Introduction
In order to reconstruct small- or medium-sized soft
tissue defects following lesion excision, there are a number of
operative approaches available to plastic surgeons. These include
skin graft, local flap and free-tissue transfer procedures
(1–3). These techniques often make use of
tissues from a donor site to meet the reconstructive requirements
of the recipient site. Soft-tissue expansion techniques generate
extra skin tissue from donor sites adjacent to the lesion with
similar characteristics to the damaged skin; for example,
appropriate color match, fine texture, sensibility and substantial
adnexa to aesthetically restore the resulting defect. To obtain
extra skin tissue via soft-tissue expansion, one or more temporary
expanders are implanted under the skin. The expanders are capable
of accumulating saline solution via injection through a gel-filled
valve system in the reservoir dome. The internal pressure of the
expander exerts force on the soft tissue of the donor site, which
gradually expands, providing additional tissue for the recipient
area while the donor site remains preserved. Temporary expanders
are available in different sizes and shapes, depending on the
clinical reconstructive requirements. This expansion technique
safely and effectively enhances methods used in plastic surgery.
Plastic surgeons have a number of common preferences regarding the
placement positions and levels of soft-tissue expanders, and have
also investigated methods to prevent complications of this
technique (4–6). Models for estimating the expanded
soft tissue during the expansion process have been created
(7,8). However, certain inevitable
consequences, including visible scars and, in particular,
additional incision scars, dissatisfy patients. Although additional
incisions are unavoidable when unfurling hemispheric expanded flaps
and correcting ‘dog-ear’ deformities, reducing the scar burden as
much as possible via the use of expanded flaps is essential,
particularly in exposed areas, including the face and neck. In
addition, shortening the treatment time to reduce the cost of
treatment is also important. The shortcomings of the tissue
expansion technique, including the production of additional
incision scars, prolonged expansion time and high rates of
complication, limit its use in the treatment of small defects of
the face, neck and limbs that may not be excised and sutured
directly in one procedure. In order to solve these problems,
certain improvements have been gradually applied and achieved
during clinical experience. In the present study, tissue expanders
were implanted under the lesions, using the lesions as the center
and fully expanding the surrounding normal tissue, so as to reduce
the relative size of the lesions. This method has been named the
‘expansion in-situ’ technique. It not only reduces the
length of additional incisions and the number of tissue expanders
used, but it also shortens the expansion period. The expanded skin
tissue surrounds the lesion in all directions and is fully utilized
so that closure of the defect by direct suturing may be performed
without tension. In the present study, the expansion in-situ
technique was applied in 10 cases to repair small- and medium-sized
soft-tissue defects, which it was not possible to suture directly.
Successful results were achieved within a shorter period of time
than traditional expansion techniques.
Materials and methods
Patients
Between August 2006 and December 2011, the expansion
in-situ technique was applied to 10 patients (4 females and
6 males) in order to reconstruct soft tissue defects resulting from
nevi (n=5) and scar excisions (n=5) located on the face and upper
limbs. The largest defect was 15×7.5 cm, resulting from a facial
scar excision. The smallest defect was 3×2.5 cm, resulting from
removal of a nevus on the limb. The remaining 8 cases comprised of
4 cases of cicatrices (2 face and 2 upper limb) and 4 cases of nevi
(1 face and 3 upper limb). The age range of the patients was 12–30
years (mean, 21.3 years). The volume of the tissue expanders was
50–400 ml depending on the size and characteristics of the defect.
The duration of tissue expander inflation ranged from 6 to 10 weeks
(mean, 8 weeks; Table I). This
study was conducted in accordance with the Declaration of Helsinki
and with approval from the Ethics Committee of the Chinese Academy
of Medical Sciences (Beijing, China). Written informed consent was
obtained from all participants.
 | Table I.Summary of patient
characteristics. |
Table I.
Summary of patient
characteristics.
| Case no. | Age (years) | Gender | Defect size (cm) | Cause | Expander volume
(ml) | Inflation time
(weeks) | Complications | Follow-up time
(months) |
|---|
| 1 | 16 | F | 3.0×2.5 | Facial nevus | 50 | 7 | None | 12 |
| 2 | 22 | F | 7.0×3.0 | Facial scar | 200 | 8 | Poor incision
healing | 12 |
| 3 | 12 | M | 10.0×6.0 | Upper limb nevus | 300 | 10 | None | 12 |
| 4 | 27 | F | 3.0×2.5 | Facial nevus | 50 | 7 | None | 24 |
| 5 | 17 | M | 15.0×7.5 | Facial scar | 400 and 100 | 9 | None | 36 |
| 6 | 19 | M | 9.0×6.5 | Upper limb nevus | 200 | 8 | None | None |
| 7 | 17 | M | 9.0×5.0 | Upper limb nevus | 200 | 9 | None | None |
| 8 | 24 | M | 7.5×3.0 | Upper limb scar | 80 | 7 | None | None |
| 9 | 30 | F | 6.0×3.0 | Facial scar | 100 | 8 | None | None |
| 10 | 29 | M | 7.0×3.0 | Upper limb scar | 100 | 6 | None | None |
Surgical techniques
The first stage of the surgery involved the
insertion of a tissue expander and its serial expansion. The
operative design used the lesion as the center mark for a rhombic
incision line, the length and width of which did not exceed the
size of the lesion. With the patient under anesthesia, the
superficial tissue in the marked rhombic area was excised. A pocket
was created subcutaneously or to the level of the deep fascia. It
was necessary to ensure good hemostasis in the expander pocket. An
optimally sized rectangular tissue expander was placed into the
pocket and a drainage tube was placed beneath the expander
simultaneously. The injection port was placed so as to facilitate
inflation of the tissue expander. Overlapping suturing of the
de-epithelialized dermal flaps on both sides of the incision was
conducted. A pressure dressing was applied to the operative area.
From 10 days after surgery, the expander was serially inflated with
saline solution on a weekly basis until an adequate volume was
achieved. The expander was removed in the second stage of the
surgery when an adequate volume was achieved and sufficient stable
skin had been generated. The lesion was excised and the incision
was sutured directly during this surgery. If the incision was too
long, an ‘S-shaped’ suture was created. A drainage tube was placed
intraoperatively and removed 3–5 days after the operation.
Following a day of observation, the patient was able to be
discharged. The suture was removed at 10–12 days
postoperatively.
Results
A total of 10 cases were completed, including
complete nevus resection and scar removal. The average time
required for tissue expansion was 8 weeks. Necrosis of the skin
flaps did not occur. All wounds were closed directly, with the
exception of one case of poor wound healing. In this case, the
wound finally healed well after a careful dressing change. There
were no cases of infection, wound dehiscence or other
complications. A follow-up survey was returned by five respondents
who agreed to attend a check-up. The average follow-up period was
19.2 months. No hyperplasia of incision scars or relapse of lesions
was reported and all the patients who were followed up were
satisfied with their final reconstructive and aesthetic
outcomes.
Typical cases
Case 1
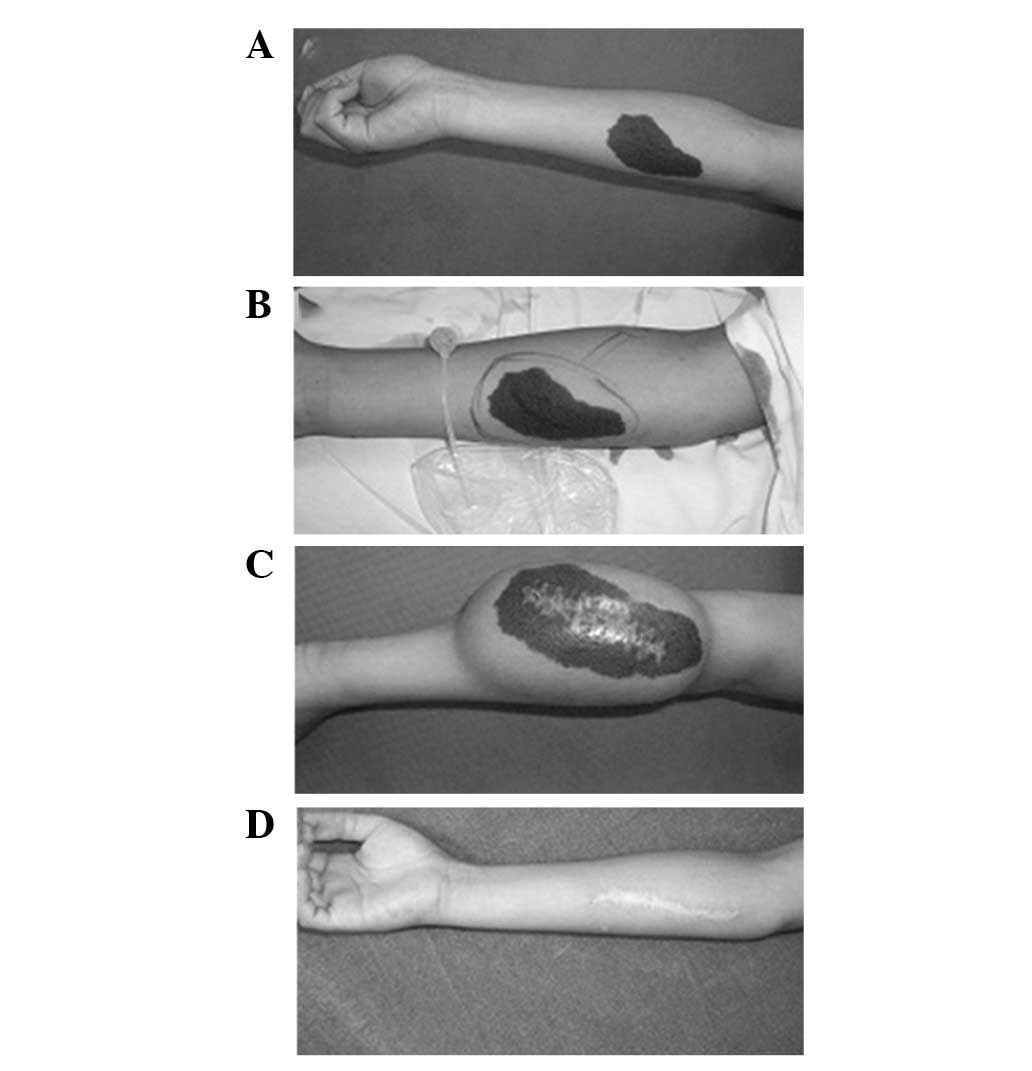
A 16-year-old female patient presented with a giant
nevus. The conventional approach to treatment would be the
implantation of an expander in the buccal or temporal regions. This
approach is likely to have involved excessively long additional
incisions and visible ‘dog-ear’ deformities. An alternative
approach is the use of an expanded forehead flap based on the
superficial temporal vessel or an expanded medial arm flap.
However, these approaches would take a long time and may have led
to obvious donor site morbidities. Instead, a 50-ml rectangular
tissue expander was implanted under the nevus and its circumambient
normal skin. Partial epidermal removal of the nevus and overlapping
suturing of the remaining dermal flaps was conducted to ensure
smooth healing of the incision. After 7 weeks of inflation with
saline, the nevus was excised with the 3.0×2.5 cm defect and the
expanded flaps were transferred and sutured directly without
additional incisions. After one year of follow-up, the patient was
satisfied with the results (Fig.
1).
Case 3
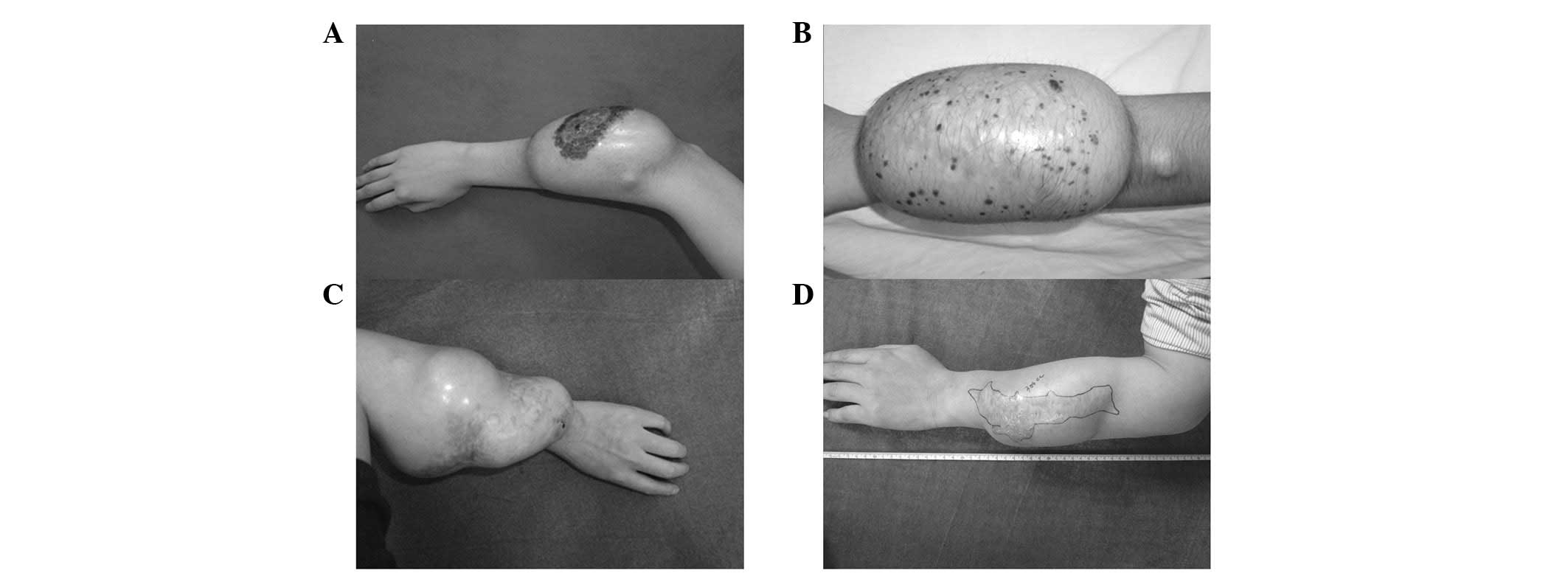
A 12-year-old male presented with a congenital nevus
on the right forearm. The nevus was 10.0×6.0 cm in size.
Reconstruction using an autologous skin graft to repair the defect
after nevus excision may have led to a difference in the texture
and color of the skin in the recipient area. The patient also was
unable to accept resection more than once. Traditional expansion
techniques would have involved placing expanders under both sides
of the nevus. These approaches are of low efficiency since it is
not possible to apply the expanded flap effectively in the transfer
process. The resulting wound with additional incision also
discomforted. Therefore, the incision was performed inside the
nevus and part of the nevus was excised. Overlapping suturing of
the dermal tissue was conducted in order to ensure smooth healing
of the incision. A 300 ml rectangular tissue expander was implanted
under the nevus and surrounding normal skin area. The expander was
inflated for 10 weeks. In a second-stage procedure, the nevus was
resected completely with only a short incision. One year later,
there was no relapse and the scar was acceptable (Fig. 2).
Case 5
A 17-year-old female presented with a rectangular
left facial scar between the temporal and buccal region that was
caused by a scald injury in childhood. The scar was 15×7.5 cm in
size. The areas of normal skin at the sides of the scar were not
sufficient for tissue expansion and transfer. Thus, an incision was
performed inside the rectangular scar and two rectangular expanders
were implanted under the cicatricial area and ambient normal skin.
To ensure smooth healing of the incision, overlapping suturing of
the dermal tissue was conducted. After 9 weeks of expander
inflation, the facial scar was completely removed and the expanded
flap was transferred to the center of the defect. More than three
years after surgery, the incision scar was no longer evident and
the patient was satisfied with the resulting appearance (Fig. 3).
Case 9
A 30-year-old female patient presented with a left
facial scar caused by a burn in childhood. The scar was 6.0×3.0 cm.
A 100-ml expander was implanted under the scar and overlapping
suturing of the incision was conducted. The expanded flap was
transferred to the center of the defect and the facial scar was
completely removed after 8 weeks of expander inflation (Fig. 4).
Discussion
The soft-tissue expansion technique was first
reported in 1957 in a study by Neumann (9) in which a rubber balloon with an
external port was used to reconstruct a traumatic ear defect. Since
Radovan (10) reported breast
reconstruction using tissue expansion in 1982, the clinical
applications of soft-tissue expansion techniques have been
continuously developed and used increasingly on a number of regions
of the body. Traditional soft-tissue expansion methods use an
expander that is gradually filled with saline to expand the
overlying skin immediately adjacent to a wound. As this technique
has been developed, the expander materials and application of the
method have undergone various improvements (11–15).
Currently, there are a wide array of expanders of different shapes
and sizes that have been developed to maximize the volume of tissue
expansion in any given anatomical location (16–18).
Innovations, including the use of increasing numbers of tissue
expanders and repeated expansion in the same region, have been
achieved in difficult clinical situations (19–21).
Thus, tissue expansion techniques are becoming an extremely
important tool for plastic surgeons. Despite a number of benefits
of tissue expansion in the reconstruction of large and complex
soft-tissue defects, there are several significant problems that
limit its clinical applicability. The drawbacks of traditional
expansion techniques involve low utility rates of the expanded
flap, additional incisions during flap transfer, prolonged
expansion periods and high complication rates (4). These shortcomings are even more
significant in the treatment of small defects of the face, neck and
limbs that it is not possible to excise directly and suture in one
procedure or via serial excision. Effective methods to repair these
defects using tissue expansion techniques are not available. To
solve these problems, certain improvements have been gradually
applied and achieved during clinical situations.
Cai et al (22) were the first to report expansion
under the cicatrix and the utilization rate and flexibility to
transfer the expanded flap were shown to be increased. However,
expansion was performed under the cicatrix only and the vertical
incision made to implant the expander was in the normal area
surrounding the cicatrix. In the present study, the tissue expander
was implanted under the lesions besides the cicatrix (Fig. 5) and the dermal flaps created
following the de-epithelialization of the lesion on both sides of
the wound by insertion of the expander were closed by overlapping
suturing. This method is named ‘expansion in-situ’. This
technique used the lesion as the center and fully expanded the
surrounding normal skin, so as to reduce the relative size of the
lesion. In a two-stage operation, lesions were excised and the
expanded flaps surrounding the defects were transferred to the
center in order to close the wound directly without a great amount
of tension. The flexibility of the expanded flap allowed an
‘S-shaped’ suture to be created. No additional incisions were made
and no donor site morbidities occurred.
A number of techniques have also been devised in
attempts to close the incision created for implantation of the
expander (22). The overlapping
suture aids the effective healing of dermal tissue and avoids wound
dehiscence during the expansion period. The overlapping suture aids
the effective healing of dermal tissue and avoids wound dehiscence
during the expansion period. A partial subcutaneous scar may form
in the overlapping area. The expansion capacity of cicatricial
tissue is lower than that of the surrounding normal skin tissue.
Hence, during expander inflation, the augmentation of surrounding
normal skin tissue is greater than that of the overlapping section
of lesions with the same expansion pressure. As a result, there is
an expansion of normal skin tissue and relative reduction of the
lesion area.
This method is not suitable for all lesions,
including large lesions that it is not possible to resect via
one-time expansion, lesions without sufficient surrounding normal
skin tissue to implant an expander and lesions with a tendency for
implantation metastasis. The method is more suitable for small- or
medium-sized lesions that cannot be excised and sutured directly in
a one-stage procedure or via serial excision. The expanded normal
skin tissue that surrounds the lesion in all directions is fully
utilized and allows closure of the defect by direct suturing
without any tension. However, this technique may be combined with
traditional expansion techniques in order to repair larger defects.
The size of lesions suitable for resection using this method and
the maximum bearing force of the overlapping suture area remain to
be determined. Further studies are required to determine these
factors. However, if these problems are solved, this technique is
likely to be used more frequently in the future.
In conclusion, this method is suitable for repairing
small- or medium-sized defects with normal surrounding skin tissue.
It does not increase the risk of complications or the difficulty of
surgery. Compared with traditional expansion techniques, the
expansion in-situ technique implants an expander under the
lesion, reducing the number of expanders required, the damaged
caused and the treatment duration. This novel approach to expansion
markedly improves the clinical usefulness of the expanded flap
without the requirement for additional incisions or a risk of
compromising the blood supply to the extended flaps. Certain
factors, including the size of defects that it is possible to
reconstruct using this method and the bearing force of the
overlapping-suture area on the expansion, remain to be
investigated.
References
|
1.
|
Heller L, Cole P and Kaufman Y: Cheek
reconstruction: current concepts in managing facial soft tissue
loss. Semin Plast Surg. 22:294–305. 2008. View Article : Google Scholar
|
|
2.
|
Kuehnemund M and Bootz F: Reconstruction
of the Cheek. Facial Plast Surg. 27:284–290. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Gajiwala KJ: Biaxial serial excision: A
technique to deal with benign skin lesions and scars. Indian J
Plast Surg. 45:522–525. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Huang X, Qu X and Li Q: Risk factors for
complications of tissue expansion: a 20-year systematic review and
meta-analysis. Plast Reconstr Surg. 128:787–797. 2011.PubMed/NCBI
|
|
5.
|
Khalatbari B and Bakhshaeekia A: Ten-year
experience in face and neck unit reconstruction using tissue
expanders. Burns. 39:522–527. 2013.PubMed/NCBI
|
|
6.
|
Bauer BS and Margulis A: The expanded
transposition flap: shifting paradigms based on experience gained
from two decades of pediatric tissue expansion. Plast Reconstr
Surg. 114:98–106. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Duits EH, Molenaar J and van Rappard JH:
The modeling of skin expanders. Plast Reconstr Surg. 83:362–367.
1989. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Shively RE: Skin-expander volume
estimator. Plast Reconstr Surg. 77:482–483. 1986.PubMed/NCBI
|
|
9.
|
Neumann CG: The expansion of an area of
skin by progressive distension of a subcutaneous balloon; use of
the method for securing skin for subtotal reconstruction of the
ear. Plast Reconstr Surg. 19:124–130. 1957. View Article : Google Scholar
|
|
10.
|
Radovan C: Breast reconstruction after
mastectomy using the temporary expander. Plast Reconstr Surg.
69:195–208. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Iconomou TG, Michelow BJ and Zuker RM:
Tissue expansion in the pediatric patient. Ann Plast Surg.
31:134–140. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Pisarski GP, Mertens D, Warden GD and
Neale HW: Tissue expander complications in the pediatric burn
patient. Plast Reconstr Surg. 102:1008–1012. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Librero J, Marín M, Peiró S and Munujos
AV: Exploring the impact of complications on length of stay in
major surgery diagnosis-related groups. Int J Qual Health Care.
16:51–57. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Bauer BS, Vicari FA and Richard ME: The
role of tissue expansion in pediatric plastic surgery. Clin Plast
Surg. 17:101–112. 1990.PubMed/NCBI
|
|
15.
|
Egeland BM and Cederna PS: A minimally
invasive approach to the placement of tissue expanders. Semin Plast
Surg. 22:9–17. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Fan J and Wang J: The “silicone suture”
for tissue expansion without an expander: A new device for repair
of soft-tissue defects after burns. Plast Reconstr Surg.
114:484–488. 2004.
|
|
17.
|
Fan J, Eriksson M and Nordström RE:
External device for tissue expansion: Clinical evaluation of the
skin extender. Scand J Plast Reconstr Surg Hand Surg. 30:215–220.
1996. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Fan J: Tissue expansion of a tube flap
during the last transferring stage in reconstructions of the face
and neck. Scand J Plast Reconstr Surg Hand Surg. 32:229–232. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Liu Y, Zang M, Song B, et al: The ‘buddy
flap’ concept of soft-tissue-defect reconstruction. J Plast
Reconstr Aesthet Surg. 64:1475–1482. 2011.
|
|
20.
|
Roposch A, Steinwender G and Linhart WE:
Implantation of a soft-tissue expander before operation for club
foot in children. J Bone Joint Surg Br. 81:398–401. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
21.
|
Huo R, Yang W, Shangbin L, et al: A
microscopic and biomechanical study of skin and soft tissue after
repeated expansion. Dermatol Surg. 35:72–79. 2009.PubMed/NCBI
|
|
22.
|
Cai GB, Liu L, Li TY, Zhang Y and Wang CM:
Tissue expansion under the cicatrix. Zhonghua Zheng Xing Wai Ke Za
Zhi. 21:348–350. 2005.(In Chinese).
|