Introduction
Surgical trauma, burns, and severe infections cause
damage to the structure and function of intestinal mucosa, and
facilitate intestinal bacterial translocation. This can lead to
multiple organ function failure, which is potentially be
life-threatening (1).
Glutamine (Gln) is a free amino acid that comprises
>50% of the body's free amino acid pool (2). Gln is a precursor for protein synthesis
and is a preferential energy source for immune and mucosal cells.
In addition, this amino acid is an important intermediate in many
metabolic pathways (3). Animal
experiments and clinical studies demonstrated that Gln increases
the height of intestinal villi, reduces intestinal mucosal
permeability and enhances intestinal immune function (4). In addition, it prevents bacterial
translocation and contributes to maintaining the intestinal mucosal
barrier (4). The effects of Gln on
intestinal inflammatory response and mucosal permeability remain to
be elucidated.
In the present study, we conducted a meta-analysis
to evaluate the effects of Gln supplementation in patients
undergoing abdominal surgery.
Materials and methods
Search strategy
A search of the PubMed (http://www.pubmed.com), EMBASE (http://www.embase.com), Web of Science (http://apps.webofknowledge.com), and The Cochrane
Library (http://www.thecochranelibrary.com) databases was
conducted. Specific search strategies were developed for each
database, using different combinations and variations of search
terms, including ‘glutamine’, ‘Gln’, ‘surgery’, ‘surgical’,
‘inflammatory reaction’, ‘CRP’, ‘TNF-α’, ‘IL-2R’, ‘IL-6′,
‘intestine permeability’ ‘intestinal barrier’,
‘lactulose/mannitol’, ‘DAO’, ‘D(−)lactic acid’, ‘endotoxin’, and
their variants.
Study selection
Inclusion criteria for the meta-analysis were: i)
Study design was a randomized controlled trial, ii) study included
patients undergoing abdominal surgery, iii) study patients received
a supplementation with Gln peptide (Ala-Gln or Gly-Gln) whereas
control patients did not use any supplements, and iv) study
outcomes included inflammatory markers [C-reactive protein (CRP),
tumor necrosis factor-α (TNF-α), interleukin (IL)-2R, or IL-6] and
markers of intestinal permeability (lactulose/mannitol, diamine
oxidase, D(−)lactic acid, and endotoxin). Exclusion criteria for
the study were: i) Studies were required to be basic research or
animal studies, or systematic reviews, ii) they did not include
abdominal surgery patients, iii) data were not complete or original
data were not presented, and iv) repeated published reports.
Data extraction
Data were extracted independently by two
investigators according to the pre-specified selection criteria.
Discrepancies were resolved by discussion. From each study,
information on first author, publication year, sample size, patient
age and gender, outcomes, 95% confidence interval (CI), standard
deviation, and P-values were extracted. Since differences in study
populations and design may have caused variations, a study-quality
score was assigned using the methodological quality assessment.
This assessment utilized the Jadad quality evaluation scale to rank
the quality of the included randomized controlled trials. Thus,
studies scored 0 point if they were not randomized controlled
trials (these studies were excluded). The studies ranked 1–2 points
were low quality studies, whereas studies with 3–5 points were high
quality studies. The studies that received 1–5 points were included
in this meta-analysis (Table I).
 | Table I.Methodological quality assessment of
randomized controlled studies. |
Table I.
Methodological quality assessment of
randomized controlled studies.
| Items | 0 | 1 | 2 |
|---|
| Randomization | Not randomized or
inappropriate method of randomization | Randomized study
design | Randomization method
has been described and has been appropriate |
| Double blinding | No blinding or
inappropriate method of blinding | Double-blinded
study | The method of double
blinding has been described and has been appropriated |
| Withdrawals and
dropouts | Follow up not
described | Description of
withdrawals and dropouts has been included |
|
Statistical analysis. Data were analyzed using the
statistical software provided by the Cochrane Collaboration (RevMan
5.2; Baltimore, MD, USA) and presented as means ± standard
deviations. A classified variable was presented as a relative risk
with 95% CI. A summary estimate of continuous data was presented as
a weighted mean difference (WMD) with 95% CI. Before calculating
the standardized mean effect for the trials, statistical
heterogeneity test was evaluated by using the I2
statistic (α=0.05), which assessed the appropriateness of pooling
individual study results. The I2 values of 25, 50 and
75%, respectively, corresponded to low, moderate, and high levels
of heterogeneity. The meta-analysis was performed using a
fixed-effects model when there was no heterogeneity of results. For
heterogeneity, a random-effects model was used. Statistical
significance was set at P<0.05, and two-tailed tests were
used.
Results
Study characteristics
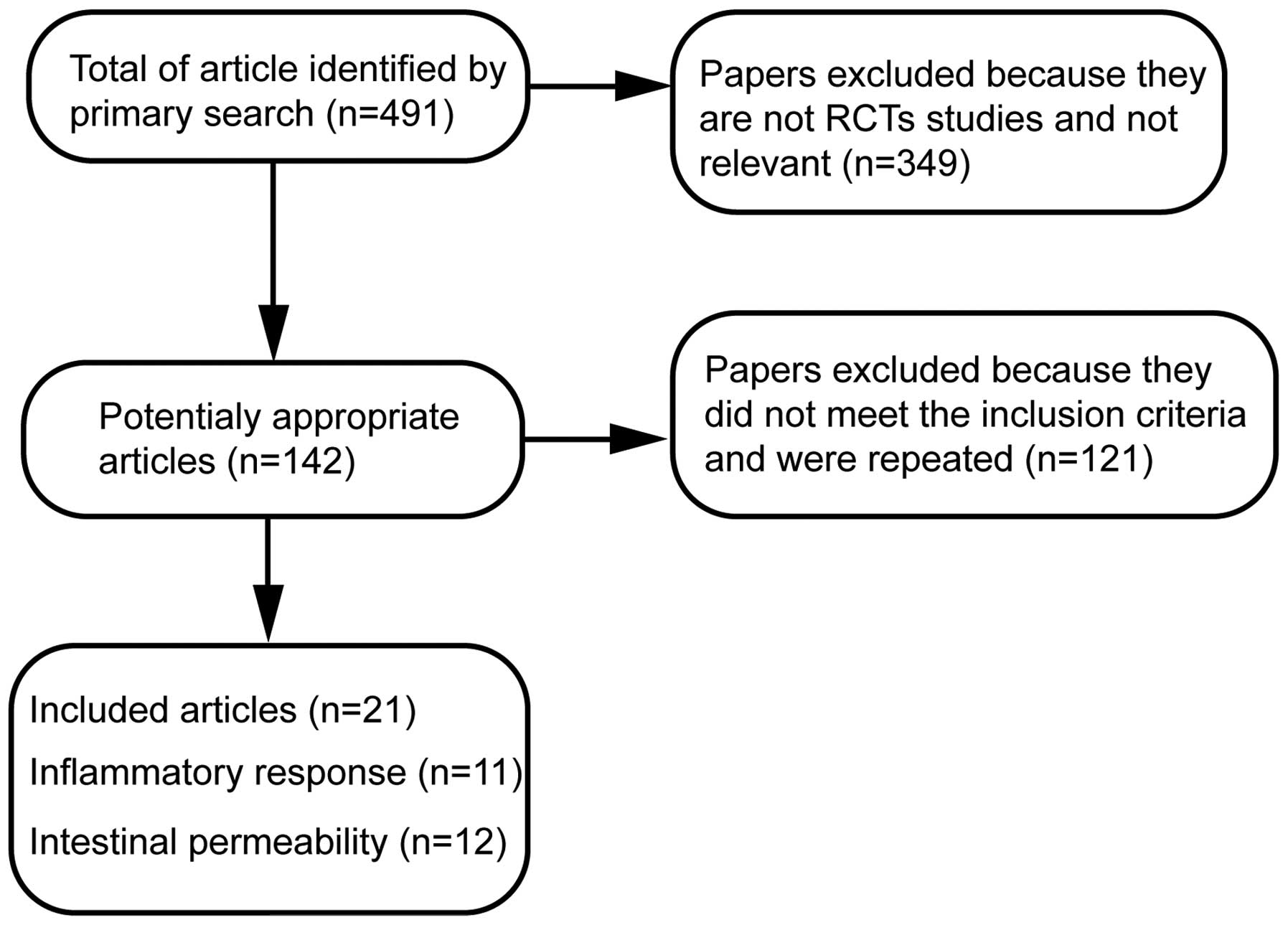
A total of 491 papers using the specified searching
strategies were identified. By screening titles, and reading the
abstracts and entire papers, 21 randomized controlled trials were
selected (Fig. 1) (5–25). The
included trials were published between August, 1966 and June 2014.
Of these trials, 11 randomized controlled trials evaluated the
effects of Gln on inflammatory response and 12 randomized
controlled trials examined the effects of Gln on markers of
intestinal permeability in abdominal surgery patients.
Characteristics of randomized controlled trials included in the
meta-analysis and the quality assessment of included randomized
controlled trials are presented in Table II.
 | Table II.RCTs included in the
meta-analysis. |
Table II.
RCTs included in the
meta-analysis.
|
| Sample size | Mean age | Gender (M vs. F) |
|
|
|
|
|---|
|
|
|
|
|
|
|
|
|
|---|
| RCT |
Controls/glutamine-supplemented |
Controls/glutamine-supplemented |
Controls/glutamine-supplemented | Patient type | Outcomes | Jadad quality
evaluation scale | Refs. |
|---|
| Dong et al
(2008) | 20/20 | 64.2/66.5 | 14 vs. 6/13 vs.
7 | Total
gastrectomy | CRP, TNF-α | 4 | (5) |
| Li et al
(2012) | 40/40 | 58/57 | 23 vs. 17/25 vs.
15 | Gastric cancer | TNF-α and IL-6 | 4 | (6) |
| Feng et al
(2007) | 58/58 | 56/56 |
| Gastric cancer | TNF-α | 4 | (7) |
| Lu et al
(2011) | 25/25 | 66.6/66.8 | 16 vs. 9/18 vs.
7 | Gastrointestinal
cancer | CRP, TNF-α, IL-6 | 4 | (8) |
| Richard et al
2014 | 11/11 | 47/45 | 5 vs. 6/6
vs. 5 | Hepatic
resection | CRP | 4 | (9) |
| Yeh et al
(2008) | 35/35 | 59/58 | 18 vs. 17/20 vs.
15 | Gastrointestinal
surgery | CRP | 4 | (10) |
| Xu et al
(2011) | 40/40 | 61.2/62.3 | 21 vs. 19/20 vs.
20 | Gastrectomy | TNF-α,
lactulose/mannitol, diamine oxidase | 3 | (11) |
| Yang et al
(1999) | 7/7 | 43/43 |
| Gastrectomy | IL-2R | 3 | (12) |
| Song et al
(2002) | 20/20 | 56/56 |
| Colorectal
cancer | IL-2R | 4 | (13) |
| Quan et al
(2010) | 10/10 | 52/50 | 6 vs.
4/5 vs. 5 | Abdominal
surgery | IL-6,
Lactulose/mannitol, diamine oxidase | 4 | (14) |
| Lin et al
(2005) | 23/25 | 67.6/66.7 | 14 vs. 9/14 vs.
11 | Abdominal
surgery | IL-6 | 4 | (15) |
| Jian et al
(1999) | 30/30 | 54.5/55.5 | 31 vs. 29/35 vs.
25 | Gastrointestinal
surgery |
Lactulose/mannitol | 4 | (16) |
| Quan et al
(2004) | 10/10 | 48.3/48.3 | 7 vs.
3/6 vs. 4 | Abdominal
surgery | Lactulose/mannitol,
diamine oxidase | 4 | (17) |
| Zhu et al
(2005) | 20/21 | 67.6/68.4 | 12 vs. 8/12 vs.
9 | Abdominal secondary
surgery | Lactulose/mannitol,
endotoxin | 4 | (18) |
| Zhu et al
(2000) | 15/15 | 66.7/68.3 | 7 vs.
8/6 vs. 9 | Gastrointestinal
surgery |
Lactulose/mannitol | 4 | (19) |
| Zhao et al
(2010) | 20/20 | 61.7/62.5 | 12 vs. 8/14 vs.
6 | Gastric cancer | Diamine
oxidase, D(−)lactic acid | 3 | (20) |
| Gu et al
(2006) | 36/36 | 61.7/62.5 | 28 vs. 12/20 vs.
12 | Gastric cancer | D(−)lactic
acid | 3 | (21) |
| Niu et al
(2011) | 29/29 |
| 15 vs. 14/17 vs.
12 | Abdominal
surgery | D(−)lactic
acid | 3 | (22) |
| Li et al
(2006) | 40/40 | 57.6/58.2 | 30 vs. 10/27 vs.
13 | Cardiac
carcinoma | Endotoxin | 4 | (23) |
| Yao et al
(2002) | 14/14 | 60.1/59.0 |
| Abdominal
surgery | Endotoxin | 4 | (24) |
| Yao et al
(2005) | 20/20 | 57.4/56.1 |
| Gastrointestinal
surgery | Endotoxin | 4 | (25) |
Inflammatory outcomes
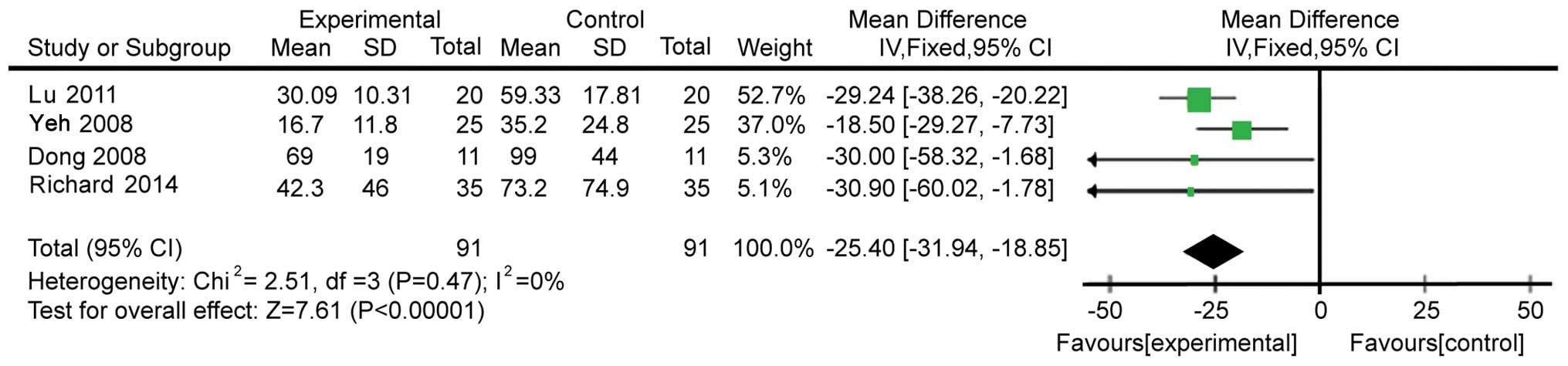
Four studies with 182 subjects presented data on CRP
levels. The data were homogeneous (χ2=2.51, P=0.47,
I2=0%; Fig. 2).
Therefore, a fixed-effects model was used for analysis. The CRP
levels in Gln-supplemented patients were lower than those in the
control patients (WMD=−25.40, 95% CI: −31.94, −18.85;
P<0.00001).
We then identified five studies comprising 286
patients and evaluating the modulation of TNF-α. These studies
showed heterogeneity (χ2=190.20, P≤0.00001,
I2=98%; Fig. 3).
Therefore, a random-effects model was utilized. We demonstrated
that patients on the Gln supplementation showed a more pronounced
decrease of TNF-α levels compared with control patients
(WMD=−21.75, 95% CI: −32.67, −10.83; P<0.0001).
The following tested inflammatory outcome was IL-2R,
which was evaluated in two studies comprising 44 patients. The
fixed-effects model was used because of acceptable heterogeneity
(χ2=2.36, P=0.12, I2=58%; Fig. 4). The levels of IL-2R in patients
supplemented with Gln were higher than those in control patients
(WMD=4.46, 95% CI: 2.85, 6.06; P<0.00001).
The final inflammatory marker analyzed was IL-6.
Four studies (n=198) tested the change of IL-6 levels on Gln
supplementation. These studies were heterogeneic
(χ2=11.45, P=0.010, I2=74%; Fig. 5). Therefore, a random-effects model
was used for analysis. IL-6 levels were significantly lower in
patients supplemented with Gln (WMD=−10.29, 95% CI: −16.56, −4.02;
P=0.001 vs. control patients). Publication bias is shown in
Fig. 6.
Evaluation of mucous membrane
permeability
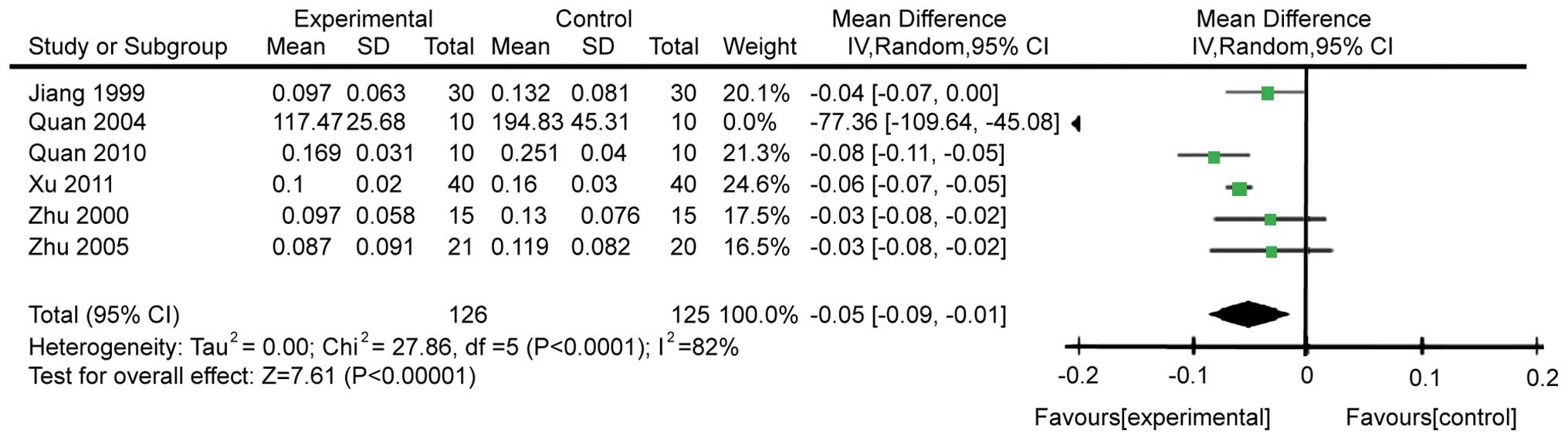
We analyzed the effects on the ratio of
lactulose/mannitol after abdominal surgery. There were six studies
comprising 251 patients that reported this ratio. These studies
were heterogeneous (χ2=27.86, P<0.0001,
I2=82%; Fig. 7).
Heterogeneity may have been caused by different times of Gln
supplementation or different doses, or by the type of disease.
Thus, the random-effects model was utilized for the meta-analysis.
Gln was found to significantly decrease intestinal permeability
(WMD=−0.05, 95% CI: −0.09, −0.01; P=0.007; Fig. 8). Publication bias is shown in
Fig. 8.
Modulation of the diamine oxidase levels was also
analyzed. Four studies comprising 160 patients were included. The
heterogeneity was acceptable (χ2=3.81, P=0.28,
I2=21%), allowing to use the fixed effects model for
meta-analysis. Gln significantly decreased the levels of diamine
oxidase (WMD=−1.60, 95% CI: −1.89, −1.31; P<0.00001; Fig. 9). Publication bias is shown in
Fig. 10.
The effects of Gln supplementation on the levels of
D(−)lactic acid were analyzed. Three studies (n=160) reported the
effects after abdominal surgery. Due to the heterogeneity of these
studies (χ2=134.29, P≤0.00001, I2=99%), the
random-effects model was utilized. The difference between
Gln-treated and control patients did not reach statistical
significance (WMD=−8.14, 95% CI: −18.12, −1.84; P=0.11; Fig. 11).
The effects of Gln on endotoxin levels were then
analyzed. Five studies comprising 210 subjects were performed and
the endotoxin levels reported. The studies were heterogeneous
(χ2=983.78, P<0.0001, I2=100%), prompting
us to use the random effects model. The results showed that Gln
significantly decreases the levels of endotoxin (WMD=−0.36, 95% CI:
−0.45, −0.27; P<0.00001; Fig.
12).
Discussion
Gln is as an important free amino acid in the human
body and is used in clinical practice as a supportive
supplementation. Gln improves immune function and nutritional
status, and protects gastrointestinal mucosa. These effects promote
patient recovery. Gln ameliorates the function of intestinal
mucosal cells, lymphocytes, macrophages, and neutrophils (12–15).
This amino acid is indispensible for intestinal mucosal epithelial
cell metabolism as it improves intestinal mucosal repair and
restoration of barrier function of the intestinal mucosa (26,27).
Thus, patients who do not receive Gln supplementation demonstrate
increased intestinal permeability (28).
Our study evaluated the effects of Gln on
inflammatory markers CRP, TNF-α, IL-2R, and IL-6 in patients after
abdominal surgery. CRP, often used as an inflammatory and disease
activity marker (29), is a
sensitive marker of non-specific inflammatory response. TNF-α is an
important inflammatory mediator in trauma, infection and stress
situations. IL-2R binds to IL-2, which is an important immune
regulatory cytokine (30). IL-6 is
an inflammatory mediator closely associated with disease outcome
and prognosis. The results of the present meta-analysis show that
the levels of CRP, TNF-α, and IL-6 were decreased by Gln
supplementation, whereas the levels of IL-2R were increased.
We evaluated the effects of Gln on the markers of
intestinal mucosal permeability, as demonstrated by parameters such
as lactulose/mannitol ratio, and the levels of diamine oxidase,
D(−)lactic acid, and endotoxin. When the intestinal mucosal barrier
function is impaired, the connection between intestinal mucosal
cells is disturbed and intercellular space increases, leading to an
increased lactulose/mannitol ratio (31). Damaged intestinal mucosal epithelial
cells release diamine oxidase, which elevated the levels of this
marker in blood plasma. Therefore, diamine oxidase is a reliable
plasma marker for indirect assessment of the integrity of the
mucosal epithelial cell layer (32,33).
D(−)lactic acid is the metabolite of bacterial fermentation. When
intestinal mucous membrane permeability increases, higher levels of
D(−)lactic acid reach the bloodstream (34). Thus, monitoring of D(−)lactic acid
levels in blood can reflect intestinal mucosal damage and impaired
permeability. Endotoxin is a virulence factor produced by
gram-negative bacteria. Under normal circumstances, intact
intestinal barrier prevents endotoxin from entering the blood
circulation (33). When the
intestinal barrier is damaged, endotoxin levels in peripheral blood
increase. Our analyses show that the lactulose/mannitol ratio, and
the levels of diamine oxidase and endotoxin were significantly
lower in patients supplemented with Gln. This result indicates that
Gln can decrease intestinal mucosal permeability in patients after
abdominal surgery and restore the intestinal mucosal barrier
function.
This meta-analysis also has certain limitations.
First, this study included 21 studies, with higher proportion of
studies from China and lower proportion of international studies.
This constituted a possible selection bias. Second, whereas all the
studies included in the meta-analysis utilized a randomized and
parallel study design, they were not always blinded. Third, because
of insufficient sample size, publication bias may be large. For
example, since there were only three published reports on
D(−)lactic acid, heterogeneity and publication bias was
sizable.
In conclusion, Gln appears to effectively reduce the
inflammatory response and intestinal mucosal permeability in
patients after abdominal surgery.
Acknowledgements
The present study was supported by the ‘Twelfth
Five-Year’ National Key Technology R&D Program of China (grant
no. 2012BAI35B03).
References
|
1
|
Fink MP and Delude RL: Epithelial barrier
dysfunction: A unifying theme to explain the pathogenesis of
multiple organ dysfunction at the cellular level. Crit Care Clin.
21:177–196. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Marik PE: Maximizing efficacy from
parenteral nutrition in critical care: Appropriate patient
populations, supplemental parenteral nutrition, glucose control,
parenteral glutamine, and alternative fat sources. Curr
Gastroenterol Rep. 9:345–353. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Morlion BJ, Stehle P, Wachtler P, Siedhoff
HP, Köller M, König W, Fürst P and Puchstein C: Total parenteral
nutrition with glutamine dipeptide after major abdominal surgery: A
randomized, double-blind, controlled study. Ann Surg. 227:302–308.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Jiang ZM and Yu JK: Gut barrier
dysfunction and parenteral/enteral nutrition update. Med Res Bul.
29:2–5. 2000.(In Chinese).
|
|
5
|
Dong GL, Kang ZH, Liu XN, Ji G, Wang CY,
Wang Y, Liu DH and Wang WZ: Effect of alanyl-glutamine on the
clinical outcome of patients after gastrectomy. Chin J Clin Nutr.
16:70–73. 2008.(In Chinese).
|
|
6
|
Li XH, Yi SY, Zhao J and Rou RL: Effects
of preoperative glutamine-supplemented enteral nutrition support on
immunity and inflammatory response in patients with gastric cancer
following radical operation. Front Med. 3:121–122. 2012.(In
Chinese).
|
|
7
|
Feng MH, Xiong B, Chen JK, Xue XB, Wu ZQ,
Yang GL, Wang F and Hu MB: Glutamine enhances heat shock protein 70
and attenuates tumor necrosis factor-α release in neoplastic
patients after operation. Chin J Exp Surg. 24:1589–1590. 2007.(In
Chinese).
|
|
8
|
Lu CY, Shih YL, Sun LC, Chuang JF, Ma CJ,
Chen FM, Wu DC, Hsieh JS and Wang JY: The inflammatory modulation
effect of glutamine-enriched total parenteral nutrition in
postoperative gastrointestinal cancer patients. Am Surg. 77:59–64.
2011.PubMed/NCBI
|
|
9
|
Richard V, Dahiya D, Kaman L, Raj P and
Behera A: Effect of perioperative glutamine administration on
C-reactive protein and liver function tests in patients undergoing
hepatic resection. Pol Przegl Chir. 86:11–16. 2014.PubMed/NCBI
|
|
10
|
Yeh CN, Lee HL, Liu YY, Chiang KC, Hwang
TL, Jan YY and Chen MF: The role of parenteral glutamine supplement
for surgical patient perioperatively: Result of a single center,
prospective and controlled study. Langenbecks Arch Surg.
393:849–855. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Xu XD, Sun YS, Shao QS, Hu JF, Qian ZY,
Zhou YL and Ye ZY: Effect of early enteral nutrition supplemented
with glutamine on postoperative intestinal mucosal barrier function
in patients with gastric carcinoma. Zhonghua Wei Chang Wai Ke Za
Zhi. 14:436–439. 2011.(In Chinese). PubMed/NCBI
|
|
12
|
Yang JT, Wang ZG and Zhu PF: Effect of
glutamine supplementation on cellular immunity in surgical
patients. Chin J Exp Surg. 16:124–126. 1999.(In Chinese).
|
|
13
|
Song JX, Qing SH, Huang XC and Qi DL:
Clinical importance of glutamine-supplemented parenteral nutrition
in patients with colorectal cancer. Chin J Clin Nutr. 10:165–168.
2002.(In Chinese).
|
|
14
|
Quan ZF, Yuan ZC and Li JS: Effects of
alanyl-glutamine dipeptide administration on postoperative
intestinal permeability and systemic inflammatory response.
Parenter Enter Nutr. 17:13–16. 2010.(In Chinese).
|
|
15
|
Lin MT, Kung SP, Yeh SL, Liaw KY, Wang MY,
Kuo ML, Lee PH and Chen WJ: Glutamine-supplemented total parenteral
nutrition attenuates plasma interleukin-6 in surgical patients with
lower disease severity. World J Gastroenterol. 11:6197–6201. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Jian ZM, Cao JD, Zhu XG, Zhao WX, Yu JC,
Ma EL, Wang XR, Zhu MW, Shu H and Liu YW: The impact of
alanyl-glutamine on clinical safety, nitrogen balance, intestinal
permeability, and clinical outcome in postoperative patients: A
randomized, double-blind, controlled study of 120 patients. JPEN J
Parenter Enteral Nutr. 23:(Suppl 5). S62–S66. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Quan ZF, Yang C, Li N and Li JS: Effect of
glutamine on change in early postoperative intestinal permeability
and its relation to systemic inflammatory response. World J
Gastroenterol. 10:1992–1994. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Zhu MW, Tang DN, Wei JM, Zhao X, Ye GD,
Long HK and Cao JD: Effects of glutamine dipeptide on plasma
endotoxin, outcome and health economy of elderly post-abdominal
operation patients. Chin J Geriatr. 24:585–588. 2005.(In
Chinese).
|
|
19
|
Zhu M, Tang D, Zhao X, Cao J, Wei J, Chen
Y, Xiao L and Sun Q: Impact of glutamine of gut permeability and
clinical prognosis on the aging patients undergoing
gastric-intestinal operation. Zhongguo Yi Xue Ke Xue Yuan Xue Bao.
22:425–427. 2000.(In Chinese). PubMed/NCBI
|
|
20
|
Zhao XL, He XD, Cui Q, Deng ZY and Yang Y:
Effects of glutamine on intestinal barrier function in patients
undergoing postoperative chemotherapy for gastric cancer. Chinese
Journal of General Surgery. 4:132–134. 2010.(In Chinese).
|
|
21
|
Gu YH, Ca H, Li YP and Yi Y: Effects of
glutamine on patients undergoing postoperative chemotherapy for
gastric cancer. Chin J Clin Nutr. 14:369–373. 2006.(In
Chinese).
|
|
22
|
Niu ZJ, Zhang XF, Zhao CL, Liu T and Zhai
ET: Value of glutamine in conservative treatment of patients with
intestinal obstruction after abdominal operation. World Chin J
Digestology. 19:3714–3718. 2011.(In Chinese).
|
|
23
|
Li JM, Lai DN and He XL: Support of
ala-glutamine-enriched parenteral nutrition on radical resection of
cardiac carcinoma patients. Journal of Abdominal Surgery.
19:226–228. 2006.(In Chinese).
|
|
24
|
Yao GX, Jiang ZM, Wang XR, Ma EL, Yang NF
and Zhao YP: Role of perioperative glutamine-dipeptide
supplementation on plasma endotoxin level, plasma endotoxin
inactivation capacity, and clinical outcome. Chin J Clin Nutr.
10:19–23. 2002.(In Chinese).
|
|
25
|
Yao GX, Xue XB, Jiang ZM, Yang NF and
Wilmore DW: Effects of perioperative parenteral glutamine-dipeptide
supplementation on plasma endotoxin level, plasma endotoxin
inactivation capacity and clinical outcome. Clin Nutr. 24:510–515.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
dos Santos R, Viana ML, Generoso SV,
Arantes RE, Davisson Correia MI and Cardoso VN: Glutamine
supplementation decreases intestinal permeability and preserves gut
mucosa integrity in an experimental mouse model. JPEN J Parenter
Enteral Nutr. 34:408–413. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Wu GH, Wang H, Zhang YW, Wu ZH and Wu ZG:
Glutamine supplemented parenteral nutrition prevents intestinal
ischemia- reperfusion injury in rats. World J Gastroenterol.
10:2592–2594. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
van der Hulst RR, van Kreel BK, von
Meyenfeldt MF, Brummer RJ, Arends JW, Deutz NE and Soeters PB:
Glutamine and the preservation of gut integrity. Lancet.
341:1363–1365. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Sablotzki A, Börgermann J, Baulig W,
Friedrich I, Spillner J, Silber RE and Czeslick E:
Lipopolysaccharide-binding protein (LBP) and markers of acute-phase
response in patients with multiple organ dysfunction syndrome
(MODS) following open heart surgery. Thorac Cardiovasc Surg.
49:273–278. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Taniguchi T and Minami Y: The IL-2/IL-2
receptor system: A current overview. Cell. 73:5–8. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Kubica P, Kot-Wasik A, Wasik A, Namieśnik
J and Landowski P: Modern approach for determination of lactulose,
mannitol and sucrose in human urine using HPLC-MS/MS for the
studies of intestinal and upper digestive tract permeability. J
Chromatogr B Analyt Technol Biomed Life Sci. 907:34–40. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Luk GD, Bayless TM and Baylin SB: Diamine
oxidase (histaminase). A circulating marker for rat intestinal
mucosal maturation and integrity. J Clin Invest. 66:66–70. 1980.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Ferrier L, Bérard F, Debrauwer L, Chabo C,
Langella P, Buéno L and Fioramonti J: Impairment of the intestinal
barrier by ethanol involves enteric microflora and mast cell
activation in rodents. Am J Pathol. 168:1148–1154. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Lin J, Nafday SM, Chauvin SN, Magid MS,
Pabbatireddy S, Holzman IR and Babyatsky MW: Variable effects of
short chain fatty acids and lactic acid in inducing intestinal
mucosal injury in newborn rats. J Pediatr Gastroenterol Nutr.
35:545–550. 2002. View Article : Google Scholar : PubMed/NCBI
|