Introduction
Retinal artery occlusion is a common eye disease,
which is classified into central retinal artery occlusion (CRAO),
branch retinal artery occlusion and ciliary retinal artery
occlusion. CRAO is the most commonly occurring type of retinal
artery occlusion, and is a disease of the eye that leads to sudden,
acute and painless sight loss with poor prognosis. The main causes
of CRAO are arteriosclerosis, embolus and inflammation (1–4).
As part of the nervous system of the brain, the
central retinal artery is sensitive to hypoxia. When occlusion of
the retinal artery occurs, blood supplies to the inner retina are
blocked, leading to ischemia and necrosis of the inner retina, or
even acute ischemic necrosis of the nerve fiber and ganglion cell
layers. In addition, lesions of varying severity may occur in the
retinal inner nuclear and inner plexiform layers. Nutrition is
provided to the retinal visual cell layer by the choriocapillaris
formed by the ciliary artery. Therefore, retinal visual cells
retain their integrity at the early stage of CRAO, but begin to
shrink at the late stage. The ciliary retinal artery is crucial for
the protection of vision. The effect of ciliary retinal artery
occlusion on vision is dependent on the size of the macular area
supplied by the artery (2).
CRAO can be easily diagnosed by fundoscopic
examination, and timely treatment is crucial for the alleviation of
CRAO (5–8). In the present study, the fundus
fluorescein angiography (FFA) results of CRAO patients attending
the Tianjin Eye Hospital (Heping, China) were retrospectively
investigated. The association between FFA and central visual
impairment was analyzed, and the results may provide a basis for
the clinical treatment and prognosis of CRAO.
Materials and methods
Patients
This study included 63 patients (63 eyes) who were
diagnosed with CRAO by fundoscopic examination and FFA at the
Tianjin Eye Hospital (Heping, China) between September 2010 and
March 2014, including 28 males and 35 females (aged 43–75 years,
with an average of 56.51 years). The time period between the time
point at which the patient was aware of a sudden deterioration of
vision and admission to our hospital was 1–15 days, with an average
of 6.07 days. Among these patients, 44 cases had hypertension, 12
cases suffered from diabetes, and 9 cases had carotid stenosis or
plaque. Exclusion criteria were: Ciliary retinal artery macula;
heart rate outside 60–100 bpm and blood pressure outside
90–140/60–90 mmHg, which are the allowed ranges for radiography;
and history of trauma, surgery, oxygen inhalation or retrobulbar
injection of drugs. All procedures were approved by the Ethics
Committee of Nankai University (Tianjin, China). Informed consent
was obtained from all patients or their families.
Central vision detection
Visual dysfunction is classified into severe, mild
and light degrees (9). Patients with
a severe degree of visual dysfunction cannot sense light or can
only sense a hand movement in front of the eye; those with mild
visual dysfunction can count the number of fingers or have a visual
acuity of 0–0.08; those with light visual dysfunction have a visual
acuity >0.1.
FFA examination
Tropicamide was administered for mydriasis. FFA
examination was performed using Heidelberg retinal tomography, with
the observation time of radiography being 10–15 min (10). Sodium fluorescein (0.6 g; Zhongheng
Pharmaceuticals, Guangzhou, China) was dissolved in 2 ml sterile
normal saline, and administered by intravenous infusion using a 22G
needle within 5 sec. The starting time of central retinal artery
perfusion and the time of the appearance of retinal vein laminar
flow were recorded. The difference between the two time points was
considered as the retinal arteriovenous phase.
Statistical analysis
All statistical analyses were performed using SPSS
software, version 10.0 (SPSS, Inc., Chicago, IL, USA). The genders
of the patients were analyzed using the χ2 test. Ages
and the courses of disease were compared using analysis of variance
(ANOVA). P<0.05 was considered to indicate a statistically
significant difference.
Results
Fundus performance evaluation for
preliminary CRAO diagnosis
Prior to the diagnosis of CRAO, the fundus
performance was evaluated. For the majority of the patients with
CRAO, the retina exhibited a milky white haze, and the retinal
artery was thinner than normal, with variable thickness. The color
of the optic disc was lighter, with total or partial blur on the
boundaries. The macular area showed ‘cherry red’ spots or edema.
Segmental blood flow appeared in the retinal artery, or cotton-wool
spots were observed in the retina. Five cases were found to be
normal by fundoscopic examination. These results suggested that the
evaluation of fundus performance was a useful step for preliminary
CRAO diagnosis.
FFA indicates that there are three
types of CRAO
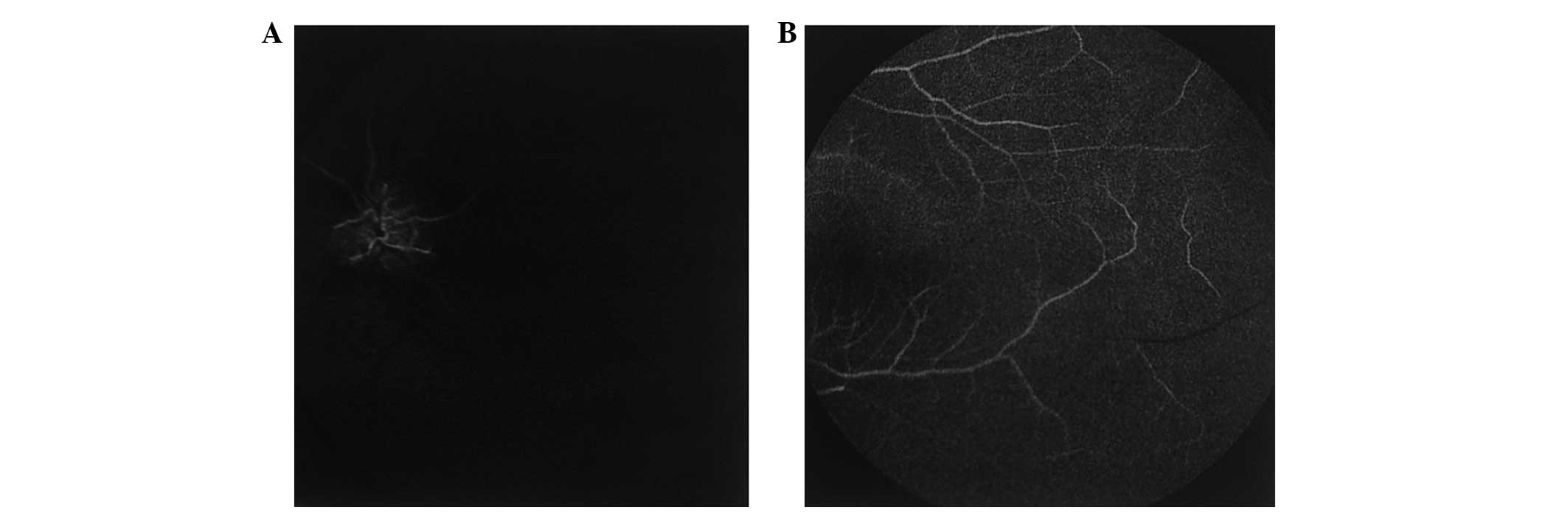
In order to classify CRAO in each patient, FFA was
performed. Among the 63 cases, 18 eyes were classified as the poor
perfusion type, with a circulation time from the arm to the retina
of >23 sec. Arterial perfusion at the early phase of FFA was
slow (Fig. 1A), but perfusion was
recovered in the peripheral retinal artery at the late phase
(Fig. 1B). The optic disc and
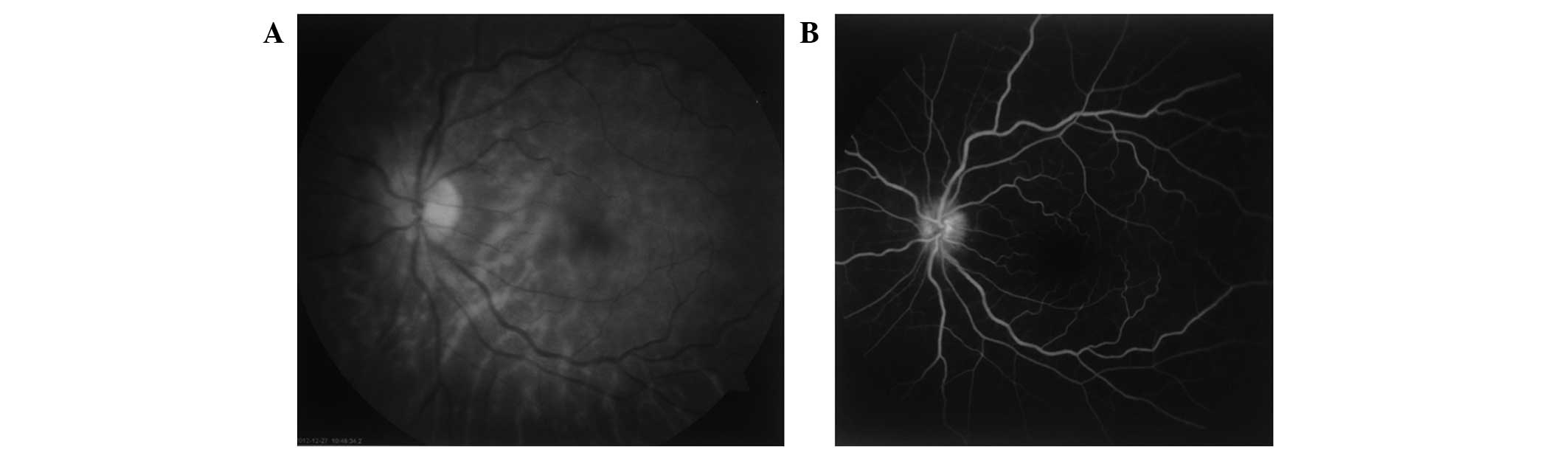
vascular wall were normal or slightly stained. Moreover, 22 eyes
were classified as having the exudation type of CRAO. These eyes
had a normal retinal arteriovenous perfusion time. At the early
phase, the optic disc exhibited high fluorescence with blurred
boundaries (Fig. 2A). At the
arteriovenous phase, the retinal vascular wall exhibited
fluorescein leakage. At the late phase, fluorescein leakage
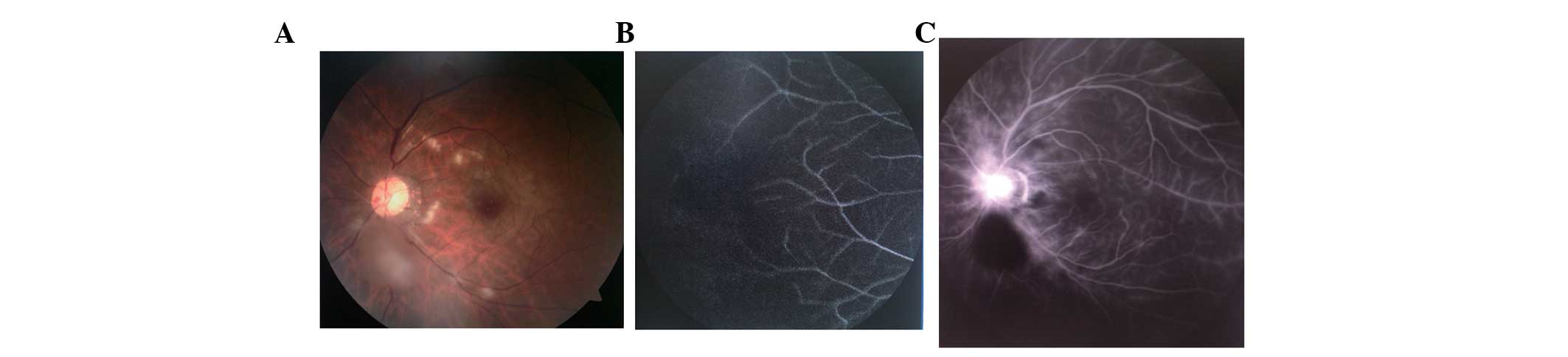
occurred at the optic disc or retinal vascular wall (Fig. 2B). In addition, 23 eyes were
considered as being affected by a mixed type of CRAO, having
characteristics of the poor perfusion and exudation types (Fig. 3). The FFA results within the study
group identified three types of CRAO.
Gender and disease course do not
correlate with the type of CRAO
Statistical analysis was performed to study the
correlation of age, gender and disease course with different types
of CRAO. Among the 63 eyes in the total study group, there were 18
eyes (28.57%) of the poor perfusion type, comprising 7 eyes
(11.11%) from males and 1 eye (17.46%) from a female. In the 22
eyes (34.92%) of the exudation type, there were 10 eyes (15.87%)
from males and 12 eyes (19.05%) from females. Among the 23 eyes
(36.51%) of the mixed type, there were 11 eyes (17.46%) from males
and 12 eyes (19.05%) from females. The results identified no
statistical difference in gender (χ2=0.176, P=0.916) and
disease course among the three types of CRAO (P>0.05; Table I). The data suggest that gender and
disease course did not correlate with CRAO type.
 | Table I.Comparison of patient gender, age and
disease course among the three types of CRAO. |
Table I.
Comparison of patient gender, age and
disease course among the three types of CRAO.
| CRAO type | Male (n=28) | Female (n=35) | Age (years) | Disease course
(days) |
|---|
| Poor perfusion | 7 | 11 | 56.67±9.18 | 6.22±4.40 |
| Exudation | 10 | 12 | 57.00±8.32 | 6.05±4.03 |
| Mixed | 11 | 12 | 58.17±9.06 | 6.00±3.94 |
| F-value |
|
| 0.171 | 0.016 |
| P-value |
|
| 0.844 | 0.984 |
Exudation type of CRAO causes less
severe damage compared with poor perfusion or mixed types
To evaluate the severity of damage caused by the
three types of CRAO, the numbers of patients with severe, mild and
light degrees of CRAO were counted, respectively. Among the 63
eyes, 8 eyes (12.70%) had severe damage, including 2 eyes with no
ability to sense light, 3 eyes able to sense light and 3 eyes able
to sense hand movement; 28 eyes (44.44%) had mild damage, including
12 eyes with the ability to count fingers, and 16 eyes with a
visual acuity of 0.01–0.08; 27 eyes (42.86%) had light damage.
Among the patients having the poor perfusion type or mixed type of
CRAO, 4 patients from each group had severe damage, and the
percentages of patients having mild and light damage were similar
in these two groups. By contrast, no severe visual damage was
observed for patients with the exudation type of CRAO, with more
than half of the patients having only light damage (Table II). These data demonstrate that the
exudation type of CRAO caused less severe damage compared with the
poor perfusion and mixed types.
 | Table II.Severity of damage caused by the three
types of CRAO. |
Table II.
Severity of damage caused by the three
types of CRAO.
| CRAO type | Severe damage, n
(%) | Mild damage, n
(%) | Light damage, n
(%) |
|---|
| Poor perfusion | 4 (22.22) | 8
(44.44) | 6
(33.33) |
| Exudation | 0 | 9
(40.91) | 13 (59.09) |
| Mixed | 4 (17.39) | 11 (47.83) | 8
(34.78) |
| Total | 8 (12.70) | 28 (44.44) | 27 (42.86) |
Discussion
The average age of the 63 patients in this study was
56.51 years, which is lower than the average age (69.5 years)
reported for patients with CRAO by researchers conducting a study
in France (5). No statistically
significant difference was observed in the incidence of CRAO
between male and female patients, which differs from the results
obtained in a Korean study, in which the CRAO incidence for males
was higher than that for females (11). The typical symptom of CRAO was
unrelieved amaurosis of the affected eye. Some patients experienced
transient amaurosis. Fundoscopic examination showed that at the
early stage of CRAO, the patients exhibited light retinal edema,
retinal artery stenosis and unobvious changes of the optic disc,
easily leading to an erroneous diagnosis that delayed treatment.
The retinas of most eyes affected by CRAO appeared grey in color,
which was even evident at the posterior pole. The macular area
exhibited red lesions, which are known as ‘cherry red spots’. The
optic disc appeared light in color with tissue edema. In some eyes
affected by CRAO, the retinal edema regressed, with the color
returning to normal. At this time, fundoscopic examination showed
normal results, but retinal tissue necrosis had already occurred,
resulting in the retinal artery becoming thinner and occluded, and
the optic nerve becoming atrophied; visual function is not able to
recover from such damage (12).
FFA is a commonly used method for the diagnosis of
CRAO. In contrast to fundoscopic examination, FFA images vary
considerably, due to differences in the degree of artery occlusion
and in the length of disease history. Among the 63 cases in the
present study, 41 cases (66%) had a longer arterial perfusion time
than normal, of which 24 cases were relieved and 17 cases formed
blurs in the peripheral and retinal macular regions at the late
phase of FFA, revealed as non-perfusion fluorescence. In addition,
45 cases had hyperfluorescence leakage from the optic disc at an
early phase of FFA, or fluorescence leakage from the retinal
vascular wall at the arteriovenous or late phases. Comparison of
the damage to vision for the three types of CRAO indicated that the
poor perfusion and mixed types of CRAO caused more severe visual
damage to vision than did the exudation type. The poor perfusion
type had a similar distribution of damage severity as the mixed
type. These observations concur with the findings of Altmann et
al (13), indicating that poor
perfusion of the retina is an important reason for visual
dysfunction and the low treatment response.
Notably, it was observed that some of the patients
with CRAO had normal fundoscopic examination and FFA results but
severely damaged vision. This might be due to the formation of
emboli from platelets, fibrin and cholesterol, which were quickly
degraded and transported to the periphery. Therefore, it would not
be possible to observe a totally occluded retinal artery by FFA,
and irreversible lesions could have already occurred on ganglionic
cells that were more sensitive to ischemia (14), leading to severely damaged vision.
Because of this, it is important to not neglecting CRAO when
patients present with symptoms of transient amaurosis. In addition,
retinal neovascularization was not found in any of the CRAO cases.
However, iris neovascularization was observed in 4 patients. We
hypothesize that retinal neovascularization rarely occurs in CRAO
because the epithelial layer of the retinal nerve is extensively
damaged and the non-perfused region cannot generate. By contrast,
iris neovascularization is caused by ischemia of the ophthalmic
artery outside the retina. Previous studies have indicated that
iris neovascularization usually occurs at 2–16 weeks after CRAO
(15), and patients with secondary
neovascular glaucoma account for 15% of all CRAO patients (16).
In conclusion, the FFA observations of CRAO can be
classified into three types of manifestations. Visual damage in
patients with CRAO is likely to be associated with poor perfusion
in the retinal artery rather than with exudation of the retina or
optical disc. The type of clinical manifestations does not
correlate with age, gender or disease course.
Acknowledgements
This study was supported by Tianjin Eye Hospital and
Nankai University.
References
|
1
|
Varma DD, Cugati S, Lee AW and Chen CS: A
review of central retinal artery occlusion: Clinical presentation
and management. Eye (Lond). 27:688–697. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Hayreh SS: Acute retinal arterial
occlusive disorders. Prog Retin Eye Res. 30:359–394. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hayreh SS: Ocular vascular occlusive
disorders: Natural history of visual outcome. Prog Retin Eye Res.
41:1–25. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hayreh SS, Podhajsky PA and Zimmerman MB:
Branch retinal artery occlusion: Natural history of visual outcome.
Ophthalmology. 116:1188–94, e1–e4. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Coisy S, Leruez S, Ebran JM, Pisella PJ,
Milea D and Arsene S: Systemic conditions associated with central
and branch retinal artery occlusions. J Fr Ophtalmol. 36:748–757.
2013.(In French). View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Padrón-Pérez N, Aronés JR, Muñoz S,
Arias-Barquet L and Arruga J: Sequential bilateral retinal artery
occlusion. Clin Ophthalmol. 8:733–738. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Mößner A, Jurisch D and Meier P: Bilateral
retinal artery occlusion. Ophthalmologe. 111:970–972. 2014.(In
German). View Article : Google Scholar : PubMed/NCBI
|
|
8
|
McLeod D: Central retinal artery occlusion
and cerebral stroke. Eye (Lond). 27:14222013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wang RS, Lv PL, Wang B, Wan YQ and Lei XQ:
Relationship between retinal circulation time and visual loss in
patients with central retinal artery occlusion. Zhonghua Yan Di
Bing Za Zhi. 23:177–179. 2007.(In Chinese).
|
|
10
|
Maguire JI and Federman JL: Intravenous
fluorescein angiography. Duane's Ophthalmology. Tasman W and Jaeger
EA: (2013). Lippincott Williams and Wilkins. (Philadelphia, PA).
2013.
|
|
11
|
Park SJ, Choi NK, Seo KH, Park KH and Woo
SJ: Nationwide incidence of clinically diagnosed central retinal
artery occlusion in Korea, 2008 to 2011. Ophthalmology.
121:1933–1938. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Weger M, Pichler T, Franke GH, Haas A,
Thaler HV, Kraigher-Krainer N, Groselj-Strele A, Wedrich A and
Rabensteiner DF: Assessment of vision-related quality of life in
patients with central retinal artery occlusion. Retina. 34:539–545.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Altmann M, Ertl M, Helbig H, Schömig B,
Bogdahn U, Gamulescu MA and Schlachetzki F: Low endogenous
recanalization in embolic central retinal artery occlusion-the
retrobulbar ‘spot sign’. J Neuroimaging. 25:251–256. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Miyake Y: Acquired Retinal Diseases.
Electrodiagnosis of Retinal Disease. Springer. (Tokyo).
1812006.
|
|
15
|
Rudkin AK, Lee AW and Chen CS: Ocular
neovascularization following central retinal artery occlusion:
Prevalence and timing of onset. Eur J Ophthalmol. 20:1042–1046.
PubMed/NCBI
|
|
16
|
Körner-Stiefbold U: Central retinal artery
occlusion-etiology, clinical picture, therapeutic possibilities.
Ther Umsch. 58:36–40. 2001.(In German). View Article : Google Scholar : PubMed/NCBI
|