Introduction
Successful endovascular aneurysm repair (EVAR)
requires sufficient proximal and distal landing zones that are
relatively free from disease (1).
If the aortoiliac aneurysm involves the iliac bifurcation,
successful EVAR may be limited. In these cases, the distal landing
zone should be in external iliac artery (EIA) which may interrupt
the flow of internal iliac artery (IIA). Bilateral IIA occlusion
during the endovascular repair of aneurysms is associated with
significant morbidity, including buttock claudication, erectile
dysfunction and ischemia of the sigmoid colon and perineum
(2,3).
Open or endovascular approaches are used to maintain
IIA circulation in such cases during EVAR. Endovascular options
include the double-barrel technique (4) or the use of iliac branch devices
(IBDs) (5). External-to-internal
iliac artery bypass is a reasonable option for an open approach to
preserve pelvic circulation (6).
The present report describes a patient with a common iliac artery
(CIA) aneurysm who underwent external-to-internal iliac bypass
surgery, and a second patient who was treated via a novel hybrid
approach to repair an IIA aneurysm.
Case reports
Case 1
A 70-year-old male patient presented with severe
claudication of the left leg. Hypertension and a cerebrovascular
attack featured in the past medical history of the patient. The
patient’s ankle brachial index (ABI) was 1.11 for the right leg and
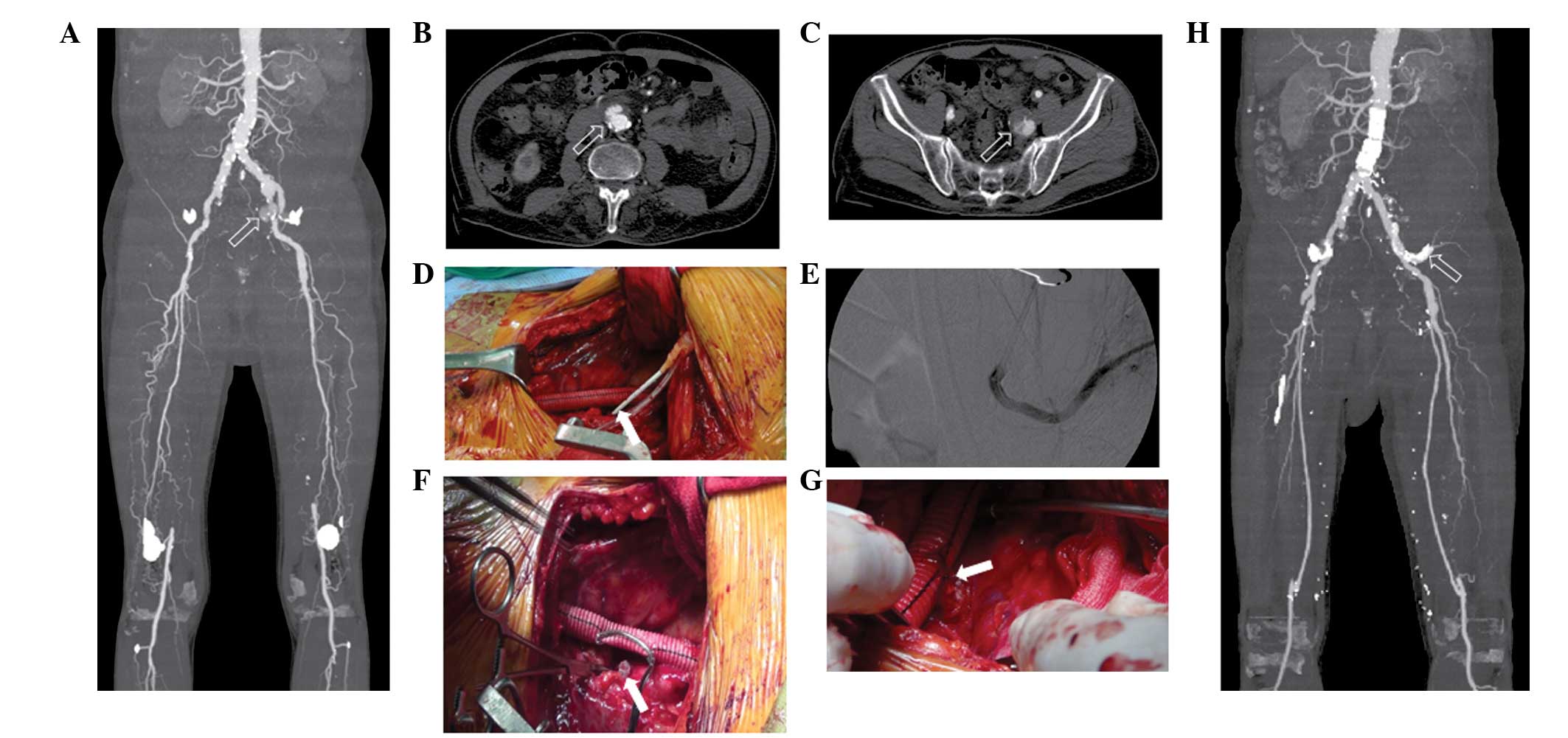
0.55 for the left. Computed tomography-angiography (CTA) showed
long-segment occlusion of the left iliac artery and a right CIA
aneurysm with a maximal diameter of 3.2 cm (Fig. 1A and C). There were multiple
penetrating atherosclerotic ulcers (PAUs) in the infrarenal
abdominal aorta (Fig. 1B).
Simultaneous repairs of the right CIA aneurysm and bypass surgery
for the left iliac occlusion were planned. A longitudinal skin
incision, ~5 cm long, was made in the left inguinal crease,
exposing the left femoral artery. A second oblique skin incision
was made on the right lower abdomen to approach the right iliac
arteries. The right EIA was tortuous. Following the division of the
right IIA, the proximal end was sealed using 4-0 Prolene™ (Ethicon,
Blue Ash, OH, USA) sutures (Fig.
1D). The distal portion of the IIA was anastomosed with a 7-mm
expanded polytetrafluoroethylene (ePTFE) graft. Two 7F introducer
sheaths were subsequently inserted into the right EIA with separate
punctures (Fig. 1E). One sheath
was used for the angiogram, while the other was used for the
delivery of the stent graft. A 5F pigtail catheter was inserted
though the distal introducer sheath to obtain the angiogram. A
28-mm Zenith main body device and a Zenith converter (Cook, Inc.,
Bloomington, IN, USA) were deployed serially in the aorta and the
iliac aneurysm (Fig. 1F). The
distal landing of the device was placed in the right EIA.
Subsequently, the tortuous portion of the right EIA was excised,
prior to being anastomosed in an end-to-end fashion. The ePTFE
graft, which was anastomosed with the right IIA, was connected onto
the right EIA. A second 7-mm ePTFE graft was placed though the
lower abdominal wall. An extra-anatomic bypass was made from the
IIA bypass graft to the left femoral artery (Fig. 1G). Postoperative CTA showed that
the repair of the aneurysm was successful and the bypass graft was
patent (Fig. 1H).
Case 2
A 69-year-old male patient presented with severe
claudication of his bilateral lower extremities. The patient had
hypertension, chronic obstructive pulmonary disease,
cerebrovascular attack and atrial fibrillation, as well as an ABI
of 0.56 for the right leg and 0.55 for the left. Preoperative CTA
showed bilateral superficial femoral artery occlusion. A focal
aneurysmal change was observed in the infrarenal abdominal aorta
and a left IIA aneurysm was visualized (Fig. 2A–C). The maximal diameter of the
left IIA aneurysm was 3.2 cm. A right femoropopliteal bypass was
performed using the ipsilateral great saphenous vein. One month
later, left femoropopliteal bypass and the repair of the infrarenal
aortic aneurysm and IIA aneurysm were planned. A routine
femoropopliteal bypass was prepared with the left great saphenous
vein. An oblique skin incision was made on the left lower abdomen
to approach the left iliac artery. Following the exposure of the
left iliac artery, the left CIA was divided. Having closed the
distal portion of the left CIA, a 10-mm Dacron graft (Meadox
Medicals, Oakland, NJ, USA) was connected to the proximal portion
of the left CIA. Two 7F introducer sheaths were then inserted into
the Dacron graft. One sheath was used for a 5F pigtail catheter,
which was placed for the angiograms, while the second sheath was
used for the insertion of the stent graft. A 24×58 mm aortic
extender of the Zenith device (Cook Inc.) was implanted into the
abdominal aorta to fix the aortic aneurysm. Following the
successful repair of the aneurysm, the Dacron graft was anastomosed
with the distal EIA. A 7F introducer sheath was inserted into the
IIA aneurysm by direct puncture (Fig.
2D). With this sheath, a 6×100 mm Gore®
Viabahn®-covered stent (W. L. Gore and Associates, Inc.,
Flagstaff, AZ, USA) was placed into the IIA aneurysm. The
completion angiogram showed that there was no endoleak into the IIA
aneurysm (Fig. 2E). A
thrombin-soaked Gelfoam® (Pfizer, Brussels, Belgium) was used to
fill the aneurysm. The scalloped, proximal portion of the Viabahn
stent was excised. The stent was then anastomosed with the Dacron
graft (Fig. 2F). Following the
successful repair of the aortic aneurysm and left IIA aneurysm,
routine femoropopliteal bypass was performed using the ipsilateral
great saphenous vein of the patient’s left leg. Postoperative CTA
showed no endoleaks at the site of aneurysm repair and a patent
vein graft, as well as the Viabahn-covered stent in the IIA
aneurysm.
Discussion
The use of EVAR for the repair of aortoiliac
aneurysms is steadily increasing. If a sufficient distal landing
zone is not present in the CIA during EVAR, there may be a
requirement to extend the iliac limbs into the EIA. Embolization of
the IIA may be required to prevent type II endoleaks from the IIA.
The pelvic circulation may be interrupted if embolization of the
bilateral IIA is necessary. The interruption of the pelvic
circulation may result in buttock ischemia, spinal cord, bowel and
bladder ischemia, as well as erectile dysfunction (7). For this reason, novel endovascular
approaches have recently been investigated, including the
double-barrel technique (4) or the
use of IBDs (5).
External-to-internal iliac artery bypass is another
open approach strategy. Unno et al (6) described five patients who underwent
external-to-internal iliac artery bypass during the endovascular
repair of abdominal aortic aneurysms and bilateral CIA aneurysms
(6). None of these patients had
experienced new-onset erectile dysfunction or buttock claudication
one month subsequent to surgery. In the present study, 7-mm ePTFE
grafts were used in the patients. Since the IIA is in a deeper
portion of the pelvic cavity, it is difficult to anastomose the
graft and the IIA. To overcome this difficulty, the graft was
connected to the IIA in an end-to-end fashion. Following the
completion of the EVAR, the graft was connected to the EIA.
The EIA is smaller in diameter and more tortuous
than the CIA. The deployment of endograft limbs into the EIA leads
to higher rates of occlusion and leg amputation (8). Franz reported that the excision of
the tortuous EIA and end-to-end anastomoses were able to overcome
the difficulties associated with the tortuosity of the EIA
(9). This simple procedure was
performed in the first patient described in the present study.
Following the deployment of the stent graft, the tortuous portion
of the EIA was excised and end-to-end anastomosis was subsequently
achieved using 5-0 Prolene sutures.
In the first patient described in this study, the
left iliac artery was already occluded. Another route was therefore
sought in order to obtain an angiogram during the placement of the
stent graft. In such situations, the left brachial artery is
commonly used. However, the brachial approach is associated with
complications. Alvarez-Tostado et al (10) revealed that brachial access
site-related complications occurred in 21 (6.5%) out of 323
patients (10). Thirteen of the 21
patients (62%) required surgical correction, mostly for brachial
artery thrombosis or pseudoaneurysm. In the present study, it was
possible to insert two introducer sheathes into the EIA in the
patients, since the EIA had already been exposed. It is more
comfortable for the patient for the angiogram sheath to be inserted
distally, since this avoids the interruption of the pigtail
catheters during the insertion of the main body.
The endovascular options for the repair of IIA
aneurysms include the double-barrel technique and the use of IBDs.
However, in some countries, IBDs are not available. In the second
patient in the present study, the treatment plan was to repair the
aortic aneurysm and bypass the stenotic segment of the left iliac
artery. Therefore, a 10-mm Dacron graft was connected to the left
CIA following division. This type of graft is commonly used to
create iliac conduits during EVAR or thoracic endovascular aneurysm
repair (11). The graft was then
anastomosed to the distal EIA. A 7F introducer sheath was directly
inserted into the IIA aneurysm. Using this sheath, a
Viabahn-covered stent was easily inserted into the IIA aneurysm.
Having confirmed that there was no endoleak, thrombin-soaked
Gelfoam® was used to fill the aneurysm. This covered
stent was anastomosed to the bypassed Dacron graft and suturing was
completed without difficulty. This approach is a feasible option
for the repair of IIA aneurysms.
References
|
1
|
Woodburn KR, Chant H, Davies JN, Blanshard
KS and Travis SJ: Suitability for endovascular aneurysm repair in
an unselected population. Br J Surg. 88:77–81. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Karch LA, Hodgson KJ, Mattos MA, Bohannon
WT, Ramsey DE and McLafferty RB: Adverse consequences of internal
iliac artery occlusion during endovascular repair of abdominal
aortic aneurysms. J Vasc Surg. 32:676–683. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Domoto S, Tagusari O, Takai H, Nakamura Y,
Seike Y and Ito Y: Pelvic abscess following internal iliac artery
embolization prior to endovascular aneurysm repair. J Vasc Surg.
56:1734–1736. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
DeRubertis BG, Quinones-Baldrich WJ,
Greenberg JI, Jimenez JC and Lee JT: Results of a double-barrel
technique with commercially available devices for hypogastric
preservation during aortoilac endovascular abdominal aortic
aneurysm repair. J Vasc Surg. 56:1252–1259. 2012. View Article : Google Scholar
|
|
5
|
Parlani G, Verzini F, De Rango P, et al:
Long-term results of iliac aneurysm repair with iliac branched
endograft: A 5-year experience on 100 consecutive cases. Eur J Vasc
Endovasc Surg. 43:287–292. 2012.PubMed/NCBI
|
|
6
|
Unno N, Inuzuka K, Yamamoto N, Sagara D,
Suzuki M and Konno H: Preservation of pelvic circulation with
hypogastric artery bypass in endovascular repair of abdominal
aortic aneurysm with bilateral iliac artery aneurysms. J Vasc Surg.
44:1170–1175. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Rayt HS, Bown MJ, Lambert KV, et al:
Buttock claudication and erectile dysfunction after internal iliac
artery embolization in patients prior to endovascular aortic
aneurysm repair. Cardiovasc Intervent Radiol. 31:728–734. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Conway AM, Modarai B, Taylor PR, et al:
Stent-graft limb deployment in the external iliac artery increases
the risk of limb occlusion following endovascular aaa repair. J
Endovasc Ther. 19:79–85. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Franz RW: Unique operative approach for
dealing with a tortuous external iliac artery during abdominal
aortic aneurysm endografting. Int J Angiol. 18:49–51. 2009.
View Article : Google Scholar
|
|
10
|
Alvarez-Tostado J, Moise M, Bena J, et al:
The brachial artery: A critical access for endovascular procedures.
J Vasc Surg. 49:378–385. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Criado F: Iliac arterial conduits for
endovascular access: Technical considerations. J Endovasc Ther.
14:347–351. 2007. View Article : Google Scholar : PubMed/NCBI
|