Introduction
The liver is the second most frequently injured
solid organ in the abdominal cavity. Blunt liver trauma demands
emergency treatment and remains a great challenge for surgeons
(1,2). Normally, the rib cage and the
vertebral column protect the liver from violent forces from outside
the body; the ligaments and vena cava fix the liver in place to
avoid violent movements (3).
However, under certain extreme circumstances, the rib cage and the
ligaments take part in the liver trauma. There are two previously
described mechanisms of blunt liver trauma, deceleration injury and
crush injury (1,2,4). The
patterns of blunt liver trauma are closely correlated with the
characteristics of the blunt force. The direction, velocity, grade
and site where the blunt force lands, as well as the position and
motion of the victim when the injury occurred, all contribute to
the patterns and severity of the blunt liver injury. The present
study utilizes illustrations to demonstrate the patterns of blunt
liver trauma following various blunt forces, in the hope that in
this way the mechanisms of blunt liver injury may be clearly
understood and memorized, therefore aiding emergency surgeons to
improve the management of major blunt liver injuries.
Patients and methods
A total of 53 blunt liver trauma patients who
underwent surgery in the First Affiliated Hospital of Wenzhou
Medical College between 1999 and 2009 were included in this study.
The doctor’s and nurse’s notes were reviewed for information on
gender, age and hospital stay. Special attention was given to the
cause of the injury, the direction of the blunt force and the site
on which it landed. Surgical records and CT films were particularly
studied to obtain information on the patterns and severity of the
liver injuries. Overall, 47 male and 6 female patients aged between
15 and 71 years old (mean, 37.5 years) were included in this study.
All CT scans were performed and reviewed by qualified doctors.
Experienced surgeons performed all surgical procedures and the
details of these procedures were recorded carefully. The study was
approved by the ethics committee of the First Affiliated Hospital
of Wenzhou Medical College, Wenzhou, China. Written informed
patient consent was obtained from the patient’s family.
Results
General items
At the time of admission, the mean blood pressure of
the 53 patients was 12.4±4.6/7.4±3.3 kPa and the mean heart rate
was 103±19 beats per min. The mean hospital stay was 16±10 days.
Multiple injuries and organ dysfunctions resulted in a mortality
rate of ∼19% (10 patients). In total, 44 patients had multiple
injuries. Of these, 25 patients had coexisting thoracic injuries,
the majority in the form of multiple rib fractures and lung
contusions. Pelvic bone fractures and bladder ruptures were
diagnosed in 3 patients, while 2 patients had splenic injuries, 1
patient had a right renal laceration and 2 patients suffered spine
bone fractures. The average intraperitoneal hemorrhage volume was
2,144±1,469 ml and the mean quantity of red blood cells infused was
10 units. A CT was not used in 22 patients.
Characteristics of the blunt
force
Injuries were caused by traffic accidents in 35
patients and by falls from varying heights in 10 patients, while
the remainder were injured by being hit with fists (3 patients) and
heavy objects (5 patients). A total of 30 patients had records on
the site of the blunt force; the majority landed on the upper right
quadrant or the belly. ‘Hit’ or ‘crush’ were the words most
frequently used to depict the way in which the blunt force
occurred. No details were provided as to the velocity of the blunt
force or the motion of the victims in the accidents.
Scale and patterning of the blunt
liver trauma
According to the American Association for the
Surgery of Trauma (AAST) liver injury scale (1994 version)
(5), every trauma was grade II or
beyond; there were 5 grade II, 8 grade III, 27 grade IV and 13
grade V. During surgery, 32 patients suffered active bleeding. To
control this bleeding, 5 patients received hepatic artery ligation,
while the remaining patients underwent either direct ligation of
the bleeding or suturing of the lacerated liver. A total of 36
traumas (67.9%) occurred in the right lobe of the liver, 18 of
which had lacerations between the anterior and posterior lobes.
Liver lacerations along Cantlie’s line were identified in 7
patients. A total of 9 traumas (17%) were in the left lobe of the
liver and of these, 7 patients had a laceration either to the left
or to the right of the falciform ligament. Only 1 patient (1.9%)
suffered trauma in Couinaud segment I. With regard to injuries to
the right lobe of the liver, the majority were irregular in shape
(stellate).
Discussion
Mechanisms of blunt liver trauma
There were previously two well-recognized mechanisms
of blunt liver trauma: deceleration injury and crush injury
(1,2,4). In
the present study, acceleration injury has been identified as
another mechanism. The following descriptions and illustrations aim
to demonstrate the mechanisms of blunt liver trauma clearly and
accurately.
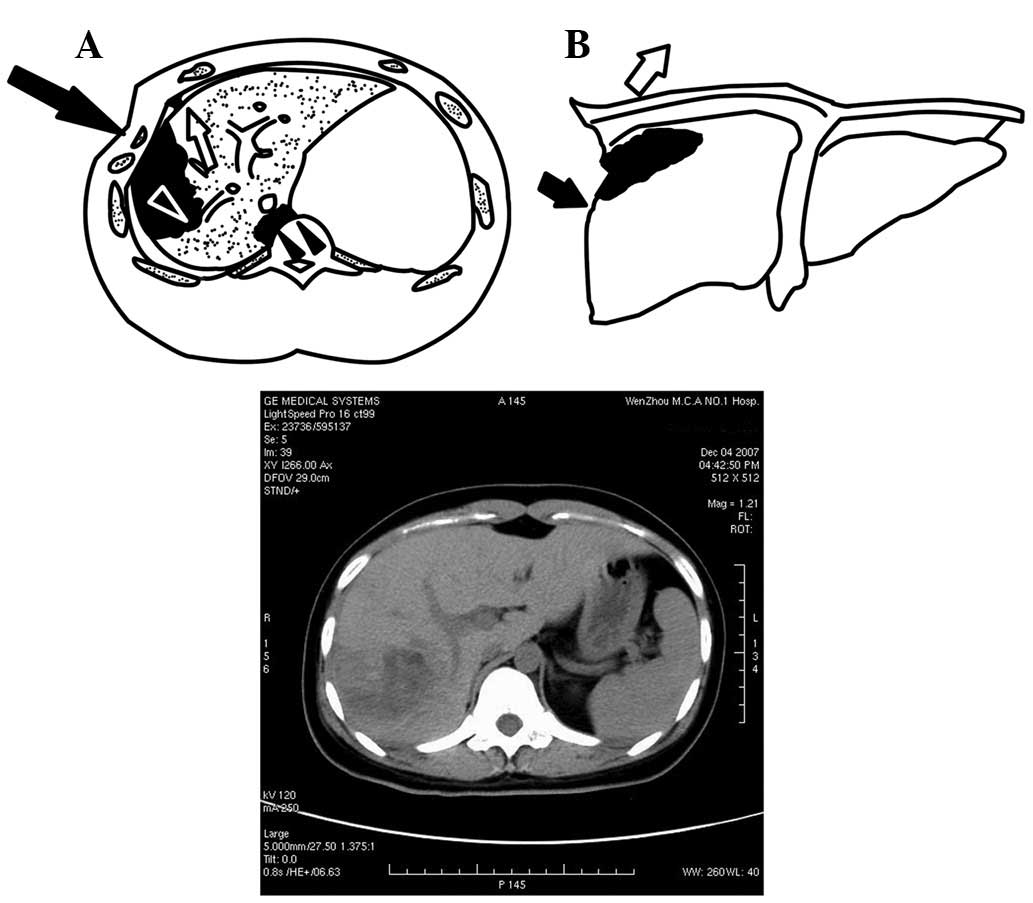
Acceleration injury
Acceleration injury in the right lobe
of the liver
Although the right lobe of the liver is under the
protection of the rib cage, it is susceptible to blunt forces when
the speed or impact are large enough. Trauma in the right lobe
accounted for 67.9% of all traumas in the present study, which is
consistent with previous studies (1,2,6).
These types of injuries are usually caused by forces from a
lateral, right direction. The force lands on the chest wall,
depresses it and then swiftly propels the liver. The right
triangular ligament attaches to the site between Couinaud segments
VII and VIII, making segment VII relatively fixed while segments
VIII and V continue to move violently. This explains why
lacerations are most frequently located between the anterior and
posterior lobes. In the present study, out of the 36 right lobe
lacerations, 18 cases were of this category. Under huge forces and
high speeds, these lacerations may occasionally reach the inferior
vena cava where the hepatic veins join, and result in the
laceration of the retrohepatic vena cava and major hepatic vein
(Fig. 1) (4,7–10).
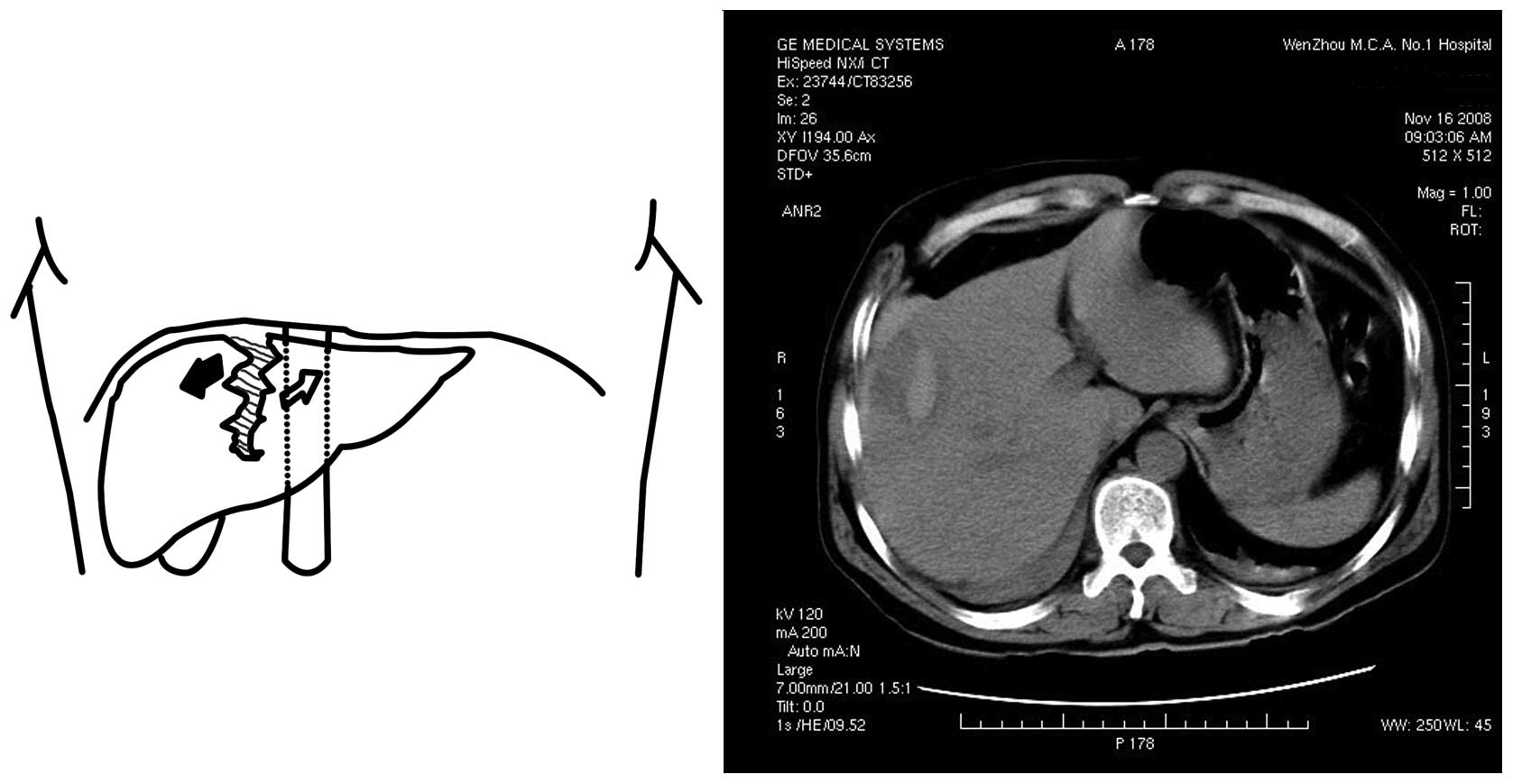
When the blunt force comes from the front, the liver
is propelled in an anterior-posterior direction. As the vena cava
is relatively fixed and serves as a counterforce when the right
lobe is pushed towards the back, the liver lacerates along
Cantlie’s line. The existence of the plane along Cantlie’s line
also makes this site weaker and less able to resist the force
causing the laceration (Fig. 2)
(3–5,11).
Acceleration injury in the left lobe
of the liver
When the blunt force lands on the front of the
chest, the left lobe of the liver is pushed towards the back. The
falciform ligament fixes the liver to the diaphragm and prevents
its movement, so that in blunt force trauma to the chest the
attachment site on the liver bears the majority of the stress and
is lacerated (4). When the blunt
force is to the left of the falciform ligament, the lateral left
lobe is pushed backwards and the laceration is to the left of the
falciform ligament. When the blunt force is to the right of the
falciform ligament, the laceration is also to the right of the
falciform ligament (Fig. 3). The
left hepatic vein and the left branches of the portal vein or
hepatic bile duct may be ‘cut off’ in deep lacerations of this
pattern.
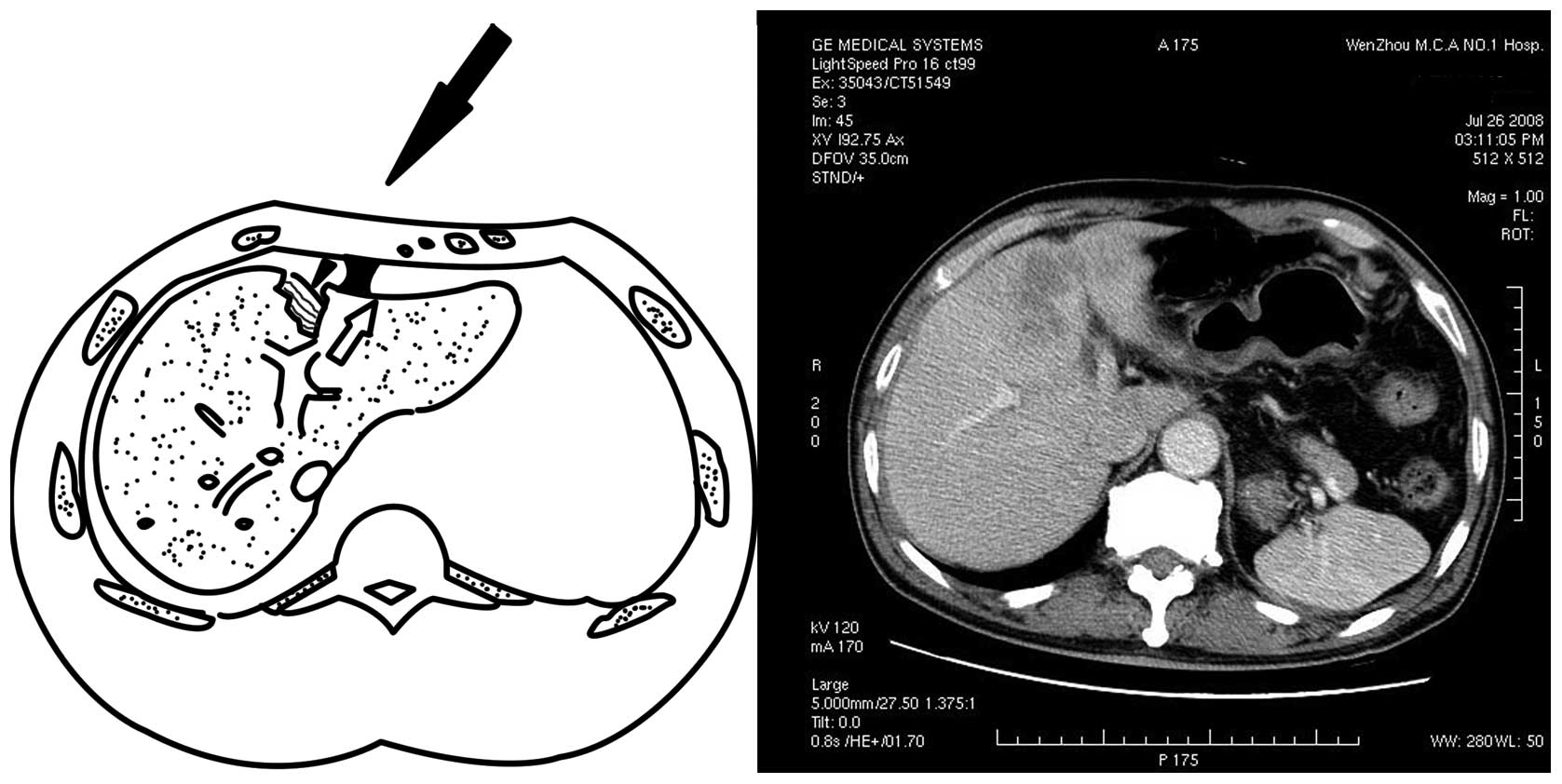
Deceleration injury
Another mechanism of liver injury in the right lobe
of the liver is deceleration injury. This type of injury often
occurs in traffic accidents and falls. When the rapidly moving body
is suddenly stopped, the liver keeps moving and collides against
the chest wall, resulting in a deceleration injury. The liver may
also be propelled by huge forces at high speeds, then move towards
and collide against the posterior abdominal wall, crushing or
lacerating this section of the liver (Fig. 4).
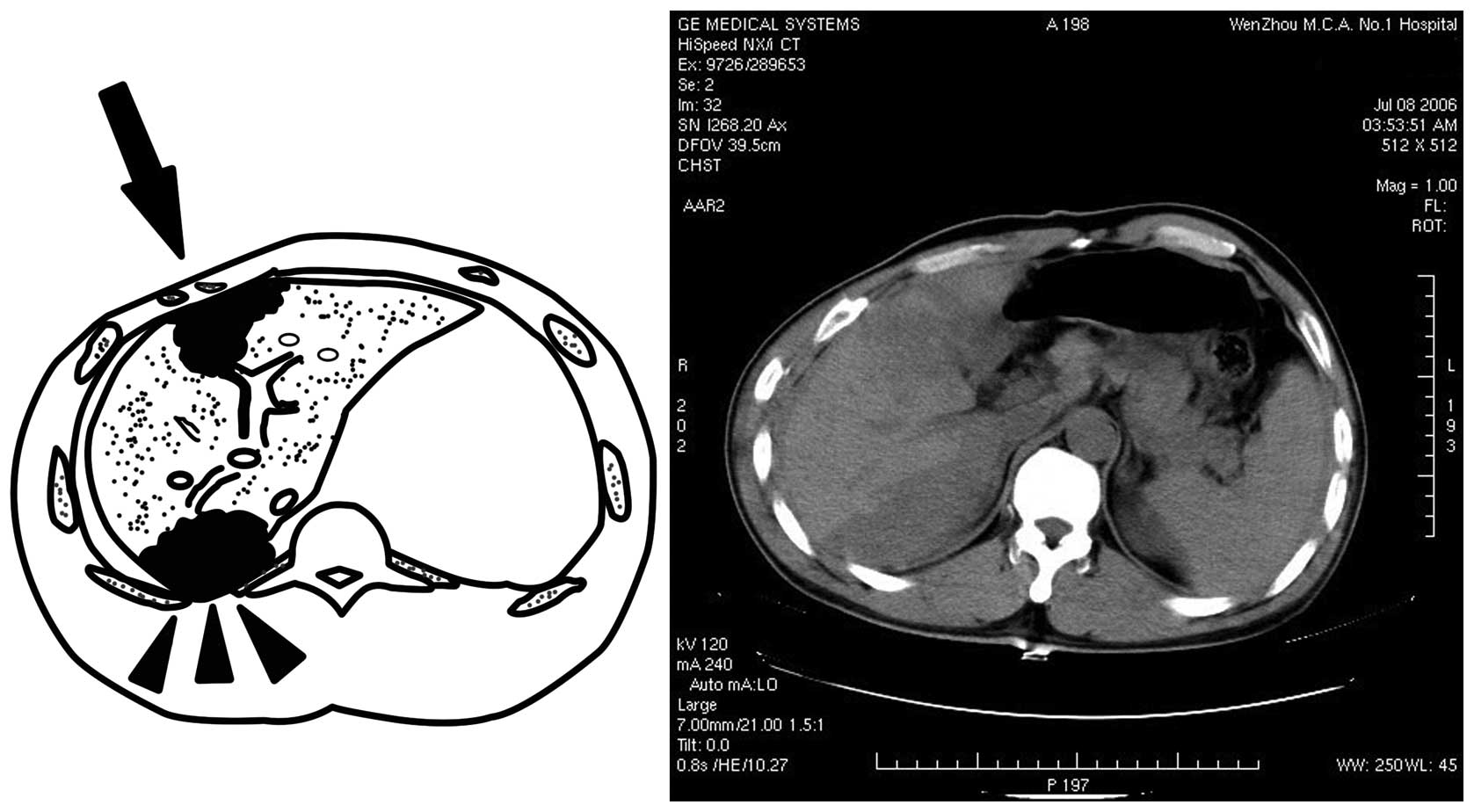
Compression injury
Compression injuries of the liver have previously
been mentioned in other studies (1,2). The
right lobe of the liver is relatively large and fixed so that when
the upper right quadrant is under compression in an
anterior-posterior manner, the liver has no room to escape and is
crushed between the anterior and posterior walls of the rib cage.
As a result, the posterior and anterior sides of the right lobe of
the liver lacerate at the same time. Occasionally the laceration
becomes a penetrating laceration or may even be completely
destroyed if the compression force is large enough (Fig. 5).
Clinical implications
Although the present study identified three main
patterns of blunt liver trauma, it also revealed that liver trauma
is not decided by one single factor and that liver trauma in one
patient is not confined to one single pattern. Certain superficial
lacerations may be the result of the violent friction of the liver
against the chest wall, particularly when the chest wall is broken
and the surface is no longer smooth. When these lacerations are
small, they are difficult to identify on CT scans. As the left lobe
is smaller than the right, and is less fixed, in the present study
it appeared that there were fewer compression and deceleration
injuries in the left lobe than in the right lobe of the liver.
These findings indicate the importance of
investigations into the circumstances in which the injury occurred.
The forensic experts would be able to speculate the cause of the
blunt liver trauma according to the patterns of the trauma when no
other details were available (12). As for clinical doctors, attention
should be paid to the speed at which a traffic accident occurs, the
direction of the blunt force, the site the force hits and whether
or not the victim was compressed, as these factors make a
difference to the outcome of the injury. It is difficult to
investigate the conditions under which the injuries take place, but
careful and detailed investigation of the history is of great
importance in the analysis of the trauma as the patterns and the
severity of the liver injury are predominantly decided by the
pattern of the blunt force.
Knowing that major hepatic trauma is always
associated with thoracic injury (13), special attention should be paid to
the chest; if possible, the chest should also be included in the CT
scan. The CT scan provides the most valuable details, including
site, type and severity of the trauma and whether there is also
active bleeding (14–16). When performing CT scans and
surgery, attention should be paid to the opposite side of the liver
to which the blunt force landed. Occasionally the major injury is
easily identified on the side where the forces land, but the injury
on the opposite side is neglected.
Liver injuries caused by blunt force trauma are
mainly associated with the right lobe. In the present study it
appeared that the demarcation lines of the liver, be it on the
surface or intrahepatically, were the sites where the trauma most
often occurred. The anatomical demarcation line of the liver is the
area where major hepatic veins are located. Severe injuries between
Couinaud segments VII and VIII may injure the retrohepatic vena
cava and the right hepatic vein. Injuries in the right lobe of the
liver are extremely deep in the abdominal cavity and difficult to
expose, which demands that surgeons select an appropriate incision
to expose the laceration and avoid any improper movements of the
liver that may make the laceration even worse. Occasionally this
may lacerate the major hepatic vein or vena cava (4,17,18).
The deep laceration along the falciform ligament caused by
acceleration also demands great attention, as the left hepatic vein
or the left branches of the portal vein or hepatic bile duct may be
cut off by the injury.
Conclusion
Blunt liver trauma follows certain patterns and is
mainly cause by three mechanisms: acceleration, deceleration and
compression. The properties of the blunt force play a key role in
blunt liver trauma. A thorough understanding of the mechanisms
behind blunt liver trauma may aid doctors in the management of
patients with this condition.
References
|
1.
|
Ahmed I and Beckingham IJ: Liver trauma.
Trauma. 9:171–180. 2007. View Article : Google Scholar
|
|
2.
|
Beckingham IJ and Krige JE: ABC of
diseases of liver, pancreas, and biliary system: Liver and
pancreatic trauma. BMJ. 322:783–785. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Rutkauskas S, Gedrimas V, Pundzius J,
Barauskas G and Basevicius A: Clinical and anatomical basis for the
classification of the structural parts of liver. Medicina (Kaunas).
42:98–106. 2006.PubMed/NCBI
|
|
4.
|
Sherlock DJ and Bismuth H: Secondary
surgery for liver trauma. Br J Surg. 78:1313–1317. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Moore EE, Cogbill TH, Jurkovich GJ,
Shackford SR, Malangoni MA and Champion HR: Organ injury scaling:
spleen and liver (1994 revision). J Trauma. 38:323–324. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Rivkind AI, Siegel JH and Dunham CM:
Patterns of organ injury in blunt hepatic trauma and their
significance for management and outcome. J Trauma. 29:1398–1415.
1989. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Buckman RF Jr, Miraliakbari R and
Badellino MM: Juxtahepatic venous injuries: a critical review of
reported management strategies. J Trauma. 48:978–984. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Phelan H, Hunt JP and Wang YZ:
Retrohepatic vena cava and juxtahepatic venous injuries. South Med
J. 94:728–731. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Ciresi KF and Lim RC Jr: Hepatic vein and
retrohepatic vena caval injury. World J Surg. 14:472–477. 1990.
View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Moulton SL, Lynch FP, Canty TG, Collins DL
and Hoyt DB: Hepatic vein and retrohepatic vena caval injuries in
children: Sternotomy first? Arch Surg. 126:1262–1266. 1991.
View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Arnoux PJ, Serre T, Cheynel N, et al:
Liver injuries in frontal crash situations a coupled
numerical-experimental approach. Comput Methods Biomech Biomed
Engin. 11:189–203. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Brammer RD, Bramhall SR, Mirza DF, et al:
A 10-year experience of complex liver trauma. Br J Surg.
89:1532–1537. 2002.PubMed/NCBI
|
|
13.
|
Poletti PA, Mirvis SE, Shanmuganathan K,
Killeen KL and Coldwell D: CT criteria for management of blunt
liver trauma: correlation with angiographic and surgical findings.
Radiology. 216:418–427. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Mauritz W and Weninger P: Multislice
computed tomography in blunt abdominal trauma. Trauma. 9:195–212.
2007. View Article : Google Scholar
|
|
15.
|
Becker CD, Gal I, Baer HU and Vock P:
Blunt hepatic trauma in adults: correlation of CT injury grading
with outcome. Radiology. 201:215–220. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Kirby RM and Braithwaite M: Management of
liver trauma. Br J Surg. 87:17322000. View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Parks RW, Chrysos E and Diamond T:
Management of liver trauma. Br J Surg. 86:1121–1135. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Vock R: Liver rupture caused by isolated
blunt force impact: the result of a blow, a kick or a fall? Int J
Legal Med. 114:244–247. 2001. View Article : Google Scholar : PubMed/NCBI
|