Introduction
Retroperitoneal fibrosis (RPF) is a rare disease of
unclear etiology, which was first described by Albarran in 1905
(1). Recently, there have been
more cases of this disease reported (2,3). RPF
is characterized by a chronic non-specific inflammation of the
retroperitoneum, which may entrap and obstruct retroperitoneal
structures, particularly the ureters.
Patients with RPF show non-specific clinical
symptoms, including poorly localized back pain, general malaise,
weight loss, anemia, features of renal failure and occasionally,
mild fever (4–7). In addition, RPF is difficult to
detect. In the present case report, a patient that had been
suffering from abdominal pain and weight loss for three months was
primarily diagnosed with lumbar and back myofascitis. However,
traditional treatments had no effect on the patient, therefore, a
further examination was performed and a biopsy of the mass was
employed. Prednisone was administered to the patient and the
retroperitoneal mass decreased in size and finally disappeared.
Case report
A 36-year-old male was admitted to the Second
Xiangya Hospital, Central South University (Changsha, China) with a
3-month history of lower right abdominal pain (intermittent) and
weight loss (5 kg). The patient had no previous history of drug use
for specific medical conditions or lymphoma and no drug or food
allergies. A physical examination showed that the patient’s abdomen
was soft and flat with normal bowel sounds. No pain sensation was
detected in the bilateral renal area and the superficial lymph
nodes were not palpable. The patient’s fecal occult blood test
results were negative and the urinalysis result was normal. The
complete blood cell count showed normochromic normocytic anemia
with a hematocrit level of 32.2% (normal value, 37–51%). The blood
urea nitrogen level was 3.83 mmol/l (normal value, 2.9–7.14 mmol/l)
and the serum creatinine was 71.9 μmol/l (normal value,
40–133 μmol/l). The plasma β2-microglobulin level was 3.66
mg/l (normal value, 1–3 mg/l), the serum ferritin was 375.26 ng/ml
(normal value, 21.8–274.66 ng/ml) and the C-reactive protein was 72
mm/l (male, 0–15 mm/l). The human leucocyte antigen-B27 and
tuberculosis antigen analysis results were negative. The
antistreptolysin O test and rheumatoid factors were also negative.
The tumor marker levels, including those of carcinoembryonic
antigen (CEA), CA19-9, CA125, lactate dehydrogenase and
alpha-fetoprotein (AFP) were within normal ranges. The results of
the other biochemical screening and electrolyte tests were all
within normal limits. An infrared thermal imaging examination
showed lumbar and back myofascitis. Abdominal ultrasonography,
gastrointestinal endoscopy and colonoscopy showed no noteworthy
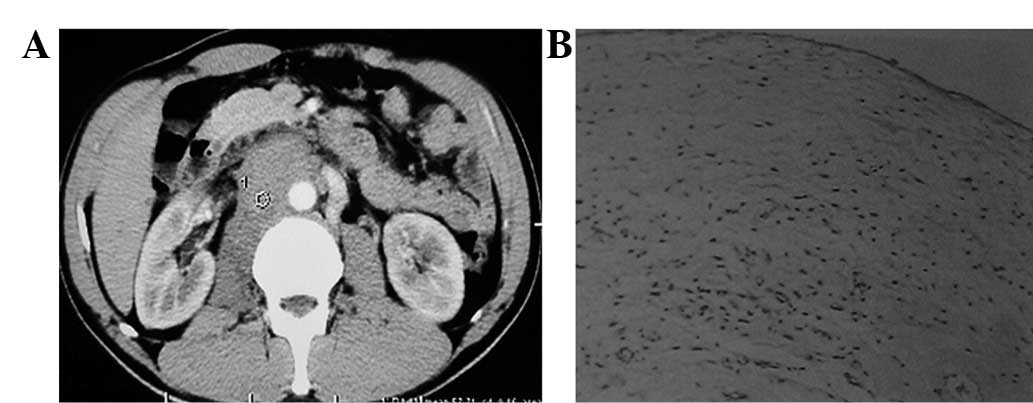
findings. A CT scan of the abdomen revealed a retroperitoneal mass
(∼7×2 cm) on the plane of the right renal vein (Fig. 1A) with no signs of hydronephrosis
or ureteral dilation. A retroperitoneal mass biopsy was then
performed laparoscopically. An adhesion was identified between the
right upper ureter and the inferior vena cava during the surgery.
The mass covered the surface of the abdominal aorta and the
inferior vena cava near the right renal hilum. Three shots with an
automated biopsy gun were employed to biopsy the mass. The results
showed that the biopsy specimen was made up of fiber and fat
tissues which were infiltrated by inflammatory cells (Fig. 1B).
The patient began taking prednisone one month
subsequent to the surgery at a dose of 10 mg, three times a day for
one month. The dose was reduced to 25 mg once each day after one
month and then reduced by 5 mg each day. A dose of 5 mg was
maintained lasting for approximately two months until August 2011
and then was reduced to 1 mg once each day for another month.
Therefore, in total, the prednisone was continuously taken by the
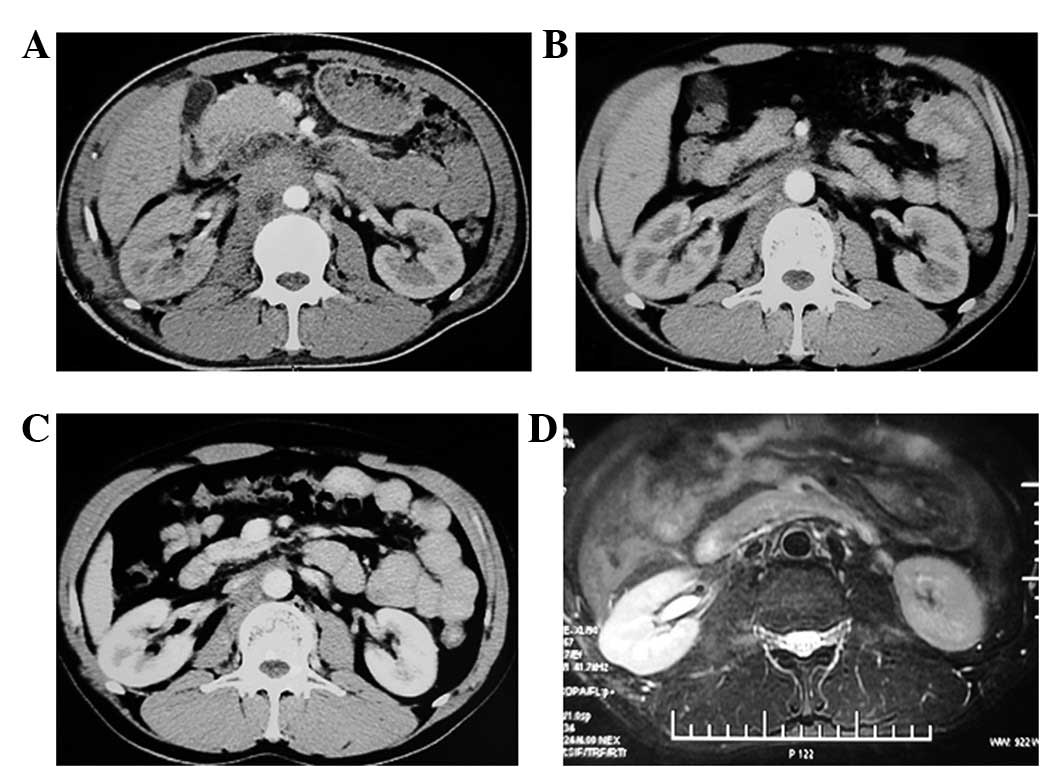
patient for 1 year. During this treatment, the patient underwent a
CT scan of the abdomen every three or six months. The images from
the CT scans showed that the retroperitoneal mass was decreasing in
size with the progression of the treatment (Fig. 2A, B and C). The mass had almost
disappeared on the final month’s MRI scan in August (Fig. 2D). Prior written and informed
consent were obtained from every patient and the study was approved
by the ethics review board of Central South University.
Discussion
RPF is a rare disease of unclear etiology; however,
the clinical manifestations are non-specific in the early stages of
its course. It is important for researchers to create enough
awareness of this disease. The lesions often begin with aortic
associations, gradually ending as associated with the aorta,
inferior vena cava and ureter and also involved with the mesenteric
and renal arteries (8). The
disease may cause obstructions of certain structures, including the
mesenteric artery, duodenal choledochal duct and inferior vena
cava.
Data accumulated from China reveal that RPF occurs
mainly in males in their fifties and sixties, with the
male-to-female ratio being ∼1.9:1 (9). The early symptoms are non-specific
and an accurate diagnosis is often achieved only subsequent to
urological obstruction or the occurrence of renal failure. The
majority of patients feel pain in the lower back, flank and/or
abdomen. These are the most obvious symptoms and the pain is dull
and non-colicky in the beginning, becoming more severe with the
progress of the disease. Other symptoms that are quite frequent
include weight loss, anorexia, nausea, vomiting, claudication,
ureteral colic and hematuria. Symptoms including fever, testicular
pain, abdominal angina, intermittent claudication, edema, scrotal
effusion and Raynaud’s syndrome are quite rare. Meanwhile, certain
symptoms, including various degrees of ureteral obstruction,
hydronephrosis and renal failure, are the earliest and most common
clinical manifestations. Although a number of scientific journals
devoted to RPF are present in the literature, there is no accepted
diagnostic or therapeutic strategy for this disease. However, there
are several therapeutic strategies which have been proven to be
effective. It is commonly noted in the literature that patients
with non-malignant RPF are treated primarily with steroids or with
a combination of azathioprine (2 mg/kg) and steroids (10–12).
In the present study, the patient’s physical
examination was normal, with the exception of the presence of back
pain. The mass was located on the plane of the right renal vein
with no signs of hydronephrosis or ureteral dilation on the CT
scan. The back pain became more serious with the progression of the
therapy. In addition, the aggravation of the pain was accompanied
with side effects, including vomiting and nausea. The mass was
observed to be closely adhered to the inferior vena cava during the
surgery and their separation was not possible. The results of the
biopsy showed that the specimen was made of fiber and fat tissues
infiltrated by inflammatory cells, therefore, a diagnosis of
malignancy or abscess was excluded. The biochemical tests on the
serum for conditions, including autoimmune system diseases and
lymphoma, were negative. Therefore, the patient was treated with
prednosione and the pain symptoms and the retroperitoneal mass
almost disappeared subsequent to one year of treatment. Afterwards,
a diagnosis of early stage retroperitoneal fibrosis was
established.
In conclusion, the diagnosis of retroperitoneal
fibrosis is an effective process that excludes the other diagnoses
for the lesion. A biopsy of the mass is a necessity for the final
stage of diagnosis and is supported by the response to the steroid
treatment. CT scans or MRI are effective examination tools, which
help researchers to diagnose and monitor the progress of the
disease.
References
|
1
|
Albarran J: Rétention rénale par
périurétérite. Libération externe de l’uretère. Assoc Fr Urol.
9:511–517. 1905.
|
|
2
|
Ghanaati H, Mohammadifar M, Ghajarzadeh M,
et al: The role of multidetector CT in the diagnosis of
retroperitoneal fibrosis: report of a case. Iran J Radiol. 9:28–31.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Yokoyama R, Tazaki R, Morita H, et al:
Retroperitoneal fibrosis in a patient with gastric cancer
manifested by lower extremity edema and hydrocele. Intern Med.
51:2157–2160. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Gilkeson GS and Allen NB: Retroperitoneal
fibrosis. A true connective tissue disease. Rheum Dis Clin North
Am. 22:23–38. 1996.PubMed/NCBI
|
|
5
|
Buff DD, Bogin MB and Faltz LL:
Retroperitoneal fibrosis. A report of selected cases and a review
of the literature. NY State J Med. 89:511–516. 1989.PubMed/NCBI
|
|
6
|
van Bommel EF, van Spengler J, van der
Hoven B and Kramer P: Retroperitoneal fibrosis: report of 12 cases
and a review of the literature. Neth J Med. 39:338–345.
1991.PubMed/NCBI
|
|
7
|
Lepor H and Walsh PC: Idiopathic
retroperitoneal fibrosis. J Urol. 122:1–6. 1979.
|
|
8
|
Stone JR: Aortitis, periaortitis, and
retroperitoneal fibrosis, as manifestations of IgG4-related
systemic disease. Curr Opin Rheumatol. 23:88–94. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
An LM, Xu YF and Zhang ZL: Clinical
features and prognostic analysis of retroperitoneal fibrosis in 32
patients. Beijing Da Xue Xue Bao. 44:265–269. 2012.(In
Chinese).
|
|
10
|
Husband P and Knudsen A: Idiopathic
cervical and retroperitoneal fibrosis: report of a case treated
with steroids. Postgrad Med J. 52:788–793. 1976. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Dedeoglu F, Rose CD, Athreya BH, et al:
Successful treatment of retroperitoneal fibrosis with tamoxifen in
a child. J Rheum. 28:1693–1695. 2001.PubMed/NCBI
|
|
12
|
van Bommel EF: Retroperitoneal fibrosis.
Neth J Med. 60:231–242. 2002.
|