Introduction
Gynecomastia is a common benign condition of the
male breast, most frequently observed in newborns, adolescents and
the elderly, and it may be associated with discomfort and mental
stress (1). The pathogenesis of this
condition is multifactorial and in most cases idiopathic (2). Prevalence rates are 60–90% in newborns,
50–60% in adolescents and 70% in males aged 50–69 years (1).
Disease progression has several stages. Asymptomatic
males with long-standing breast enlargement do not usually require
treatment other than therapy. In males who suffer from pain or
embarrassment, treatment is guided by the cause of gynecomastia and
patient expectations (3). It is
ideal for medicinal treatments to be applied during the
proliferation phase of gynecomastia (4). However, if gynecomastia has been
present for >1 year, it would not be expected to regress
substantially, either spontaneously or with medicinal therapy, due
to the presence of fibrosis (5).
Under these circumstances, surgical excision to remove tissue is
the only effective method.
Surgical management of gynecomastia includes four
general approaches: Excision of breast tissue, liposuction and skin
resection, alone or in combination. Liposuction may be used to
treat pseudo gynecomastia, as fat deposition is a major concern in
such cases (6). Liposuction and
excision may be considered when the breast is composed primarily of
fibrotic tissue (7). If there is
excessive skin, skin resection may also be considered (1). The periareolar incision technique is
effective, but endoscopic techniques are associated with a better
cosmetic outcome (1,5,8). The
present study reports two cases of patients with gynecomastia, who
were managed considering cosmetic outcome and efficacy using a
TriPort (Fig. 1), which combines
endoscopic surgery and liposuction.
Patients and methods
Case 1
A 51-year-old male exhibited a body mass index of
17.4. According to Simon's classification (9), the right breast had exhibited grade II
gynecomastia for 6 years and the left breast had exhibited grade I
gynecomastia for 3 years. Following treatment with antiestrogens
for 15 months, no breast reduction was observed. Liver function
tests and serum creatinine were normal. All endocrinological
findings were normal, with the exception of luteinizing hormone
levels 17.63 IU/l (Normal range: 1.7–8.6 IU/l). A brain magnetic
resonance imaging (MRI) scan was performed, revealing no abnormal
findings. On breast ultrasonography, breast tissue echoes were
identified, with a range of 4.5×0.8×1.1 cm on the right and
2.3×0.5×2.2 cm on the left breast. On physical examination, a
rubbery mound of tissue was palpated bilaterally, which was
concentric with the nipple-areolar complex. Thus, the patient was
diagnosed with gynecomastia according to Braunstein GD's diagnostic
criteria (5). The patient requested
an endoscopic resection in his right breast and open resection in
the left, with periareolar incisions and underwent surgical
treatment.
Case 2
A 48-year-old man (body mass index, 17.4) exhibited
grade II gynecomastia of the right breast, according to Simon's
classification (9) for 6 months. On
breast ultrasonography, breast tissue echoes in the right breast
were identified with a range of 3.3×2.5×0.8 cm. Liver function
tests and serum creatinine were normal. All endocrinological
findings were within the normal range, with the exception of
prolactin level, which was increased by 2-fold compared with the
normal value (632.90 IU/l). A brain MRI was recommended, but the
patient refused. The patient underwent direct excision of the left
breast tissue 4 years previously. The patient requested
single-incision surgery for the right breast.
Surgical technique
Prior to procedure, modalities of the reconstruction
were discussed by surgeon and patient. Open and closed procedures
were explained and risks of scarring were discussed. Patients were
admitted to the Binzhou Medical University Hospital (Binzhou,
China) in April 2017 (case 1) and May 2017 (case 2). Informed
consent and ethics approval were obtained respectively from
patients and the Ethics Committee of Binzhou Medical University
(Binzhou, China).
For single-incision surgery for gynecomastia,
preoperative markings were made on the patient to ensure precise
demarcation of the operative area (Fig.
2). Under general anesthesia, the patient was placed in a
supine position, with the arms abducted to 90° and fixed. A single
skin incision was performed along the mid-axillary line in order to
hide the scar when the arms are resting at the sides. Lipolysis
solution (200 ml sterile purified water, 200 ml physiological
saline, 30 ml 5% NaHCO3, 20 ml 2% lidocaine and 1 ml 0.1%
adrenaline; total solution volume of 451 ml) (10,11) was
injected into the subcutaneous and retromammary spaces, and
liposuction was performed after 15 min. The volume of liposuction
was 204 ml and 182 ml (case 2), as determined by the volume of the
aspirator cylinder subtracted by 451 ml lipolysis solution. When
liposuction was completed, only the Cooper ligaments remained
between breast gland and skin. The sleeve pedestal was inserted in
the incision by separating the surrounding subcutaneous tissue. The
pedestal was then connected with the TriPort (HTKD Medical; Beijing
HangTian KaDi Technology R&D Institute, Beijing, China; product
model, HK-FDDC-4FX). To establish the working space, CO2
was insufflated and inflation pressure was maintained at 8 mmHg.
The suture line was used to secure nipple and areola. The
endoscope, ultrasound knife, assistant clamp and other equipment
were fixed on the TriPort (Fig. 3).
The four quadrants of the breast, retromammary cellular space,
Cooper's ligament and nipple-areolar tissues were separated
successively. The excision process was controlled under endoscopic
visualization with an ultrasound knife or electrocautery, enabling
adequate tissue removal, bleeding control and preservation of the
pectoral fascia.
In the left breast of case 1, a direct excision was
made through radial incision. Along with the superficial fascia,
the fat and mammary gland tissue layers were separated.
Furthermore, some gland tissue was left behind the nipple and
areola to support the complex. The incision was closed following
successful removal of all gland tissue. No equivalent procedure was
performed in case 2.
The total operative time was 60 min in case 1 and 57
min in case 2 (mean, ~58 min). A drain and gauze compressing the
breast surface were used to prevent postoperative bleeding. To
achieve a more satisfying cosmetic result, intradermal absorbable
sutures were used to close the incision (Fig. 4).
Results
Patients were discharged on the third (case 1) and
second (case 2) postoperative day, following postoperative
pathology to confirm gynecomastia diagnosis. All patients were
satisfied with the cosmetic result and short hospitalization time.
Less postoperative bleeding (~110 ml for case 1 and 100 ml for case
2 during hospitalization) was observed compared with the direct
excision method, as excision combined with endoscopic visualization
using an ultrasound knife and electrocautery achieved hemostasis.
Drain and gauze were removed, 5 days following surgery and there
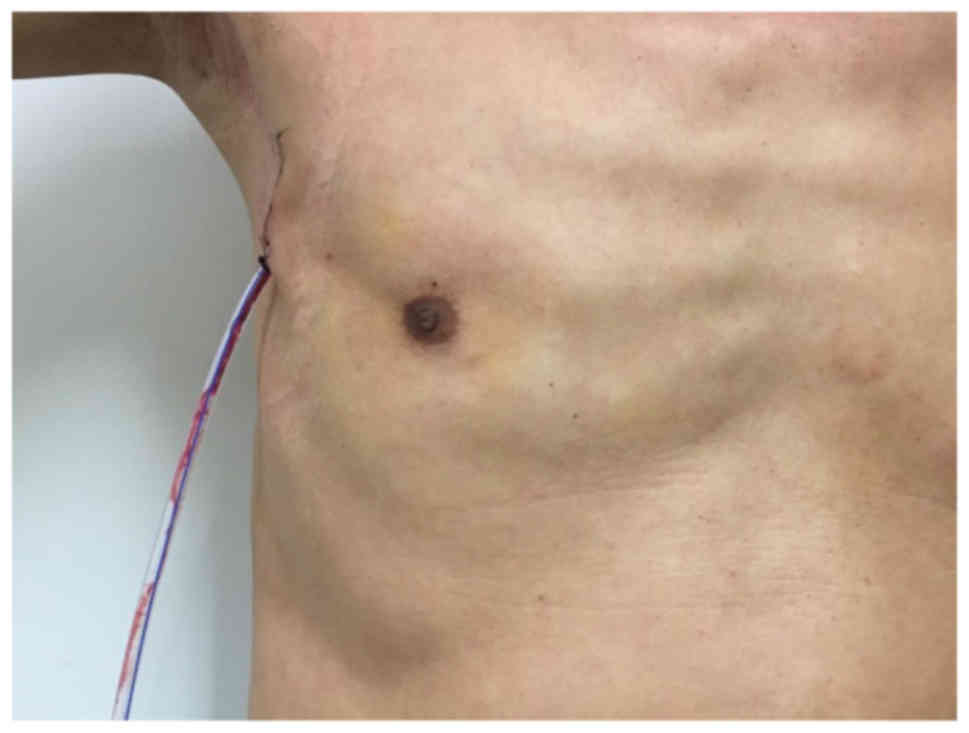
were no postoperative complications. Single incisions were
completely covered by the arms, while the left periareolar incision
in case 1 was more obvious (Fig. 5).
There were no recurrences or complications during 5 months of
follow-up.
Discussion
Gynecomastia is a common cause of discomfort and
embarrassment for men. Surgical excision remains one of the most
effective methods for gynecomastia management, particularly in
patients with fibrosis or with a disease course of >1 year
(7). Previously, minimally invasive
techniques, including power-assisted and ultrasound-assisted
liposuction, have been a popular approach due to their satisfactory
cosmetic outcome (12–15). However, interest is now focused on
minimally invasive surgery to minimize external scars (14). Our ultimate goals are minimal
incision, better cosmetic outcome, efficacy and
reproducibility.
Jarrar et al (13) used a single 15-mm incision during
surgery of gynecomastia. The authors were experienced in endoscopy
and were able to achieve a good cosmetic outcome. However, a longer
time was required for resecting and extracting tissues and if
extracted tissues were larger or of a tougher consistency, the use
of scissors or graspers and diathermy may not have been the optimal
approach. The size of the incision allowed for the use of an
endoscope during surgery. The amplification provided by an
endoscope clearly visualized the operating field on the monitor
screen, allowing for improved view compared with previous single
incision procedures. In addition, the amplification of an endoscope
allows the surgeon to identify and cauterize minor bleeds, thereby
reducing postoperative bleeding and shortening hospitalization
time. Increased surgery length may lead to hypothermia and increase
the neurotoxicity of the narcotic agent (16). Balance between incision length and
final cosmetic outcome is important during gynecomastia surgery.
Zhu and Huang (6) reported the use
of three incisions to introduce an endoscope. The whole excision
process was performed under endoscopic visualization, enabling
adequate removal, good bleeding control and preservation of the
pectoral fascia. However, the final incision was enlarged to
extract excised tissue, which prolonged the procedure. The final
incision was longer compared with the single incision performed in
the current study, and tissue injury was more extensive.
Recently, Chang and Lee (14) reported an increasing interest in
minimally invasive surgery with an emphasis on minimizing scars.
The authors demonstrated that liposuction was associated with
minimizing incisional scars, but the procedure was less effective
in removing glandular tissue. Therefore, direct excision of
glandular tissues remained irreplaceable. The present study
hypothesized that patients may prefer surgery that enables control
under endoscopic visualization in combination with a smaller, but
adequate, incision.
In the current study a TriPort was applied during
surgery, which has previously been used in laparoscopic surgery
(17,18). The TriPort enables completion of
gynecomastia surgery through a single incision, combining endoscopy
and liposuction. This TriPort-based method enabled good control of
endoscopic and operating instruments, separation of different
tissues and hemostasis throughout surgery, and it may shorten
operative time. It was previously reported that the mean operative
time was 82 min (range, 65–100 min) compared with 58 min observed
in the current study (10). Due to
different trocars on the TriPort, there is no interference with
different tractors, due to the stability provided by TriPort, under
endoscopic view, achieving a result of better control of these
tractors comparable with that of three-incisional surgery. The
excision process was controlled by endoscopic visualization,
enabling adequate tissue removal, good bleeding control and
preservation of the pectoral fascia. Benefits, including a positive
postoperative recovery, less postoperative bleeding, a decreased
incidence of complications and shortening of hospitalization
period, were not reported in previous single-incision procedures
(13,19). Furthermore, the inner diameter of the
TriPort was sufficient to extract excised tissue integrally,
decreasing the operative time and avoiding residual tissue left
following the procedure. Various types of TriPort are available
with inner diameters ranging from 50 to 120 mm, which have the
potential to remove varying amounts of breast tissue. The tractors
on the TriPort provide the option of using other equipment if
necessary, achieving a larger surgical space compared with
conventional minimally invasive methods. The height of the TriPort
is adjustable, ranging from 40 to 200 mm, which may be useful
during surgery of obese patients. In addition, extraction of
excised tissue en bloc shortens the duration under anesthesia.
Therefore, combination of liposuction and endoscopic resection may
be an effective method for removing mammary tissue, accompanied by
a favorable cosmetic result, decreased hospitalization time
compared with direct excision methods and adequate control of
bleeding.
To the best of our knowledge, this is the first
report describing the use of TriPort, which combines endoscopic
surgery and liposuction, in the management of gynecomastia.
Single-incision endoscopic surgery through the TriPort may be an
effective and safe way for the management of gynecomastia, as it
ensures an aesthetic result and complete removal of the glandular
tissue. Further studies are required to allow a systematic
evaluation of this method.
Acknowledgements
Not applicable.
Funding
This study was supported by grants from the National
Natural Science Foundation of China (grant nos. 30973932 and
81173601), the Natural Science Foundation of Shandong Province
(grant nos. ZR2017LH072, ZR2017MH033 and ZR2014HQ020), the Projects
of Binzhou Technology Development Program (grant no. 2015ZC0301),
the Scientific Research Staring Foundation of Binzhou Medical
University (grant nos. BY2014KYQD36 and BY2014KJ36) and the Science
and Technology Program of Universities in Shandong Province (grant
no. J15LL51).
Availability of data and materials
All data generated or analysed during this study are
included in this published article.
Authors' contributions
JL, KC and YH wrote the manuscript and performed
surgery; XW and ZY designed the present study; and FG and JL were
responsible for patient follow-up and data collection. All authors
read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the was obtained
from Ethics Committee of Binzhou Medical University (Binzhou,
China; approval no. 2018-002-01). Written informed consent was
obtained from patients prior to enrolment.
Consent for publication
The patient provided written informed consent for
the publication of any associated data and accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Sansone A, Romanelli F, Sansone M, Lenzi A
and Di Luigi L: Gynecomastia and hormones. Endocrine. 55:37–44.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Rahmani S, Turton P, Shaaban A and Dall B:
Overview of gynecomastia in the modern era and the Leeds
Gynaecomastia Investigation algorithm. Breast J. 17:246–255. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Carlson HE: Approach to the patient with
gynecomastia. J Clin Endocrinol Metab. 96:15–21. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Cao H, Yang ZX, Sun YH, Wu HR and Jiang
GQ: Endoscopic subcutaneous mastectomy: A novel and effective
treatment for gynecomastia. Exp Ther Med. 5:1683–1686. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Braunstein GD: Clinical practice.
Gynecomastia. N Engl J Med. 357:1229–1237. 2007. View Article : Google Scholar
|
|
6
|
Zhu J and Huang J: Surgical management of
gynecomastia under endoscope. J Laparoendosc Adv Surg Tech A.
18:433–437. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Dickson G: Gynecomastia. Am Fam Physician.
85:716–722. 2012.PubMed/NCBI
|
|
8
|
Waltho D, Hatchell A and Thoma A:
Gynecomastia classification for surgical management: A systematic
review and novel classification system. Plast Reconstr Surg.
139:638e–648e. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Simon BE, Hoffman S and Kahn S:
Classification and surgical correction of gynecomastia. Plast
Reconstr Surg. 51:48–52. 1973. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Fan L, Yang X, Zhang Y and Jiang J:
Endoscopic subcutaneous mastectomy for the treatment of
gynecomastia: A report of 65 cases. Surg Laparosc Endosc Percutan
Tech. 19:e85–e90. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Shi F, Huang Z, Yu J, Zhang P, Deng J, Zou
L, Zhang C and Luo Y: Immediate liposuction could shorten the time
for endoscopic axillary lymphadenectomy in breast cancer patients.
World J Surg Oncol. 15:352017. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Brown RH, Chang DK, Siy R and Friedman J:
Trends in the Surgical Correction of Gynecomastia. Semin Plast
Surg. 29:122–130. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Jarrar G, Peel A, Fahmy R, Deol H, Salih V
and Mostafa A: Single incision endoscopic surgery for
gynaecomastia. J Plast Reconstr Aesthet Surg. 64:e231–e236. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Chang HP and Lee DW: Discussion: Surgical
management of gynecomastia: Subcutaneous mastectomy and
liposuction. Aesthetic Plast Surg. 41:985–986. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kisu I, Banno K, Kobayashi Y, Ono A,
Masuda K, Ueki A, Nomura H, Hirasawa A, Abe T, Kouyama K, et al:
Flexible hysteroscopy with narrow band imaging (NBI) for endoscopic
diagnosis of malignant endometrial lesions. Int J Oncol.
38:613–618. 2011.PubMed/NCBI
|
|
16
|
Jevtovic-Todorovic V, Absalom AR, Blomgren
K, Brambrink A, Crosby G, Culley DJ, Fiskum G, Giffard RG, Herold
KF, Loepke AW, et al: Anaesthetic neurotoxicity and
neuroplasticity: An expert group report and statement based on the
BJA Salzburg Seminar. Br J Anaesth. 111:143–151. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Erhart D and Pohnán R: 55 laparoscopic
cholecystectomies using single incision laparoscopic
surgery-initial experience. Rozhl Chir. 90:361–364. 2011.(In
Czech). PubMed/NCBI
|
|
18
|
Pagano D, Echeverri GJ, Gridelli B, Spada
M, Botrugno I and Bartoccelli C: Natural orifice transumbilical
cholecystectomy using a tri-port trocar and conventional
instruments. J Am Coll Surg. 210:1013–1014. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Mentz HA, Ruiz-Razura A, Newall G,
Patronella CK and Miniel LA: Correction of gynecomastia through a
single puncture incision. Aesthetic Plast Surg. 31:244–249. 2007.
View Article : Google Scholar : PubMed/NCBI
|