Introduction
In 2013, 72,570 new cases of bladder cancer were
diagnosed and 15,210 deaths occurred in the United States (1). The majority of these cancers are
superficial bladder cancer at the first time of diagnosis (2), 20–40% and infiltrative associated with
a high risk of death (3,4). The radical surgical removal of the
bladder within urinary diversion remains the standard treatment in
the management of muscle invasive or high risk bladder cancer
(5).
Mainz pouch II, through the detubularized sigmoid
colon forms a high capacity pouch and low pressure, and was
introduced by Fisch et al (6). Several studies have demonstrated that
Mainz pouch II is a safe and accepted procedure of urinary
diversion with high continence rate and low incidence of
complications (7,8).
We performed total laparoscopic radical cystectomy
(LRC) with Mainz pouch II when our department had gained experience
in nearly 200 open radical cystectomy (ORC) and 23 LRC.
Patients and methods
Patients
During a period of 19 months from October 2010 to
April 2012, we performed total LRC in 5 patients with
muscle-invasive bladder cancer with Mainz pouch II as a urinary
diversion at the Department of Urology of Lanzhou University Second
Hospital. The patients included 5 men with a mean age of 58.8±7.6
years (range, 49–69 years). All patients underwent computed
tomography (CT) and other analysis.
Anaesthetic risk was I in 3 patients, and II in 2
patients according to the American Society of Anesthesiologists.
Only one patient underwent transurethral resection of bladder tumor
(TURBT) and received preoperative chemotherapy before surgery. This
study was approved by the Ethics Committee of the Second Hospital
of Lanzhou University. Signed written informed consents were
obtained from all participants before the study.
Surgical treatment
All patients received mechanical bowel preparation
and broad-spectrum antibiotic for 3 days before the surgical
procedure. The patients were given general anaesthesia, placed in a
lithotomy position and set in the Trendelenburg position at 25
degrees, bilateral leg bandages were applied. An immanent bladder
catheter was inserted using sterile techniques.
For placement of the camera port, first 10 mm trocar
was placed at superior crease of the umbilicus. The
pneumoperitoneum was established after insufflation of
CO2 to a pressure of 14–15 mmHg and then the second 5 mm
trocar and third 12 mm trocar were placed 2 cm below the umbilicus
in the midclavicular line on left and right sides respectively. The
fourth 5 mm trocar was 2–3 cm superior and medial to anterosuperior
iliac spines on the right side.
The peritoneum was opened on the furcation level
plane of the common iliac vessels was dissociated the ureter until
the bladder. The vasa deferentia and seminal vesicles were
dissected, starting dissection of the space of anterior bladder
wall after opening Denonvilliers fascia. At the end of this step,
dissection of the pelvic fascia and puboprostatic ligament was
performed. The deep dorsal vein of penis complex was controlled and
then ligation was performed with 1–0 Vicryl. Vascular control of
the prostatic pedicles, dorsal vein complex, urethra, prostate and
bladder were then completely clipped and transected, and the
bladder catheter was removed.
With the aid of unipolar forceps, ~24-cm segment of
the sigmoid and rectum 8 cm above anus was isolated
laparoscopically. Then, the dissected tissues were extracted in
Endo-Pouch through rectum using sponge forceps swingingly with
bladder body towards lower limbs avoiding the opened rectum
rupture.
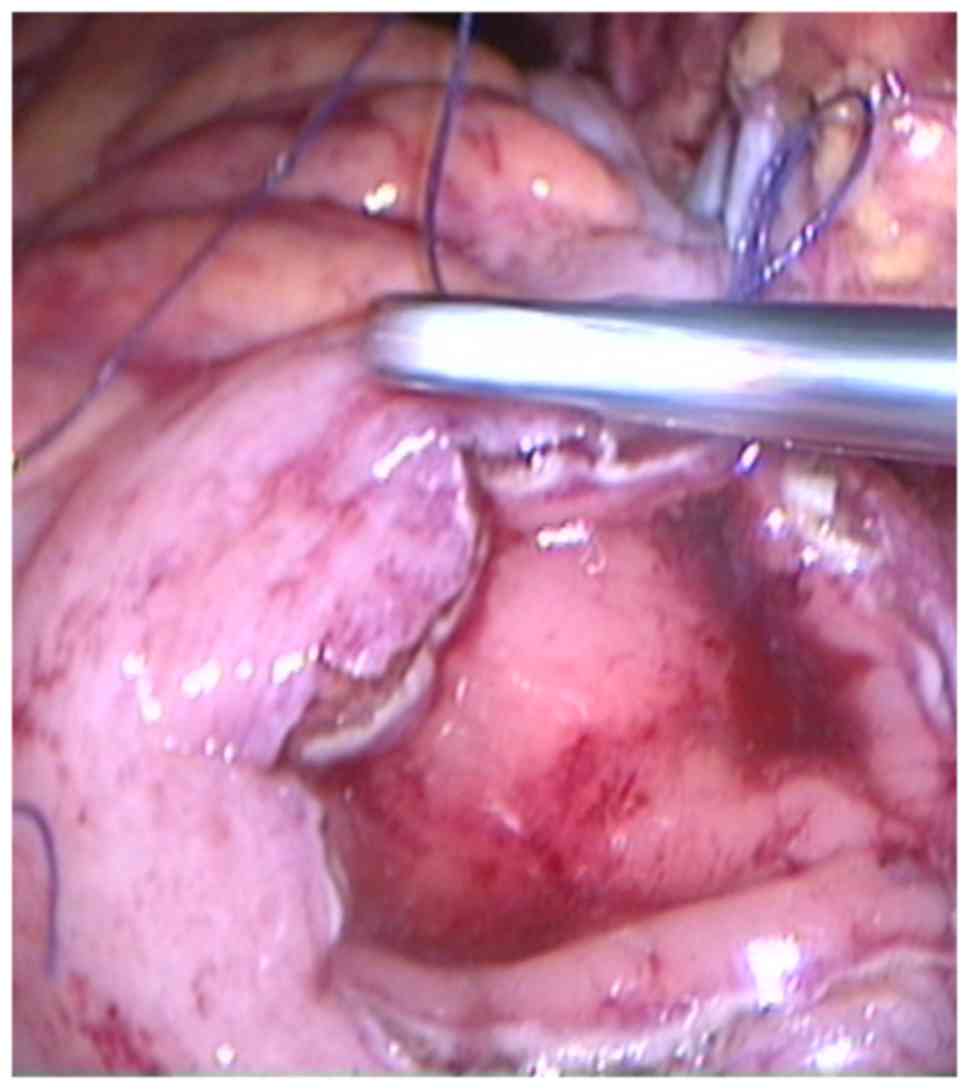
The posterior wall of the sigmoid and rectum were
stitched side-to-side using 3–0 polygalactin discontinuously and
then fixed to serosa by another 3–0 polygalactin, emerging from the
posterior wall of the pouch. The mobilized ureters were drawn
through the completed pouch plate and secured with sutures. Then a
papilla was formed by suturing the mucosa over the ureters to
perform an anti-reflux mechanism by laparoscopy (Fig. 1). Two F7 Double-J catheters were
placed into bilateral ureter and fixed at the drainage tube after a
drainage tube was inserted transanally. Eventually the anterior
wall of the pouch was closed laparoscopically using 3–0
polygalactin continuously. A F22 Foley catheter was placed for
drainage transurethrally.
Results
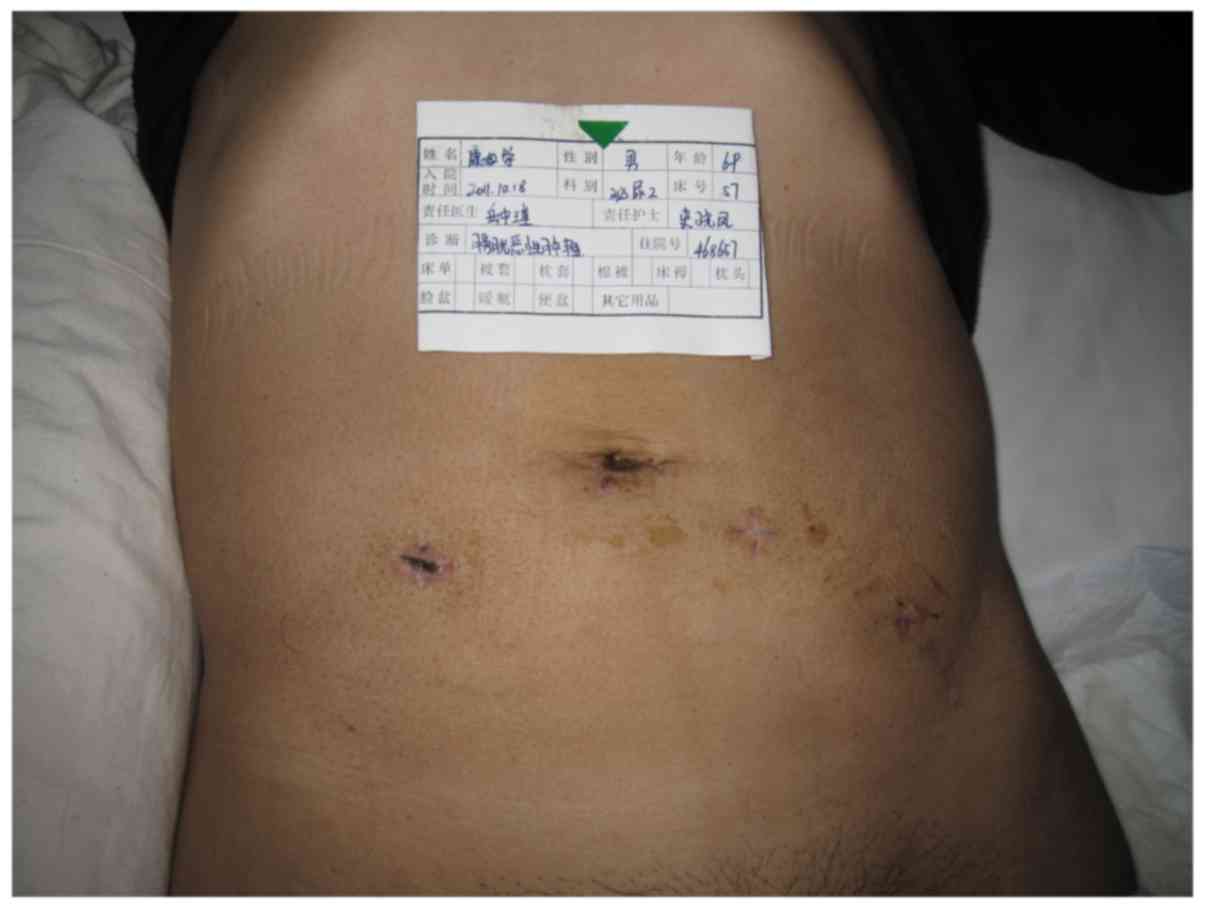
The follow-up time was 15.4±4.72 months (range 8–21
months). The urinary diversion were completed laparoscopically as
planned without any intraoperative or open conversion (Fig. 2).
The histological types observed were transitional
cell carcinoma in all five patients (100%). Further, the
pathological staging disclosed T2 in five (100%) cases. Two (40%)
cases were classified as grade II, three (60%) as grade III. Four
cases were initially diagnosed, the another case was second
management after cystoscopy with TURBT six months earlier.
Mean operative time was 577.0±126.4 min ranging
between 480 and 795 min. The patients were hospitalized for a mean
of 29.4±9.2 days ranging from 21 to 43 days. Average blood loss was
280.0±130.38 ml ranging from 100 to 400 ml. Two cases received
blood transfusion (300 and 400 ml, respectively).
After removal of the rectal tube, the patients were
continent, except two patients who had night incontinence, one case
had initial voiding interval of 1–1.5 h for the first month
post-operatively. However, three months post-operatively, the
patients were continent by day and night, except one who had
occasionally day incontinent when walking or coughing. The mean
voided volume was on 350.0±40.82 ml ranging between 300 and 400 ml
except one case had pyuria.
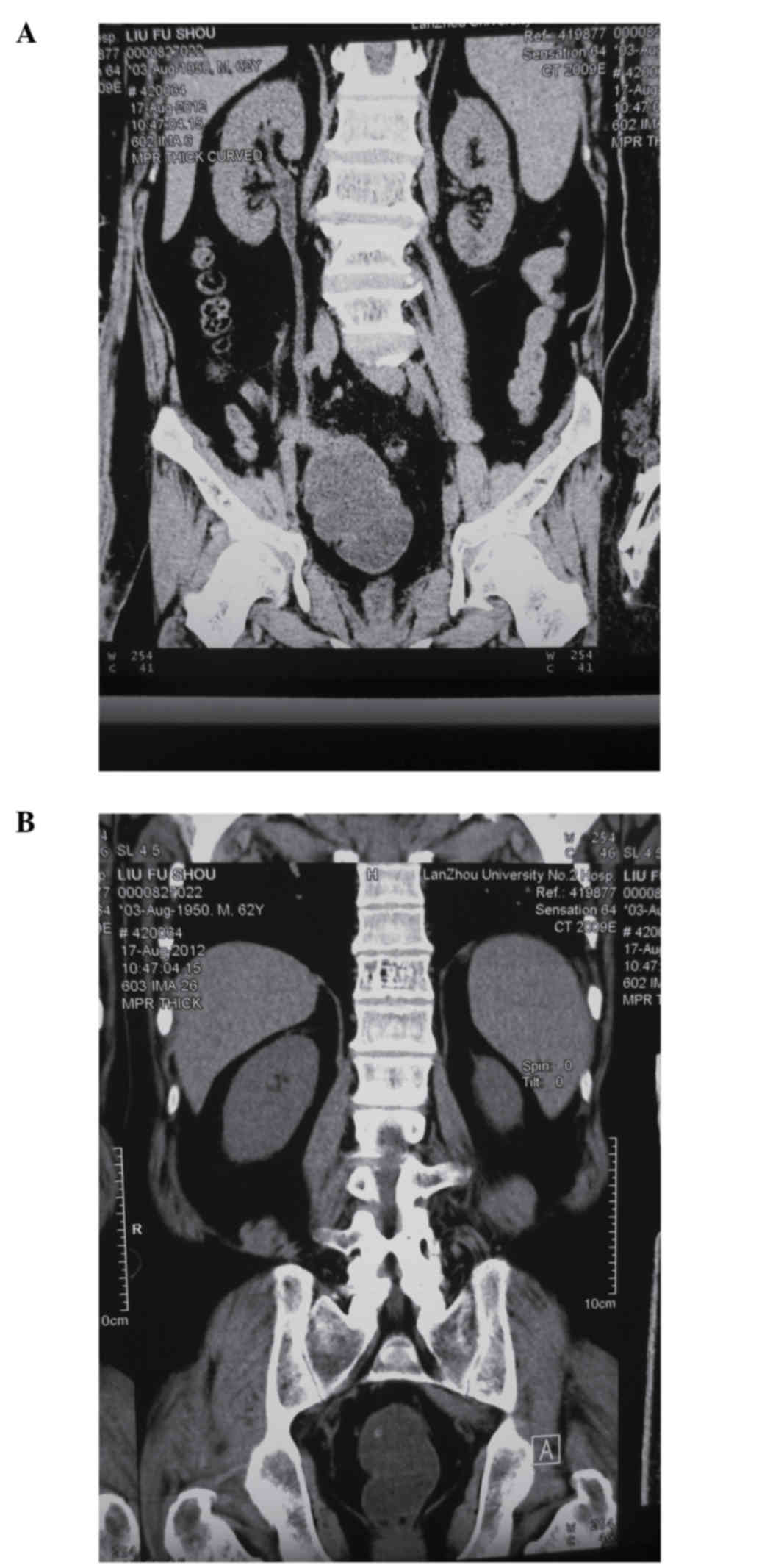
Cystography was performed post-operation to assess
the configuration of the upper urinary tract and to test the
antireflux procedure or leakage. As we can see, the upper urinary
tract did not show any back pressure signs according to the IVU
post-operatively (Figs. 3–5).
Immediate and late complications were observed in 2
cases. After Mainz II diversion one patient developed urinary
leakage seven days post-operatively and was treated with
antibiotics for twelve days. One case showed fever (39 degrees) and
a transanal drainage tube was placed for three days, and afterwards
no other adverse events occurred.
Discussion
Radical cystectomy is the standard for muscle
invasive or high risk bladder carcinoma (9). Laparoscopic treatment of infiltrative
bladder tumors was introduced to be one of the surgical approaches,
and developed to decrease the perioperative morbidity and trauma in
the field of minimally invasive surgery. It has been reported that
laparoscopic radical cystoprostatectomy with intracorporeal ileal
was conducted for urinary diversion for the first time in 2000
(10). Since then, several groups
reported the use of laparoscopy for radical cystectomy and
indicated the safety and practicability of LRC (11,12).
To our knowledge, LRC is not yet widely used in the
management of infiltrative bladder tumors in many areas because of
the technical difficulties of this approach, challenging urologist
to dissect large pelvic lymph node dissection (PLND), and lengthy
operative time.
Compared to ORC, LRC is conducive to expose vital
tissues in the pelvic cavity (e.g., the deep dorsal vein of penis
complex or sphincter urethra). LRC also leads to smaller vascular
injury intraoperatively compared to PLND, fast recovery, rapid
return to daily activities, and short postoperative hospital stay
time.
Park et al (12) reported their technique and initial
results in pure LRC for muscle-invasive bladder cancer. They
performed ileal conduit with a 6-cm sized midline incision
extracorporeally after LRC in thirty cases. The median operative
time required for extended bilateral PLVD was 527.5 min and no one
converted to open surgery. The results indicated that LRC is a
feasible management for invasive bladder cancer.
The laparoscopic group had more mean operative time,
significantly less mean blood loss, analgesic requirement and
transfusion requirement than in ORC group (13). The mean follow-up was 76 and 80% in
LRC and ORC groups, respectively. However, the results indicated
that pathological stage or grade, cancer-specific, and
recurrence-free survival rates were not significantly different
between the LRC and ORC groups in terms of 3-year overall survival
(64.2 vs. 72.6, 73.0 vs. 75.3 and 70.5 vs. 72.5%, respectively)
(14).
Nevertheless, the data for longer follow-up of LRC
in a larger cohort of patients is warranted to assess the
complications rate and oncologic outcomes in the robot assisted
area.
In our series, the mean operative time,
hospitalization days, average blood loss, and blood transfusion
rate were 577.0±126.4 min, 29.4±9.2 days, 280.0±130.38 ml, and 40%,
respectively, results were similar with the study of Park et
al (12). However, the operative
time was longer than those in other series. The longer time maybe
caused by PLND, and isolating laparoscopically the sigmoid 24-cm
segment with the aid of a unipolar forceps with a more punctilious
dissection.
In many series, an extended incision transperitoneal
approach ~6–10 cm was used. The scar of incision may effect the
aesthetic appreciation of the abdomen, especially for women.
Therefore, we isolated the sigmoid and rectum an incision instead
of transperitoneal approach, which avoids increasing mental strain
of patients and causing more trauma.
We also had a rate of incontinence of 20% (1 of 5
patients), which is higher than in other series. The reason may be
the limited number of cases. Unfortunately, there was no female
patient in our series. Thus, the difference of operative time,
blood loss, continence, or complications is still lacking.
In conclusion, total LRC with urinary diversion is
feasible for the management of muscle-invasive bladder cancer by
experienced surgeons despite the high level of difficulty of these
procedures. The key point is isolating the sigmoid and rectum a
segment with the aid of a unipolar forceps, which was performed
laparoscopically rather than making an extended incision by
transperitoneal approach. This approach shows the benefits of
laparoscopic surgery. However, more efficient performance of large
samples, more rigorous long-term randomized clinical controlled
trials on the outcomes and comparison with other approaches are
urgently needed.
Glossary
Abbreviations
Abbreviations:
|
LRC
|
laparoscopic radical cystectomy
|
|
TURBT
|
transurethral resection of bladder
tumor
|
|
PLND
|
pelvic lymph node dissection
|
|
ORC
|
open radical cystectomy
|
References
|
1
|
Siegel R, Naishadham D and Jemal A: Cancer
statistics, 2013. CA Cancer J Clin. 63:11–30. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Parkin DM: The global burden of urinary
bladder cancer. Scand J Urol Nephrol. (Suppl). 12–20. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Meller AE, Nesrallah LJ, DallOglio MF and
Srougi M: Complications in radical cystectomy performed at a
teaching hospital. Int Braz J Urol. 28:522–525. 2002.PubMed/NCBI
|
|
4
|
Rübben H, Lutzeyer W, Fischer N, Deutz F,
Lagrange W and Giani G: Natural history and treatment of low and
high risk superficial bladder tumors. J Urol. 139:283–285.
1988.PubMed/NCBI
|
|
5
|
Stenzl A, Cowan NC, De Santis M, Kuczyk
MA, Merseburger AS, Ribal MJ, Sherif A and Witjes JA: European
Association of Urology: Treatment of muscle-invasive and metastatic
bladder cancer: update of the EAU guidelines. Actas Urol Esp.
36:449–460. 2012.(In Spanish). View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Fisch M, Wammack R, Müller SC and
Hohenfellner R: The Mainz pouch II (sigma rectum pouch). J Urol.
149:258–263. 1993.PubMed/NCBI
|
|
7
|
Atta MA: Detubularized isolated
ureterosigmoidostomy: description of a new technique and
preliminary results. J Urol. 156:915–919. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Gilja I, Kovacić M, Radej M, Kosuta D,
Bakula B and Goles L: The sigmoidorectal pouch (Mainz pouch II).
Eur Urol. 29:210–215. 1996.PubMed/NCBI
|
|
9
|
Smith JA Jr: Surgical treatment of bladder
carcinoma: why is it underutilized? Cancer. 104:1563–1566. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Gill IS, Fergany A, Klein EA, Kaouk JH,
Sung GT, Meraney AM, Savage SJ, Ulchaker JC and Novick AC:
Laparoscopic radical cystoprostatectomy with ileal conduit
performed completely intracorporeally: the initial 2 cases.
Urology. 56:26–29; discussion 29–30. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Gao ZL, Fan J, Zhao JJ, Xia SJ, Shi L, Men
CP, Wang H, Wang L, Yang DD, Sun DK, et al: Laparoscopic radical
cystectomy with extracorporeal ileal conduit urinary diversion for
treatment of Chinese bladder cancer patients. Urol Int. 79:204–209.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Park B, Jeong BC, Jeon SS, Lee HM, Choi HY
and Seo SI: Pure laparoscopic radical cystectomy with ileal
conduit: a single surgeons mid-term outcomes. Yonsei Med J.
54:912–920. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Hemal AK and Kolla SB: Comparison of
laparoscopic and open radical cystoprostatectomy for localized
bladder cancer with 3-year oncological follow-up: a single surgeon
experience. J Urol. 178:2340–2343. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ha US, Kim SI, Kim SJ, Cho HJ, Hong SH,
Lee JY, Kim JC, Kim SW and Hwang TK: Laparoscopic versus open
radical cystectomy for the management of bladder cancer: mid-term
oncological outcome. Int J Urol. 17:55–61. 2010. View Article : Google Scholar : PubMed/NCBI
|