Introduction
Cryptococcal meningitis (CM) is a burden disease in
middle- and low-income countries with over 1 million cases and
600,000 mortalities per year (1). CM
caused by the fungus Cryptococcus neoformans remains a
leading cause of morbidity and mortality among immunocompromised
patients, such as those with a malignancy, connective tissue
disorder, immunodeficiency virus (HIV) infection or having
undergone organ transplantation (2).
However, immunocompetent patients are susceptible to CM and can
present in the clinic with signs and symptoms typical of
meningitis, such as fever, headache and neck stiffness (3). Treatment of CM consists of three
phases: Induction, consolidation, and maintenance; effective
induction therapy requires potent fungicidal drugs (2,4).
Loss of vision, diplopia and ocular motility deficit
have been reported previously (5–7). In the
present study, a female immunocompetent patient with CM is reported
who initially presented with eye symptoms, and subsequently fully
recovered with complete resolution of the initial symptoms
following combined treatment with amphotericin B and
fluconazole.
Case report
A 42-year-old female presented in September 2014 at
the Department of Ophthalmology (Lishui Hospital Affiliated to
Zhejiang University, Lishui, China) with complaints of blurred
vision in both eyes and intermittent fatigue for ~1 month. No
additional symptoms, such as ocular pain, diplopia, headache,
nausea or vomiting, were reported. The patient had no previous
history of medical illness. The patient was admitted to the
hospital for further evaluation. The study was approved by the
Human Research Ethics Committee of Lishui Hospital Affiliated to
Zhejiang University, and was performed according to the Declaration
of Helsinki. Written informed consent was obtained from the patient
for publication of this Case report and the accompanying
images.
A general examination performed upon hospital
admission demonstrated that the clinical parameters, including
height, body weight and body mass index, of the patient were within
normal limits. The patient was afebrile and her vital signs were
normal. An ocular examination indicated uncorrected distance visual
acuities of 1.0 and 0.8 in the right and left eye, respectively. An
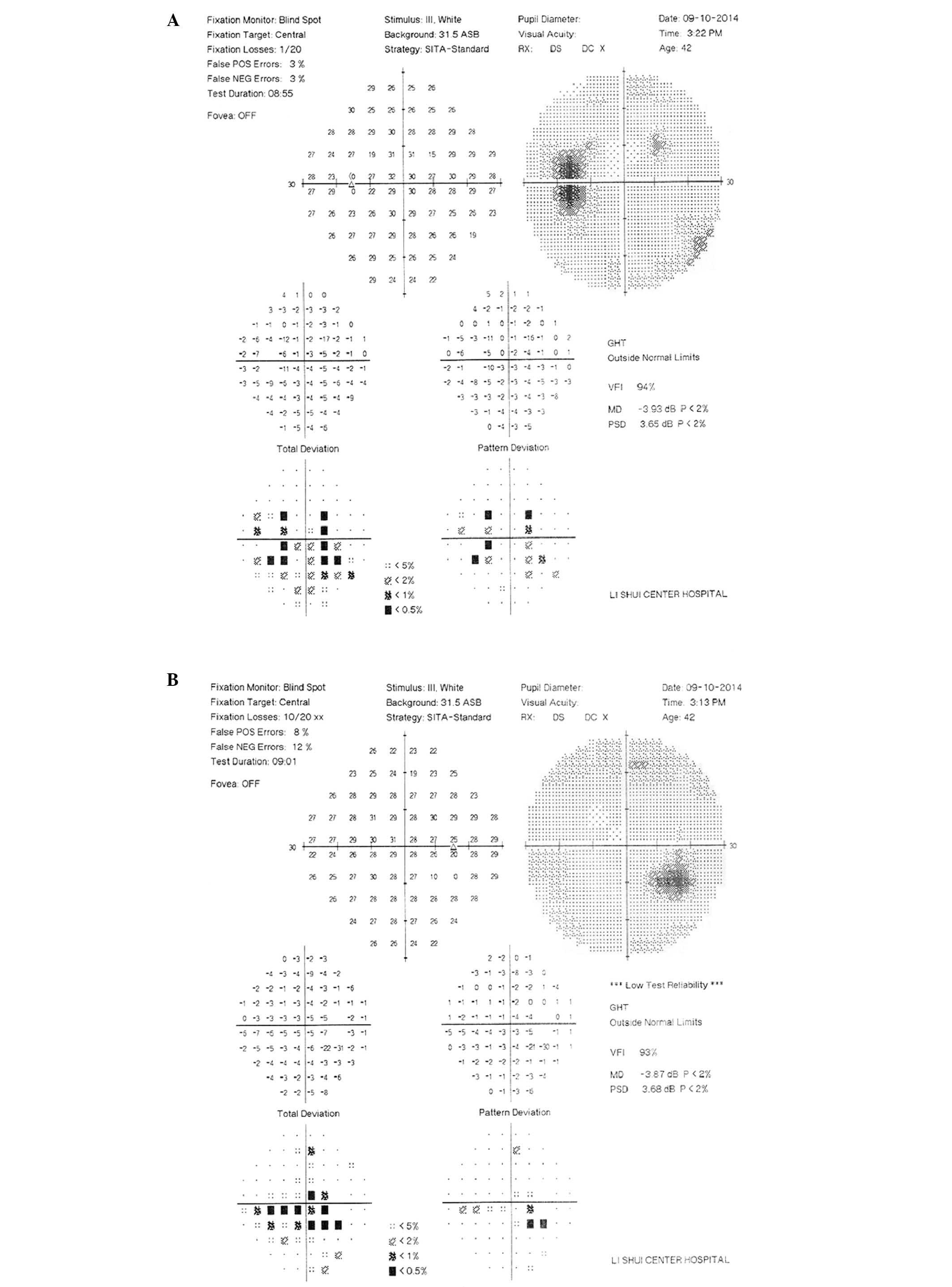
automated visual field test using the 30–2 fast threshold program
included with the Humphrey Visual Field Analyzer (Humphrey 750i;
Carl Zeiss AG, Oberkochen, Germany) showed marginally enlarged
blind spots in both eyes (Fig. 1),
and a slit lamp examination showed quiet anterior chambers without
significant abnormalities or an afferent pupillary defect.
Fundoscopy revealed marked elevated discs and evidence of bilateral
splinter optic disc hemorrhaging (Fig.
2). The maculae, retinal vasculature and retinal peripheries
were normal. Fluorescein (Alcon, Shanghai, China) angiography
showed staining of the optic disc and late peripapillary dye
pooling (Fig. 3). The intraocular
pressure of the patient remained in the normal range (10–21 mmHg)
throughout all examinations, and there was no ptosis, proptosis or
chemosis. A motor and sensory examination of both eyes showed
normal results, and the remainder of the neurological examination
indicated the following characteristics: Clear and co-operative
mentality, with normal advanced neural activity; no atrophy in the
limb muscles; normal muscle tension; muscle strength grade V;
positive tendon reflex of the limbs; negative bilateral Hoffmann
reflex, with the bilateral Babinski reflex not being elicited;
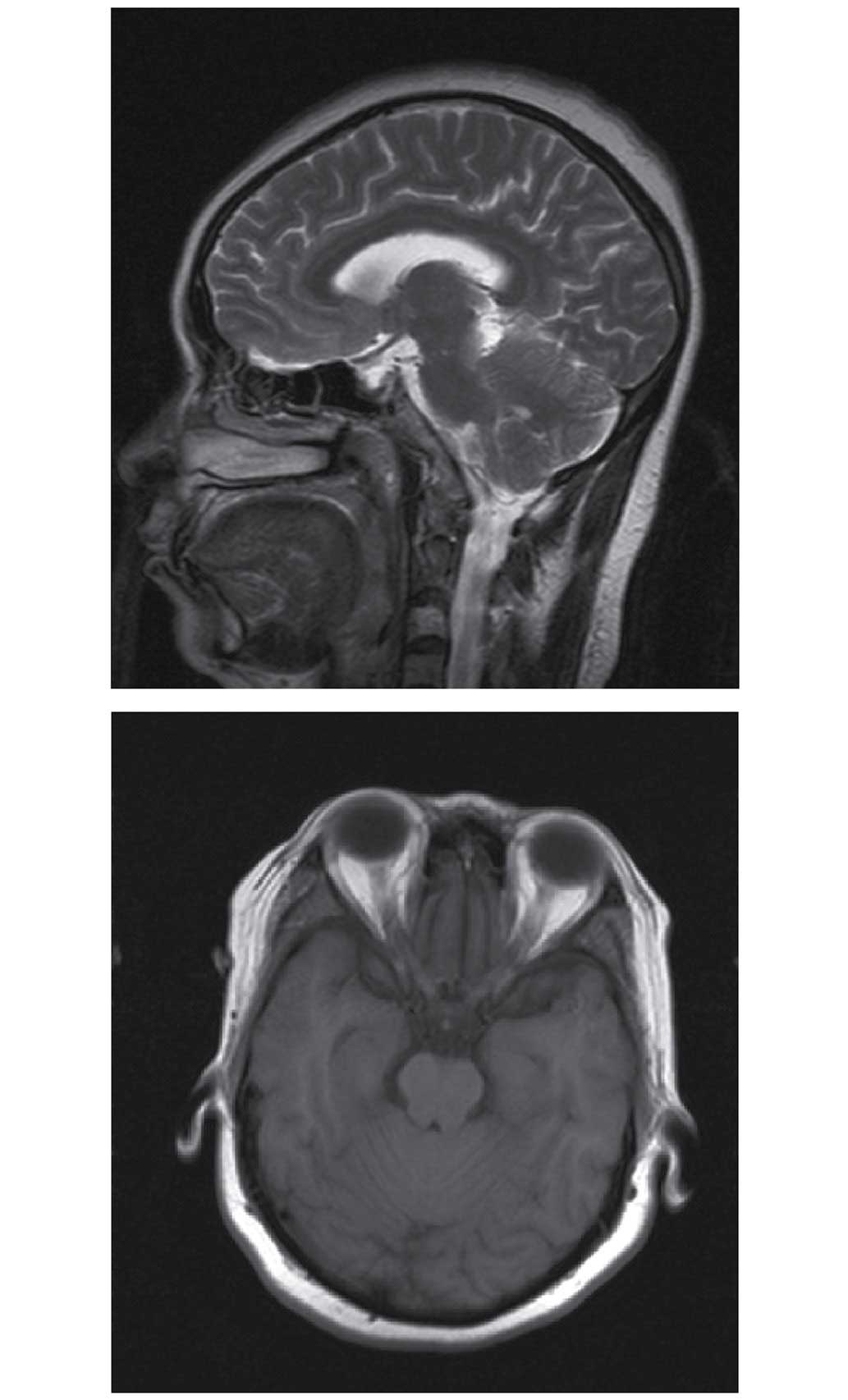
normal gait; and no ataxia. A chest X-ray (Fig. 4) and brain magnetic resonance imaging
(MRI) scan (Fig. 5) showed no
evident abnormalities.
The patient's initial diagnosis following admission
was optic nerve inflammation, and the patient was treated with
intravenous (IV) methylprednisolone (1 g/day for 3 days; Pfizer,
Inc., New York, NY, USA) followed by oral prednisone (1 mg/day for
11 days; Xianju Pharmaceutical Co., ltd., Taizhou, China). On day
18 following admission, the patient reported having a persistent
stabbing headache, but did not display other symptoms, such as
nausea, vomiting, fever, neck stiffness or confusion. It was
considered that the papilledema of the patient may be secondary to
a prolonged increase in intracranial pressure and infectious
infiltration of the optic nerve sheath. A lumbar puncture
demonstrated an opening pressure >400 mmH2O, and an
analysis of cerebrospinal fluid (CSF), including cell counts,
measurements of protein and glucose levels, showed a markedly
elevated protein concentration (0.77 g/l; reference range, 0.2–0.4
g/l) and decreased glucose concentration (1.08 mmol/l; reference
range, 2.5–0.4 mmol/l). The results of a common bacterial culture,
smear and culture for acid fast bacilli in the CSF were negative;
however, a microscopic examination (CX31; Olympus Corporation,
Tokyo, Japan) and India ink test (Yuanmu Biological Technology Co.,
Ltd., Shanghai, China), performed according to the manufacturer's
instructions as described in a previous study (8), showed the presence of Cryptococcus
neoformans. The results of other laboratory tests, including an
enzyme-linked immunosorbent assay for toxoplasmosis (cat. no.
S20020001; Haitai Biological Pharmaceutical Co., Ltd., Zhuanghe,
China), treponema pallidum hemagglutination (cat. no. NV30918;
Jianlun Science and Technology Co., Ltd., Guangzhou, China) tests
and an HIV antibody test (cat. no. S19990046; Zhongshan Biological
Pharmaceutical Co., Ltd., Zhongshan, China) were all negative.
Based on the clinical symptoms and positive
microscopic examination and India ink test results, the patient was
diagnosed with CM. Following diagnosis, the patient was treated
with amphotericin B (IV; 1.0 mg/kg/day; North China Pharmaceutical
Co., Ltd., Shijiazhuang, China) in combination with oral
fluconazole (200 mg, twice daily; Bokang Gene Science and
Technology Co., Ltd., Beijing, China). Additionally, IV mannitol
(125 ml, twice daily; Shuanghe Pharmaceutical Co., Ltd, Wuhan,
China) and oral acetazolamide (200 mg, twice daily; Aoyibaoling
Pharmaceutical Co., Ltd., Hangzhou, China) were administered during
the early phase of drug therapy to control the elevated
intracranial pressure. Following treatment for 1.5 months, the
patient fully recovered her visual acuity and regained a normal
optic disc. At this point, previous medications were halted and the
patient began a 2-month course of mono-treatment with oral
fluconazole (400 mg/day). After 2 months of treatment with oral
fluconazole, the results of a repeat CSF examination were negative
for Cryptococcus neoformans, and the patient showed no
evidence of disease recurrence at a 3 month follow-up visit.
Discussion
Cryptococcosis, caused by Cryptococcus
neoformans, is an important infectious disease with a worldwide
presence (1,9,10).
Cryptococci are encapsulated saprophytic yeasts often found in soil
contaminated with avian excreta (11). Humans typically become infected by
inhaling the aerosolized organisms, following which the infection
can be asymptomatic or limited to the lungs (11,12);
however, the infection can later spread hematogenously to other
areas of the body, in particular to the meninges (3).
Compared with its presence in immunocompetent
patients, Cryptococcosis is more common in immunocompromised
patients, including those with impaired cell-mediated immunity
(13). Such impaired patients
include those with a malignancy, connective tissue disorder, HIV
infection or those who have undergone organ transplantation
(2,14). However, previous studies have shown
that a number of patients infected with Cryptococcosis are
immunocompetent (6,15–17). CM
causes morbidity and mortality worldwide, particularly in patients
with impaired cell-mediated immunity; however, the clinical
outcomes in immunocompetent patients are more favorable.
The initial clinical manifestations of a CM
infection are highly variable. In non-immunocompromised patients,
CM typically presents with signs and symptoms associated with
meningitis, such as a fever, headache and neck stiffness (3,18).
Additionally, cranial neuropathies and ophthalmoplegia are common
complications in patients with CM (5,6,16,19).
However, primary bilateral blurred vision without any accompanying
symptoms is a rare initial presentation of a cryptococcal
infection. In the current case, the only abnormalities of the
patient upon presentation consisted of decreased uncorrected
distance visual acuity in both eyes and bilateral papilledema,
which was present for ~1 month. Other common signs and symptoms
that could be attributed to intracranial pressure, such as
headache, confusion, nausea and vomiting, were absent upon
admission. Such a presentation may result in the delayed diagnosis
of a brain disease.
A satisfactory evaluation for CM requires a lumbar
puncture with measurement of the opening pressure, and subsequent
CSF analysis, including measurements of protein and glucose
expression levels. In addition, India ink staining, a fungal
culture and cryptococcal antigen tests should be performed
(20). A definitive diagnosis of CM
requires visualizing the fungus in CSF using the India ink test,
positive CSF latex agglutination assay results or CSF culture
results positive for Cryptococcus neoformans (21). In the present case, CM was diagnosed
based on results of the India ink test, which, according to
previous reports, has a sensitivity of 75–85%. Additionally,
increased protein expression levels and decreased glucose
expression levels in CSF may indicate the presence of a more severe
inflammation, which is concordant with the results in the present
study. Imaging tests may also provide information useful for
diagnosing CM. For example, a communicating hydrocephalus may occur
early in a CM infection due to acute meningeal exudate, and can
also occur in a late-stage infection due to the presence of
meningeal adhesions (22). However,
in the present case, the cranial MRI scan of the patient upon
hospital admission was normal, and showed no evidence of cranial
infection or increased intracranial pressure.
The optimal treatment regimen and duration for a
Cryptococcosis infection in non-HIV-infected patients
remains largely unknown (23).
Current recommendations are derived from previous clinical
experience with HIV-infected individuals, but are not supported
with evidence obtained from large randomized controlled clinical
trials. In the current study, the patient was treated with
amphotericin B (IV; 1.0 mg/kg/day) administered in conjunction with
fluconazole (oral; 400 mg/day). It has been reported that using a
dose of amphotericin B (0.7–1 mg/kg/day) may result in a slightly
lower mortality rate (24).
In conclusion, the present study demonstrates that
eye symptoms may constitute the initial presentation of CM in an
immunocompetent patient, and such symptoms can lead to its delayed
diagnosis. CM should be suspected in any cases of decreased visual
acuity of unknown origin accompanied with unexplained bilateral
papilledema in patients with or without a compromised immune
system.
References
|
1
|
Park BJ, Wannemuehler KA, Marston BJ,
Govender N, Pappas PG and Chiller TM: Estimation of the current
global burden of cryptococcal meningitis among persons living with
HIV/AIDS. AIDS. 23:525–530. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Sloan DJ and Parris V: Cryptococcal
meningitis: Epidemiology and therapeutic options. Clin Epidemiol.
6:169–182. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Chen SC, Slavin MA, Heath CH, Playford EG,
Byth K, Marriott D, Kidd SE, Bak N, Currie B, Hajkowicz K, et al:
Australia and New Zealand Mycoses Interest Group
(ANZMIG)-Cryptococcus Study: Clinical manifestations of
Cryptococcus gattii infection: Determinants of neurological
sequelae and death. Clin Infect Dis. 55:789–798. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Pappalardo MC, Szeszs MW, Martins MA,
Baceti LB, Bonfietti LX, Purisco SU, Baez AA and Melhem MS:
Susceptibility of clinical isolates of Cryptococcus neoformans to
amphotericin B using time-kill methodology. Diagn Microbiol Infect
Dis. 64:146–151. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Muslikhan Y, Hitam WH, Ishak SR, Mohtar I
and Takaran J: Cryptococcus meningitis in an immunocompetent
teenage boy presented early with diplopia. Int J Ophthalmol.
3:92–94. 2010.PubMed/NCBI
|
|
6
|
Liyanage DS, Pathberiya LP, Gooneratne IK,
Caldera MH, Perera PW and Gamage R: Cryptococcal meningitis
presenting with bilateral complete ophthalmoplegia: A case report.
BMC Res Notes. 7:3282014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Moodley A, Rae W, Bhigjee A, Connolly C,
Devparsad N, Michowicz A, Harrison T and Loyse A: Early clinical
and subclinical visual evoked potential and Humphrey's visual field
defects in cryptococcal meningitis. PloS One. 7:e528952012.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Saha DC, Xess I and Jain N: Evaluation of
conventional & serological methods for rapid diagnosis of
cryptococcosis. Indian J Med Res. 127:483–488. 2008.PubMed/NCBI
|
|
9
|
Leal AL, Faganello J, Fuentefria AM, Boldo
JT, Bassanesi MC and Vainstein MH: Epidemiological profile of
cryptococcal meningitis patients in Rio Grande do Sul, Brazil.
Mycopathologia. 166:71–75. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Pyrgos V, Seitz AE, Steiner CA, Prevots DR
and Williamson PR: Epidemiology of cryptococcal meningitis in the
US: 1997–2009. PloS One. 8:e562692013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Perfect JR and Casadevall A:
Cryptococcosis. Infecti Dis Clin North Am. 16:837–874. 2002.
View Article : Google Scholar
|
|
12
|
Corti M, Solari R, Cangelosi D, Domínguez
C, Yampolsky C, Negroni R, Arechavala A and Schtirbu R: Sudden
blindness due to bilateral optic neuropathy associated with
cryptococcal meningitis in an AIDS patient. Rev Iberoam Micol.
27:207–209. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Schimpff SC and Bennett JE: Abnormalities
in cell-mediated immunity in patients with Cryptococcus neoformans
infection. J Allergy Clin Immunol. 55:430–441. 1975. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Gonzalez-Duarte A, Saniger-Alba Mdel M and
Higuera-Calleja J: Cryptococcal meningitis in HIV-negative patients
with systemic connective tissue diseases. Neurol Res. 37:283–287.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Louro R, Ferreira R, Pinheiro C, Parada H,
Faria D and Monteiro E: Fungal meningitis in an immunocompetent
patient. Clin Drug Investig. 33(Suppl 1): S47–S50. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Portelinha J, Passarinho MP, Almeida AC
and Costa JM: Bilateral optic neuropathy associated with
cryptococcal meningitis in an immunocompetent patient. BMJ Case
Rep. 2014:pii2014.
|
|
17
|
Saigal G, Post MJ, Lolayekar S and Murtaza
A: Unusual presentation of central nervous system cryptococcal
infection in an immunocompetent patient. AJNR. Am J Neuroradiol.
26:2522–2526. 2005.PubMed/NCBI
|
|
18
|
McMullan BJ, Sorrell TC and Chen SC:
Cryptococcus gattii infections: Contemporary aspects of
epidemiology, clinical manifestations and management of infection.
Future Microbiol. 8:1613–1631. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Espino Barros Palau A, Morgan ML, Foroozan
R and Lee AG: Neuro-ophthalmic presentations and treatment of
Cryptococcal meningitis-related increased intracranial pressure.
Can J Ophthalmol. 49:473–477. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Khairullah S, Sulaiman H, Yahya F, Jasmin
R, Cheah TE, Sockalingam S, Bick J and Chin Teck NG: Cryptococcal
meningitis and SLE: A diagnostic and therapeutic challenge. Acta
Reumatol Port. 39:254–258. 2014.PubMed/NCBI
|
|
21
|
Patil SA, Katyayani S and Arvind N:
Significance of antibody detection in the diagnosis of cryptococcal
meningitis. J Immunoassay Immunochem. 33:140–148. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Sarkis RA, Mays M, Isada C and Ahmed M:
MRI findings in cryptococcal meningitis of the non-HIV population.
Neurologist. 19:40–45. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Day JN, Chau TT, Wolbers M, Mai PP, Dung
NT, Mai NH, Phu NH, Nghia HD, Phong ND, Thai CQ, et al: Combination
antifungal therapy for cryptococcal meningitis. N Engl J Med.
368:1291–1302. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Lui G, Lee N, Ip M, Choi KW, Tso YK, Lam
E, Chau S, Lai R and Cockram CS: Cryptococcosis in apparently
immunocompetent patients. QJM. 99:143–151. 2006. View Article : Google Scholar : PubMed/NCBI
|