Introduction
Hashimoto’s encephalopathy (HE) is a neurological
complication of autoimmune thyroid disease, which is independent of
thyroid status. HE is also known as steroid-responsive
encephalopathy with autoimmune thyroiditis (1,2). The
condition is more frequently found in females than in males, with a
ratio of ~4:1, however, the occurrence of the disease is not
associated with age. Two types of initial clinical presentation may
be observed for HE. Firstly, a vasculitic type with stroke-like
episodes and mild cognitive impairment; and secondly, a diffuse
progressive type with predominant dementia (3). Since the first report of HE by Brain
et al in 1966 (5), the
majority of HE cases have been shown to be associated with
hypothyroid function. However, HE associated with hyperthyroid
function is very rare (6,7). In the present study, an HE case
associated with hyperthyroid function was reported.
Case report
A 56-year-old female patient that presented with
dysarthria, gait disturbance, somniloquy and delirium was admitted
to the Second Hospital Affiliated to Harbin Medical University
(Harbin, China) in March 2012. Prior written and informed consent
was obtained from the patient and the study was approved by the
Ethics Review Board of Harbin Medical University. The patient had
been diagnosed with hyperthyroidism 14 years previously and had
received bilateral subtotal thyroidectomy surgery 12 years
previously. Following this therapy, the patient had not been
administered any drugs associated with thyroid disease or presented
with hyperthyroidism-associated symptoms. For three months prior to
hospital admission, the patient had been suffering from diarrhea
and weight loss. The condition was treated as colitis gravis and
the symptom of diarrhea was remitting. At the time of admission,
the body temperature of the patient was 36°C, the pulse rate was
159 beats per minute with normal regularity and the blood pressure
was 140/80 mmHg. Neural-system examination revealed dysarthria and
mild attenuation of the muscle force of the limbs without
pathological relax.
Thyroid function tests indicated hyperthyroidism.
Thyroid autoantibodies tests were positive, with particularly high
titrates of anti-thyroid peroxidase antibody (TPO-Ab; Table I). In addition, ultrasonography
revealed that the residual thyroid parenchyma had heterogeneous
echogenicity with an abundant blood flow. Radioiodine uptake was
56% at 3 h and additional biochemical tests were all in a normal
range (Table II). The disease
history, symptoms and laboratory test results supported the
diagnosis of hyperthyroidism. However, after two weeks of
antihyperthyroidism treatment, there had been no decrease in the
neurological/psychiatric symptoms.
 | Table IThyroid function test results at the
baseline and during the one-year follow-up. |
Table I
Thyroid function test results at the
baseline and during the one-year follow-up.
| Time points | FT3
(pmol/l) (2.63–5.7) | FT4
(pmol/l) (9.01–19.5) | TSH (μIU/l)
(0.35–4.94) | Tg-Ab (IU/ml)
(0–4.11) | Tpo-Ab (IU/ml)
(0–5.61) |
|---|
| Mar 12, 2012 | 35.44 | 61.23 | 0.0010 | 20.56 | 905.58 |
| May 27, 2012 | 6.93 | 33.99 | 0.012 | 5.67 | 350.38 |
| Aug 26, 2012 | 5.45 | 14.36 | 0.0380 | 9.87 | 550.32 |
| Nov 14, 2012 | 6.86 | 19.17 | 0.0011 | 40.97 | >1000 |
| Jan 12, 2013 | 4.59 | 16.67 | 0.23 | 8.32 | 458.9 |
| May 2, 2013 | 3.78 | 15.67 | 1.34 | 7.78 | 256.45 |
 | Table IILaboratory test results of the
patients. |
Table II
Laboratory test results of the
patients.
| Investigations | Results | Reference range |
|---|
| Hemoglobin (g/l) | 129 | 120–150 |
| Creatinine
(μmol/l) | 59 | 49–110 |
| Aspartate
aminotransferase (IU/l) | 26 | 0–40 |
| Alkaline phosphatase
(U/l) | 92 | 35–150 |
| Serum potassium
(mmol/l) | 4.36 | 3.5–5.5 |
| Serum calcium
(mmol/l) | 2.2 | 2.1–2.7 |
| Serum magnesium
(mmol/l) | 1.03 | 0.7–1.25 |
| Fasting plasma
glucose (mmol/l) | 4.9 | 3.9–6.1 |
| ANCA | <1:10 | 1:10 |
| ANA | Negative | <1:100 |
| RF (IU/ml) | 12.2 | 0–15 |
| CRP (mg/ml) | 4.32 | 0–5 |
| Anti-HIV-1/-2 | Negative | - |
| HbsAg | Negative | - |
| CEA (ng/ml) | 3.1 | <5 |
| TRAB (IU/ml) | 42.89 | 0.11–30 |
| Cerebrospinal
fluid |
| Protein
(mmol/l) | 1056 | 150–450 |
| Glucose
(mmol/l) | 3.6 | 2.8–4.4 |
| Culture | Negative | - |
| Gram stain | Negative | - |
| TPO-Ab | Positive | - |
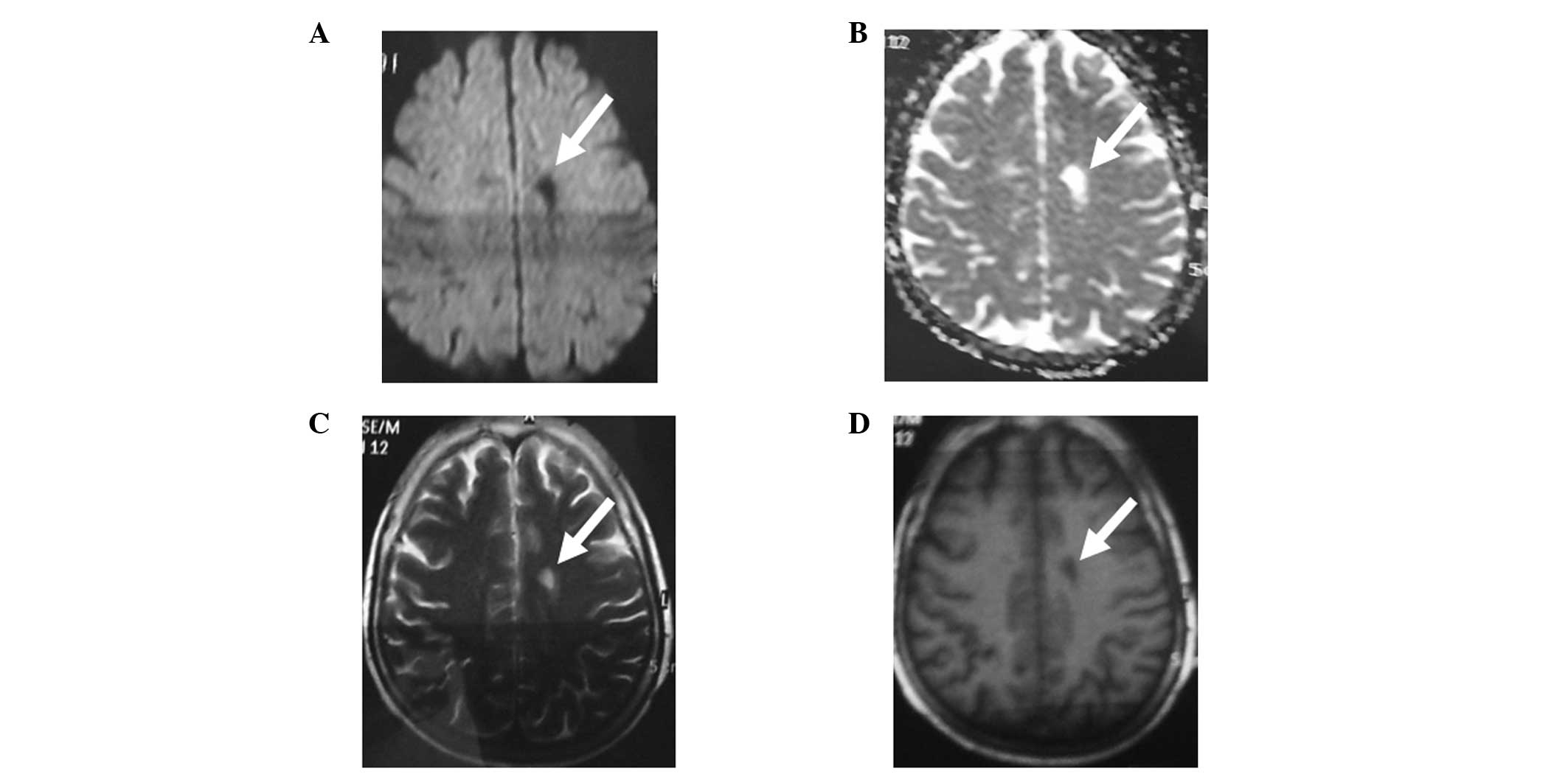
Magnetic resonance imaging (MRI) of the brain
revealed that there was a soft focus at the site of the commissural
magna cerebri and the signals of intracranial artery vessels were
rigor, uneven and inconsistent (Fig.
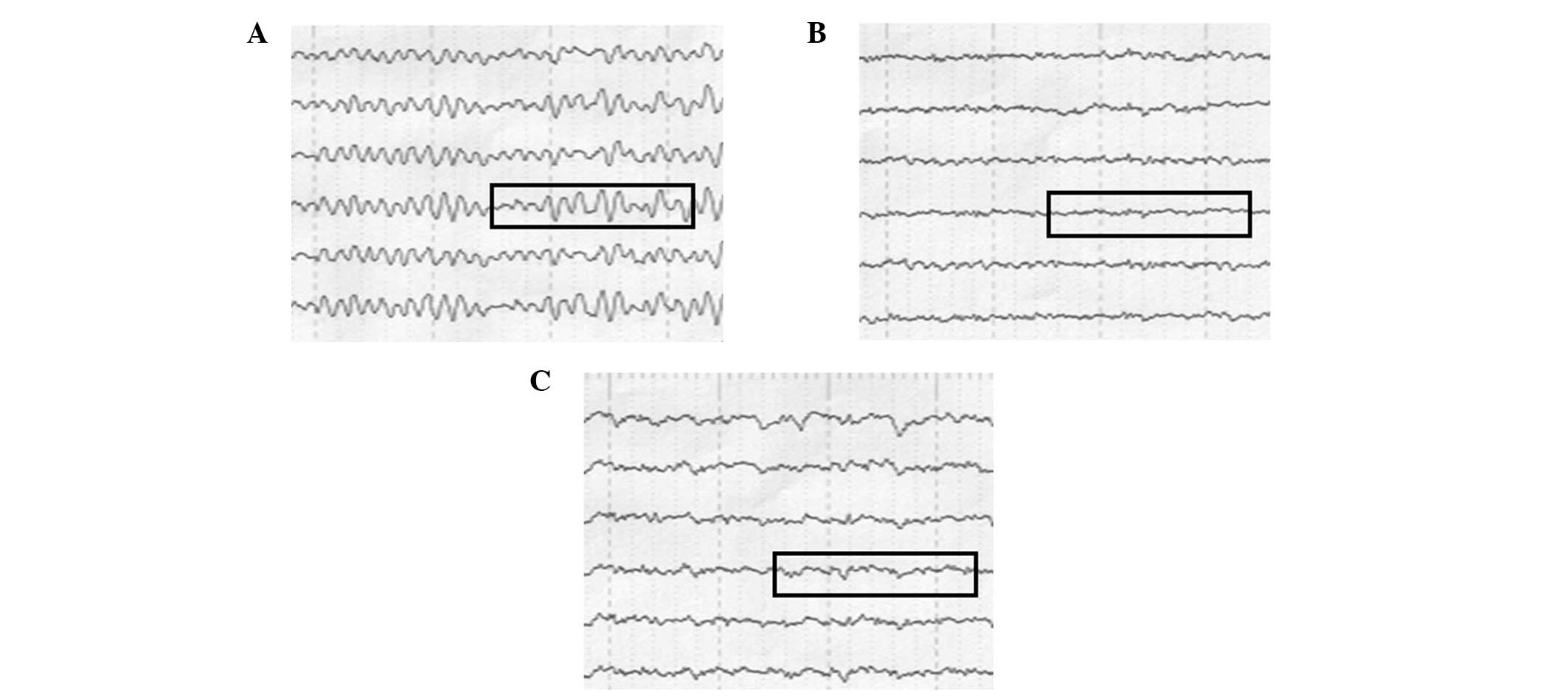
1). Electroencephalogram (EEG) images showed a high-power θ
wave at the central region of the frontal region and diffuse slow
waves (Fig. 2A). In addition,
cerebrospinal fluid tests revealed that the concentration of
protein was high and that there were no cells. The assay for TPO-Ab
was positive in the cerebrospinal fluid (Table I), which confirmed the diagnosis of
HE. After three days of methylprednisolone (500 mg/day)
administration, the symptoms of somniloquy and delirium
disappeared. In addition, the dysarthria and motor function
improved and the patient was able to walk when aided by another
person. The steroid agent was changed to oral prednisolone with a
first dose of 30 mg/day (Table
III) and the patient was administered corticosteroid drugs for
almost three months (Table III).
The neurological/psychiatric symptoms recovered and there was no
recurrence during the one-year follow-up investigation. EEG
examinations at the two-month and one-year follow-ups revealed no
abnormal changes, with the exception of certain slow waves
(Fig. 2B and C). The patient
continued to receive antihyperthyroidism treatment with Methimazole
(5 mg/day) while the titrates of TPO-Ab remained at a high level,
despite exhibiting euthyroid function (Table I). The daily life of the patient
was independent and housework was performed freely. The results
indicated that the treatment administered was effective for this
rare case of HE.
 | Table IIISteroid treatments for the
patient. |
Table III
Steroid treatments for the
patient.
| Treatments
(mg/days) | Duration (days) |
|---|
| Intravenous pulse
methylprednisolone |
| 500 | 3 |
| Dose of oral
prednisolone |
| 30 | 10 |
| 25 | 10 |
| 20 | 10 |
| 15 | 10 |
| 10 | 10 |
| 5 | 30 |
Discussion
A rare case of HE associated with hyperthyroidism
was reported in the present study. Although at first the patient
was suspected to have thyrotoxic psychosis, increasing evidence,
including results from the brain MRI, EEG, cerebrospinal fluid
tests and steroid responsiveness, supported the diagnosis of a rare
cases of HE that was associated with hyperthyroidism. HE is
commonly characterized by neurological/psychiatric symptoms, high
levels of anti-thyroid antibodies, non-specific radiological
examinations or EEG abnormalities and responsiveness to
corticosteroid treatment. The case reported in the present study
complied with all the aforementioned symptoms. Previously, a
specific HE case was shown to be clinically and biochemically
euthyroid, exhibiting onset symptoms similar to presenile dementia
(8).
With regard to the current case, the TPO-Ab assay
was also positive in the cerebrospinal fluid, which may be more
sensitive compared with serum antibody detection. Although the role
of thyroid autoantibodies is unclear, HE is a type of autoimmune
encephalopathy. The majority of patients respond to treatment with
steroids, while certain patients undergo spontaneous remission
without steroid administration (9)
and other patients fail to improve with steroid treatment (10). Although HE is a rare disease, the
condition typically represents autoimmune encephalopathy. In the
present study, the one-year follow-up results indicated that the
treatment administered for this rare HE case was effective.
References
|
1
|
Chong JY, Rowland LP and Utiger RD:
Hashimoto encephalopathy: syndrome or myth? Arch Neurol.
60:164–171. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Shaw PJ, Walls TJ, Newman PK, et al:
Hashimoto’s encephalopathy: a steroid-responsive disorder
associated with high anti-thyroid antibody titers - report of 5
cases. Neurology. 41:228–233. 1991.
|
|
3
|
Kothbauer-Margreiter I, Sturzenegger M,
Komor J, Baumgartner R and Hess CW: Encephalopathy associated with
Hashimoto thyroiditis: diagnosis and treatment. J Neurol.
243:585–593. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Mocellin R, Walterfang M and Velakoulis D:
Hashimoto’s encephalopathy: epidemiology, pathogenesis and
management. CNS Drugs. 21:799–811. 2007.
|
|
5
|
Brain L, Jellinek EH and Ball K:
Hashimoto’s disease and encephalopathy. Lancet. 2:512–514.
1966.
|
|
6
|
Ngiu CS, Ibrahim NM, Yahya WN, et al: A
case of Hashimoto encephalopathy in a Malay woman with Graves
disease. BMJ Case Rep. 2009:pii: bcr01.2009.1501. 2009.PubMed/NCBI
|
|
7
|
Carlone C, Todini L, Marini I, Majorana M,
et al: Acute psychiatric presentation of steroid-responsive
encephalopathy: the under recognized side of autoimmune
thyroiditis. Riv Psichiatr. 48:169–173. 2013.PubMed/NCBI
|
|
8
|
Chong CS, Leung JL, Wong IH, Ng PW and
Miao MY: Presenile dementia: a case of Hashimoto’s encephalopathy.
East Asian Arch Psychiatry. 21:32–36. 2011.
|
|
9
|
Li L, Zheng FP, Wang G and Li H: Recurrent
Hashimoto’s encephalopathy, showing spontaneous remission: a case
report. Intern Med. 50:1309–1312. 2011.
|
|
10
|
Flanagan EP, McKeon A, Lennon VA, et al:
Autoimmune dementia: clinical course and predictors of
immunotherapy response. Mayo Clin Proc. 85:881–897. 2010.
View Article : Google Scholar : PubMed/NCBI
|