Introduction
Chinese children have a very high incidence of
gluteal muscle contracture (GMC) due to the extensive use of
intramuscular injections over the last century (1,2). Since
an association was found between the intramuscular injection of
benzyl alcohol and GMC (3),
aetiological prevention has led to a significant reduction in new
cases of GMC (2,4,5).
However, there are still numerous patients with untreated GMC who
have not received an early diagnosis or treatment due to a lack of
awareness of the disease.
Currently, adult patients with untreated GMC have a
relatively less severe form of GMC. According to the GMC
classification criteria of Zhao et al (1,6), most of
them were ranked as grade II GMC. Most patients first experience
the inconvenience of GMC in work and life during adulthood. Since
these patients are generally well educated, they often use the
internet and other channels to acquire GMC-related information.
This patient population has a strong desire for treatment with
clear goals. They expect to achieve a good treatment effect without
an effect on their appearance.
Conservative treatment (e.g., manual massage and
functional exercises involving crouching with the knees close
together) can be used to treat grade I GMC, while open surgery is
required for grade III GMC. At present, two surgical options are
available for adult patients with grade II GMC including open GMC
release and arthroscopic GMC release. These two surgical options
have different characteristics. Open surgery is considered to be
reliable and effective but it may cause large trauma and high
incidences of postoperative complications. Arthroscopic surgery has
a limited effect on appearance and results in a small incision,
reduced trauma and fewer complications. However, it has a
relatively lower rate of release and has the possibilities of
insufficient release. To our knowledge, there has been no previous
report comparing the two surgical options for adult patients with
grade II GMC. Therefore, the aim of this study was to compare the
clinical effects of arthroscopic surgery with open surgery for
grade II GMC in adults and discuss the indication and technique for
arthroscopic GMC release.
Patients and methods
Patients
The study was approved by the ethics committee of
The Second Affiliated Hospital of Xi'an Jiaotong University (Xi'an,
China) and conducted in accordance with the Declaration of
Helsinki. Signed consent was obtained from each patient. From 2011
to 2016, 113 adult patients with grade II GMC who underwent surgery
at our department were included in this study. GMC is diagnosed
primarily by history and some important physical examinations
(6). Patients with hip pain,
radiographic evidence of hip dislocation or hip dysplasia by X-ray
examinatio, history of hip infection, clinical manifestations of
neurological damage, grades I and III GMC were excluded. Patients
with gluteal soft tissue tumours and gluteal compartment syndrome
were also excluded. The clinical symptoms of GMC include history of
repeated intramuscular injections into the buttocks, abduction and
external rotation with limited flexion and adduction of affected
hip, unable to bring knees together during squatting, sits in
frog-leg position, out-toeing gait/cannot walk in straight line,
snapping sound while squatting, unable to cross or overlap legs,
knee crepitus, and anterior knee pain (6). The signs of GMC include Ober's sign
positive, active flexion test positive, reverse Ober's sign
positive, palpable snapping sound while squatting, pelvic tilt
toward severe side, compensatory scoliosis, apparent leg length
discrepancy (affected leg looks longer), flattened or cone-shaped
buttock, and dimpling of skin in the buttock area (6). The severity of GMC was according to a
previous classification method of Zhao et al (6). Based on the GMC classification criteria
of Zhao et al (6), all the
patients were ranked as grade II, with no grade III or I cases by
two trained and experienced authors. Among these patients,
seventy-two patients were treated with open GMC release (open
surgery group) and forty-one patients were treated with
arthroscopic surgery (arthroscopic surgery group). All the surgical
procedures were completed by the same surgeon (Siyue Xu). Among
these patients, there were 34 men and 38 women with a mean age of
22.39±3.80 years in the open surgery group and 23 men and 18 women
with a mean age of 23.05±4.67 years. In both groups, patients had
bilateral contracture. The two groups of patients did not differ
significantly regarding age and gender, age at disease onset and
mean postoperative followup time (all P>0.05; Table I).
 | Table I.Baseline characteristics of each
group. |
Table I.
Baseline characteristics of each
group.
| Characteristic | Open surgery
(n=72) | Arthroscopic surgery
(n=41) | P-value |
|---|
| Age, years | 22.39±3.80 | 23.05±4.67 | 0.42 |
| Sex, n |
|
| 0.36 |
| Male | 34 | 23 |
|
|
Female | 38 | 18 |
|
| Mean follow-up time,
years | 2.23±0.31 | 2.10±0.23 | 0.09 |
| Age at disease onset,
years | 6.25±1.11 | 6.43±1.52 | 0.58 |
Patient interviews showed that 96 (85%) had received
repeated intramuscular injections of penicillin using benzyl
alcohol as a solvent before the age of 6 years, while 17 (15%) were
uncertain about their history. Five cases had undergone
conservative treatment such as manual massage and functional
exercise by crouch with both knees close to each other. All the
patients had dysfunctions when crouching and sitting cross-legged
and 97 experienced hip snapping.
Surgical procedures
Open surgery: The patient was placed in the lateral
decubitus position. A surgical incision, generally 4–6 cm long, was
made in the lower middle 1/3 of a line between the trochanter major
and the posterosuperior iliac spine (Fig. 1) (1,7). The
thinned superficial fascia was cut open to expose tough white
contractile bands consistent with the direction of the muscle
fibres. The contractile bands were cut into two parts: The tensor
fasciae latae anterior-exterior to the incision and the gluteus
maximus and medius posterior-inferior to the incision. In cases of
grade II GMC, the tough white fibrotic cords are relatively limited
and generally do not exceed the gluteus maximus and medius. A blade
or electrotome was placed perpendicular to the direction of the
gluteal muscle fibres, and the function of the adductors was
significantly improved immediately after the white tough fibrous
cords and thickened fascia latae were cut. During the surgery, the
contractile bands were cut and allowed to retract freely without
removal. Ober's test was conducted during surgery, with extension
and flexion of the knee and hip joints. After satisfactory hip
adduction at different extension and flexion angles was confirmed,
haemostasis was carefully conducted, and the wound was closed.
Arthroscopic surgery: The patient was placed in the
lateral decubitus position. The outline of the trochanter major was
marked before surgery. Bilateral disinfection, draping and surgery
were performed. During surgery, 3,000 ml of normal saline
supplemented with 1 ml of 0.1% epinephrine was used for continued
gravity perfusion and irrigation, which facilitated intraoperative
haemostasis and maintained a clear surgical field.
Surgical portals were established at the lower
middle 1/3 of the line between the trochanter major and the
posterosuperior iliac spine (Portal A) and the tip of the
trochanter major (Portal B). The position of Portal B was adjusted
based on the position of the contractile bands determined before
surgery and the expected release area. For instance, if the
contractile bands were relatively posterior, then Portal B could be
adjusted posteriorly along the horizontal line of the trochanter
major. Portal A was the viewing portal, and Portal B was the
working portal (Fig. 2). The
subcutaneous tissue was bluntly dissected, and any subcutaneous
adipose tissue that blocked the surgical view was properly resected
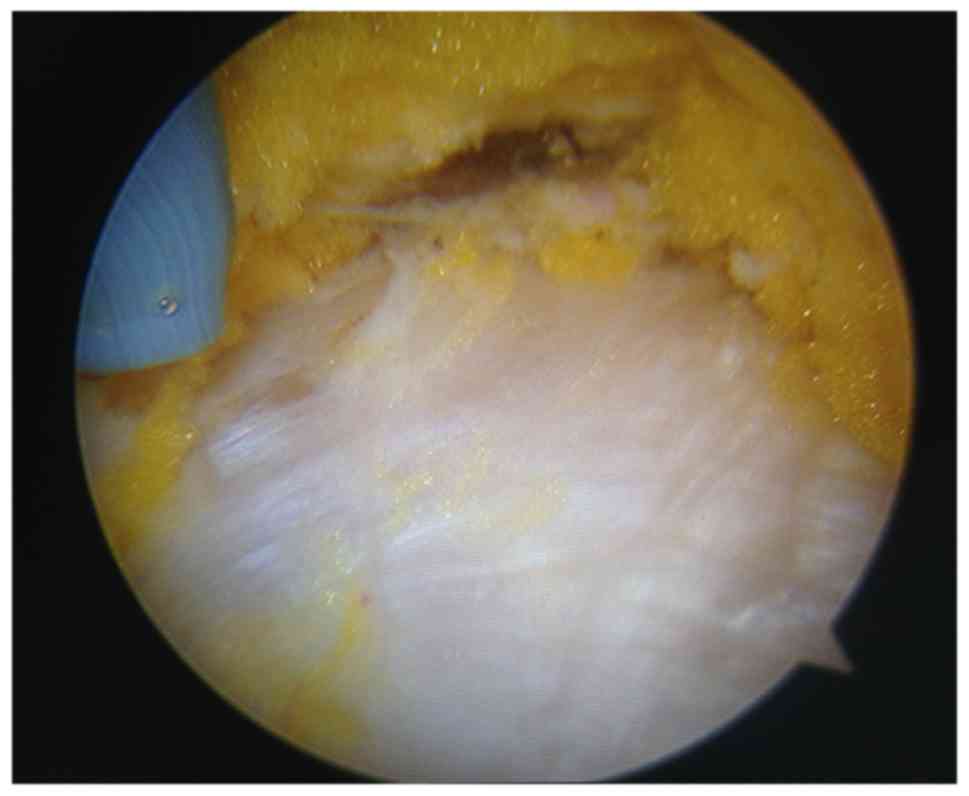
by arthroscopy shaver. The contractile bands were identified using
arthroscopy. The contractile bands usually resembling scar tissue
in texture with a white colour were markedly different from normal
muscle tissue (Fig. 3). A
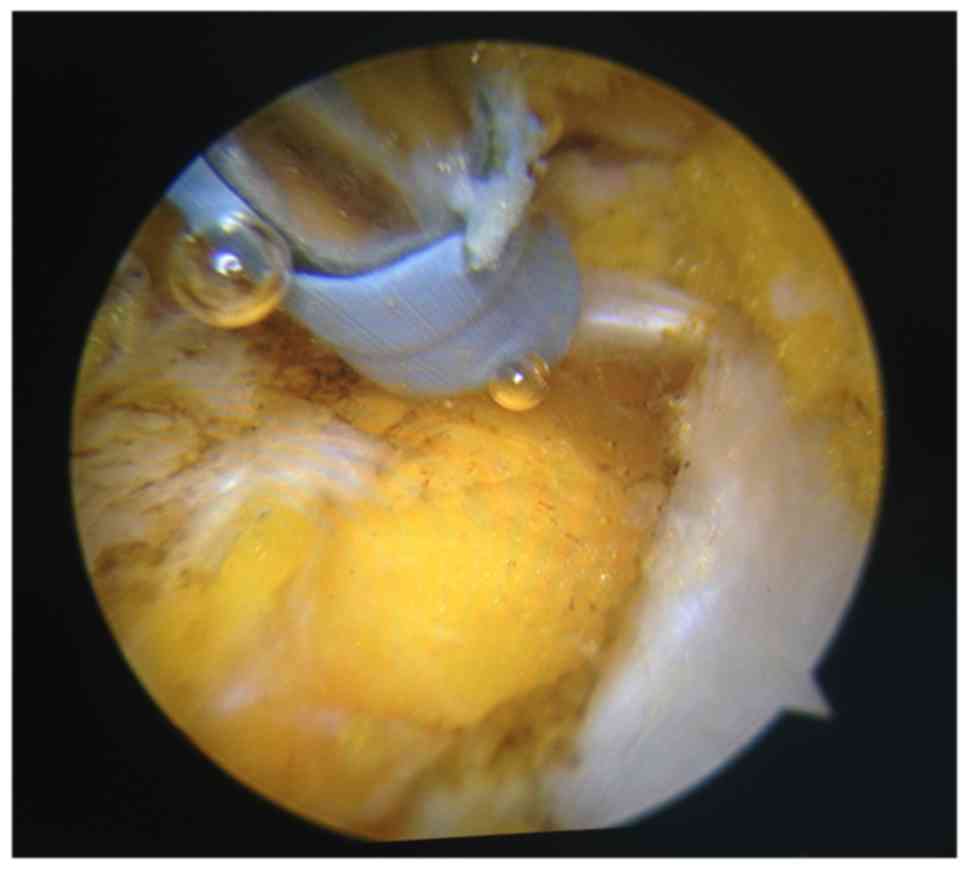
radiofrequency device was used to cut the contractile bands around
the trochanter major without cutting the muscle tissue, and
haemostasis was conducted during release (Figs. 4 and 5). Ober's test was conducted, and the
sliding of contractile bands was monitored with arthroscopy to
determine the extent of release and the position of the residual
contractile bands. If passive adduction was limited in the flexed
position, it was generally necessary to release the contractile
bands posterior to the trochanter major. If adduction was limited
near the fully extended position, it was generally necessary to
release the contractile bands anterior to the trochanter major. The
extent and depth of the release were adjusted based on Ober's test
and endoscopic observations. The release was performed until there
was no snapping in passive flexion, adduction and internal rotation
of the hip and these motions were no longer limited. The typical
release procedure for grade II GMC was as follows: First, the
contractile bands were released around the trochanter major for the
tensor fascia latae and gluteus maximus anterior to the trochanter
major; then, the contractile bands were released for the gluteus
maximus and medius posterior to the trochanter major. The position
of the sciatic nerve was kept in mind, and efforts were made to
ensure that the release was not too posterior or deep. If the
contractile bands were relatively posterior, making surgery
difficult, the hip could be flexed to slide the contractile bands
anteriorly. Before wound closure, as much subcutaneous fluid as
possible was drained through a drainage tube.
Postoperative treatments
Open surgery group: Negative pressure drainage was
routinely performed, and the drainage tube was removed when the
24-h unilateral drainage volume was less than 20 ml. Pressure
dressings were applied over the wound for 3 days after surgery. The
patients generally began functional exercises such as crouching
with the knees close together and walking in a straight line on day
3 after surgery. Functional exercises were generally performed 3–5
times a day for 20–30 cycles each time based on the patient's
tolerance.
Arthroscopic surgery group: Negative pressure
drainage was routinely performed, generally for no more than 48 h.
After placement of the drainage tube postoperatively, we squeezed
the surroundings of the wound and changed the direction of drainage
tube to discharge the arthroscopic fluid via the drainage tube as
much as possible. The drainage tube was removed when the 24-h
unilateral drainage volume was less than 20 ml. No pressure
dressings were applied over the wound after surgery. The patients
began functional exercises such as crouching with the knees close
together and walking in a straight line as soon as the drainage
tube was removed. The functional exercises were generally performed
3–5 times a day for 20–30 cycles each time based on the patient's
tolerance.
If any patient in either group experienced
intolerable pain after surgery, oxycodone and acetaminophen was
orally administered. Each tablet contained 5 mg of oxycodone
hydrochloride and 325 mg of acetaminophen.
Outcome measurements
GMC has special characteristics and methods of
outcome evaluations although it can also be considered as one kind
of the hip joint disease. The function evaluation indicators of GMC
include crouch with knees close together, cross-legged sitting
functions, gait, pain, and discomfort, etc. Thus single hip range
of motion will not fully reflect function improvement of GMC. The
criteria applied to evaluate the GMC function and effect during the
follow-up period in this study were according to previous
literatures (8,9). The validity of the results was
described in terms of four grades: Excellent (100–85 points), good
(84–70 points), fair (69–60 points) and poor (<60 points). The
evaluation indicators were as follows: A full score of 10 points
was recorded for normal crouching with both knees close together,
significantly improved walking gait, no hip snapping, no hip pain
or discomfort, normal blood vessel and nerve functions, and normal
hip adduction activities; a full score of 8 points was recorded for
normal hip flexion and cross-legged sitting functions, negative
Ober's sign, normal crossed-leg test, no haematoma and effusion,
and wound healing after first treatment.
Statistical analysis
Statistical analysis was performed with SPSS
software (version 20.0; SPSS, Inc., Chicago, IL, USA). Enumeration
data were analysed by χ2 tests, Measurement data were
tested for normality with the Kolmogorov-Smirnov test and the
statistical analysis was performed with the two-tailed Student's
t-test. P<0.05 was considered to indicate a statistically
significant difference.
Results
The mean follow-up time was 2.23 years (range, 1–5
years) for the open surgery group and 2.10 years (range, 1–5 years)
for the arthroscopic surgery group. There was no significant
difference in the follow-up time between the two groups. The
surgical duration (bilateral) was 30 to 70 min (mean: 42.89 min) in
the open surgery group and 50 to 80 min in the arthroscopic surgery
group (mean: 62.68 min). The sizes of incisions (bilateral) were 8
to 13 cm (mean: 10.23 cm) in the open surgery group, and 3 to 4 cm
(mean: 3.07 cm) in the arthroscopic surgery group. The mean blood
loss (bilateral) was 214.51 ml for the open surgery group and 76.83
ml for the arthroscopic surgery group. The hospital stay was 5 to
17 days (mean: 9.30 days) for the open surgery group and 5 to 8
days (mean: 6.12 days) for the arthroscopic surgery group. The mean
postoperative analgesic dose (based on oxycodone) was 6.83 mg for
the open surgery group and 3.29 mg for the arthroscopic surgery
group. The two groups showed significant differences in terms of
surgical duration, incision size, blood loss (intraoperative plus
postoperative), hospital stay and postoperative analgesic dose
(P<0.05; Table II).
 | Table II.Comparison of surgical duration,
incision size, blood loss, hospital stay and analgesic dose. |
Table II.
Comparison of surgical duration,
incision size, blood loss, hospital stay and analgesic dose.
| Surgery group | Surgical duration
(min) | Incision size
(cm) | Blood loss (ml) | Hospital stay
(days) | Analgesic dose
(mg) |
|---|
| Open surgery
(n=72) | 42.89±9.17 | 10.23±1.45 | 214.51±34.43 | 9.30±1.98 | 6.83±4.80 |
| Arthroscopic surgery
(n=41) | 62.68±8.88 | 3.07±0.26 | 76.83±21.53 | 6.12±0.81 | 3.29±3.08 |
| P-value | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 |
The open surgery group had 60 patients rated
excellent, 6 patients rated good, 5 patients rated acceptable and 1
patient rated poor. The arthroscopic surgery group had 33 patients
rated excellent, 5 patients rated good, 3 patients rated acceptable
and no patient rated poor. Excellent and good rates accounted for
91.67% in the open surgery group, and 92.68% in the arthroscopic
surgery group, respectively. There was no significant difference in
the ranking of functions and effects between the two groups
(χ2=0.037, P=0.848; Table
III).
 | Table III.Functional outcomes in each group. |
Table III.
Functional outcomes in each group.
|
| Functional outcome
(%) |
|---|
|
|
|
|---|
| Surgery group | Excellent | Good | Fair | Poor | P-value |
|---|
| Open surgery
(n=72) | 60 (83.34) | 6 (8.33) | 5 (6.94) | 1 (1.40) | 0.848 |
| Arthroscopic surgery
(n=41) | 33 (80.48) | 5 (12.20) | 3 (7.32) | 0 (0.00) |
|
In the open surgery group, 6 cases experienced wound
haematoma, while 4 cases showed delayed wound healing and wound
rupture. No patients in this group had residual hip snapping or
vessel and nerve injuries after surgery. One patient in this group
presented a ‘swaying gait’ after surgery that improved after 3
months of functional exercise. In the arthroscopic surgery group,
we found no wound haematoma, delayed wound healing and rupture,
wound infection, hip muscle weakness, ‘swaying’ gait, postoperative
residual snapping of the hip, or vascular and nerve injuries.
Discussion
GMC often occurs in patients who received
intramuscular injections as infants and pre-schoolers (3). Epidemiological investigations in China
show that the incidence of GMC ranges from 0.7 to 10.1% (1,2,4,5). The
pathogenesis of GMC is not completely understood. Numerous studies
have suggested that repeated intramuscular injections are the
primary pathogenic factor for GMC and that chemical stimulation via
drug injection plays a greater role than simple mechanical
stimulation (1,3,10–12). Patients with GMC walk with a toe-out
gait, present impairments when crouching with the knees close
together, and have limitations in the abduction and internal
rotation of the hip. The surgical treatment of GMC aims to improve
lower limb function and gait and to improve patients' social
function and appearance (13).
Surgical treatments for GMC include open surgery and
arthroscopic surgery. These two types of surgeries have specific
advantages and disadvantages and different scopes of application.
The advantages of open GMC release are as follows (14–21): it
supports clear exposure; it allows for complete release that
includes the joint capsule and the biceps femoris tendon in cases
of severe GMC [grade III, according to the classification criteria
of He et al (1)], and it
exposes and protects the sciatic nerve. The disadvantages are that
it results in substantial surgical trauma; it is difficult to
achieve complete haemostasis after the scar tissue is cut off,
which results in considerable postoperative wound drainage and
encourages deep wound haematomas and haematoma-induced delayed
wound healing and wound infection; and it requires a relatively
long incision, which affects the patients' appearance and may
particularly affect young women. The advantages of arthroscopic GMC
release are that allows the surgeon to clearly identify scar tissue
under the arthroscope and accurately release the contractile bands
scattered between muscle bundles without cutting off normal muscle;
it allows for simultaneous haemostasis, including that of minor
bleeding points during release, which significantly reduces
postoperative wound drainage and the probability of wound
haematoma; and it requires a small incision, which meets the
patients' aesthetic requirements, particularly those of young
women. The disadvantages are that the procedure for severe GMC is
difficult; it is difficult to effectively expose the gluteus
minimus, piriformis, joint capsule and sciatic nerve; for
contractures deeper than the gluteus medius, it is difficult
to achieve extensive and thorough release while ensuring the safety
of the sciatic nerve; for GMC cases with the same degree of
contracture, the duration of arthroscopic surgery performed by
beginners is longer than that of open surgery; and it has a
relatively low efficiency for release and is unsuitable for the
release of GMCs in large areas (22,23).
Generally, open surgery is suitable for releasing
various degrees and types of GMC, and it is particularly suitable
for severe (e.g., grade III) GMC (1,7,14,19,24).
Arthroscopic surgery is suitable for mild GMC (e.g., grade II) with
a relatively limited area. At present, most GMC patients seeking
treatment in China are adults with relatively mild contractures.
The technical characteristics of arthroscopic GMC release indicate
that this surgical approach is more suitable than open surgery for
such patients.
In this study, the arthroscopic surgery group had a
slightly longer surgical duration than the open surgery group. This
is because the efficiency of release with the radiofrequency device
under arthroscopy is lower than the efficiency of an electrotome or
blade during open surgery. Despite its lower release efficiency,
arthroscopic surgery achieves more accurate release and more
careful haemostasis. The incision length in the arthroscopic
surgery group was markedly shorter than that of the open surgery
group. Moreover, it has been reported that skin scarring caused by
surgical incision is prominent in patients with GMC and seriously
affects their appearance. He et al reported that of 187
patients who underwent open surgery, 62 developed a severely
bulging scar that was raised as high as 0.8 cm above the
surrounding skin (1). In GMC cases,
the scar tissue bleeds more than normal muscle tissue;
additionally, the broken end of the scar tissue retracts after
release, which increases the difficulty of obtaining haemostasis
during open surgery. In contrast, arthroscopic surgery can clearly
identify the bleeding points and quickly stop the bleeding,
resulting in markedly less postoperative drainage in the
arthroscopic surgery group than in the open surgery group. The
analgesic dose can indirectly reflect a patient's degree of
surgical trauma. In this study, the analgesic dose was
significantly lower in the arthroscopic surgery group compared with
the open surgery group, which also indirectly indicates that the
arthroscopic surgery was less invasive. There was a significant
difference in the duration of hospital stay between the
arthroscopic and open surgery groups, mainly because the patients
in arthroscopic surgery group began functional exercises earlier
and required less time for wound observation and functional
exercise guidance.
The comparison of postoperative functions and
effects revealed no significant differences between the
arthroscopic and open surgery groups, indicating that the two
surgeries achieved equivalent release effects. However, 6 cases in
the open surgery group developed wound haematoma. Of these, 2 cases
improved after conservative treatment (puncture and drainage), and
4 cases showed delayed wound healing and wound rupture and healed
after debridement. Among the 4 cases of wound rupture, 1 case
developed infection. Bacterial culture result revealed the presence
of Escherichia coli and the case was cured after treatment with
appropriate antibiotics. In the arthroscopic surgery group,
rigorous haemostasis resulted in no wound haematoma, delayed wound
healing, wound rupture, or wound infection.
The follow-up results reported above show that
arthroscopic GMC release resulted in less trauma, less invasion and
fewer surgical complications while achieving a release effect
consistent with that of open surgery.
Because at present, untreated GMC patients are
primarily adults, the GMC patients who were followed in this study
were all adults. Based on previous clinical experience in our
department, juveniles might have better flexibility, and
postoperative functional recovery in GMC is generally faster and
better for juveniles than for adults. Zhao et al found that
age was an important factor that influenced the results of both
non-surgical and surgical management. Patients in the juvenile
group had better results than the adolescent group for both
treatments (6). A simple follow-up
study of adults could exclude the effect of age-related physical
factors on functional recovery and be more conducive to assessing
the effect differences in treatment methods (24).
The study has several limitations. Firstly, the
retrospective non-randomized design has all of the inherent
limitations of such study. Secondly, the decision in treatment
modality is made at the discretion of the chief operating surgeon
which may produce potential bias. Thirdly, the findings showed in
this study are from a single-center hospital, which may reflect
regional and institutional bias.
In conclusion, existing untreated patients with GMC
mostly have low-severity (e.g., grade II) contractures of limited
area are more suitable for arthroscopic GMC release due to its
advantages of limited surgical trauma, a small incision, lower
blood loss and fewer surgical complications. Preoperative accurate
assessment of the depth, range, and distribution of scars of GMC by
a combined clinical and radiographic examination is the future
direction because it can accurately guide the release of GMC during
surgery and reduce unnecessary injuries.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
TZ and XH conceived the study. TZ performed the
literature search and wrote the manuscript. SX analyzed and
interpreted the data. HL and FZ collected and assembled the data.
All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the ethics committee of
the Second Affiliated Hospital of Xi'an Jiaotong University and
conducted in accordance with the Declaration of Helsinki. Written
informed consent was obtained from each patient prior to the
surgical procedures.
Consent for publication
The subjects gave written informed consent for the
publication of their data and accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
He X, Li H and Wang D: Classification and
management of the gluteal muscles contracture. Chinese J Orthop.
23:96–99. 2003.
|
|
2
|
Wang B, He X, Wu Y, Fang D and Liu J: The
prospective study and factors analysis for gluteus contracture.
China J Orthop Traumatol. 3:157–158. 2003.(In Chinese).
|
|
3
|
de Valderrama Fernandez JA and de Miguel
Esteve R: Fibrosis of the gluteus maximus: A cause of limited
flexion and adduction of the hip in children. Clin Orthop Relat
Res. 67–78. 1981.
|
|
4
|
Wang Y, Shi J, Chen W and Gao Y: The
epidemiological investigation of gluteal muscle contracture of male
students in the physical examination for navy pilot recruitment.
Chin J Aerospace Med. 26:203–207. 2015.
|
|
5
|
Hu X, Tan X, Zheng M, Kuang R, Liang J,
Wei W, Wang H, Zeng B and Wang G: Epidemiological survey of gluteal
muscle contracture of primary and secondary students in Rongchang
county. Chongq Med. 44:368–371. 2015.(In Chinese).
|
|
6
|
Zhao CG, He XJ, Lu B, Li HP, Wang D and
Zhu ZZ: Classification of gluteal muscle contracture in children
and outcome of different treatments. BMC Musculoskelet Disord.
10:342009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wang D, Liu Z, He X, Li H and Xu S:
Operative treatment of the serious gluteus contracture. Orthoped J
China. 17:1189–1190. 2009.(In Chinese).
|
|
8
|
Liu YJ, Xue J, Zhou M, Wang ZG, Li ZL, Cai
X, Wei M, Wang Y and Zhu JL: Arthroscope monitored solution of
adult intramuscular injection associated gluteal muscle contracture
by radiofrequency. Zhonghua Wai Ke Za Zhi. 46:970–972.
2008.PubMed/NCBI
|
|
9
|
Fu D, Yang S, Xiao B, Wang H and Meng C:
Comparison of endoscopic surgery and open surgery for gluteal
muscle contracture. J Pediatr Orthop. 31:e38–e43. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zhao CG, He XJ, Lu B, Li HP and Kang AJ:
Increased expression of collagens, transforming growth
factor-beta1, and -beta3 in gluteal muscle contracture. BMC
Musculoskelet Disord. 11:152010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zhao CG, Qin J, He XJ, Guan YC, Jia Y and
Lei W: Sphingosine-1-phosphate is a possible fibrogenic factor in
gluteal muscle fibrosis. Physiol Res. 62:691–699. 2013.PubMed/NCBI
|
|
12
|
Zhang X, Ma Y, You T, Tian X, Zhang H, Zhu
Q and Zhang W: Roles of TGF-β/Smad signaling pathway in
pathogenesis and development of gluteal muscle contracture. Connect
Tissue Res. 56:9–17. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Rai S, Meng C, Wang X, Chaudhary N, Jin S,
Yang S and Wang H: Gluteal muscle contracture: Diagnosis and
management options. SICOT J. 3:12017. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Liu G, Yang S, Du J, Zheng Q, Shao Z and
Yang C: Treatment of severe gluteal muscle contracture in children.
J Huazhong Univ Sci Technolog Med Sci. 28:171–173. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Al Bayati MA and Kraidy BK: Gluteal muscle
fibrosis with abduction contracture of the hip. Int Orthop.
40:447–451. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Xu J, Geng X, Muhammad H, Wang X, Huang
JZ, Zhang C and Ma X: Comparison of the incisions for the open
surgical treatment of gluteal muscle contracture. J Pediatr Orthop
B. 23:435–440. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ye B, Zhou P, Xia Y, Chen Y, Yu J and Xu
S: New minimally invasive option for the treatment of gluteal
muscle contracture. Orthopedics. 35:e1692–e1698. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Tang X, Liu L and Peng M: Diagnosis and
treatment of gluteal muscle contracture associated with unequal leg
length caused by pelvis obliquity. Zhongguo Xiu Fu Chong Jian Wai
Ke Za Zhi. 20:835–837. 2006.(In Chinese). PubMed/NCBI
|
|
19
|
Chen HS and Yang XL: Insertion of gluteus
maximus tendo-chilles lengthening with Z-shaped for the treatment
of severe gluteal muscle contracture. Zhongguo Gu Shang.
28:524–526. 2015.(In Chinese). PubMed/NCBI
|
|
20
|
Chen X, Tang X, Jiang X, Wang D, Peng M
and Liu L: Diagnosis and treatment of unilateral gluteal muscle
contracture. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 25:530–532.
2011.(In Chinese). PubMed/NCBI
|
|
21
|
Xiao Y, Tang ZH, Zhang SR, Zou GY, Xiao
RC, Liu RD and Hu JZ: The first exploration of a minimally invasive
lysis subcutaneouly for the treatment of gluteal muscle contracture
based on relatively safe region around standard injection point of
gluteal muscle. Zhongguo Gu Shang. 24:514–516. 2011.(In Chinese).
PubMed/NCBI
|
|
22
|
Liu YJ, Wang Y, Xue J, Lui PP and Chan KM:
Arthroscopic gluteal muscle contracture release with radiofrequency
energy. Clin Orthop Relat Res. 467:799–804. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Zhang X, Jiang X, He F, Liang Z, You T,
Jin D and Zhang W: Arthroscopic revision release of gluteal muscle
contracture after failed primary open surgery. Int Orthop.
41:1521–1526. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Liu GH, Cao FQ, Yang SH and Zhu JF:
Factors influencing the treatment of severe gluteal muscle
contracture in children. J Pediatr Orthop B. 20:67–69. 2011.
View Article : Google Scholar : PubMed/NCBI
|