Introduction
Knee osteoarthritis (KOA) is a degenerative disorder
that results from cartilage failure or an imbalance of the
degradation and repair processes of chondrocytes, cartilage matrix
and subchondral bone, which are induced by a complex interplay of
biochemical and biomechanical factors with secondary components of
inflammation (1,2). Studies have shown that the incidence
of KOA in people aged >65 years ranges from 60 to 70%, with the
incidence rate reaching up to 85% in the population aged >75
years (3). Joint stiffness and
pain are the main clinical symptoms of KOA (4). However, there is no effective
treatment for KOA. Care focuses on alleviating the symptoms of
stiffness and pain, and improving or maintaining the physical
function of the knee joint, based on the guidelines published by
the American College of Rheumatology (5,6).
Conventional therapies for KOA, which are designed
to regulate the symptoms of stiffness and pain, include topical
analgesics, glucosamine, nonsteroidal anti-inflammatory drugs,
intra-articular injection of sodium hyaluronate and surgical
treatment (7,8). However, these therapies are not
considered curative, and are usually accompanied by a number of
side-effects ranging from patient discomfort to kidney and liver
damage. The majority of patients with KOA are not satisfied with
the recurring side-effects of conventional drug therapies, which
results in the use of alternative and complementary therapies
(9,10). Traditional Chinese medicine (TCM),
including acupuncture and Chinese herbal medicine, has been shown
to be particularly efficacious for treating pain for thousands of
years, especially when related to joint diseases such as KOA
(11–13). At present, an increasing number of
patients are turning to alternative and complementary medicine
owning to the limitations and side-effects of conventional
therapies. Therefore, it is necessary to explore the mechanisms of
these therapies for treating KOA.
KOA is a chronic, retrogressive knee disease often
occurring in the elderly, with most cases belonging to the TCM
‘stasis of the channels’ type (14). In needle-knife therapy, a physician
stimulates local tissue using a needle-knife to loosen and release
adhesions so as to relieve tension pain and recover internal force
equilibrium of the knee joint (15). Needle-knife therapy may also slow
down the degradation of articular cartilage and improve and
maintain the function of the joint (16). Indications of KOA include joint and
myofascial pain, and refractory pain and inflammation in rheumatoid
disorders. Due to the fact that it causes minimal injury to local
tissue, does not compromise the overall structure of the knee and
enables rapid patient recovery, needle-knife therapy has been
widely used to treat a variety of rheumatoid disorders involving
joint stiffness, pain and swelling, including rheumatoid arthritis
and KOA (15,17,18).
The aim of the present study was to identify a more
effective therapy for reducing joint pain and disability, as well
as to prevent and mitigate cartilage degradation. A randomized,
controlled study was performed to evaluate the safety and efficacy
of needle-knife therapy for treating KOA. The basic design of this
study involved the quantification and comparison of the efficacy of
needle-knife therapy and acupuncture for KOA. The effects of the
two treatments on the clinical symptoms of KOA and the expression
of inflammatory cytokines were investigated.
Materials and methods
Patient information
A total of 170 patients with KOA from the Fuzhou
General Hospital of Nanjing Military Command (Fuzhou, China) from
April 2010 to March 2013 were enrolled in this study. The clinical
characteristics of the patients were recorded in a uniform data
collection table.
All patients enrolled were randomly assigned to two
groups by lottery and their general characteristics are listed in
Table I. There was no significant
difference in gender, age, illness course and number of affected
knees between the two groups (P>0.05); hence, the groups were
comparable. The study was approved by the Ethics Committee of the
Fuzhou General Hospital of Nanjing Military Command. Informed
consent was obtained from all patients.
 | Table IGeneral characteristics of patients
with knee osteoarthritis. |
Table I
General characteristics of patients
with knee osteoarthritis.
| Group | Cases | Affected knee
(cases) | Stage | Gender (cases,
M/F) | Age (years) | Course of disease
(months) | No. of knees |
|---|
|
|---|
| Single | Bilateral |
|---|
| Treatment | 85 | 39 | 46 | I | 9/11 | 52.52±8.63 | 10.76±7.92 | 28 |
| | | | II | 13/10 | 57.66±11.35 | 18.34±11.47 | 35 |
| | | | III | 11/14 | 58.71±10.54 | 24.22±15.24 | 47 |
| | | | IV | 8/9 | 60.43±7.87 | 26.92±10.53 | 21 |
| Control | 85 | 37 | 48 | I | 8/10 | 51.43±9.12 | 11.36±8.41 | 26 |
| | | | II | 12/14 | 55.94±12.67 | 16.94±13.62 | 44 |
| | | | III | 12/13 | 59.36±13.50 | 22.53±17.72 | 43 |
| | | | IV | 9/7 | 61.65±8.92 | 27.83±11.42 | 20 |
Standards for diagnosis and
inclusion
Standards for the diagnosis of KOA in
Western medicine
The diagnosis of KOA was formulated according to the
standards issued by the American College of Rheumatology (5,19).
Patients must have either knee joint pain or osteophytes and
fulfill at least one of the following three criteria: i) Age >40
years; ii) morning stiffness lasting <30 min and an audible
sound of bone friction; and iii) enlarged tender bone and no
evident heat in the joint. The severity of KOA was classified into
5 stages (20), specifically:
Stage 0, normality; stage I, appearance of lip-like osteophytes;
stage II, noticeable osteophytes narrowing the joint gap; stage
III, moderate and multiple osteophytes markedly narrowing the joint
gap with bony sclerosis and wear; and stage IV, large osteophytes
markedly narrowing the joint gap with serious bony sclerosis and
evident wear of the bone.
Standards for the diagnosis of KOA in
TCM
The TCM syndrome of ‘stasis of the channels’ type
was differentiated with reference to the standards for diagnosis in
Efficacy Evaluation of TCM Diseases and Syndromes and the Guiding
Principle of Clinical Research on New Drugs of Traditional Chinese
Medicine (14). Diagnosis included
knee joint pain, difficulty in flexion and extension, weakness and
soreness in the loin and knees, accompanied by the presence of a
reddish tongue with a thin or thin greasy coating and a taut
pulse.
Standards for exclusion
The patients with the following conditions were
excluded: Patients aged >70 years; patients with concurrent
rheumatoid arthritis, psoriasis, syphilitic neuropathy, ochronosis,
metabolic osteopathy, acute trauma and other diseases affecting the
joints; women in pregnancy or lactation; patients with accompanying
severe cardiovascular, hepatic, renal or with mental disease;
patients who had been treated with other methods that may have
influenced the observation of indices in this study; and patients
who discontinued treatment during the study or refused to
objectively provide evaluation data in this study.
Treatment
The patients in the treatment group were treated
with needle-knife (Hanzhang Acupotome; Beijing Huaxia Acupotome
Medical Equipment Factory, Beijing, China) therapy at the dominant
acupoints of Neixiyan (Ex-LE4) and Waixiyan (Ex-LE5), as well as
the conjugate points Xuanzhong (GB39), Xuehai (SP10), Dubi (ST35)
and Taixi (KI3) (Figs. 1 and
2). The patient lay in a supine
position with general skin disinfection. After the acupoints were
disinfected, needle-knives was inserted at the dominant acupoints,
parallel to the direction of muscles, nerves and vessels. Following
the needle-knife surgery, patients undertook passive activities of
knee flexion, extension and rotation. The treatment was conducted
once as one therapeutic course and two courses were administered to
each patient with a 6-day interval between the two courses.
The patients in the control group were treated with
acupuncture at the dominant acupoints of Neixiyan and Waixiyan, as
well as the conjugate points Xuanzhong, Xuehai, Dubi and Taixi. The
patients were seated with the knee joints flexed. After the
acupoints were disinfected, routine, disposable needles were
inserted at the dominant acupoints for 1.5 Cun, with twisting up
and down to induce ‘De-Qi’. The treatment was conducted daily for 5
days as one therapeutic course, and two courses were administered
to each patient with a 2-day interval between the two courses.
Indices for observation
The clinical symptoms scores of the patients were
evaluated for 11 items following the criteria set in reference to
the Guiding Principle of Clinical Research on New Drugs of TCM
(14): i) Morning pain or
stiffness after getting up; ii) resting pain of the knee joint;
iii) sensation of discomfort or pain while walking; iv) swollen
knee joint; v) tenderness of the knee joint; vi) difficulty in
extension and flexion of the knee joint; vii) maximum distance of
walking; viii) daily life activity; ix) heat sensation in the local
skin of the knee joint; x) local reddish skin; and xi) help needed
when moving from a sitting to a standing position.
The symptoms of items i)–vii) were ranked by
severity in three grades and scored from 1 to 3; the more severe
the symptom, the higher the score, and no symptom scored 0. A
similar method was performed on the symptoms of items viii) and
ix), but they were ranked in two grades and scored from 1 to 2; as
for items x) and xi), when they occurred, the score was 1,
otherwise it was 0. The severity of KOA was estimated in three
grades based on the total score of symptoms (the sum of various
symptoms): mild grade, the total score was <10; moderate grade,
the total score was from 10 to 18; and severe grade, the total
score was >18. The maximum possible symptom score was 33.
Standard for curative effects
With reference to the Guiding Principle of clinical
Research on New Drugs of TCM (14), according to the subjective
sensation of the patients and their knee joint function, the
therapeutic efficacy on the affected knee joints was evaluated
using the following four grades: Grade 1 (excellent), symptoms
disappeared with normal function and the severity of KOA scored 0
or 1; grade 2 (good), symptoms basically disappeared and function
was recovered, enabling daily activities and work to be carried
out, and the KOA severity score was decreased by >2/3; grade 3
(moderate), pain disappeared with basic normal knee joint extension
and flexion functions, some improvement in daily activities, and
the KOA severity score was reduced by between 1/3 and 2/3; and
grade 4 (bad), no evident alleviation of the symptoms. The
percentage of knees in a group that were of the former three grades
was defined as the effective rate.
Determination of inflammatory cytokine
levels
For the assessment of the IL-1β, IL-6 and TNF-α
levels in the synovial fluid, the synovial fluid collected from the
patients with KOA prior to and following treatment was dispensed
into 1-ml aliquots. The synovial fluid was diluted with diluent’s
buffer (Nanjing Jiancheng Biochemicals Ltd., Co., Nanjing, China)
to the appropriate detection range for evaluation by enzyme-linked
immunosorbent assay (ELISA). The levels of the proteins of interest
in the synovial fluid were measured using commercially available
ELISA kits (Nanjing Jiancheng Biochemicals Ltd., Co.), following
the manufacturer’s instructions.
Safety evaluation
The symptoms and physical signs of adverse reactions
that occurred following the two treatments (needle-knife therapy
and acupuncture) were recorded, and routine blood, urine and stool
tests, electrocardiogram (ECG) tests, and evaluations of liver and
renal functions were performed before and after treatment.
Statistical analysis
All data were analyzed using SPSS software for
Windows, version 13.0 (SPSS, Inc., Chicago, IL, USA). Statistical
analysis of the data was performed with Student’s t-test and
one-way analysis of variance. The enumeration data was analyzed by
the chi-square test. P<0.05 was considered to indicate a
statistically significant difference.
Results
Accomplishment of study
From the 170 patients (264 knees) enrolled in this
study, 151 patients (233 knees) completed the trial and 19 patients
(31 knees) were removed. In this study, 76 patients (117 knees) and
75 patients (116 knees) completed the trial in the treatment and
control groups, respectively. The nineteen patients (31 knees) that
were excluded due to uncompleted prescribed therapeutic courses
included nine patients (14 knees) in the treatment group with two
joints of stage I, three joints of stage II, five joints of stage
III and four joints of stage IV; and 10 patients (17 knees) in the
control group, which comprised three joints of stage I, six joints
of stage II, five joints of stage III and three joints of stage IV.
The exclusion rates in the two groups were not significantly
different and the influence of exclusion on the intergroup
proportionality of the baseline was negligible.
Comparison of total symptom scores of
KOA
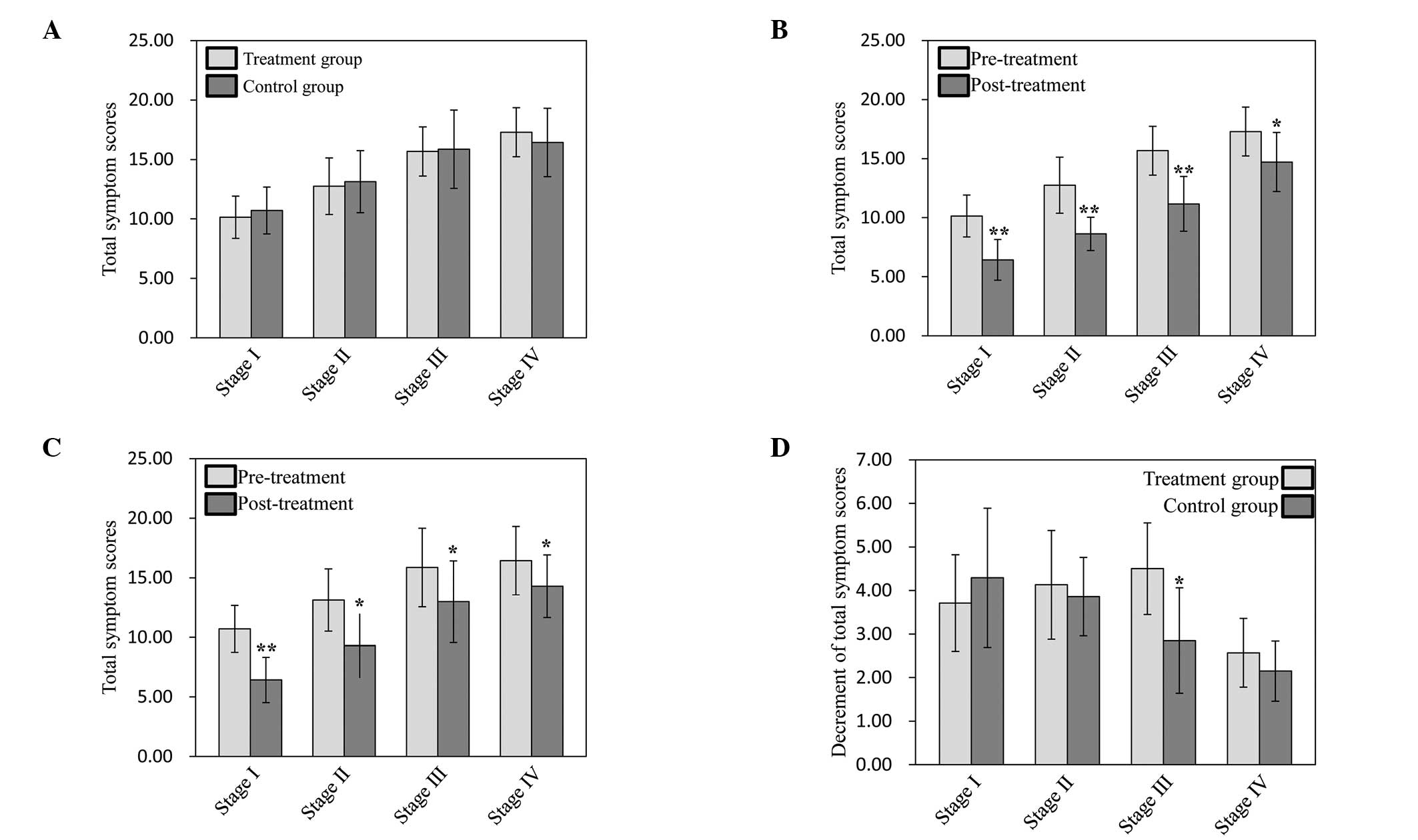
The symptom scores of KOA at the corresponding
stages were not significantly different between the two groups
prior to treatment (P>0.05). Following treatment, the symptom
scores of KOA in stages I–IV were reduced significantly in the
treatment group (P<0.05 or P<0.01), and the scores of KOA in
stages I–III were decreased significantly in the control group
(P<0.05 or P<0.01), while those of stage IV were not
significantly changed (P>0.05), although a slight reduction was
detected (Fig. 3A–C).
In a comparison between the two groups, with the
exception of a significant reduction in the total symptom scores of
KOA in stage III in the treatment group compared with that in the
control group (P<0.05), no significant differences were observed
in the symptom scores of KOA at other stages of the disease
(P>0.05), although a few divergences were revealed (Fig. 3D).
Comparison of clinical effectiveness
No statistically significant difference between the
two groups was detected in the excellent rates of the treatments in
the patients at stages I–IV and in the effective rates of the
treatments in the patients of stages I and II (P>0.05). The
effective rate in patients of stages III and IV in the treatment
group was significantly higher than that in the control group
(P<0.05) (Table II).
 | Table IIComparison of clinical
effectiveness. |
Table II
Comparison of clinical
effectiveness.
| Group | Cases | Stage | No. of knee | Grade of
effectiveness (no. of knee) | Excellent rate
(%) | Effective rate
(%) |
|---|
|
|---|
| Excellent | Good | Moderate | Bad |
|---|
| Treatment | 76 | I | 26 | 5 | 12 | 6 | 3 | 65.38 | 88.46 |
| | II | 32 | 3 | 12 | 11 | 6 | 46.88 | 81.25 |
| | III | 42 | 0 | 7 | 26 | 9 | 16.67 | 78.57* |
| | IV | 17 | 0 | 1 | 10 | 6 | 5.88 | 64.71* |
| Control | 75 | I | 23 | 3 | 11 | 7 | 2 | 60.87 | 91.30 |
| | II | 38 | 2 | 15 | 13 | 8 | 44.74 | 78.95 |
| | III | 38 | 0 | 4 | 19 | 15 | 10.53 | 60.53 |
| | IV | 17 | 0 | 1 | 6 | 10 | 5.88 | 41.18 |
Comparison of the synovial fluid
concentrations of IL-1β, IL-6 and TNF-α
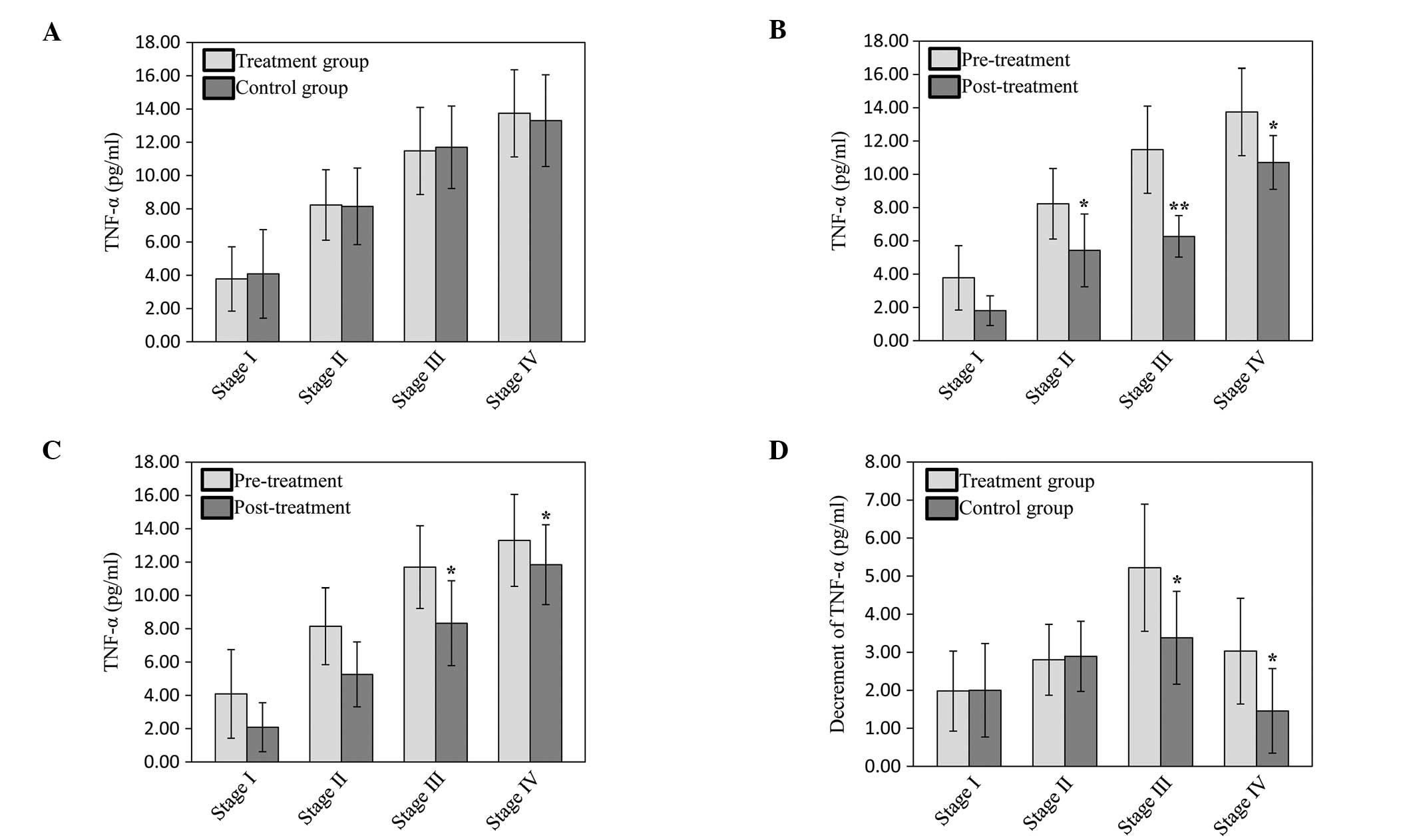
To evaluate the effect of needle-knife therapy on
the expression levels of inflammatory cytokines, the concentrations
of IL-1β, IL-6 and TNF-α in the synovial fluid of the patients with
KOA were investigated by ELISA. As shown in Figs. 4–6, the synovial fluid concentrations of
IL-1β, IL-6 and TNF-α were not different between the treatment and
control groups. In stages III and IV of KOA, the decrement of IL-1β
in the treatment group was significantly higher than that in the
control group (P<0.05). In stage III of KOA, the synovial fluid
concentration of IL-6 in the treatment group was significantly
different between pre- and post-treatment (P<0.05), and the
decrement of IL-6 in the treatment group was significantly
decreased compared with that of the control group (P<0.01). The
concentration of TNF-α in the synovial fluid following treatment
was markedly decreased compared with that prior to treatment in
stages II, III and IV of the treatment group (P<0.05 and
P<0.01), while the changes of TNF-α levels in the control group
in stages III and IV were similar to those in the treatment group
(P<0.05). This suggests that needle-knife therapy inhibited the
expression of inflammatory cytokines.
Comparison of X-ray features
No significant changes in the X-ray features between
before and after treatment were observed in either group,
indicating that although treatment in the two groups effectively
alleviated the symptoms of KOA, it did not improve the organic
changes that had previously occurred.
Safety evaluation
No adverse reaction-associated signs and symptoms or
laboratory indices were identified during the whole treatment
course.
Discussion
The results of the present support the use of
needle-knife therapy as a safe and effective method for the
treatment of KOA. It was shown to be more effective than routine
acupuncture for the alleviation of pain and improvement of
physiological function by inhibiting the expression of inflammatory
cytokines. In addition, the results also indicated that acupuncture
may relieve knee stiffness and pain and improve the function scores
of KOA.
KOA increases in prevalence with age and is a major
cause of pain and locomotor disability worldwide. It belongs to the
category of Gu Bi in TCM, which means either the limbs or the
joints are suffering from pain and malfunction. TCM suggests that
the disease is based on Gan-Shen insufficiency and weakness of
tendons and bones, and is importantly linked to blood stasis
(21). Currently, there is no
definitive cure for KOA, and available treatments are aimed at
improving pain and function in the hopes of delaying knee
replacement surgery (22). TCM has
shown significant advancements against KOA, such as improving the
clinical presentation of patients, and inhibiting inflammatory
reaction and cartilage degradation (23). Needle-knife, an ancient traditional
Chinese medical therapy, is used widely to treat KOA. When
practiced by a certified provider, it is safe and patients often
find it calming and relaxing. Although the biological mechanisms by
which needle-knife therapy improves the clinical consequences of
KOA are not fully understood, its analgesic effect and ability to
improve cold-dampness pathogen components are likely to have an
important role (24). In order to
observe the curative effects of needle-knife therapy for treating
KOA, the curative effects and changes in the total score of
symptoms prior to and following treatment between a needle-knife
therapy group and an acupuncture therapy group were determined.
Patients with KOA require better pain control and
reduced adverse events. Therefore, as comorbidities and aging
increase, a more convenient approach is necessary (25). Needle-knife, as an effective, safe
and non-pharmaceutical therapy regimen, has also been used widely
for the management of KOA. According to TCM theory, KOA is a bone
obstruction disease, in which the knee joints suffer from
stiffness, pain, and/or malfunction due to invasions of dampness or
wind cold, accompanied by the disharmony of Qi and blood,
consequently resulting in the syndrome of ‘blood stasis’ and ‘cold
dampness’ (26,27). Therefore, the acupoints of Neixiyan
(Ex-LE4), Waixiyan (Ex-LE5), Xuehai (SP10) and Dubi (ST35) were
selected in the treatment for activating the blood, resolving
stasis, dispelling cold and removing dampness, which may induce
stimulation, directly reaching the illness site and acting to
alleviate clinical symptoms and improve the function of the knee
joint.
According to the features of KOA, two widely applied
acupoints, Xuanzhong (GB39) and Taixi (KI3), were selected to
dredge the meridian-collaterals and nourish Shen to strengthen
bone, which may effectively improve the Gan-Shen insufficiency and
weakness of tendons and bones, raise the endurance of
peri-articular tissue to inflammatory stimulation, and be helpful
for knee joint pain alleviation and knee joint function restoration
to attain good therapeutic effectiveness. Hence, needle-knife
therapy may effectively alleviate pain in the knee joints and
improve the scope of motion. Results of this study showed that the
clinical symptoms in patients with KOA of stages I–IV were improved
significantly following treatment with needle-knife or acupuncture
therapy, while needle-knife therapy showed a better efficacy than
acupuncture for the patients of stages III and IV.
KOA is characterized by an imbalance of matrix
synthesis and matrix degradation in cartilage at the cell and
tissue levels. Chondrocytes, the only cell type present in
articular cartilage, are responsible for the synthesis and
breakdown of the extracellular matrix (ECM) (28). Signals generated by growth factors,
cytokines and the ECM control chondrocyte metabolic activity.
During the pathological progression of KOA, excessive ECM
degradation overwhelms ECM synthesis and this appears to be due to
inflammatory and catabolic signals that are present in excess of
the anti-inflammatory and anabolic signals. Pro-inflammatory
cytokines associated with KOA include IL-1β, IL-6 and TNF-α
(29). Of these cytokines, IL-1β
is considered to be the major cytokine mediating cartilage
destruction, which induces a cascade of inflammatory and catabolic
events, including the expression of nitric oxygen production,
prostaglandin E2 release and cartilage degrading matrix
metalloproteinases, while inhibiting collagen and proteoglycan
synthesis (30–33). In addition, IL-6 is thought to have
a regulatory role and is capable of downregulating type II collagen
gene expression in articular chondrocytes (34). TNF-α and IL-1β also affect the
synthetic activity of chondrocytes by inhibiting the synthesis of
type II collagen and proteoglycans (35,36).
The results of the present study showed that the decrements of
IL-1β, IL-6 and TNF-α in the treatment group were greater than
those in the control group.
The preliminary findings in the present study
indicate that needle-knife therapy is effective in improving knee
pain, stiffness and physical function in patients with KOA. The
curative and the long-term curative effects are to be determined in
further follow-up visits. The major limitation in the present study
was the small sample size, and a randomized controlled study with a
larger sample size will be conducted in the future.
Acknowledgements
This study was supported by the National Natural
Science Foundation of China (grant no. 81102609) and the Natural
Science Foundation of Fujian Province (grant no. 2011J05074).
References
|
1
|
Li XH, Peng J, Xu YF, et al:
Tetramethylpyrazine (TMP) promotes chondrocyte proliferation via
pushing the progression of cell cycle. J Med Plants Res.
5:3896–3903. 2011.
|
|
2
|
Li X, Lang W, Ye H, et al: Tougu Xiaotong
capsule inhibits the tidemark replication and cartilage degradation
of papain-induced osteoarthritis by the regulation of chondrocyte
autophagy. Int J Mol Med. 31:1349–1356. 2013.
|
|
3
|
Sarzi-Puttini P, Cimmino MA, Scarpa R, et
al: Osteoarthritis: an overview of the disease and its treatment
strategies. Semin Arthritis Rheum. 35(1 Suppl 1): 1–10. 2005.
View Article : Google Scholar
|
|
4
|
Felson DT, Lawrence RC, Dieppe PA, et al:
Osteoarthritis: new insights. Part 1: the disease and its risk
factors. Ann Intern Med. 133:635–646. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
No authors listed. Recommendations for the
medical management of osteoarthritis of the hip and knee: 2000
update. American College of Rheumatology Subcommittee on
Osteoarthritis Guidelines. Arthritis Rheum. 43:1905–1915. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Jordan KM, Arden NK, Doherty M, et al;
Standing Committee for International Clinical Studies Including
Therapeutic Trials ESCISIT. EULAR Recommendations 2003: an evidence
based approach to the management of knee osteoarthritis: Report of
a Task Force of the Standing Committee for International Clinical
Studies Including Therapeutic Trials (ESCISIT). Ann Rheum Dis.
62:1145–1155. 2003. View Article : Google Scholar
|
|
7
|
Hamburger MI, Lakhanpal S, Mooar PA and
Oster D: Intra-articular hyaluronans: a review of product-specific
safety profiles. Semin Arthritis Rheum. 32:296–309. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Felson DT, Lawrence RC, Hochberg MC, et
al: Osteoarthritis: new insights. Part 2: treatment approaches. Ann
Intern Med. 133:726–737. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Blower AL, Brooks A, Fenn GC, et al:
Emergency admissions for upper gastrointestinal disease and their
relation to NSAID use. Aliment Pharmacol Ther. 11:283–291. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
McGettigan P and Henry D: Cardiovascular
risk and inhibition of cyclooxygenase: a systematic review of the
observational studies of selective and nonselective inhibitors of
cyclooxygenase 2. JAMA. 296:1633–1644. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Health Quality Ontario. Arthroscopic
lavage and debridement for osteoarthritis of the knee: an
evidence-based analysis. Ont Health Technol Assess Ser. 5:1–37.
2005.PubMed/NCBI
|
|
12
|
Fu MY and Zhang ZL: Knee osteoarthritis
treated with acupuncture at the points selected according to
syndrome differentiation: a randomized controlled trial. Zhongguo
Zhen Jiu. 31:1062–1066. 2011.(In Chinese).
|
|
13
|
Ahsin S, Saleem S, Bhatti AM, Iles RK and
Aslam M: Clinical and endocrinological changes after
electro-acupuncture treatment in patients with osteoarthritis of
the knee. Pain. 147:60–66. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wu MX, Li XH, Lin MN, et al: Clinical
study on the treatment of knee osteoarthritis of Shen-Sui
insufficiency syndrome type by electroacupuncture. Chin J Integr
Med. 16:291–297. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zeng GG, Zhang XF, Quan WC, et al: Effects
of needle knife relaxing therapy on tension of local soft tissue
and pain of osteoarthritis of knee. Zhongguo Zhen Jiu. 28:244–247.
2008.(In Chinese).
|
|
16
|
Lu D, Xu WX, Ding WG, Guo QF, Ma GP and
Zhu WM: Case-control study on needle-knife to cut off the medial
branch of the lumbar posterior ramus under C-arm guiding for the
treatment of low back pain caused by lumbar facet osteoarthritis.
Zhongguo Gu Shang. 26:214–217. 2013.(In Chinese).
|
|
17
|
Guo CQ, Ji B, Chen YN, et al: Affection of
acupotomy lysis on leu-enkephalin (L-ENK) content in different
parts of centrum of rats with knee osteoarthritis. Zhongguo Gu
Shang. 24:656–658. 2011.(In Chinese).
|
|
18
|
Hawker GA, Mian S, Bednis K and Stanaitis
I: Osteoarthritis year 2010 in review: non-pharmacologic therapy.
Osteoarthritis Cartilage. 19:366–374. 2011.PubMed/NCBI
|
|
19
|
Oliveria SA, Felson DT, Reed JI, Cirillo
PA and Walker AM: Incidence of symptomatic hand, hip, and knee
osteoarthritis among patients in a health maintenance organization.
Arthritis Rheum. 38:1134–1141. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Sharif M, George E and Dieppe PA:
Correlation between synovial fluid markers of cartilage and bone
turnover and scintigraphic scan abnormalities in osteoarthritis of
the knee. Arthritis Rheum. 38:78–81. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Li XH, Liang WN and Liu XX: Clinical
observation on curative effect of dissolving phlegm-stasis on 50
cases of knee osteoarthritis. J Tradit Chin Med. 30:108–112. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Wang HM, Liu JN and Zhao Y: Progress on
integrated Chinese and Western medicine in the treatment of
osteoarthritis. Chin J Integr Med. 16:378–384. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Mao JJ and Kapur R: Acupuncture in primary
care. Prim Care. 37:105–117. 2010. View Article : Google Scholar
|
|
24
|
Li HY, Cui L, Cui M and Tong YY: Active
research fields of acupuncture research: a document co-citation
clustering analysis of acupuncture literature. Altern Ther Health
Med. 16:38–45. 2010.PubMed/NCBI
|
|
25
|
Lechner M, Steirer I, Brinkhaus B, et al:
Efficacy of individualized Chinese herbal medication in
osteoarthrosis of hip and knee: a double-blind,
randomized-controlled clinical study. J Altern Complement Med.
17:539–547. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Tan C, Wang J, Feng W, Ding W and Wang M:
Preliminary correlation between warm needling treatment for knee
osteoarthritis of deficiency-cold syndrome and metabolic functional
genes and pathways. J Acupunct Meridian Stud. 3:173–180. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Li XH, Wu MX, Ye HZ, et al: Experimental
study on the suppression of sodium nitroprussiate-induced
chondrocyte apoptosis by Tougu Xiaotong Capsule-containing serum.
Chin J Integr Med. 17:436–443. 2011. View Article : Google Scholar
|
|
28
|
Goldring MB and Goldring SR:
Osteoarthritis. J Cell Physiol. 213:626–634. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Yuan PW, Liu DY, Chu XD, Hao YQ, Zhu C and
Qu Q: Effects of preventive administration of juanbi capsules on
TNF-alpha, IL-1 and IL-6 contents of joint fluid in the rabbit with
knee osteoarthritis. J Tradit Chin Med. 30:254–258. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Goldring MB and Berenbaum F: The
regulation of chondrocyte function by proinflammatory mediators:
prostaglandins and nitric oxide. Clin Orthop Relat Res. 427(Suppl):
S37–S46. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Smith RL, Allison AC and Schurman DJ:
Induction of articular cartilage degradation by recombinant
interleukin 1 alpha and 1 beta. Connect Tissue Res. 18:307–316.
1989. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Fernandes JC, Martel-Pelletier J and
Pelletier JP: The role of cytokines in osteoarthritis
pathophysiology. Biorheology. 39:237–246. 2002.PubMed/NCBI
|
|
33
|
Stöve J, Huch K, Günther KP and Scharf HP:
Interleukin-1beta induces different gene expression of stromelysin,
aggrecan and tumor-necrosis-factor-stimulated gene 6 in human
osteoarthritic chondrocytes in vitro. Pathobiology. 68:144–149.
2000.PubMed/NCBI
|
|
34
|
Porée B, Kypriotou M, Chadjichristos C, et
al: Interleukin-6 (IL-6) and/or soluble IL-6 receptor
down-regulation of human type II collagen gene expression in
articular chondrocytes requires a decrease of Sp1. Sp3 ratio and of
the binding activity of both factors to the COL2A1 promoter. J Biol
Chem. 283:4850–4865. 2008.
|
|
35
|
Saklatvala J: Tumour necrosis factor alpha
stimulates resorption and inhibits synthesis of proteoglycan in
cartilage. Nature. 322:547–549. 1986. View
Article : Google Scholar : PubMed/NCBI
|
|
36
|
Goldring MB, Fukuo K, Birkhead JR, Dudek E
and Sandell LJ: Transcriptional suppression by interleukin-1 and
interferon-gamma of type II collagen gene expression in human
chondrocytes. J Cell Biochem. 54:85–99. 1994. View Article : Google Scholar : PubMed/NCBI
|