Introduction
In females, the most commonly diagnosed type of
cancer is breast cancer, which accounts for 23% of total cancer
cases and 14% of cancer-associated mortality (1,2). Due to
improved therapeutic strategies, the mortality rate for breast
cancer has decreased markedly. However, it remains a leading cause
of cancer-related mortality in females worldwide (1,2). The
deregulation of numerous oncogenes or tumor suppressors has been
demonstrated to participate in the development and progression of
breast cancer (3). Therefore,
studying the specific roles of these genes, as well as their
regulatory mechanisms, is promising for the development of
effective therapeutic strategies to treat breast cancer.
MicroRNAs (miRs), a type of endogenous small
non-coding RNA containing 22–25 nucleotides, are able to suppress
the expression of genes by directly binding to 3′-untranslated
region (UTR) of their target mRNAs, either causing translational
repression or leading to mRNA degradation (4). By negatively mediating their target
genes, miRs participate in a variety of cellular biological
processes including cell growth and proliferation, survival and
apoptosis, differentiation, migration and invasion (5–8).
Furthermore, it has been demonstrated that the deregulation of
certain miRs, such as miR-375, are involved in tumorigenesis and
tumor metastasis (9–11). Shi et al (12) demonstrated that miR-375 served a
suppressive role in osteosarcoma by targeting the PIK3CA gene. Shen
et al (13) suggested that
miR-375 may promote the epithelial-mesenchymal transition,
resulting in the development of chemo-resistance in cervical cancer
cells. Accordingly, miR-375 may exhibit the functions of an
oncogene or tumor suppressor in different human cancers and its
exact role is tumor-specific. Currently, the underlying molecular
mechanism by which miR-375 affects the biological processes of
breast cancer cells remains largely unknown.
Paired box (PAX) 6, a member of the PAX family, is
an important transcription factor associated with the development
of the eyes, pancreas and central nervous system (14,15).
Furthermore, it has been established that deregulated PAX6 is
involved different types of human cancer, including non-small cell
lung cancer (16), retinoblastoma
(17), glioma (18), colorectal cancer (19), prostate cancer (20) and breast cancer (21). Meng et al (21) demonstrated that miR-335 inhibited
cell cycle progression, colony formation, proliferation and
invasion by targeting PAX6 in breast cancer cells. This suggests
that PAX6 may be used as a potential target for the treatment of
breast cancer. Other miRs that are potentially involved in the
regulation of breast cancer by targeting PAX6 have not yet been
studied. Therefore, the present study aimed to investigate the role
and molecular mechanism of miR-375 in the regulation of breast
cancer growth and metastasis in vitro.
Materials and methods
Tissue collection
Breast cancer tissues (n=15) and their matched
adjacent normal tissues (n=15) were obtained from 15 female breast
cancer patients (44 to 67 years old) admitted to the Xiangya
Hospital of Central South University (Changsha, China) between
January and June 2014. Tissues were immediately snap-frozen in
liquid nitrogen following surgical resection and stored at −80°C
until use. The present study was approved by the Ethical Committee
of Xiangya Hospital of Central South University and written
informed consent was obtained from all patients.
Cell culture
The human breast cancer cell line Michigan Cancer
Foundation (MCF)-7 was purchased from the American Type Culture
Collection (Manassas, VA, USA) and cultured in passage in
Dulbecco's modified Eagle's medium (DMEM; Thermo Fisher Scientific,
Inc. Waltham, MA, USA) with 10% fetal bovine serum (FBS; Thermo
Fisher Scientific, Inc.) at 37°C with 5% CO2.
Reverse transcription-quantitative
polymerase chain reaction (RT-qPCR)
Total RNA of MCF-7 cells was isolated using TRIzol®
Reagent (Thermo Fisher Scientific, Inc.), in accordance with the
manufacturer's protocol. In order to detect miR-375 expression,
total RNA was reverse transcribed using the miScript II RT kit
(Qiagen, Hilden, Germany) in accordance with manufacturer's
protocol. qPCR was then conducted using the miScript SYBR Green PCR
kit (Qiagen). All reactions were performed using an ABI 7500 PCR
thermocycler (Thermo Fisher Scientific, Inc.). Primers were
purchased from Yearthbio, Changsha, China and the primer sequences
were commercially unavailable. The reaction conditions were as
follows: 95°C for 5 min, followed by 40 cycles of 95°C for 10 sec
and 60°C for 30 sec. Relative mRNA expression levels were
calculated using the 2−ΔΔCq method (22). The relative expression of miR was
normalized using U6.
Cell transfection
MCF-7 cells were transfected with miR-375 mimics
(Thermo Fisher Scientific, Inc.) or scrambled miR as a negative
control (miR-NC; Thermo Fisher Scientific, Inc.) using
Lipofectamine® 2000 (Thermo Fisher Scientific, Inc.) according to
the manufacturer's protocol. Briefly, MCF-7 cells were cultured to
70% confluence. miR-375 mimics, miR-NC, PAX6 plasmid (Yearthbio) or
Lipofectamine® 2000 were diluted with serum-free DMEM,
respectively. The diluted 100 nM Lipofectamine® 2000 was then mixed
with the diluted miR and incubated at room temperature for 20 min
prior to being added to the cell medium. Cells were incubated at
37°C in 5% CO2 for 6 h. The medium in each well of
6-well plates was then replaced by the normal serum-containing DMEM
medium and cultured for 24 h prior to subsequent assays.
Western blot analysis
Cells were lysed and protein was isolated in
radioimmunoprecipitation assay buffer (Thermo Fisher Scientific,
Inc.). The concentration of protein was quantified using a
bicinchoninic acid protein assay kit (Santa Cruz Biotechnology,
Inc., Dallas, TX, USA), according to the manufacturer's
instructions. A total of 50 µg protein from each sample was
separated using 12% SDS-PAGE and transferred onto a polyvinylidene
difluoride membrane (Thermo Fisher Scientific, Inc.). The membrane
was incubated with Tris-buffered saline and Tween-20 containing 5%
skimmed milk (China Mengniu Dairy Company Limited, Hong Kong,
China) at 37°C for 2 h. The membrane was then incubated with mouse
anti-PAX6 monoclonal antibody (1:100; ab197768; Abcam, Cambridge,
MA, USA), mouse anti-MMP2 monoclonal antibody (1:50; ab86607;
Abcam), mouse anti-MMP9 monoclonal antibody (1:50; ab58803; Abcam)
or mouse anti-GAPDH monoclonal antibody (1:400; ab8245; Abcam) at
room temperature for 3 h, respectively. The membrane was then
washed four times with phosphate buffered saline (PBS) and Tween 20
(PBST; Sigma-Aldrich; Merck kGaA, Darmstadt, Germany), for 10 min.
The membrane was incubated with the goat anti-mouse secondary
antibody (1:5,000; A4416; Sigma-Aldrich; Merck kGaA) at 4°C
overnight and washed a further four times for 10 min with PBST. An
Enhanced ECL Chemiluminescent Substrate Kit (Pierce Chemical,
Dallas, TX, USA) was used to perform chemiluminescent detection,
according to the manufacturer's instructions. Image-Pro plus
software version 6.0 (Media Cybernetics, Inc., Rockville, MD, USA)
was used to analyze the relative protein expression, presented as
the density ratio vs. GAPDH.
Luciferase reporter assay
The wild-type (WT) or mutant type (MUT) 3′-UTR of
PAX6 was inserted downstream of the luciferase reporter gene in the
pMIR-REPORT vector (Thermo Fisher Scientific, Inc.), generating
WT-PAX6 and MUT-PAX6. MCF-7 cells were co-transfected with miR-375
mimics/miR-NC, WT-PAX6/MUT-PAX6 and pRL-SV40 (Promega Corporation,
Madison, WI, USA) expressing Renilla luciferase. Following
48 h incubation at 37°C with 5% CO2, the luciferase
activity was measured using the Dual-Luciferase® Reporter Assay
System (Promega Corporation). Cells in the control group were
co-transfected with WT-PAX6/MUT-PAX6 and pRL-SV40 expressing
Renilla luciferase.
Cell viability analysis
To measure cell viability, an MTT assay was
performed. At 72 h post-transfection, a 100 µl cell suspension
(5,000 cells/ml) was seeded into 96-well plates and incubated at
37°C with 5% CO2 for 12, 24, 48 or 72 h. For the MTT
assay, 100 µl fresh serum-free DMEM with 0.5 g/l MTT replaced the
transfection medium in each well. Following 4 h incubation at 37°C,
the MTT medium was removed by aspiration and 50 µl dimethyl
sulfoxide was added to each well. Formazan production was detected
following 10 min at room temperature using an ELx800 Absorbance
Reader (BioTek Instruments, Inc., Winooski, VT, USA) to measure the
optical density at a wavelength of 570 nm.
Cell migration assay
To examine the cell migratory capacity,
1×105 cells/well MCF-7 cells in each group were cultured
in DMEM with 10% FBS to 100% confluence. Wounds of ~1 mm width were
created with a plastic scriber and cells were washed once using
PBS. Following 48 h culture at 37°C with 5% CO2, MCF-7
cells were observed under an inverted microscope (Olympus
Corporation, Tokyo, Japan).
Cell invasion assay
Transwell Chambers pre-coated with Matrigel (BD
Bioscience, San Jose, CA, USA) were used to examine cell invasion
capacity. Briefly, a suspension of MCF-7 cells (5×105
cells/ml) in each group was prepared in DMEM. A total of 300 µl
cell suspension was added to the upper chamber, while 500 µl DMEM
with 10% FBS was added to the lower chamber. Following 24 h
incubation at 37°C with 5% CO2, cells that did not
invade through the pores were wiped out using a cotton-tipped swab.
The filters were stained using 0.1% crystal violet and the invasive
cell number was determined from five randomly selected fields under
an inverted microscope (Olympus Corporation).
Statistical analysis
All data were expressed as mean ± standard deviation
of triplicate experiments. Statistical analysis was performed using
SPSS 17.0 statistical software (SPSS, Inc., Chicago, IL, USA). Data
was analyzed by one-way analysis of variance followed by Tukey post
hoc test or Student's t-test and P<0.05 was considered to
represent a statistically significant difference.
Results
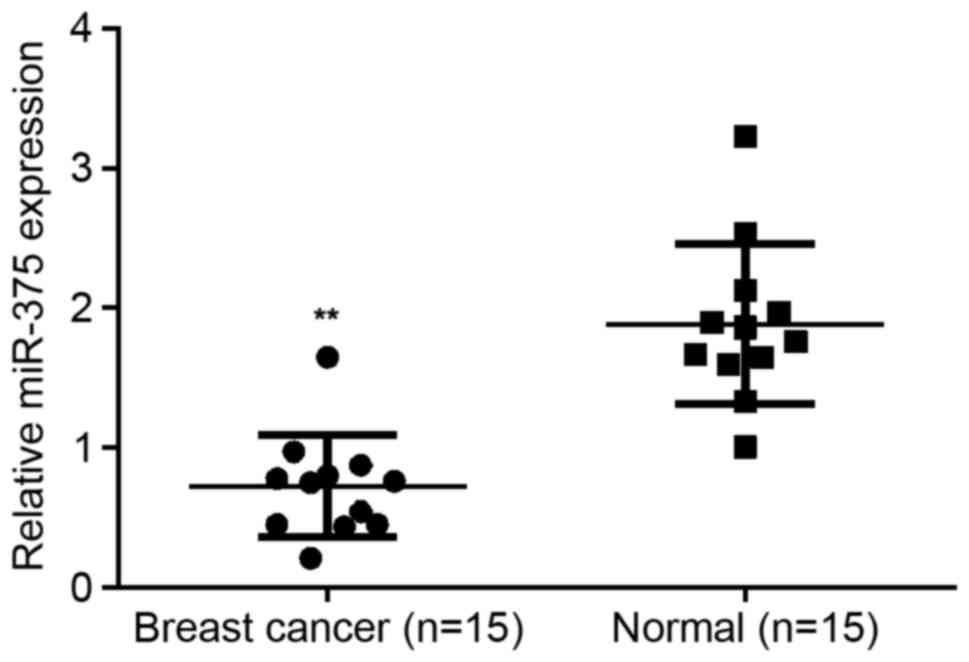
miR-375 is significantly downregulated
in breast cancer
To reveal the exact role of miR-375 in breast
cancer, RT-qPCR was conducted to examine the expression of miR-375
in breast cancer tissues as well as their matched normal adjacent
tissues. It was determined that miR-203 expression was
significantly decreased in breast cancer tissues compared with
their matched normal adjacent tissues (P<0.01; Fig. 1), suggesting that miR-375 may serve a
suppressive role in breast cancer.
miR-375 negatively mediates the
viability, migration and invasion of breast cancer cells
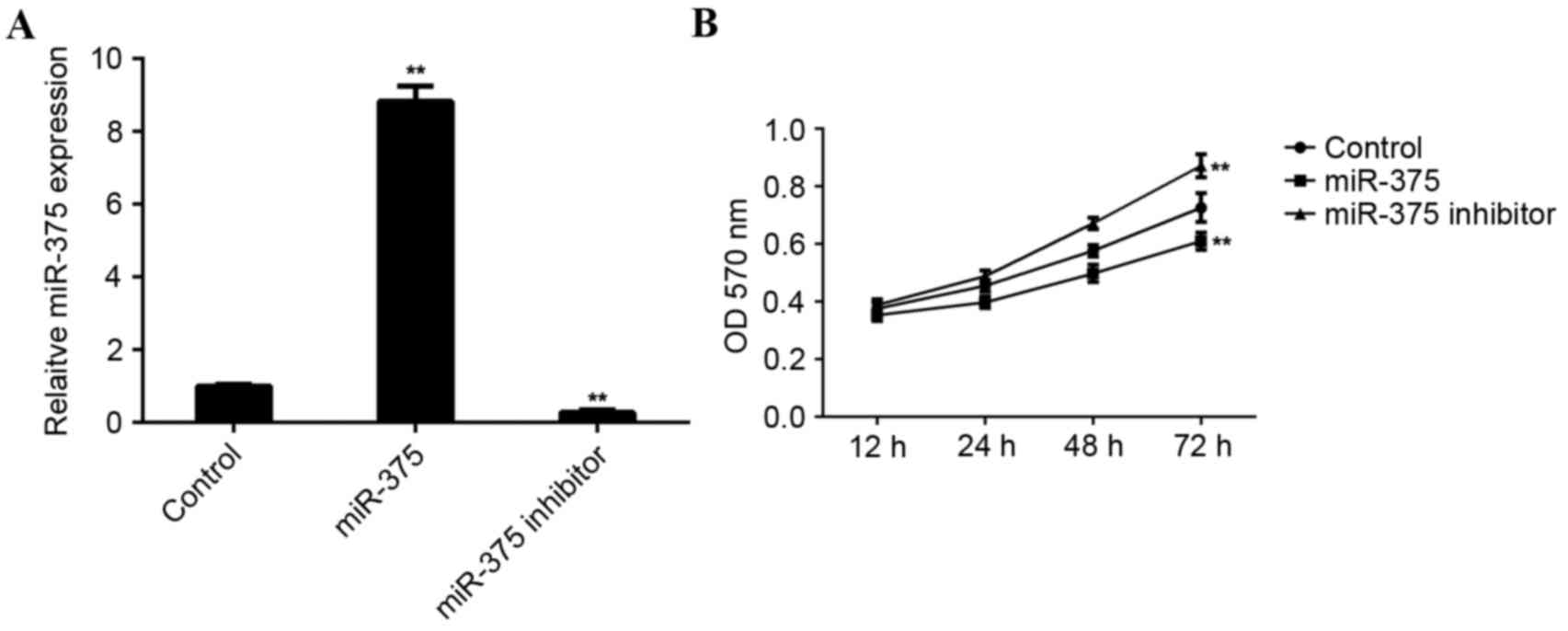
MCF-7 cells were used to investigate the role of
miR-375 in breast cancer in vitro. MCF-7 cells were
transfected with miR-375 mimic or miR-375 inhibitor. Following
transfection, RT-qPCR was conducted to examine levels of miR-375.
Transfection with miR-375 mimic led to a significant increase in
miR-375 levels (P<0.01), while transfection with miR-375
inhibitor led to a significant decrease in the level of miR-375 in
MCF-7 cells (P<0.01; Fig.
2A).
An MTT assay was conducted to determine the cell
viability rate in each group. Overexpression of miR-375
significantly inhibited MCF-7 cell viability (P<0.01). By
contrast, downregulation of miR-375 significantly promoted MCF-7
cell viability (P<0.01; Fig. 2B),
suggesting that miR-375 may serve a suppressive role in breast
cancer growth.
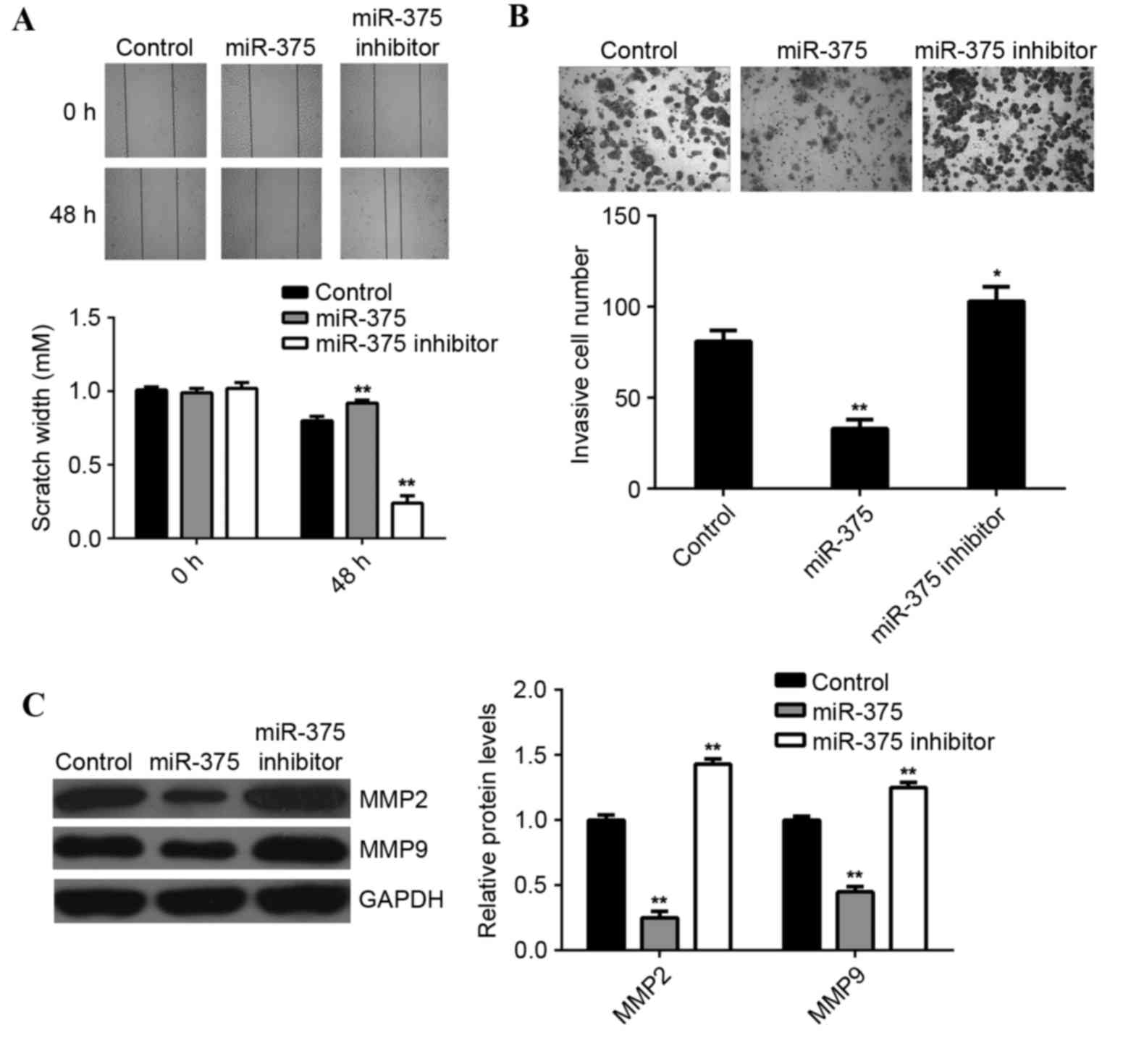
Tumor cell migration and invasion are two key
processes that occur during cancer metastasis, therefore the
effects of miR-375 on breast cancer cell migration and invasion
were further examined. Wound scratch assay data indicated that,
compared with the control group, overexpression of miR-375
significantly suppressed MCF-7 cell migration (P<0.01), while
inhibition of miR-375 led to a significant increase in the
migration of MCF-7 cells (P<0.01; Fig. 3A). Furthermore, the transwell
migration assay data indicated that overexpression of miR-375
significantly inhibited MCF-7 cell invasion (P<0.01), while
knockdown of miR-375 markedly enhanced MCF-7 cell migration, when
compared to the control group (P<0.05; Fig. 3B). This suggests that miR-375 may
have a suppressive effect on breast cancer metastasis. Moreover,
overexpression of miR-375 significantly reduced the MMP2 and MMP9
protein expression (P<0.01; Fig.
3C), while inhibition of miR-375 promoted the protein
expression of MMP2 and MMP9 in MCF-7 cells (P<0.01; Fig. 3C).
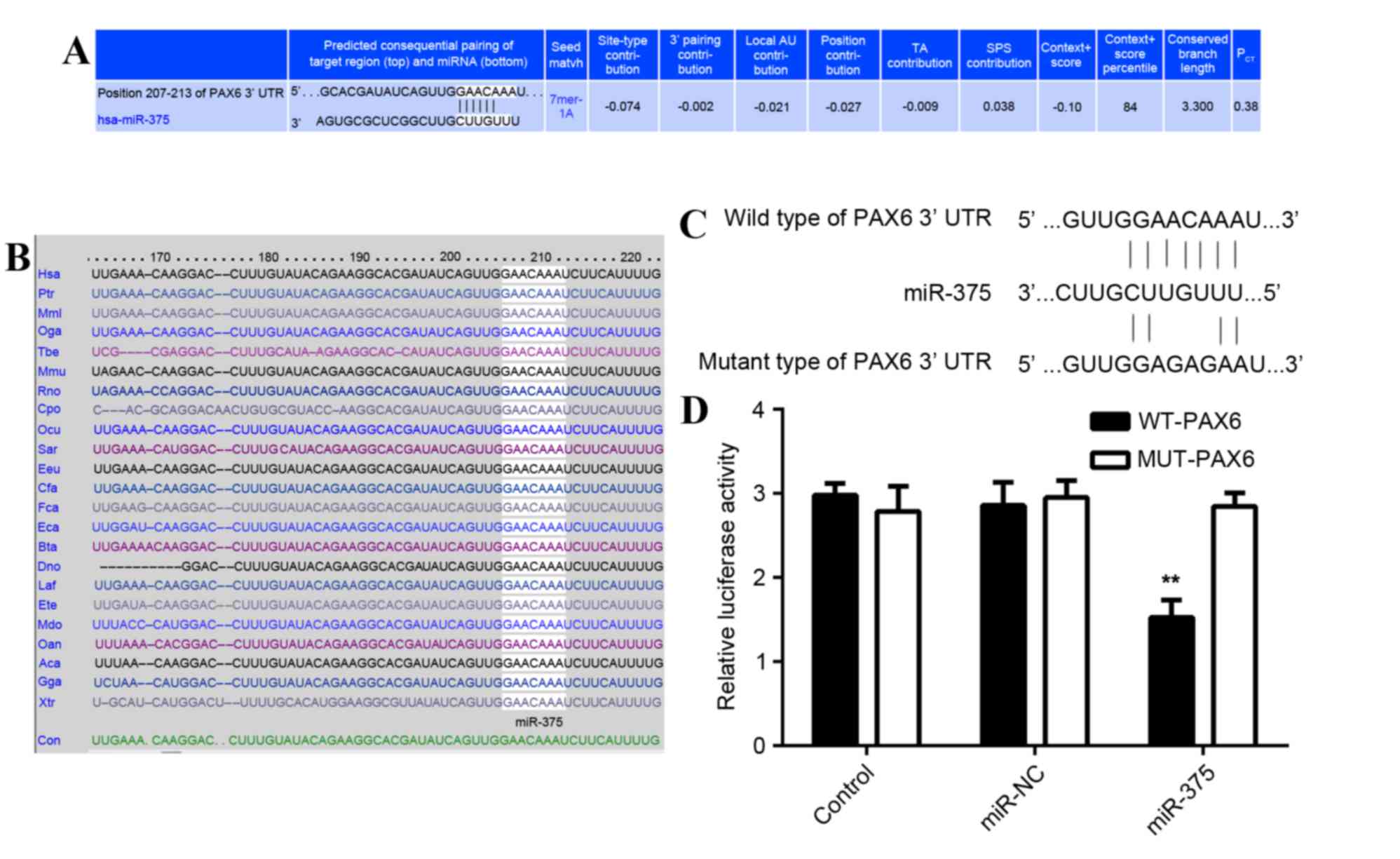
PAX6 is a direct target of
miR-375
As predicted by the online software Targetscan
(http://www.targetscan.org/vert_61/)
PAX6 is a putative target of miR-375 (Fig. 4A) and this targeting association is
evolutionally conserved (Fig. 4B).
To determine whether PAX6 was a direct target of miR-375, the WT
3′-UTR or MUT of PAX6 mRNA was inserted downstream of the
luciferase reporter gene in an apMIR-REPORT vector (Fig. 4C). A luciferase reporter assay was
then performed. In miR-375 and WT PAX6 3′-UTR co-transfected MCF-7
cells, the Renilla/firefly value of luciferase was
significantly reduced compared with the control group (P<0.01;
Fig. 4D). However, in MCF-7 cells
co-transfected with miR-375 mimic and MUT 3′UTR of PAX6, the
Renilla/firefly value of luciferase did not decrease
(Fig. 4D), indicating that miR-375
does not bind to the MUT 3′UTR of PAX6. The results suggest that
PAX6 is a novel target of miR-375.
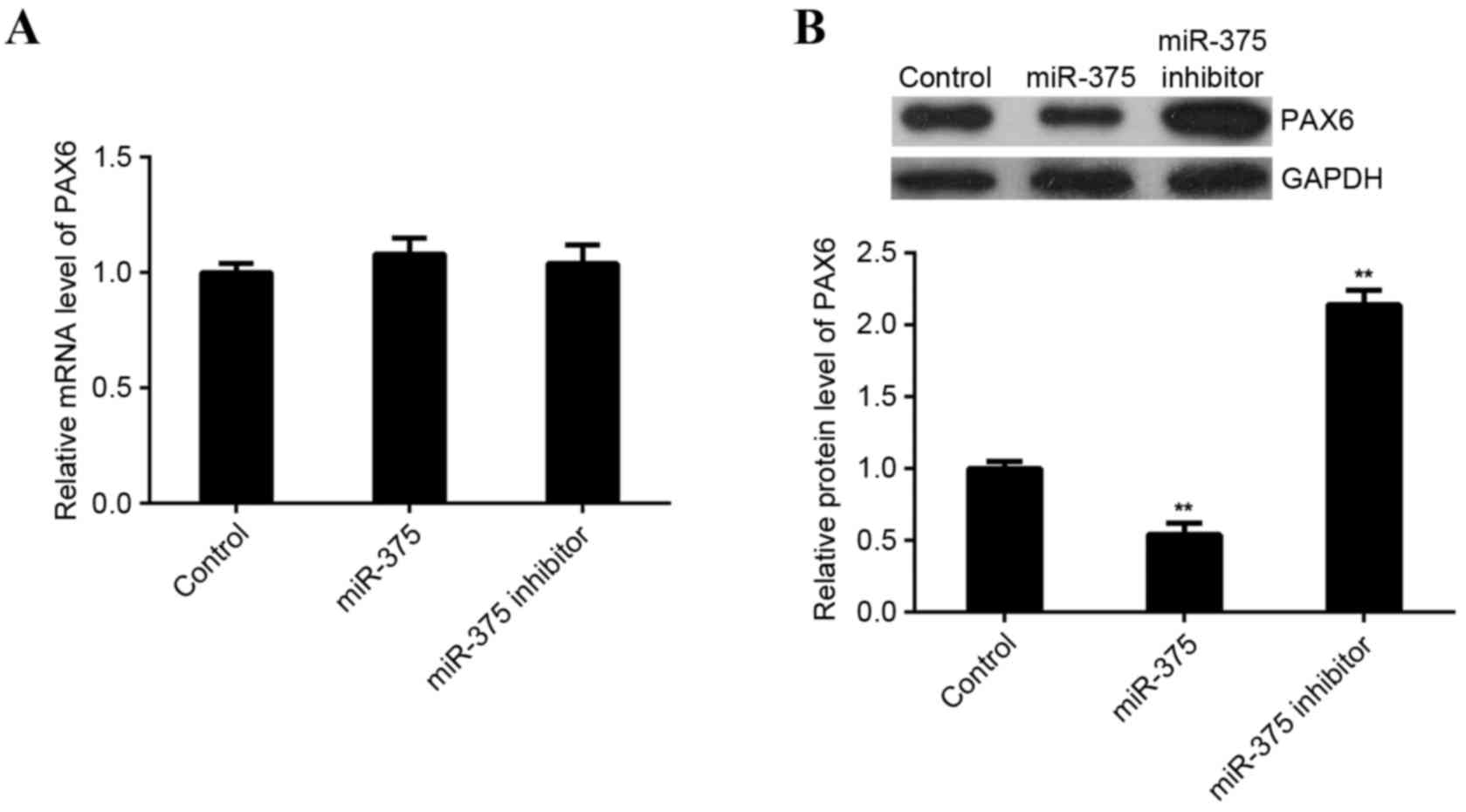
miR-375 negatively regulates the
protein expression of PAX6 in MCF-7 cells
As miRs typically inhibit the expression of their
target genes at a post-transcriptional level, the effects of
miR-375 overexpression and downregulation on the expression of PAX6
protein in MCF-7 cells was investigated. RT-qPCR and western blot
analysis were performed to examine levels of PAX6 mRNA and protein
in miR-375-upregulating or -downregulating MCF-7 cells. miR-375 did
not affect expression of PAX6 mRNA in MCF-7 cells (Fig. 5A). However, levels of PAX6 protein
were significantly reduced following upregulation of miR-375
(P<0.01) and significantly increased following miR-375 knockdown
in MCF-7 cells (P<0.01; Fig. 5B).
These findings indicate that miR-375 negatively mediates the
expression of PAX6 at the post-transcriptional level in breast
cancer cells.
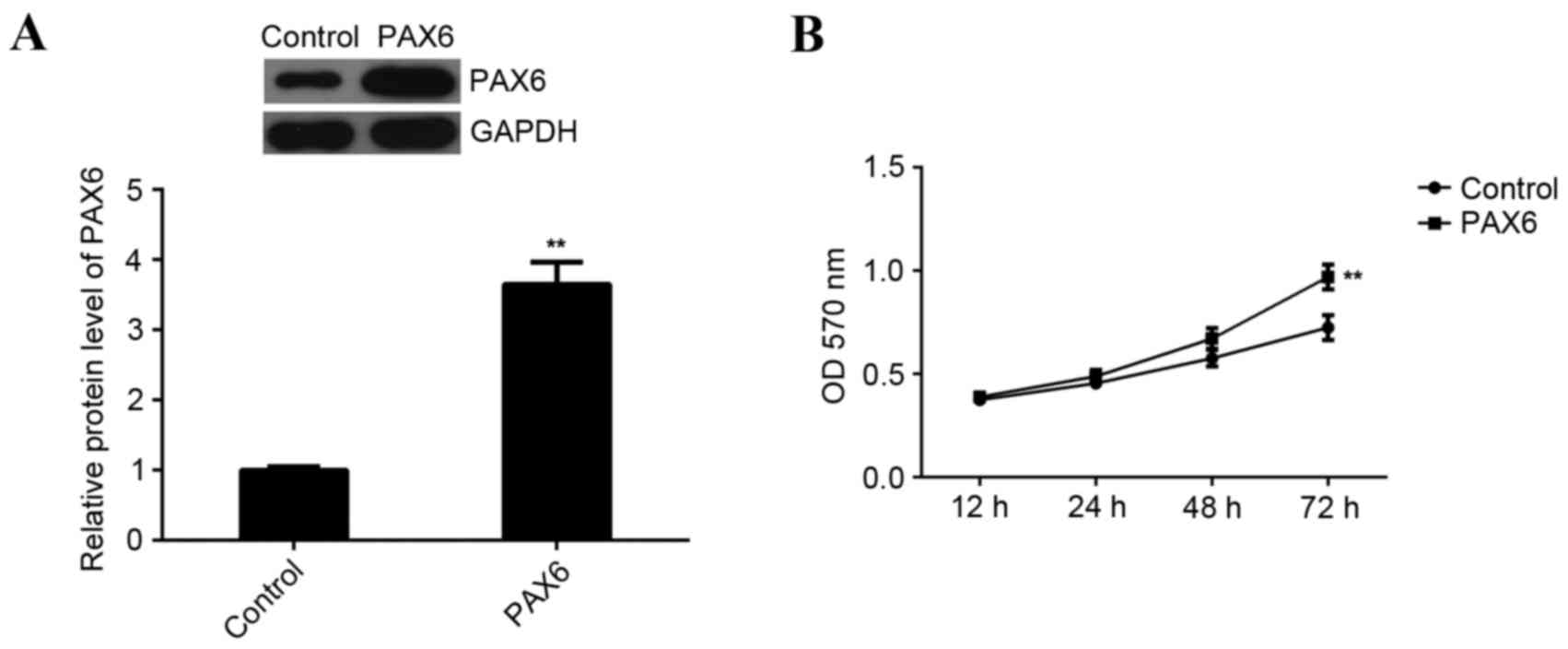
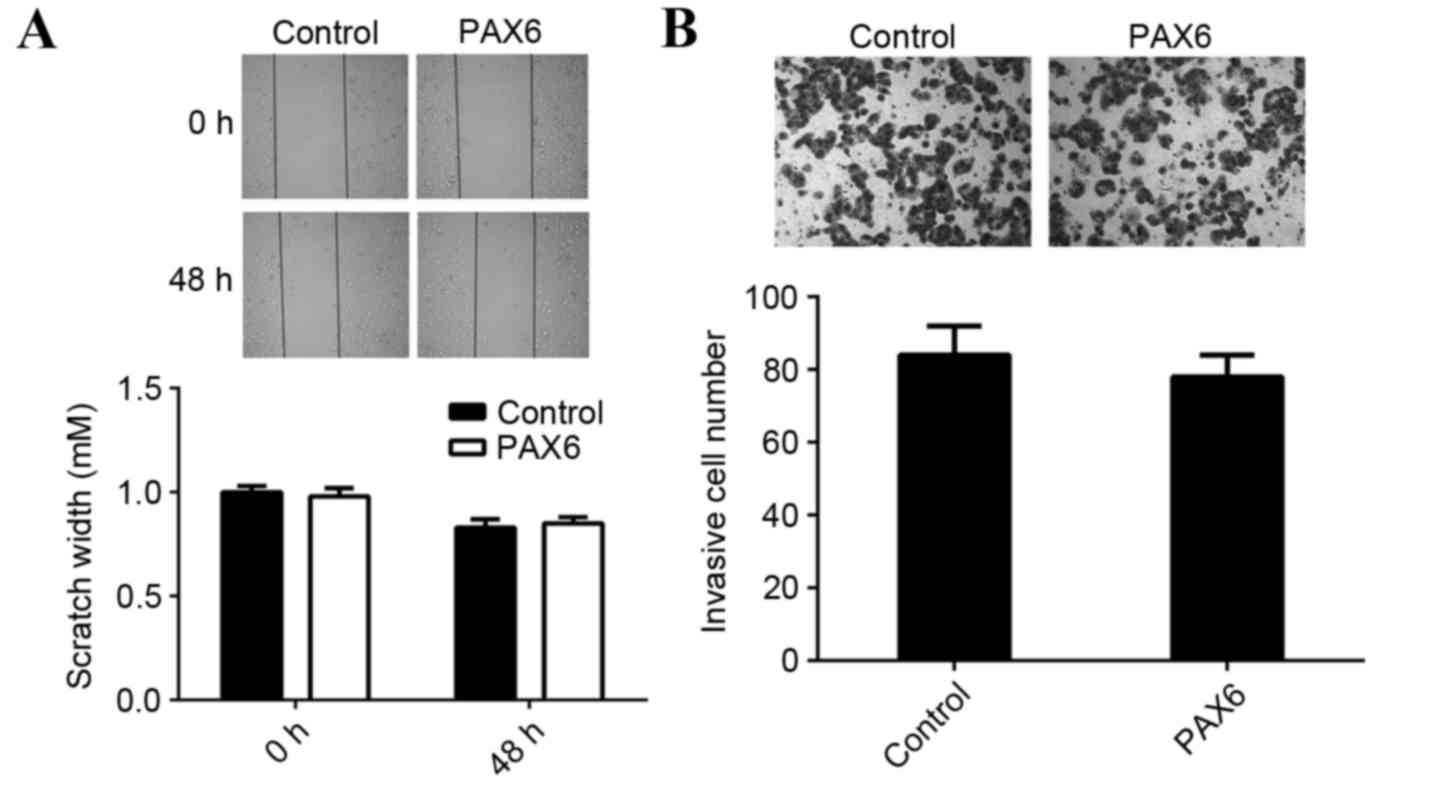
Overexpression of PAX6 inhibits cell
viability but has no effect on cell migration and invasion in MCF-7
cells
Based the aforementioned results of the present
study, the inhibitory effects of miR-375 on MCF-7 cell viability,
migration and invasion may occur via inhibition of PAX6. Thus,
MCF-7 cells were transfected with a PAX6 plasmid to upregulate PAX6
expression. Following transfection, western blot analysis data
indicated that the expression of PAX6 protein was significantly
increased compared with the control group (P<0.01; Fig. 6A). Furthermore, MTT assay data
indicated that overexpression of PAX6 significantly promoted MCF-7
cell viability compared to the control group (P<0.01; Fig. 6B). This indicates that PAX6 is
involved in the regulation of miR-375-mediated MCF-7 cell
viability. However, overexpression of PAX6 did not affect the
migration and invasion of MCF-7 cells compared with the control
group (Fig. 7). Therefore, PAX6 may
primarily regulate breast cancer growth but not metastasis and the
suppressive role of miR-375 in the regulation of MCF-7 cell
migration and invasion may occur due to mediation of other
targets.
Discussion
miRs act as key regulators in different types of
human cancer by negatively mediating their target genes, which are
oncogenes or tumor suppressors (9–11).
Deregulated miR-375 has been identified in numerous cancer types,
including laryngeal squamous cell carcinoma (23), head and neck squamous cell carcinoma
(24), prostate cancer (25), hepatocellular carcinoma (26), lung cancer (27) and breast cancer (28). Wu et al (29) examined the circulating miR profile in
patients with breast cancer by deep sequencing all circulating
small RNAs. Circulating miR-375 and miR-122 demonstrated a strong
association with the clinical outcome, including neoadjuvant
chemotherapy responses and relapse with metastatic disease
(29), suggesting that miR-375 is
involved in breast cancer.
The suppressive role of miR-375 in breast cancer has
been determined. Ye et al (30) demonstrated that miR-375 was
downregulated in human epidermal growth factor receptor 2-positive
breast cancer and its downregulation induced trastuzumab resistance
by targeting insulin like growth factor 1. Furthermore, it was
indicated that miR-375 inhibits the epithelial-to-mesenchymal
transition in breast cancer by targeting the short stature homeobox
2 gene (31). However, the detailed
molecular mechanism of miR-375 in the regulation of breast cancer
remains largely unknown. In the present study, it was observed that
miR-375 expression was reduced in breast cancer tissues compared
with matched adjacent normal tissues. Overexpression of miR-375
significantly suppressed the viability, migration and invasion of
breast cancer cells, suggesting that miR-375 acts as a tumor
suppressor in breast cancer.
To further reveal the underlying molecular
mechanism, the targets of miR-375 in breast cancer cells were
investigated in the present study. PAX6 was predicted to be a
putative target gene of miR-375. To clarify this prediction, a
luciferase reporter assay was completed. This, to the best of our
knowledge, was the first time PAX was identified as a direct target
of the miR-375 gene. Furthermore, it was demonstrated that miR-375
negatively mediates the expression of PAX6 protein in breast cancer
cells.
PAX6 is a member of the PAX gene family and acts as
a key regulator in the development of the eyes, central nervous
system and pancreas (15,32,33).
Furthermore, it has been demonstrated that PAX6 serves an oncogenic
role in breast cancer. Knockdown of PAX6 expression markedly
suppresses the viability, DNA synthesis and colony formation of
breast cancer MCF-7 and MDA-MB-231 cells, and significantly
inhibits tumorigenesis in xenograft nude mice (34). Knockdown of PAX6 expression also led
to an arrest at the G0/G1 phase in breast cancer cells (34). In the present study, overexpression
of PAX6 significantly enhanced MCF-7 cell viability, indicating
that PAX6 promotes the cell viability of breast cancer cells. As
miR-375 negatively regulated the expression of PAX6 protein in
MCF-7 cells, it is suggested that the inhibitory effect of miR-375
on MCF-7 cell viability may occur directly by inhibiting PAX6
expression. However, overexpression of PAX6 did not affect the
migration and invasion of MCF-7 cells, suggesting that PAX6 has no
effect on breast cancer metastasis. Thus, the suppressive role of
miR-375 in the regulation of MCF-7 cell migration and invasion may
occur via mediation of other targets. It has been demonstrated that
PAX6 mediates cell invasion in different types of cancer, including
lung cancer (16), glioma (18), glioblastoma (35,36) and
colorectal cancer (19). Therefore,
the role of PAX6 in cancer cell metastasis may potentially be
tumor-specific.
In conclusion, to the best of our knowledge, the
present study is the first to demonstrate that miR-375 is
downregulated in breast cancer and negatively mediates the
viability, migration and invasion of breast cancer cells. This
inhibitory effect of miR-375 on breast cancer cell viability partly
occurred via the direct targeting of PAX6. Knowledge of the
molecular mechanism of miRs in breast cancer has been expanded and
suggests that the miR-375/PAX6 axis may be a promising target for
the treatment of breast cancer in the future.
References
|
1
|
Siegel R, Naishadham D and Jemal A: Cancer
statistics, 2013. CA Cancer J Clin. 63:11–30. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wu Y, Sarkissyan M and Vadgama JV:
Epithelial-mesenchymal transition and breast cancer. J Clin Med.
5(pii): E132016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Cullen BR: MicroRNAs as mediators of viral
evasion of the immune system. Nat Immunol. 14:205–210. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Chen LJ, Lim SH, Yeh YT, Lien SC and Chiu
JJ: Roles of microRNAs in atherosclerosis and restenosis. J Biomed
Sci. 19:792012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Esau C, Kang X, Peralta E, Hanson E,
Marcusson EG, Ravichandran LV, Sun Y, Koo S, Perera RJ, Jain R, et
al: MicroRNA-143 regulates adipocyte differentiation. J Biol Chem.
279:52361–52365. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Fish JE, Santoro MM, Morton SU, Yu S, Yeh
RF, Wythe JD, Ivey KN, Bruneau BG, Stainier DY and Srivastava D:
miR-126 regulates angiogenic signaling and vascular integrity. Dev
Cell. 15:272–284. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Yates LA, Norbury CJ and Gilbert RJ: The
long and short of microRNA. Cell. 153:516–519. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Serpico D, Molino L and Di Cosimo S:
microRNAs in breast cancer development and treatment. Cancer Treat
Rev. 40:595–604. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Esquela-Kerscher A and Slack FJ:
Oncomirs-microRNAs with a role in cancer. Nat Rev Cancer.
6:259–269. 2006. View
Article : Google Scholar : PubMed/NCBI
|
|
11
|
Luo J, Wu J, Li Z, Qin H, Wang B, Wong TS,
Yang W, Fu QL and Lei W: miR-375 suppresses IGF1R expression and
contributes to inhibition of cell progression in laryngeal squamous
cell carcinoma. Biomed Res Int. 2014:3745982014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Shi ZC, Chu XR, Wu YG, Wu JH, Lu CW, Lü
RX, Ding MC and Mao NF: MicroRNA-375 functions as a tumor
suppressor in osteosarcoma by targeting PIK3CA. Tumour Biol.
36:8579–8584. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Shen Y, Zhou J, Li Y, Ye F, Wan X, Lu W,
Xie X and Cheng X: miR-375 mediated acquired chemo-resistance in
cervical cancer by facilitating EMT. PLoS One. 9:e1092992014.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Yamaoka T and Itakura M: Development of
pancreatic islets (review). Int J Mol Med. 3:247–261.
1999.PubMed/NCBI
|
|
15
|
Elso C, Lu X, Weisner PA, Thompson HL,
Skinner A, Carver E and Stubbs L: A reciprocal translocation
dissects roles of Pax6 alternative promoters and upstream
regulatory elements in the development of pancreas, brain, and eye.
Genesis. 51:630–646. 2013.PubMed/NCBI
|
|
16
|
Luo J, Li H and Zhang C: MicroRNA-7
inhibits the malignant phenotypes of non-small cell lung cancer in
vitro by targeting Pax6. Mol Med Rep. 12:5443–5448. 2015.PubMed/NCBI
|
|
17
|
Meng B, Wang Y and Li B: Suppression of
PAX6 promotes cell proliferation and inhibits apoptosis in human
retinoblastoma cells. Int J Mol Med. 34:399–408. 2014.PubMed/NCBI
|
|
18
|
Cheng Q, Cao H, Chen Z, Ma Z, Wan X, Peng
R and Jiang B: PAX6, a novel target of miR-335, inhibits cell
proliferation and invasion in glioma cells. Mol Med Rep.
10:399–404. 2014.PubMed/NCBI
|
|
19
|
Li Y, Li Y, Liu Y, Xie P, Li F and Li G:
PAX6, a novel target of microRNA-7, promotes cellular proliferation
and invasion in human colorectal cancer cells. Dig Dis Sci.
59:598–606. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Shyr CR, Tsai MY, Yeh S, Kang HY, Chang
YC, Wong PL, Huang CC, Huang KE and Chang C: Tumor suppressor PAX6
functions as androgen receptor co-repressor to inhibit prostate
cancer growth. Prostate. 70:190–199. 2010.PubMed/NCBI
|
|
21
|
Meng Y, Zou Q, Liu T, Cai X, Huang Y and
Pan J: microRNA-335 inhibits proliferation, cell-cycle progression,
colony formation, and invasion via targeting PAX6 in breast cancer
cells. Mol Med Rep. 11:379–385. 2015.PubMed/NCBI
|
|
22
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(−Delta Delta C(T)) Method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Hu A, Huang JJ, Xu WH, Jin XJ, Li JP, Tang
YJ, Huang XF, Cui HJ, Sun GB, Li RL and Duan JL: MiR-21/miR-375
ratio is an independent prognostic factor in patients with
laryngeal squamous cell carcinoma. Am J Cancer Res. 5:1775–1785.
2015.PubMed/NCBI
|
|
24
|
Jimenez L, Sharma VP, Condeelis J, Harris
T, Ow TJ, Prystowsky MB, Childs G and Segall JE: MicroRNA-375
suppresses extracellular matrix degradation and invadopodial
activity in head and neck squamous cell carcinoma. Arch Pathol Lab
Med. 139:1349–1361. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Costa-Pinheiro P, Ramalho-Carvalho J,
Vieira FQ, Torres-Ferreira J, Oliveira J, Gonçalves CS, Costa BM,
Henrique R and Jerónimo C: MicroRNA-375 plays a dual role in
prostate carcinogenesis. Clin Epigenetics. 7:422015. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Wen Y, Han J, Chen J, Dong J, Xia Y, Liu
J, Jiang Y, Dai J, Lu J, Jin G, et al: Plasma miRNAs as early
biomarkers for detecting hepatocellular carcinoma. Int J Cancer.
137:1679–1690. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Patnaik S, Mallick R, Kannisto E, Sharma
R, Bshara W, Yendamuri S and Dhillon SS: MiR-205 and MiR-375
microRNA assays to distinguish squamous cell carcinoma from
adenocarcinoma in lung cancer biopsies. J Thorac Oncol. 10:446–453.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Erbes T, Hirschfeld M, Rücker G, Jaeger M,
Boas J, Iborra S, Mayer S, Gitsch G and Stickeler E: Feasibility of
urinary microRNA detection in breast cancer patients and its
potential as an innovative non-invasive biomarker. BMC Cancer.
15:1932015. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Wu X, Somlo G, Yu Y, Palomares MR, Li AX,
Zhou W, Chow A, Yen Y, Rossi JJ, Gao H, et al: De novo sequencing
of circulating miRNAs identifies novel markers predicting clinical
outcome of locally advanced breast cancer. J Transl Med. 10:422012.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Ye XM, Zhu HY, Bai WD, Wang T, Wang L,
Chen Y, Yang AG and Jia LT: Epigenetic silencing of miR-375 induces
trastuzumab resistance in HER2-positive breast cancer by targeting
IGF1R. BMC Cancer. 14:1342014. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Hong S, Noh H, Teng Y, Shao J, Rehmani H,
Ding HF, Dong Z, Su SB, Shi H, Kim J and Huang S: SHOX2 is a direct
miR-375 target and a novel epithelial-to-mesenchymal transition
inducer in breast cancer cells. Neoplasia. 16:279–290.e1-5. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Georgala PA, Carr CB and Price DJ: The
role of Pax6 in forebrain development. Dev Neurobiol. 71:690–709.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Hanson IM: PAX6 and congenital eye
malformations. Pediatr Res. 54:791–796. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Zong X, Yang H, Yu Y, Zou D, Ling Z, He X
and Meng X: Possible role of Pax-6 in promoting breast cancer cell
proliferation and tumorigenesis. BMB Rep. 44:595–600. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Huang BS, Luo QZ, Han Y, Li XB, Cao LJ and
Wu LX: microRNA-223 promotes the growth and invasion of
glioblastoma cells by targeting tumor suppressor PAX6. Oncol Rep.
30:2263–2269. 2013.PubMed/NCBI
|
|
36
|
Mayes DA, Hu Y, Teng Y, Siegel E, Wu X,
Panda K, Tan F, Yung WK and Zhou YH: PAX6 suppresses the
invasiveness of glioblastoma cells and the expression of the matrix
metalloproteinase-2 gene. Cancer Res. 66:9809–9817. 2006.
View Article : Google Scholar : PubMed/NCBI
|