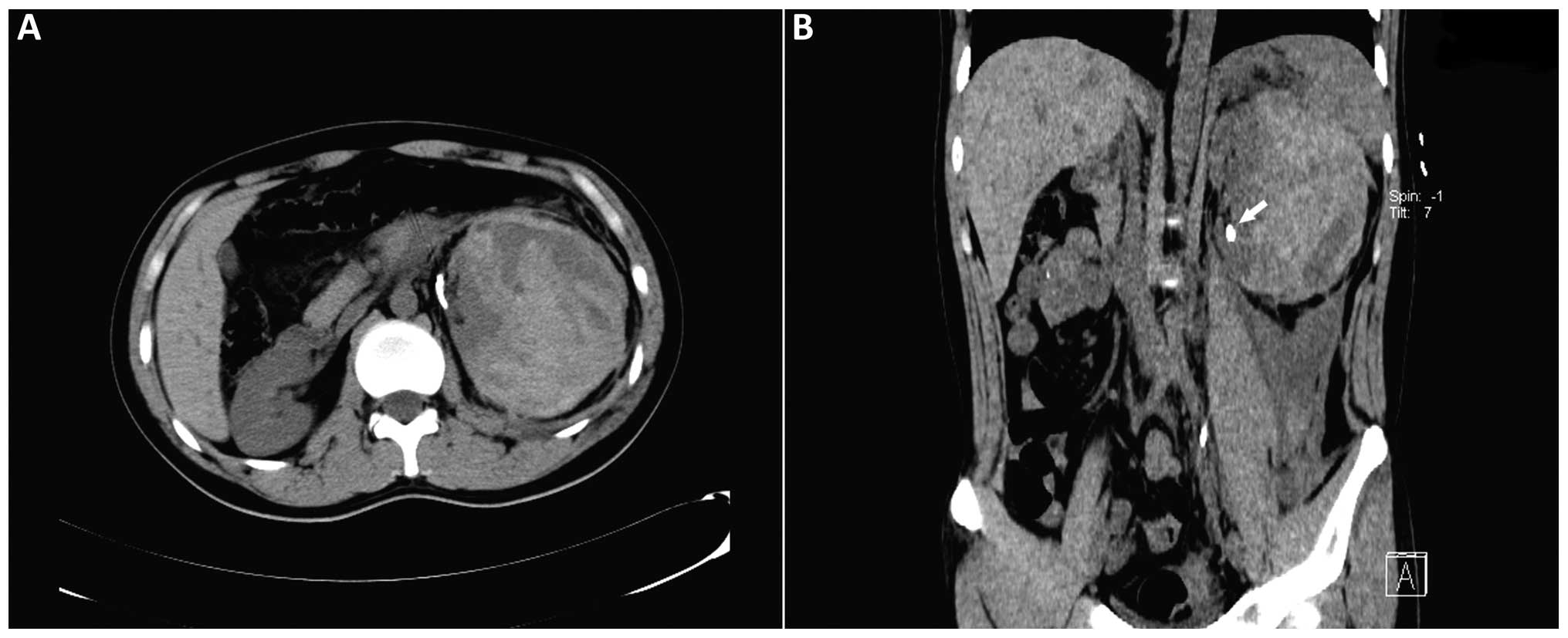
emergent abdominal CT scan revealed a huge subcapsular hematoma
(11×14×11 cm) of the left kidney and the stone in the renal pelvis
from the left proximal ureter (Fig.
2). Vital signs, urine volume and routine blood tests were
monitored, and 500 ml hydroxyethyl starch (Nanjing Zhengda Tianqing
Pharmaceutical Co. Ltd., Nanjing, China) (intravenously guttae), 2
mg tramadol (Shu Min Grunenthal GmbH, Aachen, Germany)
(intramuscular), 4 g piperacillin-tazobactam (Tazocin; Wyeth
Lederle SPA Inc., Catania, Italy), 250 ml normal saline (Sheng Li
Iv Hua Na Rong Ye, Cheng Xin Yao Ye Inc., Shang Dong, China)
(intravenously guttae) and 4 units Hemocoagulase Agkistrodon
(Shu Ning, Kang Cheng Yao Ye Inc., Beijing, China) (intravenously
guttae) were applied immediately. The patient was shown to respond
to the conservative management, and the hemoglobin level remained
at 82 g/l over the subsequent 12 h. The patient presented with a
low-grade fever (37.5°C) over several days as a result of hematoma
absorption; however, further hospitalization was uneventful. After
3 weeks, a CT scan clearly showed that the left kidney was
compressed to one side by the large surrounding unabsorbed
hematoma. The patient attended a six-month follow-up once out of
hospital and no particular event was found. In this case, however,
the large SRH was mostly absorbed after six months and no evident
hypertension or renal failure occurred. The invasive operation for
the remaining hematoma was not considered, although this may have
been due to the young and healthy condition of the patient.
Discussion
When a SRH occurs, the renal parenchyma is usually
compressed by the hemorrhage filled in the subcapsular area of the
kidney, which is a potential space where fluid can accumulate
(2). Furthermore, no coagulation
disorders or other diseases that cause bleeding were identified in
the present case and the possibility of spontaneous SRH was low
(1,2). Recently, URSL has become a common
technique for the treatment of ureteric stones due to the low
complication and high relative efficiency rates (4,5).
However, the presence of a SRH following URSL therapy has been
rarely reported in the literature; thus, understanding this
potential fatal risk is of great clinical significance (7).
In the present study, the clinical presentations and
conservative treatment of a SRH following a failed UHL procedure in
a young male patient were discussed. The sudden onset of severe
pain in the flank was associated with the appearance of a SRH and
the presentation of acute abdomen; abdominal tenderness and rebound
pain following surgery were major clinical presentations in the
patient. The hemoglobin level decreased markedly and the patient
presented signs of blood loss. In general, contrast-enhanced CT
scans were required for a confirmed diagnosis, in which the extent
of the renal injuries and the diameter of the hematoma were
assessed accurately, and the presence of active bleeding was
determined. On an enhanced CT scan, an irregular, heterogeneous
area around the kidney, with an attenuation value less than that of
the artery or renal parenchyma, is known to indicate a SRH without
active bleeding (8). In the present
case, CT imaging was undertaken to clarify the diagnosis of an
acute abdomen as quickly as possible, since a similar case had not
been experienced previously, and the bleeding was controlled under
a conservative management regimen.
In the patient discussed in the present study, there
was no evident trauma caused by the UHL, even though the ureteric
stone was unable to be fragmented and ultimately moved to the renal
pelvis. However, it was hypothesized that the wire used to guide
the rigid ureteroscope increased the intrarenal pressure, which led
to forniceal rupture and separation of the capsule from the
parenchyma, and subsequently the development of a hematoma. No
coagulation disorders or other diseases that cause bleeding were
identified in the present case, spontaneously SRH may be not.
Treatment protocols for SRH should be discussed.
When patients are without signs for active bleeding, a conservative
manner should be used to treat the SRH (1,9). With
the exception of contrast-enhanced CT, CT scan, ultrasound, routine
blood tests and coagulation status, creatinine levels, blood urea
nitrogen levels, electrolyte balance and urine tests should be
included in diagnostics (1).
Krishnamurthi and Streem found that the mean time of hematoma
resolution was 13.2 months following conservative treatment,
without adverse effects on blood pressure or renal function
(9). However, the SRH cases included
in this prospective study were small (<5 cm). Engel and Page
were the first to describe a clinical case of hypertension caused
by SRH, which improved following a nephrectomy. A subcapsular
hematoma usually compressed the kidney and was associated with high
blood pressure and occasional renal failure in the patient
(6). Percutaneous drainage or the
use of percutaneous pigtail catheters, laparoscopic decortication,
or the combined use of percutaneous drainage and urokinase
injection may promote hematoma resolution in patients with stable
vital signs; however, this therapy may induce unbearable pain or
renal compression even with a solitary kidney (10). When active bleeding fails to be
controlled by conservative management, or when there are unstable
signs of blood loss, a quick and efficient treatment method should
be conducted, such as a superselective embolization under renal
artery digital subtraction angiography or open surgery (11). In the present case, due to the stable
hematoma without evidence of active bleeding and the positive
response to conservative management, invasive surgery to drain and
eliminate the hematoma was not undertaken. The patient was required
to undergo a 6-month follow-up.
In conclusion, not only SWL, trauma and renal
angiographic procedures are causative factors for a renal hematoma.
SRH should be considered as a complication following URSL, even
though occurrence is not common.
References
|
1
|
Schnabel MJ, Gierth M, Chaussy CG, Dötzer
K, Burger M and Fritsche HM: Incidence and risk factors of renal
hematoma: A prospective study of 1,300 SWL treatments.
Urolithiasis. 42:247–253. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Chao YC, Ming HL, Yeu CC and Sun YC:
Spontaneous bilateral renal subcapsular hematoma as a possible
complication of myeloproliferative disorders. J Med Sci.
29:273–275. 2009.
|
|
3
|
Seitz C, Tanovic E, Kikic Z and Fajkovic
H: Impact of stone size, location, composition, impaction, and
hydronephrosis on the efficacy of holmium:YAG-laser
ureterolithotripsy. Eur Urol. 52:1751–1757. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
de la Rosette J, Denstedt J, Geavlete P,
et al: The clinical research office of the endourological society
ureteroscopy global study: Indications, complications and outcomes
in 11,885 patients. J Endourol. 28:131–139. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Chiu PK, Chan CK, Ma WK, To KC, Cheung FK
and Yiu MK: Subcapsular hematoma after ureteroscopy and laser
lithotripsy. J Endourol. 27:1115–1119. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Engel WJ and Page IH: Hypertension due to
renal compression resulting from subcapsular hematoma. J Urol.
73:735–739. 1955.PubMed/NCBI
|
|
7
|
Meng H, Chen S, Chen G, Tan F, Wang C and
Shen B: Renal subcapsular hemorrhage complicating
ureterolithotripsy: An unknown complication of a known day-to-day
procedure. Urol Int. 91:335–339. 2013.PubMed/NCBI
|
|
8
|
Belville JS, Morgentaler A, Loughlin KR
and Tumeh SS: Spontaneous perinephric and subcapsular renal
hemorrhage: Evaluation with CT, US and angiography. Radiology.
172:733–738. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Krishnamurthi V and Streem SB: Long-term
radiographic and functional outcome of extracorporeal shock wave
lithotripsy induced perirenal hematomas. J Urol. 154:1673–1675.
1995. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Xu L and Li G: Life-threatening
subcapsular renal hematoma after flexible ureteroscopic laser
lithotripsy: Treatment with superselective renal arterial
embolization. Urolithiasis. 41:449–451. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Shen Z, He W, Liu D, Pan F, Li W, Han X
and Li B: Novel technique for the treatment of large subcapsular
renal hematoma: Combined use of percutaneous drainage and urokinase
injection. Int Urol Nephrol. 46:1751–1755. 2014. View Article : Google Scholar : PubMed/NCBI
|