Introduction
Ectopic thyroid tissue, defined as thyroid tissue
not located anterior-laterally to the second and fourth tracheal
cartilages, is rare. It is a congenital disease caused by the
abnormal migration of thyroid tissue in the embryonic stage
(1). In the majority of cases,
ectopic thyroid is located in the midline, between the foramen
caecum and the normal location of the thyroid gland, and most often
it is located in the base of the tongue (2,3).
Patients usually present with symptoms, including a palpable but
asymptomatic neck mass, dysphagia, dysphonia or dyspnea, according
to the location and size of the mass. In the majority of cases,
ectopic thyroid is the only thyroid tissue present (1). The current report describes a rare
case: a 36-year-old female patient presented a non-functional
ectopic thyroid tissue in the lower neck with a coexisting normal
thyroid, which is infrequent in the clinic. The present study was
approved by the ethics committee of Tianjin Medical University
General Hospital (Tianjin, China) and adhered to the tenets of the
Declaration of Helsinki. In addition, the written informed consent
was obtained from the patient.
Case report
A 36-year-old female presented with a recent onset
of a painless mass in the middle of the lower neck. The patient was
asymptomatic and there was nothing significant in the medical
history. Physical examination revealed a ∼4 cm immobile, non-tender
mass in the patient’s lower neck. Thyroid function tests, as well
as the thyroglobulin (Tg) and thyroglobulin antibody (TgAb) levels
of the patient were normal: free triiodothyronine (FT3),
4.65 pmol/l (normal range, 3.5–6.5 pmol/l); free thyroxine
(FT4), 18.52 pmol/l (normal range, 11.5–23.5 pmol/l);
sensitive thyroid stimulating hormone (sTSH), 1.38 μIU/ml
(normal range, 0.3–5.0 μIU/ml); Tg, <0.20 ng/ml (normal
range, 0–55 ng/ml); and TgAb, 26 IU/ml (normal range, 0–40 IU/ml).
Thyroid hormones and TSH were determined with an immunofluorometric
assay. Tg and TgAb were measured with a radioimmunoassay. Blood
serum calcitonin, calcium and parathyroid hormone (PTH) levels were
normal. A neck ultrasound revealed a normal thyroid gland and a
solid mass of heterogeneous echotexture in the middle lower
cervical area, measuring 5.1 × 2.8 cm. The patient refused a fine
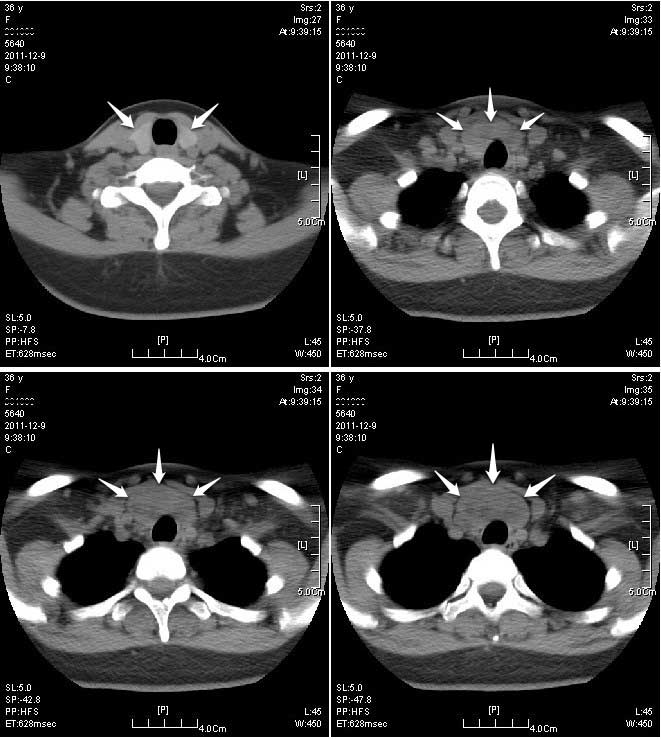
needle aspiration (FNA) biopsy. A computed tomography (CT) scan of
the neck revealed a well-defined mass below the thyroid gland, at
the border of the cervical region and the thorax (Fig. 1). The mass suppressed the trachea;
however, it was not causing narrowing of the trachea.
99mTcO4− scintigraphy of the
patient’s neck revealed only the normal thyroid gland; the cervical
mass did not show any uptake of
99mTcO4− (Fig. 2).
The patient underwent en bloc resection, in which
the cervical mass was identified as a separate structure from the
thyroid gland. The patient had an uneventful postoperative
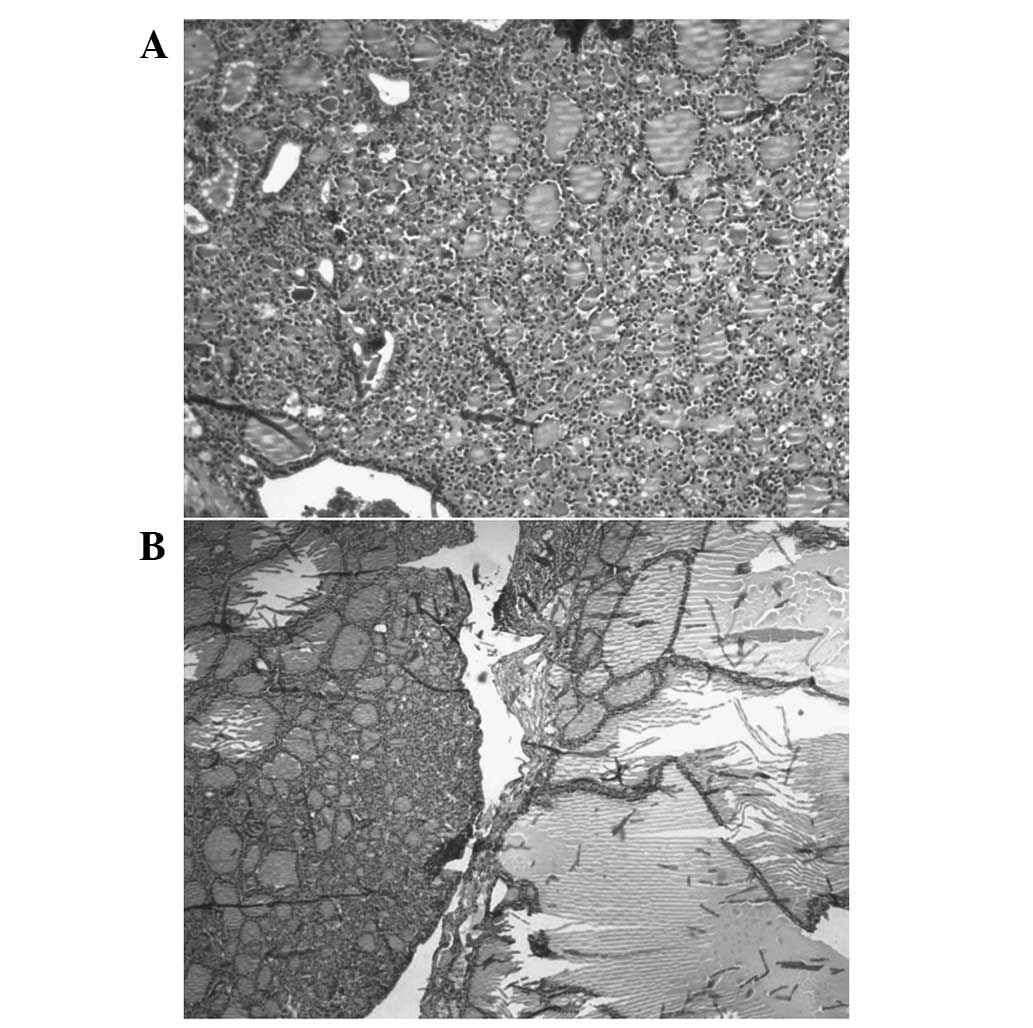
recovery. Histological examination revealed that it showed large
follicular cells of thyroid tissue distended with colloid material
which confirms the characteristic of adenomatous hyperplasia
(Fig. 3). Postoperatively the
patient was euthyroid and had normal calcium levels.
Discussion
Ectopic thyroid tissue, defined as thyroid tissue
not located anterior-laterally to the second and fourth tracheal
cartilages, is rare. It was first described by Hickman in 1869 in a
newborn baby who suffocated 16 h after birth due to a lingual
thyroid causing upper airway obstruction (4,5,6). It
is a congenital disease caused by abnormal migration of thyroid
tissue in the embryonic stage. During embryogenesis, the descent of
the thyroid does not proceed normally, leading to various possible
anomalous locations of the gland. According to the timing of the
embryonic development, thyroid descent may stop at various sites,
from the base of the tongue to any site of the thyroglossal duct
(3). In the majority of cases it
is located in the midline, between the foramen caecum and the
proper location of the thyroid gland, and most often it is located
in the base of the tongue (2,3). In
the current study, a rare case of a non-functioning ectopic thyroid
in the lower cervical area in a female patient with a normal
thyroid gland is presented.
Lingual thyroid is the most common form of ectopic
thyroid (7), which may cause
dysphonia (8). Extralingual
thyroid tissue is commonly located in the anterior cervical area,
along the path of the thyroglossal duct (3). In the patient in the present study it
was located underneath the thyroid in the lower neck, which is a
rare location. Other rare locations of ectopic thyroid include the
submandibular region (9), parotid
salivary gland (10), trachea
(11), lateral to the carotid
arteries and jugular veins (7),
mediastinum (12), heart (13), lung (14), duodenum (15), adrenal gland (16) and uterus (17).
The exact incidence of ectopic thyroid is unknown.
Post-mortem studies suggest that asymptomatic thyroid tissue may be
located along the path of the thyroglossal duct in as many as 7–10%
of adults (18). Ectopic thyroid
tissue may be the only functioning tissue (3,19,20)
or may coexist with a normal thyroid gland (9,21,22),
as in the present case.
Radionuclide imaging (RI) is considered the
definitive diagnostic test method for detecting ectopic thyroid
tissue. In the present case, no uptake of radiotracer was observed
in the ectopic thyroid. In a previous study, the findings on color
Doppler ultrasonography (CDU), gray-scale ultrasonography (GSU) and
magnetic resonance imaging (MRI) were compared with those of RI and
the sensitivities for detecting ectopic thyroid were calculated
(23). In the patients with
ectopic thyroid, the sensitivity of CDU, GSU and MRI for detecting
ectopic thyroid was 90, 70 and 70%, respectively. CDU is superior
to GSU and MRI for detecting ectopic thyroid.
Ectopic thyroid tissue may undergo the same
pathological changes as the eutopic thyroid gland, including
thyrotoxicosis (19), and may be
benign or malignant (11,12,24).
Malignant transformation of ectopic thyroid tissue is extremely
uncommon. If, however, thyroid tissue is located in the lateral
cervical lymph nodes, metastasis of a malignant thyroid tumor
should be excluded (25).
Ectopic thyroid tissue poses difficult diagnostic
and management challenges. The treatment of ectopic thyroid tissue
depends on factors such as mass size, local symptoms, the age of
the patient, the functional status of the thyroid gland and
complications, including ulceration, hemorrhage and neoplasia
(26,27). In order to prevent misdiagnosis and
mismanagement, patients with a cervical mass in the anterior
midline should be subjected to history screening, physical
examination, cervical CDU, RI, thyroid function examinations (TSH,
FT3 and FT4), FNA biopsy and histological
examinations during surgery (23).
References
|
1.
|
Noussios G, Anagnostis P, Goulis DG,
Lappas D and Natsis K: Ectopic thyroid tissue: anatomical,
clinical, and surgical implications of a rare entity. Eur J
Endocrinol. 165:375–382. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Damiano A, Glickman AB, Rubin JS and Cohen
AF: Ectopic thyroid tissue presenting as a midline neck mass. Int J
Pediatr Otorhinolaryngol. 34:141–148. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Larochelle D, Arcand P, Belzile M and
Gagnon NB: Ectopic thyroid tissue - a review of the literature. J
Otolaryngol. 8:523–530. 1979.PubMed/NCBI
|
|
4.
|
Kumar Choudhury B, Kaimal Saikia U, Sarma
D, et al: Dual ectopic thyroid with normally located thyroid: a
case report. J Thyroid Res. 2011:1597032011.PubMed/NCBI
|
|
5.
|
Bersaneti JA, Silva RD, Ramos RR,
Matsushita Mde M and Souto LR: Ectopic thyroid presenting as a
submandibular mass. Head Neck Pathol. 5:63–66. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Kumar Choudhury B, Kaimal Saikia U, Sarma
D, et al: Dual ectopic thyroid with normally located thyroid: a
case report. J Thyroid Res. 2011:1597032011.PubMed/NCBI
|
|
7.
|
Batsakis JG, El-Naggar AK and Luna MA:
Thyroid gland ectopias. Ann Otol Rhinol Laryngol. 105:996–1000.
1996. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Stoppa-Vaucher S, Lapointe A, Turpin S,
Rydlewski C, Vassart G and Deladoëy J: Ectopic thyroid gland
causing dysphonia: imaging and molecular studies. J Clin Endocrinol
Metab. 95:4509–4510. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Feller KU, Mavros A and Gaertner HJ:
Ectopic submandibular thyroid tissue with a coexisting active and
normally located thyroid gland: case report and review of
literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod.
90:618–623. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Mysorekar VV, Dandekar CP and Sreevathsa
MR: Ectopic thyroid tissue in the parotid salivary gland. Singapore
Med J. 45:437–438. 2004.PubMed/NCBI
|
|
11.
|
Hari CK, Brown MJ and Thompson I: Tall
cell variant of papillary carcinoma arising from ectopic thyroid
tissue in the trachea. J Laryngol Otol. 113:183–185.
1999.PubMed/NCBI
|
|
12.
|
Sand J, Pehkonen E, Mattila J, Seppănen S
and Salmi J: Pulsating mass at the sternum: a primary carcinoma of
ectopic mediastinal thyroid. J Thorac Cardiovasc Surg. 112:833–835.
1996. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Casanova JB, Daly RC, Edwards BS, Tazelaar
HD and Thompson GB: Intracardiac ectopic thyroid. Ann Thorac Surg.
70:1694–1696. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Bando T, Genka K, Ishikawa K, Kuniyoshi M
and Kuda T: Ectopic intrapulmonary thyroid. Chest. 103:1278–1279.
1993. View Article : Google Scholar
|
|
15.
|
Takahashi T, Ishikura H, Kato H, Tanabe T
and Yoshiki T: Ectopic thyroid follicles in the submucosa of the
duodenum. Virchows Arch A Pathol Anat Histopathol. 418:547–550.
1991. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Shiraishi T, Imai H, Fukutome K, Watanabe
M and Yatani R: Ectopic thyroid in the adrenal gland. Hum Pathol.
30:105–108. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Yilmaz F, Uzunlar AK and Sögütçü N:
Ectopic thyroid tissue in the uterus. Acta Obstet Gynecol Scand.
84:201–202. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Sauk JJ Jr: Ectopic lingual thyroid. J
Pathol. 102:239–243. 1970. View Article : Google Scholar
|
|
19.
|
Kumar R, Gupta R, Bal CS, Khullar S and
Malhotra A: Thyrotoxicosis in a patient with submandibular thyroid.
Thyroid. 10:363–365. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
20.
|
Aguirre A, de la Piedra M, Ruiz R and
Portilla J: Ectopic thyroid tissue in the submandibular region.
Oral Surg Oral Med Oral Pathol. 71:73–76. 1991. View Article : Google Scholar
|
|
21.
|
Richards PS, Ahuja AT and King AD: Clinics
in diagnostic imaging (101): multinodular accessory thyroid tissue.
Singapore Med J. 45:542–546. 2004.PubMed/NCBI
|
|
22.
|
Mace AT, McLaughlin I, Gibson IW and Clark
LJ: Benign ectopic submandibular thyroid with a normotopic
multinodular goitre. J Laryngol Otol. 117:739–740. 2003.PubMed/NCBI
|
|
23.
|
Ohnishi H, Sato H, Noda H, Inomata H and
Sasaki N: Color Doppler ultrasonography: diagnosis of ectopic
thyroid gland in patients with congenital hypothyroidism caused by
thyroid dysgenesis. J Clin Endocrinol Metab. 88:5145–5149. 2003.
View Article : Google Scholar
|
|
24.
|
Ling L, Zhou SH, Wang SQ and Wang LJ:
Misdiagnosed ectopic thyroid carcinoma: report of two cases. Chin
Med J (Engl). 117:1588–1589. 2004.PubMed/NCBI
|
|
25.
|
Kousta E, Konstantinidis K, Michalakis C,
et al: Ectopic thyroid tissue in the lower neck with a coexisting
normally located multi-nodular goiter and brief literature review.
Hormones (Athens). 4:231–234. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
26.
|
Nasiru Akanmu I and Mobolaji Adewale O:
Lateral cervical ectopic thyroid masses with eutopic multinodular
goiter: an unusual presentation. Hormones (Athens). 8:150–153.
2009.PubMed/NCBI
|
|
27.
|
Abellán Galiana P, Cámara Gómez R, Campos
Alborg V, Rivas Sánchez A, Salom Fuster JV and Muñoz Gómez C: Dual
ectopic thyroid: subclinical hypothyroidism after extirpation of a
submaxillary mass. Rev Esp Med Nucl. 28:26–29. 2009.(In
Spanish).
|