Introduction
Atrial fibrillation is one of the most common
arrhythmias in clinic. When patients are complicated with acute
myocardial infarction (AMI), the risk of atrial fibrillation is
even higher than 15% (1). Atrial
fibrillation complications may lead to an increase in ventricular
rate, further increasing the myocardial oxygen consumption, and
aggravating myocardial ischemia and hypoxia (2). A large number of studies have confirmed
(3–5)
that atrial fibrillation is an independent risk factor for MI in
patients with coronary heart disease. After coronary heart disease
develops into AMI, the mortality rate of patients may be
significantly increased if they are complicated with atrial
fibrillation. At present, revascularization can be performed
effectively via percutaneous coronary intervention (PCI) for AMI
patients complicated with atrial fibrillation, ensuring the
reperfusion of ischemic myocardium (6). However, there are few literature
studies on the effect of atrial fibrillation (new-onset or
complicated previously) on the prognosis of patients receiving PCI
after MI. In order to fill in the above gap, effects of atrial
fibrillation on complications and prognosis of patients receiving
emergency PCI after AMI were mainly investigated in this study.
Materials and methods
General data
A total of 80 AMI patients treated with
interventional vascular recanalization in the Affiliated Hospital
of Weifang Medical University (Weifang, China) from July 2015 to
October 2016 were selected and received electrocardiogram
examination when enrolled, including 40 patients complicated with
atrial fibrillation before operation (control group) and 40
patients without atrial fibrillation before operation (observation
group). The patients signed the informed consent when enrolled, and
this study was approved by the Ethics Committee of the Affiliated
Hospital of Weifang Medical University (Weifang, China). They were
aged 40–60 years with a survival time of more than 1 year. Patients
complicated with heart failure, definite primary myocardial disease
before operation, severe pulmonary infection, mental illness,
coagulation disorders, platelet dysfunction, systemic immune system
disease, other arrhythmia before onset, and pregnant and/or
breastfeeding patients were eliminated. In observation group, there
were 40 patients without atrial fibrillation, including 21 males
and 19 females. In terms of atrial fibrillation type, there were 35
cases of acute atrial fibrillation, and 5 cases of chronic atrial
fibrillation. The implementation time of interventional treatment
was 1–12 h with an average of 5.1±0.3 h. In the control group,
there were 40 patients complicated with atrial fibrillation,
including 20 males and 20 females. In terms of atrial fibrillation
type, there were 34 cases of acute atrial fibrillation, and 6 cases
of chronic atrial fibrillation. The implementation time of the
interventional treatment was 1–12 h with an average of 5.0±0.3 h.
There were no statistically significant differences in comparisons
of sex, age, atrial fibrillation type and implementation time of
the interventional treatment between the two groups
(p>0.05).
Treatment methods
After admission, all patients received continuous
electrocardiogram monitoring for 24 h, and dynamic
electrocardiogram monitoring for 24 h. The onset time, duration,
and predisposing factors of patients complicated with atrial
fibrillation were recorded, and vital signs of patients at the
onset were clear. Operation standards of PCI were as follows: After
treatment, the stenosis rate of the remaining parts in the coronary
lumen should be <20%, and coronary artery thrombolysis in
myocardial infarction (TIMI) flow grade reaches grade 3. In
perioperative PCI, 300 mg clopidogrel [NMPN J20130083, manufactured
by Sanofi Winthrop Industrie (Floirac, France), subpackaged by
Sanofi Pharmaceutical Co., Ltd. (Hangzhou, China)] was taken at a
draught each time, followed by oral administration of 75 mg
clopidogrel per day for 12 consecutive months after operation. At
the same time, 300 mg aspirin was taken at a draught before
operation, followed by oral administration of 100 mg aspirin/day
after operation for a long term.
Observation indexes
The patients were followed up for 1 year. The
systolic and diastolic blood pressure, heart rate, arrhythmia and
common complications after MI were compared between the two groups
at 1 month after intervention. Changes in coronary artery TIMI flow
grade and left ventricular ejection fraction (LVEF) of patients
before operation, immediately after operation, and at 3 months and
1 year after operation were also compared. Moreover, changes in the
brain natriuretic peptide (BNP) levels before operation and at 1
week and 1 month after operation were compared. Finally, the
recovery time of myocardial enzyme and total troponin in both
groups were recorded.
Evaluation criteria
Coronary artery TIMI flow grade is divided into a
total of 4 grades (grade 0–3) as follows: Grade 0, there is no
blood flow or perfusion; grade 1, there is very little blood flow
or perfusion, and contrast agent can be seen only in the occluded
site; grade 2, there is partial blood flow or perfusion, and
contrast agent can pass the occluded site and reach the distant
end, but the filling rate is lower than normal; and grade 3, there
is normal blood flow or perfusion. BNP was detected via
micro-particle enzyme immunoassay, and its normal range is 0–38
pg/ml. Serum lactic dehydrogenase (LDH) was detected via velocity
method, and its normal range is 100–240 U/l. Creatine kinase-MB
(CK-MB) was detected via colorimetric method, and its normal range
is 0–25 IU/l. The level of cardiac troponin (cTn), including cTnT,
cTnI and cTnC, >1.0 µg/l was used as a critical value of
diagnosis of AMI.
Statistical analysis
Statistical Product and Service Solutions (SPSS)
13.0 software (SPSS, Inc., Chicago, IL, USA) was used. Measurement
data are presented as mean ± standard deviation (mean ± SD). t-test
was used for the comparison of means between the two groups, and
Chi-square test was used for the intergroup comparison of rates.
P<0.05 was considered to indicate a statistically significant
difference.
Results
Comparison of systolic and diastolic
blood pressure as well as heart rate at 1 month after intervention
between the two groups
At 1 month after intervention, the systolic and
diastolic blood pressure in the observation group were
significantly higher than those in the control group (p<0.05),
but the heart rate was lower than that in the control group
(p<0.05) (Table I).
 | Table I.Comparison of systolic blood pressure,
diastolic blood pressure and heart rate at 1 month after
intervention between the two groups (mean ± SD). |
Table I.
Comparison of systolic blood pressure,
diastolic blood pressure and heart rate at 1 month after
intervention between the two groups (mean ± SD).
| Groups | Systolic blood
pressure (mmHg) | Diastolic blood
pressure (mmHg) | Heart rate
(time/min) |
|---|
| Observation | 105.6±2.7 | 68.9±1.1 | 87.5±2.9 |
| Control | 85.3±1.9 | 47.6±0.6 | 98.6±3.6 |
| t-test | 38.888 | 107.513 | 15.186 |
| P-value | 0.001 | 0.001 | 0.001 |
Comparison of arrhythmia between the
two groups
During the intervention, the total proportion of
patients with ventricular arrhythmia, atrial arrhythmia,
atrioventricular block and sinus tachycardia in the observation
group was significantly lower than that in the control group
(p<0.05) (Table II).
 | Table II.Comparison of arrhythmia between the
two groups (n). |
Table II.
Comparison of arrhythmia between the
two groups (n).
| Groups | Ventricular
arrhythmia | Atrial
arrhythmia | Atrioventricular
block | Sinus
tachycardia |
|---|
| Observation | 1 | 2 | 1 | 2 |
| Control | 10 | 13 | 9 | 11 |
| χ2 | 6.746 | 8.205 | 5.600 | 5.878 |
| P-value | 0.009 | 0.004 | 0.018 | 0.015 |
Comparison of common complications
after MI between the two groups
During the 1-year follow-up after operation, the
total proportion of common complications after MI, such as
ventricular aneurysm, cardiac rupture, mural thrombosis and
syndromes after MI, in the observation group was obviously lower
than that in the control group (p<0.05) (Table III).
 | Table III.Comparison of common complications
after MI between the two groups (n). |
Table III.
Comparison of common complications
after MI between the two groups (n).
| Groups | Ventricular
aneurysm | Cardiac rupture | Mural thrombosis | Syndromes after
MI | Total incidence
rate |
|---|
| Observation | 2 | 0 | 2 | 1 | 5
(12.5%) |
| Control | 6 | 1 | 7 | 3 | 17 (42.5%) |
| χ2 |
| – |
| 9.028 |
| P-value |
| – |
| 0.001 |
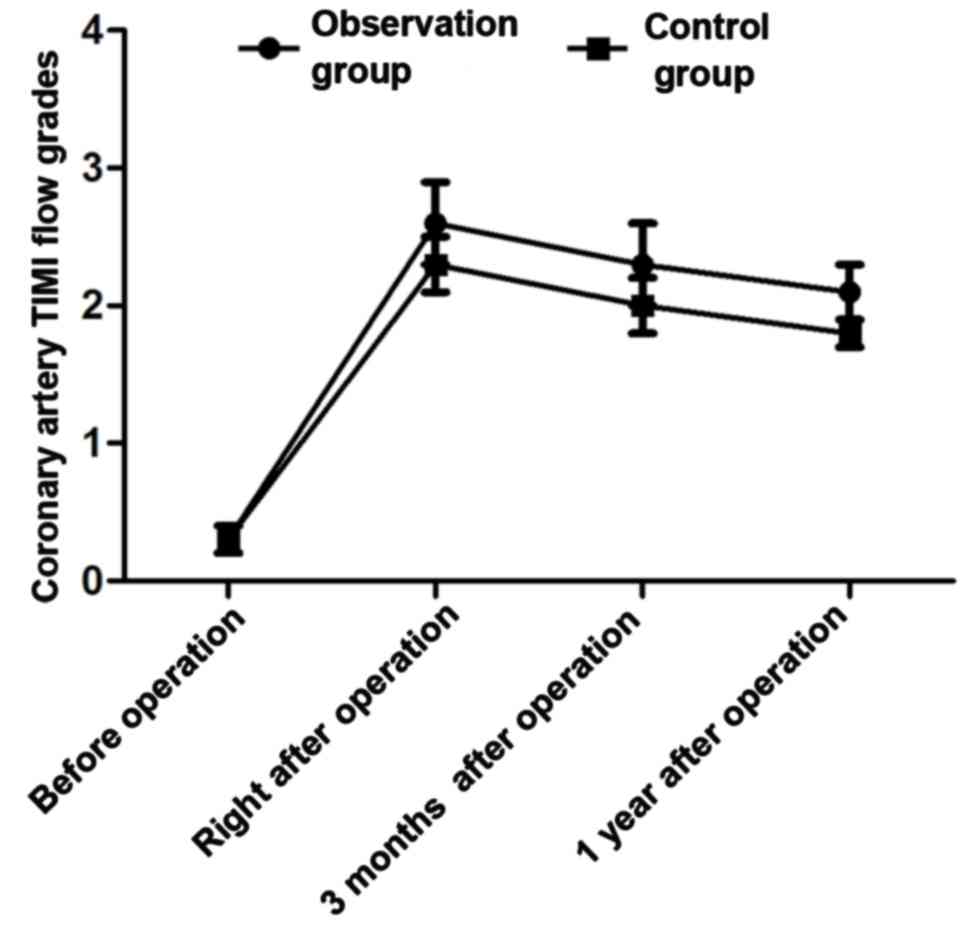
Changes in coronary artery TIMI blood
flow grades of patients at different time-points before and after
operation
There was no statistically significant difference in
the coronary artery TIMI flow grade between the two groups before
operation (grade 0.3±0.3 vs. 0.3±0.1, t=0.000, p>0.05) (Fig. 1). The coronary artery TIMI flow
grades in the observation group immediately after operation, and at
3 months and 1 year after operation were grade (2.6±0.3), (2.3±0.3)
and (2.1±0.2), respectively, which were significantly higher than
those in the control group (grade 2.2±0.2, 2.0±0.2 and 1.7±0.1)
(t=7.016, 5.262 and 11.314, p<0.05).
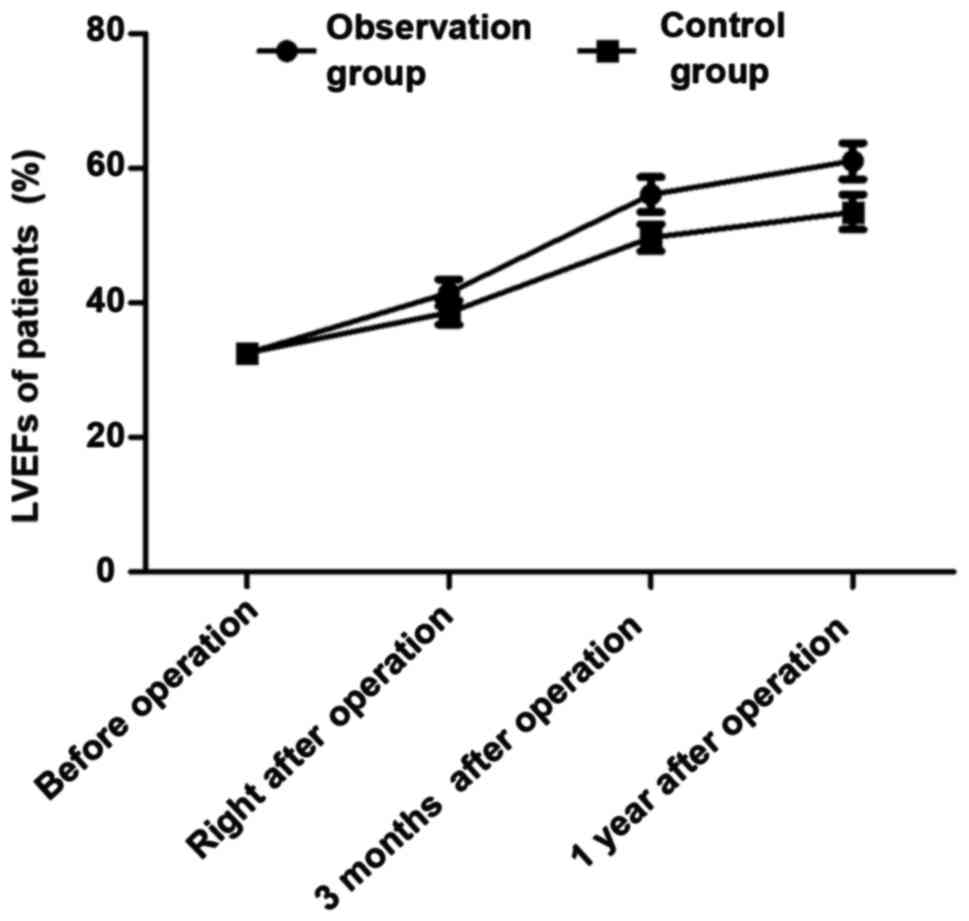
Changes in LVEFs of patients at
different time-points before and after operation
There was no statistically significant difference in
LVEF between the two groups before operation (32.5±1.5 vs.
32.6±1.5%, t=0.298, p=0.766 >0.05) (Fig. 2). LVEFs in the observation group
immediately after operation, and at 3 months and 1 year after
operation were (41.5±2.0, 56.1±2.6 and 61.1±2.7%), respectively,
which were significantly higher than those in the control group
(38.6±1.8, 49.7±2.0 and 53.5±2.6%) (t=6.816, 12.340 and 12.823,
p<0.05).
Changes in BNP levels of patients at
different time-points before and after operation
There was no statistically significant difference in
the BNP level between the two groups before operation (1285.6±23.6
vs. 1286.5±23.5 mg/l, t=0.171, p=0.865 >0.05) (Fig. 3). The BNP levels in the observation
group at 1 week and 1 month after operation were (356.6±15.1 and
113.2±5.1 mg/l), respectively, which were obviously lower than
those in the control group (689.9±20.8 and 286.9±9.5 mg/l)
(t=82.012 and 101.886, p<0.05).
Comparison of recovery time of
myocardial enzyme and total troponin between the two groups
The recovery time of myocardial enzyme and total
troponin in the observation group was significantly earlier than
that in thw control group (p<0.05) (Table IV).
 | Table IV.Comparison of recovery time of
myocardial enzyme and total troponin between the two groups (mean ±
SD). |
Table IV.
Comparison of recovery time of
myocardial enzyme and total troponin between the two groups (mean ±
SD).
| Groups | LDH (days) | CK-MB (h) | Total troponin
(days) |
|---|
| Observation | 8.1±0.2 | 65.3±2.1 | 11.3±0.5 |
| Control | 9.6±0.3 | 71.2±3.1 | 13.7±0.9 |
| t-test | 26.312 | 9.966 | 14.743 |
| P-value | 0.001 | 0.001 | 0.001 |
Discussion
Currently, the pathogenesis of AMI complicated with
atrial fibrillation is not yet fully understood in clinic, among
which sinoatrial node ischemia (7)
and decreased electrical stability of myocardium (8) are common theories. In AMI patients
complicated with atrial fibrillation, the lesion is often located
in the right coronary artery, and the possible reason is that the
obstruction of the right coronary artery is prone to cause
sinoatrial hypofunction, affecting sinus rhythm (9). At the same time, the electrical
stability of myocardium is decreased, leading to atrial
fibrillation. If AMI patients are complicated with atrial
fibrillation, the cardiac output may be further reduced, increasing
ventricular rate, causing further imbalance between myocardial
oxygen supply and demand, aggravating myocardial ischemia and
hypoxia, and even expanding the infarct size, ultimately inducing
and aggravating heart failure and even resulting in cardiac arrest
in patients (10). Timely PCI is
currently the most effective treatment method for AMI (11). At present, there is abundant
literature worldwide mainly on research on prognosis of AMI
patients complicated with atrial fibrillation, but literature on
the effect of atrial fibrillation on PCI after AMI is scarce.
In this study, AMI patients undergoing PCI were
divided into the observation group (without atrial fibrillation)
and the control group (complicated with atrial fibrillation)
according to whether they were complicated with atrial
fibrillation. All patients were followed up for 1 year. Comparisons
of systolic and diastolic blood pressure as well as heart rate
between the two groups at 1 month after intervention showed that
systolic and diastolic blood pressure in the observation group were
significantly higher than those in the control group, but the heart
rate was lower than that in the control group, suggesting that the
postoperative circulatory function of patients without atrial
fibrillation is more stable with better recovery. In addition, the
research on arrhythmia and common complications after MI in both
groups showed that the proportion of patients with ventricular
arrhythmia, atrial arrhythmia, atrioventricular block and sinus
tachycardia in the observation group was significantly lower than
that in control group, and the total proportion of common
complications after MI, such as ventricular aneurysm, cardiac
rupture, mural thrombosis and syndromes after MI, in the
observation group was obviously lower than that in the control
group, indicating that arrhythmia, ventricular aneurysm, cardiac
rupture, mural thrombosis and syndromes after MI seldom occur in
patients without atrial fibrillation receiving PCI after MI. At the
same time, it was found during the follow-up that the coronary
artery TIMI flow grades and LVEFs in the observation group
immediately after operation, and at 3 months and 1 year after
operation were obviously higher than those in the control group
during the same period, and at 1 week and 1 month after operation,
the BNP levels in the observation group were significantly lower
than those in the control group during the same period, suggesting
that in patients without atrial fibrillation, the effect of
vascular recanalization is better. The maintenance time is longer,
and postoperative LVEF can be recovered rapidly and effectively,
thus reducing myocardial damage and improving prognosis of
patients. Finally, the recovery time of myocardial enzyme and total
troponin was compared between the two groups, and it was found that
the recovery time of myocardial enzyme and total troponin in the
observation group was significantly earlier than that in the
control group, further proving that the postoperative recovery of
patients without atrial fibrillation is quicker.
Performing vascular recanalization in coronary
artery in the early stage, and maintaining myocardial perfusion,
thus quickly and effectively relieving myocardial ischemia and
hypoxia (12) have important values
in increasing and improving the sinoatrial node arterial blood
supply and reducing postoperative complications in AMI patients.
Once MI occurs in patients complicated with atrial fibrillation
before operation, especially rapid atrial fibrillation (13), cardiac function is prone to decline
significantly (14), thereby
aggravating myocardial ischemia via positive feedback, and
increasing infarct size (15).
Although timely interventional vascular recanalization is
effective, it is difficult to improve sinoatrial node function in a
short time, especially for patients with chronic atrial
fibrillation (16). The long-term
atrial fibrillation may result in mural thrombus shedding after MI,
thus causing thromboembolic disease (17). Meanwhile, atrial fibrillation
complicated before operation may further reduce the cardiac
function of patients, increase ventricular rate and myocardial
oxygen consumption (18), and lead
to hemodynamic disorders, thereby increasing myocardial infarct
size (19), even inducing heart
failure and aggravating myocardial damage (20).
In conclusion, atrial fibrillation has a certain
negative effect on circulatory function in patients with AMI after
interventional therapy, and the proportions of arrhythmia and
complications in patients after MI are increased at the same time,
so the postoperative recovery of patients is slow and with many
complications.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
YZ contributed to the conception and design of the
study and provided statistical methods. LZ performed the research
and collected and analyzed the data of this study. HZ was
responsible for carrying out additional analysis and interpreting
the results. HC wrote the initial draft, revised and finalized this
study and was responsible for the treatment of patients. All
authors have read and approved the final manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
Affiliated Hospital of Weifang Medical University (Weifang, China).
Signed informed consents were obtained from the patients or
guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Batra G, Friberg L, Erlinge D, James S,
Jernberg T, Svennblad B, Wallentin L and Oldgren J: Antithrombotic
therapy after myocardial infarction in patients with atrial
fibrillation undergoing percutaneous coronary intervention. Eur
Heart J Cardiovasc Pharmacother. 6:36–45. 2018. View Article : Google Scholar
|
|
2
|
Chen J, Wang LY, Deng C, Jiang XH and Chen
TG: The safety and efficacy of oral anticoagulants with dual versus
single antiplatelet therapy in patients after percutaneous coronary
intervention: A meta-analysis. Medicine (Baltimore).
96:e80152017.https://doi.org/10.1097/MD.0000000000008015simple10.1097/MD.0000000000008015
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Cannon CP, Bhatt DL, Oldgren J, Lip GYH,
Ellis SG, Kimura T, Maeng M, Merkely B, Zeymer U, Gropper S, et al:
RE-DUAL PCI Steering Committee and Investigators: Dual
antithrombotic therapy with dabigatran after PCI in atrial
fibrillation. N Engl J Med. 377:1513–1524. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hwang KK, Eom SY, Lee SY, Kim SM, Cho MC,
Kim YJ, Seung KB, Jeong MH and Bae JW; other Korea Acute Myocardial
Infarction Registry Investigators, : Atrial fibrillation on
admission is related with higher mortality in ST-segment elevation
myocardial infarction patients. Int Heart J. 58:486–494. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Zhai HB, Liu J, Dong ZC, Wang DX and Zhang
B: Current use of oral anticoagulants and prognostic analysis in
patients with atrial fibrillation undergoing coronary stenting.
Chin Med J (Engl). 130:1418–1423. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ispas AF, Mangin L, Paziuc A and Belle L:
Unexpected evolution of a non-stenotic lesion in the left main
coronary artery of a patient with non-ST-segment elevation
myocardial infarction. Cardiovasc Diagn Ther. 7:340–344. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Choi HI, Ahn JM, Kang SH, Lee PH, Kang SJ,
Lee SW, Kim YH, Lee CW, Park SW, Park DW, et al: Prevalence,
management, and long-term (6-year) outcomes of atrial fibrillation
among patients receiving drug-eluting coronary stents. JACC
Cardiovasc Interv. 10:1075–1085. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Topaz G, Flint N, Steinvil A, Finkelstein
A, Banai S, Keren G, Shacham Y and Yankelson L: Long term prognosis
of atrial fibrillation in ST-elevation myocardial infarction
patients undergoing percutaneous coronary intervention. Int J
Cardiol. 240:228–233. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Gwyn JCV, Thomas MR and Kirchhof P: Triple
antithrombotic therapy in patients with atrial fibrillation
undergoing percutaneous coronary intervention: A viewpoint. Eur
Heart J Cardiovasc Pharmacother. 3:157–162. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Romanov A, Martinek M, Pürerfellner H,
Chen S, De Melis M, Grazhdankin I, Ponomarev D, Losik D, Strelnikov
A, Shabanov V, et al: Incidence of atrial fibrillation detected by
continuous rhythm monitoring after acute myocardial infarction in
patients with preserved left ventricular ejection fraction: Results
of the ARREST study. Europace. 20:263–270. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bogacki P, Kabłak-Ziembicka A, Bryniarski
K, Wrotniak L, Ostrowska-Kaim E, Żmudka K and Przewłocki T: Triple
anticoagulation therapy in patients with atrial fibrillation
undergoing percutaneous coronary intervention - real life
assessment. Postepy Kardiol Interwencyjnej. 12:303–313.
2016.PubMed/NCBI
|
|
12
|
Chaudhary N, Bundhun PK and Yan H:
Comparing the clinical outcomes in patients with atrial
fibrillation receiving dual antiplatelet therapy and patients
receiving an addition of an anticoagulant after coronary stent
implantation: A systematic review and meta-analysis of
observational studies. Medicine (Baltimore). 95:e55812016.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Gibson CM, Mehran R, Bode C, Halperin J,
Verheugt FW, Wildgoose P, Birmingham M, Ianus J, Burton P, van
Eickels M, et al: Prevention of bleeding in patients with atrial
fibrillation undergoing PCI. N Engl J Med. 375:2423–2434. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zehir R, Tekkesin AI, Haykir N, Velibey Y,
Borklu EB and Gumusdag A: Peak troponin I level predicts new-onset
atrial fibrillation in patients with myocardial infarction. Clin
Invest Med. 39:E213–E219. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Prami T, Khanfir H, Deleskog A, Hasvold P,
Kytö V, Reissell E and Airaksinen J: Clinical factors associated
with initiation of and persistence with ADP receptor-inhibiting
oral antiplatelet treatment after acute coronary syndrome: A
nationwide cohort study from Finland. BMJ Open. 6:e0126042016.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Bagai A, Wang TY, Goodman SG, Fisher HN,
Welsh RC, Dery JP, Zhang X, Zhu YE, Cheema AN, Dehghani P, et al:
Canadian Observational AntiPlatelet sTudy (COAPT) Investigators:
Longitudinal treatment patterns with ADP receptor inhibitors after
myocardial infarction: Insights from the Canadian Observational
AntiPlatelet sTudy. Int J Cardiol. 228:459–464. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Cannon CP, Gropper S, Bhatt DL, Ellis SG,
Kimura T, Lip GY, Steg PG, Ten Berg JM, Manassie J, Kreuzer J, et
al: RE-DUAL PCI Steering Committee and Investigators: Design and
Rationale of the RE-DUAL PCI Trial: A prospective, randomized,
phase 3b study comparing the safety and efficacy of dual
antithrombotic therapy with dabigatran etexilate versus warfarin
triple therapy in patients with nonvalvular atrial fibrillation who
have undergone percutaneous coronary intervention with stenting.
Clin Cardiol. 39:555–564. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Dekkers OM, Horváth-Puhó E, Cannegieter
SC, Vandenbroucke JP, Sørensen HT and Jørgensen JO: Acute
cardiovascular events and all-cause mortality in patients with
hyperthyroidism: A population-based cohort study. Eur J Endocrinol.
176:1–9. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Hudzik B, Szkodziński J, Hawranek M,
Lekston A, Poloński L and Gąsior M: CHA2DS2-VASc score is useful in
predicting poor 12-month outcomes following myocardial infarction
in diabetic patients without atrial fibrillation. Acta Diabetol.
53:807–815. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Masuda M, Nakatani D, Hikoso S, Suna S,
Usami M, Matsumoto S, Kitamura T, Minamiguchi H, Okuyama Y, Uematsu
M, et al: OACIS Investigators: Clinical impact of ventricular
tachycardia and/or fibrillation during the acute phase of acute
myocardial infarction on in-hospital and 5-year mortality rates in
the percutaneous coronary intervention era. Circ J. 80:1539–1547.
2016. View Article : Google Scholar : PubMed/NCBI
|