Introduction
Ischemia-reperfusion injury (IRI) is caused by blood
flow perfusion after organ ischemia, which can bring damages to
tissues and organs (1). IRI is a
common physiological process in clinical practices. Studies have
shown that patients with renal transplantation or renal surgery are
likely to be affected by IRI. After renal transplantation, IRI may
lead to rejection to cause renal failure, which in turn shortens
the survival of patients (2–4). Renal IRI is one of the causes of acute
kidney injury. Although great efforts were made to treat this
disease, treatment outcomes are still unsatisfactory, and the
incidence and mortality are relatively high (5). Therefore, how to reduce the morbidity
and mortality is a major task for researchers.
Berberine, also known as jamaicin, is a common type
of alkaloids (isoquinolines). The active ingredients are extracted
from the roots of the rhizome. Studies have shown that this drug
has promising therapeutic effects in the treatment of digestive
diseases and diarrhea, but its absorption through oral
administration is not satisfactory, and the duration of plasma
concentration is short (6,7). Exendin-(9–39), as an antagonist of GLP-1R, can
effectively attenuate Nesfatin-1 and delay the emptying of the
stomach and reduce the intake of berberine and effectively maintain
the retention of berberine (8). In
recent years, it has been found that berberine has
anti-inflammatory functions and more and more studies confirmed
that berberine played a certain regulatory role in inhibiting the
body's immune response and anti-apoptosis response (9). In this study, rat model of renal IRI
was established to explore the therapeutic effects of berberine in
the treatment of renal IRI with the expectation of providing
references for clinical treatment.
Materials and methods
Laboratory animals and materials
A total of 40 healthy male SD rats weighing 250–300
g were purchased from Wuhan MultiSciences (Lianke) Biotech Co.,
Ltd. (Hangzhou, China). Rabbit polyclonal Bcl-2 antibody (dilution
1/500; cat. no. ab59348) and rabbit monoclonal Bax antibody
(dilution 1/500; cat. no. ab32503) were purchased Abcam (Cambridge,
MA, USA). Malondialdehyde (MDA) kit was from Beyotime Biotechnology
(Jiangsu, China). Exendin-(9–39) kit was purchased from Bachem
(Bubendorf, Switzerland). Terminal
deoxynucleotidyltransferase-mediated dUTP nick end labeling (TUNEL)
cell apoptosis kit was purchased from Trevigen (New York, NY,
USA).
Animal grouping
Forty adult SD rats were randomly divided into four
groups: sham-operation group A, renal ischemia-reperfusion group B,
berberine treatment group C and berberine + exendin-(9–39) treatment group D, 10 rats in each
group. Rats were housed in a temperature controlled room (21 ± 2°C)
on a 12:12-h light/dark cycle (lights on at 06:00 a.m.). All rats
had free access to water and food. Rats in group A and B were
intraperitoneally injected with 2 ml saline from 7 days before
surgery. Rats in group C and D were subjected to intraperitoneal
injection of berberine (0.4 mg/kg/day) 7 days before the experiment
(berberine powder was dissolved in 2 ml of saline). Besides that,
intraperitoneal injection of exendin-(9–39) was performed in group D at day 1 and
4 at a dose of 45 µg/kg/3 days after model construction. In group
A, right kidney was resected and left renal pedicle was separated,
but left renal artery was not blocked. Renal ischemia-reperfusion
model was established in other groups.
Establishment of animal model
Rats were fasted for 12 h before animal model
establishment, but were allowed to access water freely.
Intraperitoneal injection of 10% chloral hydrate (350 mg/kg) was
performed for anesthesia. Rats were fixed and disinfected. An
incision was made on the middle of the abdomen, and lateral
peritoneum was cut to expose right kidney. Left ureter was
protected, and left renal pedicle was separated. A non-destructive
vascular clamp was used for left renal artery occlusion until
kidneys turned from red to violet-black. Then vascular clamp was
removed and the successful establishment of rat model of renal IRI
is indicated by the changes of renal color from violet-black to
red. The study was approved by the Ethics Committee of People's
Hospital of Lishui Animal Center (Zhejiang, China).
Sample collection and testing
Blood samples were collected from the orbital veins
of rats before left kidney resection. Before centrifugation at
2,500 × g for 5 min at 4°C, level of MDA in plasma was determined
according to the instructions of MDA kit, and levels of serum
creatinine (SCr) and blood urea nitrogen (BUN) were detected using
an automatic biochemical analyzer after left kidney resection was
performed, and 500 mg renal tissue was washed three times with
NaCl, and stored at −4°C. Western blot analysis was used to detect
the expression of Bax and Bcl-2 in renal tissues of rats. Tissue
apoptosis was detected by TUNEL assay.
Western blot analysis
Total protein was extracted, quantified, and mixed
with buffer. After electrophoresis, transmembrane was performed on
ice under 100 V for 2 h. Membranes were blocked with 5% skim milk
for 1 h, and incubated with primary rabbit polyclonal Bcl-2
antibody (dilution 1:500; cat. no. ab59348) and rabbit monoclonal
Bax antibody (dilution 1:500; cat. no. ab32503) overnight. After
that, membranes were further incubated with secondary goat
anti-rabbit (HRP) IgG antibody(dilution 1:2,000; cat. no. ab6721)
at room temperature for 1 h. After washing with TBST, BandScan 5.0
software (Glyko, Inc., Novato, CA, USA) was used to measure gray
value of protein bands and calculate the gray ratio.
TUNEL
TUNEL assay kit was used to detect the apoptotic
cells in kidney of each group, and the operation was carried out in
strict accordance with the instructions of the kit. Cells were
counted under optical microscopy. Five visual fields were randomly
selected under optical microscope. Apoptosis rate (AI) = total
apoptotic cells/total cell number ×100%. Determination of apoptotic
cells: nuclei of apoptotic renal cells showed yellow or
yellow-brown color, and nuclei of normal renal cells showed blue
after staining.
Statistical analysis
In this study, SPSS22.0 software package was used to
analyze all the data. Measurement data were expressed as mean ±
standard deviation (mean ± SD), and comparison were performed by
ANOVA analysis followed by Least Significant Difference post hoc
test. P<0.05 was considered to indicate a statistically
significant difference.
Results
Model construction
In this study, rat model of renal IRI was
established. During model construction, 1 rat died in group A, 2 in
group B, 1 in group C and none in group D.
Comparison the renal functions among
groups
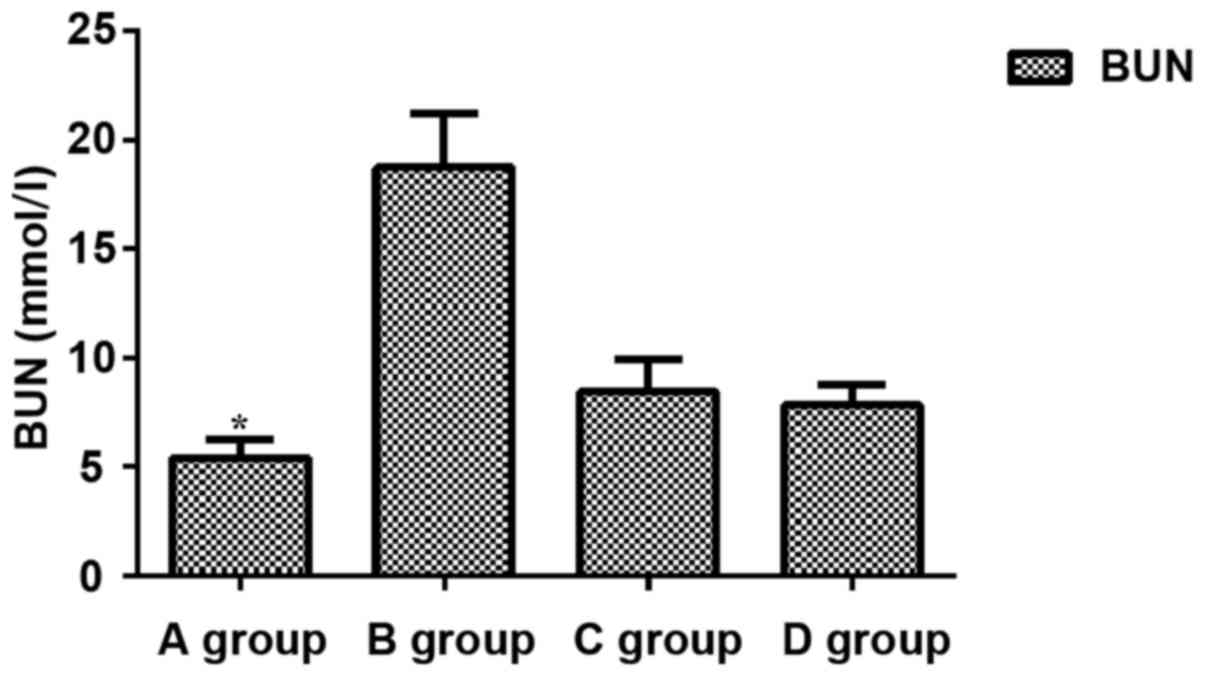
Comparisons of levels of BUN, Scr and MDA among
groups showed that levels of BUN, Scr and MDA in group B were
significantly increased compared with those in other groups
(P<0.05), while levels of BUN, Scr and MDA were significantly
lower in group A than in other groups (P<0.05). No significant
differences in levels of BUN, Scr and MDA were found between groups
C and D (P>0.05) (Figs.
1–3).
Comparison of levels of Bax and Bcl-2
among groups
Group C and D pretreated with berberine showed
significantly reduced expression level of Bax compared with that in
group B, which was not treated with berberine (P<0.05). In
contrast, expression level of Bcl-2 was significantly increased in
group C and D compared with group B (P<0.05). No significant
difference was found between C and D (P>0.05) (Fig. 4).
Comparison of renal cell
apoptosis
Apoptosis of rat renal cells was detected by TUNEL
method (the positive nucleus was brown and the negative was blue).
Apoptosis was found in a small portion of cells in group A
(3.40±1.20%). Compared with group A, cell apoptosis was
significantly increased in group B (57.41±13.65%, P<0.05).
Compared with group B, apoptosis of renal cells in group C and D
was significantly improved (17.2±4.2 and 15.1±2.7%, P<0.05).
Compared with group A, apoptosis of renal cells in group C and D
was significantly increased (17.2±4.2 and 15.1±2.7%, P<0.05). No
significant difference was found between group C and D (P>0.05)
(Table I).
 | Table I.Comparison of renal cell apoptosis
among 4 groups. |
Table I.
Comparison of renal cell apoptosis
among 4 groups.
| Groups | n | Percentage (%) |
|---|
| A | 9 | 3.40±1.20 |
| B | 8 | 57.41±13.65 |
| C | 9 | 17.2±4.2 |
| D | 10 | 15.1±2.7 |
Discussion
Kidney is a high perfusion organ that is highly
sensitive to ischemia, hypoxia and reperfusion. IRI is caused by
blood flow perfusion after long-term organ ischemia, which can
delay recovery of organ functions or even bring damages to tissues
and organs (10). Reperfusion may
also cause tissue damage, cell apoptosis and necrosis, which has
great damage to the tissues and organs of patients (11). Occurrence of renal IRI may cause
unsatisfactory treatment outcomes of shock, renal transplantation
and cardiopulmonary bypass, and is also a main cause of the failure
of renal transplantation (12). At
present, the pathogenesis of IRI is still unclear, and mainstream
theories include calcium overload, leukocyte action and ATP
deficiency (13).
Renal IRI is a complex pathological process with
cell necrosis and apoptosis involved (14). Cell necrosis refers to non-programmed
cell death mediated by the functions of cell lysates, protein
denaturation, and activation of inflammatory factor receptor. Most
of the cell necrosis is caused by reversible organ damage (15). Apoptosis is a process of programmed
cell death that occurs through the regulation of genes, activation
of extracellular molecules and external factors (16). Bcl-2, as one of the cytokines with
anti-apoptotic function, can inhibit free radicals to induce
intracellular calcium overload, causing blocked mitochondrial
membrane permeability and caspase activation, thereby inhibiting
apoptosis (17). Bax is a class of
genes that can promote apoptosis through the regulation of
cytokine, and studies have shown that the ratio of Bax/Bcl-2 can
directly reflect cell apoptosis (18).
In this study, rat IRI model was established.
Expression levels of Scr and BUN in rats of group A that were
treated with saline were significantly lower than those in group B.
Berberine and exendin-(9–39)
pretreatment significantly reduced the levels of Scr and BUN in
group C and D. Scr and BUN are protein metabolites that were
discharged through kidneys. Concentrations of Scr and BUN can
directly reflect glomerular filtration rate. Concentrations of Scr
and BUN will increase under renal damage (19). Our study showed that berberine
pretreatment can effectively inhibit the occurrence of IRI
(19). MDA, as the final products of
lipid in oxidation reactions under high levels of oxidative free
radicals, can reflect the degree of oxidation reaction (20). Therefore, plasma level of MDA was
detected. MDA level was significantly increased in group B compared
with other groups, indicating that free radical-induced peroxide is
one of the causes of tissue damage. Levels of MDA in group B were
significantly higher than those in groups C and D, which
demonstrate that pretreatment with berberine can effectively reduce
the expression of MDA. Studies have shown that (21) Bcl-2 family members play pivotal roles
in cell apoptosis, and regulation of Bax and Bcl-2 protein
expression can effectively reduce the apoptosis. In this study,
western blot analysis results showed that berberine pretreatment
significantly reduced the expression levels of Bax protein and
increased the expression of Bcl-2 protein in group C and D compared
with group B. Studies have shown that (22) Bax expression is upregulated under
cell apoptosis, Bax overexpression can promote the cell apoptosis,
while Bax expression inhibition can inhibit cell apoptosis. Bcl-2
can bind to Bax to form heterodimers, thereby decreasing the
expression of Bax and inhibiting cell apoptosis. TUNEL assay showed
that berberine pretreatment significantly improved cell apoptosis
in group C and D compared with group B. However, cell apoptosis in
group C and D was still more severe than that in group A.
Therefore, berberine pretreatment can effectively reduce the
severity of IRI, but cannot inhibit its occurrence.
However, this study is still limited by some
shortcomings. Sample size is small, and the effects caused by
different surgical methods and different ways of anesthesia were
not excluded. In addition, only animal experiments were performed,
but clinical studies were not included. Those shortcomings will be
improved in our future studies.
In conclusion, berberine can effectively improve
renal function in rats with renal IRI possibly by inhibiting Bax
expression and promoting Bcl-2 expression.
Acknowledgements
Not applicable.
Funding
The study was funded by the Scientific Research Fund
of Traditional Chinese Medicine in Zhejiang (2015ZA224).
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
HZ and JuL designed the study. JiL and LL performed
the animal experiments. HZ, JuL and LL analyzed the animal
experiment data. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
People's Hospital of Lishui Animal Center (Zhejiang, China).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Dorweiler B, Pruefer D, Andrasi TB, Maksan
SM, Schmiedt W, Neufang A and Vahl CF: Ischemia-reperfusion injury:
Pathophysiology and clinical implications. Eur J Trauma Emerg Surg.
33:600–612. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Eckle T: New ‘Guidance’ for the treatment
of hepatic ischemia reperfusion injury through semaphorins and
plexins. Crit Care Med. 44:1623–1624. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wu H, Chen G, Wyburn KR, Yin J, Bertolino
P, Eris JM, Alexander SI, Sharland AF and Chadban SJ: TLR4
activation mediates kidney ischemia/reperfusion injury. J Clin
Invest. 117:2847–2859. 2007. View
Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sung SJ, Li L, Huang L, Lawler J, Ye H,
Rosin DL, Vincent IS, Le TH, Yu J, Görldt N, et al: Proximal tubule
CD73 is critical in renal ischemia-reperfusion injury protection. J
Am Soc Nephrol. 28:888–902. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Nezu M, Souma T, Yu L, Suzuki T, Saigusa
D, Ito S, Suzuki N and Yamamoto M: Transcription factor Nrf2
hyperactivation in early-phase renal ischemia-reperfusion injury
prevents tubular damage progression. Kidney Int. 91:387–401. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zou K, Li Z, Zhang Y, Zhang HY, Li B, Zhu
WL, Shi JY, Jia Q and Li YM: Advances in the study of berberine and
its derivatives: A focus on anti-inflammatory and anti-tumor
effects in the digestive system. Acta Pharmacol Sin. 38:157–167.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Li D, Zheng J, Hu Y, Hou H, Hao S, Liu N
and Wang Y: Amelioration of intestinal barrier dysfunction by
berberine in the treatment of nonalcoholic fatty liver disease in
rats. Pharmacogn Mag. 13:677–682. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Haufe TC, Gilley AD, Goodrich KM, Ryan CM,
Smithson AT, Hulver MW, Liu D and Neilson AP: Grape powder
attenuates the negative effects of GLP-1 receptor antagonism by
exendin-3 (9–39) in a normoglycemic mouse model. Food Funct.
7:2692–2705. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Zhao GL, Yu LM, Gao WL, Duan WX, Jiang B,
Liu XD, Zhang B, Liu ZH, Zhai ME, Jin ZX, et al: Berberine protects
rat heart from ischemia/reperfusion injury via activating
JAK2/STAT3 signaling and attenuating endoplasmic reticulum stress.
Acta Pharmacol Sin. 37:354–367. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Koo TY, Lee JG, Yan JJ, Jang JY, Ju KD,
Han M, Oh KH, Ahn C and Yang J: The P2X7 receptor antagonist,
oxidized adenosine triphosphate, ameliorates renal
ischemia-reperfusion injury by expansion of regulatory T cells.
Kidney Int. 92:415–431. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Linkermann A, Bräsen JH, Darding M, Jin
MK, Sanz AB, Heller JO, De Zen F, Weinlich R, Ortiz A, Walczak H,
et al: Two independent pathways of regulated necrosis mediate
ischemia-reperfusion injury. Proc Natl Acad Sci USA.
110:12024–12029. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Thorenz A, Chen R, Rong S, Klemann C,
Haller H, Braesen JH, Klos A and Gueler F: C5aR2 deficiency
improves renal regeneration after renal ischemia reperfusion injury
and in kidney transplantation in mice. FASEB J. 31:1030.9.
2017.
|
|
13
|
Nogueira MA, Coelho AM, Sampietre SN,
Patzina RA, da Silva Pinheiro F, D'Albuquerque LA and Machado MC:
Beneficial effects of adenosine triphosphate-sensitive
K+ channel opener on liver ischemia/reperfusion injury.
World J Gastroenterol. 20:15319–15326. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Noh MR, Kim JI, Han SJ, Lee TJ and Park
KM: C/EBP homologousprotein (CHOP) gene deficiency attenuates renal
ischemia/reperfusioninjury in mice. Biochim Biophys Acta.
1852:1895–1901. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lau A, Wang S, Liu W, Haig A, Zhang ZX and
Jevnikar AM: Glycyrrhizic acid ameliorates HMGB1-mediated cell
death and inflammation after renal ischemia reperfusion injury. Am
J Nephrol. 40:84–95. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Lin M, Li L, Li L, Pokhrel G, Qi G, Rong R
and Zhu T: The protective effect of baicalin against renal
ischemia-reperfusion injury through inhibition of inflammation and
apoptosis. BMC Complement Altern Med. 14:192014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Edlich F and Martinou JC: Bcl-2 protein
interplay on the outer mitochondrial membraneMitochondria and Cell
Death. Springer; New York: pp. 69–83. 2016, View Article : Google Scholar
|
|
18
|
Liu Y, Wang L, Du Y, Chen Z, Guo J, Weng
X, Wang X, Wang M, Chen D and Liu X: Effects of apigenin
pretreatment against renal ischemia/reperfusion injury via
activation of the JAK2/STAT3 pathway. Biomed Pharmacother.
95:1799–1808. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Schrezenmeier EV, Barasch J, Budde K,
Westhoff T and Schmidt-Ott KM: Biomarkers in acute kidney injury -
pathophysiological basis and clinical performance. Acta Physiol
(Oxf). 219:554–572. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Chatterjee PK, Brown PA, Cuzzocrea S,
Zacharowski K, Stewart KN, Mota-Filipe H, McDonald MC and
Thiemermann C: Calpain inhibitor-1 reduces renal
ischemia/reperfusion injury in the rat. Kidney Int. 59:2073–2083.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Shen S and Zhou J, Meng S, Wu J, Ma J, Zhu
C, Deng G, Liu D, Shen S and Zhou J: The protective effects of
ischemic preconditioning on rats with renal ischemia-reperfusion
injury and the effects on the expression of Bcl-2 and Bax. Exp Ther
Med. 14:4077–4082. 2017.PubMed/NCBI
|
|
22
|
Decuypere JP, Ceulemans LJ, Agostinis P,
Monbaliu D, Naesens M, Pirenne J and Jochmans I: Autophagy and the
kidney: Implications for ischemia-reperfusion injury and therapy.
Am J Kidney Dis. 66:699–709. 2015. View Article : Google Scholar : PubMed/NCBI
|