Introduction
Complex fractures of the tibial plateau commonly
occur in patients following high-energy trauma, typically
accompanied by severe damage to the knee articulation and the
surrounding tissues. The diagnosis and treatment of complex tibial
plateau fractures remains a significant challenge in orthopedic
trauma (1,2). In the past, normal X-ray films were
applied in the Schatzker classification of tibial plateau
fractures; however, the information provided by the normal films is
limited and does not satisfactorily assist clinical orthopedic
physicians in the diagnosis and treatment process. In the present
study, images from X-ray films, multidetector-row computed
tomography (MDCT) and magnetic resonance imaging (MRI) were
systematically analyzed and various indices, such as fracture
location, displacement degree, degree of comminution and degree of
joint surface collapse were analyzed. The ability to identify
injuries to the menisci of the knee joint and cruciate and
collateral ligaments, as well as insidious fractures,
preoperatively to enable a precise diagnosis and the appropriate
surgical treatment was evaluated. A total of 71 patients with
complex fractures of the tibial plateau who were admitted to
hospital from March 2004 to January 2009 were included in the study
and their treatment and its effects are reported.
Patients and methods
Clinical data
Over a 5-year period, from March 2004 to January
2009, 92 patients with complex fractures of the tibial plateau were
admitted to the 98th Hospital of PLA, Huzhou, China. Seventy-one of
the patients (43 males and 28 females; mean age, 34.7 years) were
systematically examined using X-ray, MDCT and MRI and underwent
surgical treatment. A total of 40 patients presented with left
tibial plateau fractures, while 31 patients presented with right
tibial plateau fractures. According to the Schatzker classification
(3), eight fractures were type
III, 36 were type V and the remaining fractures were type IV. The
causes of the fractures were as follows: 38 due to traffic
accidents; 15 due to falls from high places; 10 due to injury by
heavy objects and eight due to falls from bicycles or
battery-powered bikes. There were 14 patients with potentially
fatal injuries to the visceral organs and head, seven patients with
other fractures around the knee joint, 10 patients with injuries to
the anterior cruciate ligament, seven patients with injuries to the
posterior cruciate ligament, eight patients with injuries to the
collateral ligament, six patients with injuries to the menisci and
three patients with injuries to the genicular vascular nerves. The
patients were diagnosed and treated by the same group of
physicians. Patients that it was not possible to examine by MRI and
MDCT and those with injuries that were classified as Schatzker
types I, II and IV were not included in the study. The study was
approved by The Ethics Committee of The Medical Ethics Committee of
The 98th Hospital of People’s Liberation Army (Huzhou, China).
Informed consent was obtained from all included patients.
Examination methods and diagnosis
X-ray or computed radiography
(CR)
A 500 mA X-ray machine (Beijing Wandong Medical
Equipment Co., Ltd., Beijing, China) was utilized in the X-ray
examinations with a Lekai film, while an Agfa MD40 IP plate (Agfa
Healthcare NV, Mortsel, Belgium) was selected for use in the CR
examinations. The IP plate was scanned with a laser in the Agfa DC
Solo system, prior to the scanned image being presented to the
workstation to be handled. Following this, the film was printed
using a Kodak 8900 laser printer (Kodak, Rochester, NY, USA). The
anterior and lateral sides of the injured knee joint were
imaged.
Computed tomography (CT) scanning and
3D reconstruction
The patients’ injured knee joints were scanned by a
Siemens Symphony 16-row spiral CT scanner (Siemens AG, Erlangen,
Germany). The scanning slices were 5 mm deep, with slice intervals
of 3 mm. A 0.75 mm bone algorithm was adopted subsequent to
scanning, and multiplanar reconstruction (MPR) and observations of
the axial, sagittal and coronal positions were performed. The
reconstruction slices were 2–3 mm thick. The MPR images were
adjusted and analyzed by two highly qualified radiologists and two
highly qualified orthopedists subsequent to the images being
handled in the workstation. Multidirectional adjustment of the MPR
images was performed to show the cross section and the sagittal,
coronal and inclined planes (the inclined plane image was based on
the plane in which there was a 30º and 60º angle with the cross
section and the sagittal and coronal planes) of the target bones,
according to the bone structure. An any-angle inclined plane image
adjustment and curve imaging were applied to show the fractures if
necessary. The trend of the fracture line was tracked to define the
area affected by the fracture.
MRI examination
The patients’ injured knee joints were examined
using a Signa 1.5 T HD scanner (GE Healthcare, Waukesha, WI, USA),
while the patients lay straight and in a supine position. The feet
entered the scanner first and then the knees were turned outward by
10–15º. Rapid spinning echo and spectrum pre-saturated inverse
recovery sequences were used for the sagittal, coronal and axial
scanning. The scanning parameters were as follows: T1WI TR 500
msec, TE 17 msec; T2W1 TR 4,000 msec, TE 100 msec; BWI/SPIR
sequence: TR 3,000 msec, TE 10 msec; 4-mm-thick slices; slice
interval, 0.4 mm; scope, 150 ram; matrix, 256×512; stimulating
times, twice.
The appropriate treatment was determined according
to the patient’s condition and degree of limb turgidity, the
radioactive assessments (X-ray film, CT and MRI), the skill of the
surgeon and the patient’s medical history. Patients were treated
with plaster immobilization or calcaneus traction, with ice bags
for external application. The injured limb was elevated and
dehydrated, dexamethasone sodium phosphate was applied and any
bleeding was stopped. Potentially fatal trauma was treated first,
prior to the patient being treated with open reduction and
anatomical reduction when the condition of the patient was stable
and turgidity was apparent (5–14 days).
Double incision and single plate
This group comprised 24 patients in total (14 males
and 10 females; mean age, 33.6 years) and the average follow-up
period was 31.4 months. The incision was initiated at the superior
edge of the lateral tibia and extended to beneath the tibial
nodule. The length of the incision was ~15 cm. The skin,
subcutaneous tissues, deep fascia and the attachment point of the
muscle group were cut open successively, in order to expose the
lateral tibial platform. Following this, the coronal ligament was
cut open and the tibial articular surface was exposed. The tibial
medial plateau was reduced using Kirschner wire with the assistance
of C-shaped arm X-ray fluoroscopy. The L-shaped supporting plate,
golf plate or locking plate was subsequently placed and fixed on
the lateral tibia. Bone from the patient’s ilium or a bone
allograft was implanted if necessary. There were three patients
whose genicular medial collateral ligament was reduced using a
genicular medial incision.
Double incision and bilateral plates
This group comprised 21 patients in total (12 males
and nine females; mean age, 33.2 years) and the average follow-up
period was 28.4 months. On the basis of the genicular anterior
incision, two other incision were made in the posterior edge of the
medial plateau of the tibia, which were 12–15 cm long and >8 cm
wide. The skin, subcutaneous tissues and deep fascia were cut open
successively to the posterior edge of the medial tibial plateau.
Following this, the tibial medial plateau and the posterior edge
beneath the periosteum were peeled and exposed. Based on the
preoperative CR films, CT, MRI and degree of joint surface
collapse, the medial plateau was reset first, prior to the medial
plateau being taken as the mark to reset the lateral plateau
fracture and to fix the double plates with screws. Bone from the
patient’s ilium or a bone allograft was implanted according to the
condition of the patient. There were two patients whose collateral
ligaments were sewn up and restored, and one patient whose menisci
were excised.
Bilateral plates via genicular anterior
midline incision
This group comprised 26 patients in total (17 males
and nine females; mean age, 35.3 years) and the average follow-up
period was 23.6 months. The genicular anterior midline incision was
18–20 cm long and was initiated from a point 2 cm above the scutum,
prior to being extended to the central and upper crest of the
tibial diaphysis and then through the middle scutum, to terminate
at the tibial nodule. The skin, subcutaneous tissues and deep
fascia were cut open successively until the condyles were exposed
beneath the deep fascia. The surgical method was designed according
to the preoperative X-ray film, CT and MRI of the knee joint. The
genicular medial joint capsule was only cut open if the patient’s
medial joint surface had collapsed. The periosteum was peeled to
expose the broken side of the lateral tibial plateau. Then, after
conducting temporary fixation with Kirschner wire, the
reconstruction plates were fixed in place with screws, and the
muscle group in front of the tibia was then cut open with an
electric knife at the point of the lateral tibial plateau. The
broken side of the lateral tibial plateau was peeled and exposed
simultaneously. The meniscal coronal ligament was cut open and the
joint surface was reset in direct view. With regard to posterior
joint surface collapse, a tibial plateau bone knife was used for
vertical splitting, in order to expose the collapse site of the
joint surface. The surface was then impacted with a periosteal
peeling tool until the joint surface became flat, and bone from the
patient’s ilium or a bone allograft was implanted in the empty
sites. L-shaped supporting plates were placed and fixed with screws
once the fracture had been reset. There were 15 patients whose
cruciate ligaments were repaired with steel or absorbed wire. Three
patients had posterior cruciate ligament tibial avulsion fractures
and collapse fractures of the posterior tibial plateau, which were
repaired through an assistant incision behind the knee. There were
three patients whose collateral ligaments was sewn and repaired and
three patients whose menisci were excised. In addition, there were
two patients whose popliteal arteriovenous vessels were examined
and repaired using assistant incision behind the knee. One
patient’s peroneal nerve was examined and decompressed.
Indices and methods
Each patient’s X-ray, MDCT and MRI examination
images were examined and a quantitative statistical satisfaction
score, showing indices such as fracture location, degree of
fracture comminution, degree of fracture displacement and degree of
bone defect, was assigned. The standard of evaluation was based on
the imaging information, with scores as follows: 0 if the fracture
was not visible, 1 if the fracture was not clearly visible and 2 if
the fracture was clearly visible; 0 if the degree of fracture
comminution was not visible, 1 if the degree of fracture
comminution was visible but vague and 2 if the degree of fracture
comminution was clear; 0 if the degree of fracture displacement was
not visible, 1 if the degree of fracture displacement was visible
but unclear and 2 if the degree of fracture displacement was
clearly visible; 0 if the bone defect was not visible, 1 if the
bone defect was visible but unclear and 2 if the bone defect was
clearly visible. An assessment of 2 points was considered
‘satisfactory’, 1 point was considered ‘moderately satisfactory’
and 0 points was considered ‘unsatisfactory’. Statistical scores
were assigned for collapsed joint surfaces and injuries of the
cruciate ligament, menisci and collateral ligament using X-ray,
MDCT and MRI examinations, respectively.
Statistical methods
The data were processed and analyzed using SPSS
statistical software version 11.5 (SPSS, Inc., Chicago, IL, USA). A
metering method was used to evaluate fracture position and number
of cases, while single factor and 3-level variance analysis were
used when comparing the scores of the three groups. A Q-test
(Newman-Keuls method) was used when comparing two mean numbers and
a χ2 test was to compare every two of several sample
rates. P<0.05 was considered to indicate a statistically
significant difference.
Results
A total of 71 patients underwent X-ray (or CR), MDCT
and MRI examinations of injured knee joints in the present study.
The average follow-up period was 31.2 months, the average duration
of surgery was 1.9±0.4 h and the average bleeding volume was
446.5±107.9 ml. The infrapatellar branch of the saphenous nerve was
injured in one patient during the surgery and healing by first
intention of fracture was performed in 71 patients. One patient
recovered following a postponement. In the surgical treatment, bone
from the patient’s ilium was excised and fixed within 8 months
subsequent to the injury. The injury then typically recovered
without further complications within the following 10 months. Two
patients suffered from superficial and deep infections following
the surgery, one of which was skin ischemic necrosis combined with
soft tissue defects, bone and plate exposure and superficial
infection. This was treated by debriding the wound and covering the
retrograde island flap pedicled with the saphenous nerve nutrient
vessel. The other patient suffered from a deep infection of the
wound and acute pyogenic osteomyelitis. Following treatment with a
pure drip for 4 weeks, which demonstrated no efficacy, the internal
fixation was removed and an external fixation bracket was used for
the fixation instead. This, in combination with the drip, cured the
patient.
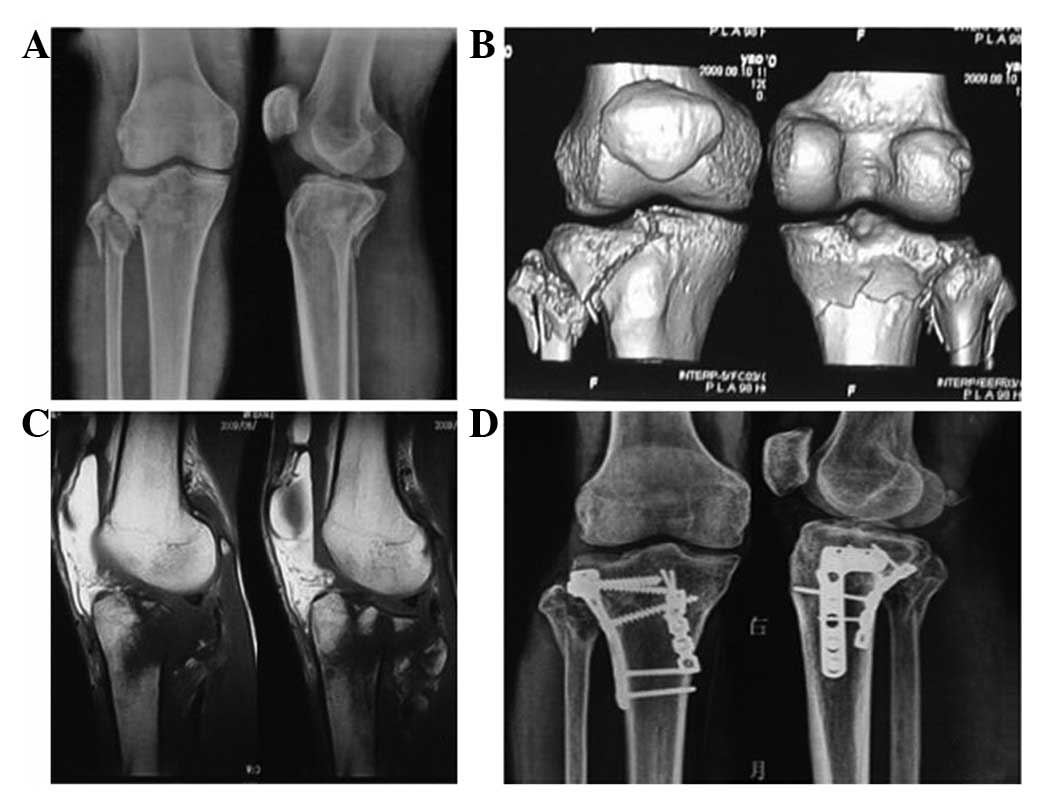
The conditions of the complex fractures of the
tibial plateau, as demonstrated by the three types of imaging
examination, are shown in Tables I
and II. MDCT was the most
sensitive method in the diagnosis of tibial articular surface
collapse, cruciate ligament tibial avulsion fracture, degree of
fracture comminution and degree of fracture displacement. MRI was
the most sensitive method in the diagnosis of injuries of the
cruciate and collateral ligaments and the meniscus and cartilage
peeling of the articular surface. Typical cases are illustrated in
Figs. 1–3.
 | Table IComparison of the satisfaction scores
from X-ray, MDCT and MRI for the diagnosis of fractures of the
tibial plateau. |
Table I
Comparison of the satisfaction scores
from X-ray, MDCT and MRI for the diagnosis of fractures of the
tibial plateau.
| Variable | Case (n) | Fracture sites | Severity of bone
comminution | Fracture
displacement | Bone defects |
|---|
| X-ray | 71 | 1.04±0.20 | 0.81±0.51 | 1.23±0.48 | 0.36±0.51 |
| MDCT | 71 | 1.82±0.38a | 1.92±0.26a | 1.92±0.26a | 1.55±0.79a |
| MRI | 71 | 1.12±0.33b | 0.83±0.60b | 0.46±0.58ab | 0.26±0.53b |
| F | - | 131.06 | 119.99 | 173.05 | 91.46 |
| P-value | - | <0.01 | <0.01 | <0.01 | <0.01 |
 | Table IIComparison of examination results from
X-ray, MDCT and MRI for the diagnosis of knee injuries. |
Table II
Comparison of examination results from
X-ray, MDCT and MRI for the diagnosis of knee injuries.
| Variable | Case (n) | Joint surface
collapse | Other (cruciate
ligament+meniscus+collateral ligament injury) |
|---|
| X-ray | 71 | 16 | 4(3+0+1) |
| MDCT | 71 | 61a | 11a(10+0+1) |
| MRI | 71 | 12b | 31ab(17+6+8) |
| χ2 | - | 85.7327 | 32.6626 |
| P-value | - | <0.01 | <0.01 |
Discussion
Certain types of fractures may be identified solely
by X-ray examination; however, fractures of the tibial plateau,
particularly complex fractures of the tibial plateau, require
evaluation by CT and MRI (4–7).
MDCT is efficacious in the classification of fractures of the
tibial plateau and enables observations of the morphology and the
degree of displacement from different levels and angles. In
particular, CT 3D reconstruction forms an intuitive image through
the rotation and incision of the axis, which enhances the
recognition of anatomical structures and pathological changes by
displaying the images from different spatial angles. This avoids
the blind zone caused by vision limitations, thus improving the
diagnostic level and enabling evaluations of the degree of
displacement of the fractures to be performed in a variety of
planes. X-ray films solely show data from the anterior and lateral
planes, which do not provide a satisfactory pathological anatomical
image for the clinical surgeons. With regard to the diagnosis of
fracture location, degree of fracture comminution, joint surface
collapse and fracture displacement, the use of MDCT was superior to
that of X-ray and MRI; however, the use of MRI was conducive to
diagnosing insidious fractures and bone contusions that were not
revealed by X-ray or CT, particularly with regard to damage of
cartilage inside the joint and soft structures. MRI was also able
to identify injuries of the menisci, the anterior and posterior
cruciate ligaments and the medial and lateral collateral ligament,
demonstrating incomparable advantages over X-ray and CT. In the
present study, six patients were diagnosed with injuries to the
menisci using preoperative MRI: 17 were diagnosed with cruciate
ligament injuries, one was diagnosed with cartilage peeling from
the joint surface of the femoral condyle and 18 were diagnosed with
an insidious fracture of the femoral condyle or bone contusions.
The study demonstrated that MDCT was able to show the condition of
the tibial plateau fractures precisely, while MRI was beneficial in
the early detection of damage to the soft structures inside the
knee joint, such as injuries of the menisci and the cruciate and
collateral ligaments and the degree of the injuries (8).
It is widely recognized that the majority of the
surgical regimens planned for the treatment of tibial plateau
fractures that have been based on common X-ray films require some
improvement or adjustment following CT and MRI evaluations. MDCT
and MRI are able to be more precise in showing the classification
of fractures and improving the surgical plan than X-rays (6). A precise and reasonable judgment may
be provided using X-ray, MDCT and 3D reconstruction and MRI, which
enables clinical surgeons to design an optimal surgical plan
according to the pathological morphologies and anatomical
characteristics. The size of a fracture fragment may be precisely
measured using imaging information, enabling a pre-reduction to be
conducted in advance using spatial imagination; furthermore, an
appropriate inner fixation object of the correct size and a
placement site may be selected, and the placement and direction of
the screws for fixation may be determined using imaging data. An
appropriate incision for exploration may be selected prior to
surgery, combined with the pathology requiring surgical repair
inside the articular cavity, such as injuries of the menisci,
ruptures of the cruciate ligaments, avulsed fractures and ruptures
of the medial and lateral collateral ligaments. If genicular cavity
exploration is required, a genicular anterior midline incision is
selected. The incision location may be adjusted either laterally or
medially, according to the requirement of the procedure. It is
beneficial to the accomplishment of the genicular cavity
exploration and surgical treatment if the incision extends towards
the appropriate site in the body. If it is not necessary to explore
the pathology of the articular cavity and only restoration of the
fat percentage of the joint surface is required, genicular medial
and lateral double incision or a genicular anterolateral
posteromedial incision is selected to reduce the surgical trauma
and to expose solely the tissues requiring surgical treatment. This
leads to a desirable treatment efficacy. In the present study,
there were no injuries of the knee joint that were not diagnosed,
no prolonged surgeries, no unnecessary trauma and no bleeding
during surgery. The infection rate of the wounds was low and good
functional recovery of the knee joints following surgery was
observed.
It has been demonstrated that MRI and MDCT may be
used to assist in the identification of insidious fractures of the
distal tibia that are involved with the joint surface (9). For patients with fractures of the
tibial plateau, the drawer and inside and outside turning tests may
not always be conducted satisfactorily, due to the early swelling
and pain of the limbs. It is not possible to identify injuries of
the cruciate and collateral ligaments and the menisci by common
X-ray examination. However, early damage of the genicular cavity
may lead to a leakage outside the joint due to arthroscopic
examination, thus preventing a further arthroscopic examination of
the knee joint from being conducted (10). If an MRI examination is not
conducted in time, it may delay the diagnosis or lead to missed
diagnoses, resulting in unnecessary medical disputes. MDCT and MRI
enable fractures and bone contusions around the knee joint and
injuries of the menisci and ligaments to be diagnosed as soon as
possible. Furthermore, MRI reveals bone contusions and the
insidious fractures that are not able to be diagnosed using common
X-ray films. The existence of bone contusions indicates that there
are injuries of the joint cavity and ligament, requiring evaluation
by MRI (11). Insidious fractures
may be identified as promptly as possible using MDCT scanning. The
efficacy of the treatment may be improved by the design of a more
appropriate surgical plan. As a result, MDCT and MRI have potential
as relatively new imaging technologies that may be applied to
complex fractures of the tibial plateau.
References
|
1
|
Catagni MA, Ottaviani G and Maggioni M:
Treatment strategies for complex fractures of the tibial plateau
with external circular fixation and limited internal fixation. J
Trauma. 63:1043–1053. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Li YC, Fu SJ, Xiao FS, et al: Case-control
studies on complex tibial plateau and posterior condylar fractures
treated through combined anterior-posterior (small incision or
micro-incision) approach. Zhongguo Gu Shang. 23:417–420. 2010.(In
Chinese).
|
|
3
|
Scharzker J, McBroom R and Bruce D: The
tibial fracture. The Toronto experience 1968–1975. Clin Orthop
Relat Rex. 138:94–104. 1979.PubMed/NCBI
|
|
4
|
Dunham CM, Ransom KJ, Flowers LL, et al:
Cerebral hypoxia in severely brain-injured patients is associated
with admission Glasgow Coma Scale score, computed tomographic
severity, cerebral perfusion pressure, and survival. J Trauma.
56:482–489. 2004. View Article : Google Scholar
|
|
5
|
Mei JR, Li XF, Zhu YM and Luo B: Spiral CT
reconstruction for typing of tibial plateau fracture to guide
surgical therapy. Zhongguo Gu Shang. 22:285–287. 2009.(In
Chinese).
|
|
6
|
Markhardt BK, Gross JM and Monu JU:
Schatzker classification of tibial plateau fractures: use of CT and
MR imaging improves assessment. Radiographics. 29:585–597. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Blin D, Cyteval C, Kamba C, et al: Imaging
of traumatic injuries of the knee. J Radiol. 88:775–788. 2007.(In
French).
|
|
8
|
Mui LW, Engelsohn E and Umans H:
Comparison of CT and MRI in patients with tibial plateau fracture:
can CT findings predict ligament tear or meniscal injury. Skeleta
Radiol. 36:145–151. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Miller JM, Svoboda SJ and Gerber JP:
Diagnosis of an isolated posterior malleolar fracture in a young
female military cadet: a resident case report. Int J Sports Phys
Ther. 7:167–172. 2012.PubMed/NCBI
|
|
10
|
Takai S, Yoshino N and Hirasawa Y:
Arthroscopic treatment of voluntary superior dislocation of the
patella. Arthroscopy. 14:753–756. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bencardino JT, Rosenberg ZS, Brown RR, et
al: Traumatic musculotendinous injuries of the knee: diagnosis with
MR imaging. Radiographics. 20:S103–S120. 2000. View Article : Google Scholar : PubMed/NCBI
|