Introduction
Left ventricular (LV) contractile function
indicators, including ejection fraction (EF) and LV size,
contribute to diagnosis (1,2),
prognosis (3–5) and treatment (1,2,5,6) in
patients with congestive heart failure (CHF). LVEF is possibly the
optimal prognostic factor in patients with HF (2–7). The
LV size is well-established as an independent predictor of
cardiovascular morbidity and mortality, and is frequently used to
guide patient care (8–10). Although LVEF and LV size can be
readily measured using angiographic, radionuclide, computed
tomography (CT), magnetic resonance imaging or echocardiographic
techniques, these tests are expensive and may not be readily
available in all clinical settings. Non-invasive imaging, such as
chest radiography (CR), is an essential component of the diagnostic
work-up and follow-up assessment of all cardiac disease.
The cardiothoracic ratio (CTR) derived from CR is
traditionally used to estimate LV size (11,12)
and is associated with LV systolic dysfunction (13,14).
A high CTR, estimated by CR, is a marker of cardiomegaly and has
been shown to be associated with poor outcomes in patients with HF
and congenital heart disease (7,15–17).
However, pilot studies have shown inconsistent associations between
CTR and LV size (12,18–20)
or systolic function (13,14,17,19).
Furthermore, these study results are conflicting and have been
marred by examination method bias (radiograph, radionuclide,
angiographic or echocardiographic) and patient selection (mostly
with depressed LVEF, congenital heart disease, CHF and other
cardiac disease) bias. The association between the CTR and LV
systolic function parameters in patients with preserved LVEF
remains unclear.
The aim of this study was to assess the association
of LV systolic function parameters evaluated by dual source CT
coronary angiography (DSCT-CA) and the CTR derived from CR in
patients with suspected coronary artery disease (CAD) with or
without preserved LVEF. The CTR was hypothesized to have different
correlations with the LV systolic function parameters according to
the value of the CTR and LVEF.
Materials and methods
Study population
The institutional review board approved this
retrospective study and waived the requirement for informed
consent. A total of 203 consecutive patients were involved between
June and October 2010, who were suspected of exhibiting CAD and
underwent CR and DSCT-CA within three weeks. Exclusion criteria
were congenital heart, pericardial, valvular heart and pulmonary
hypertension diseases. The patients were divided into four
subgroups according to the LVEF value (<55%, depressed LVEF
group; and ≥55%, preserved LVEF group) and CTR value (<0.5,
normal range CTR group; and ≥0.5, larger CTR group).
DSCT-CA protocol
All the CT examinations were performed with a DSCT
(Somatom Definition; Siemens Medical Systems, Erlangen, Germany).
Four electrocardiograph (ECG) leads were attached to the chest of
the patient in standard position and the ECG was continuously
recorded throughout the scan. Bolus tracking was used for timing
and scanning automatically started 6 sec after contrast enhancement
reached 100 HU in a region of interest placed in the descending
aorta. The scanner setting was as follows: Tube voltage of 120 kV
and effective tube current of 380 mAs for the two tubes, and ECG
pulsing window of 28–80% of the R-R interval for all the patients.
The pitch was adapted for the lowest expected heart rate during
scanning. Expected scan time was determined prior to scanning by
scan length and pitch. Scan direction was craniocaudal starting
above the coronary ostia and ending at the diaphragm below all the
cardiac structures. High concentration contrast material [370 mg
I/ml iopromide (Ultravist®); Schering AG, Berlin,
Germany] was administered with a mechanical power injector (Dual
Shot; MedRad Inc., Indianola, PA, USA) via a 20-gauge cannula
inserted into an antecubital vein. Subsequent to contrast material
delivery, 40 ml of saline solution was chased at the same rate as
the contrast material. The images were reconstructed
retrospectively using overlapping transversal images and a medium
sharp convolution kernel (B26f) with an image matrix of 512×512
pixels, and slice thickness of 0.75 mm. A total of 10 datasets of
axial images from the entire heart were reconstructed at increments
of 5% of the R-R interval, starting at 5% throughout the cardiac
cycle using a retrospective ECG-gated half-scan algorithm.
Quantitative assessment of LV systolic
function parameters
Following reconstruction, dynamic cardiac
contrast-enhanced DSCT images were transferred to an offline
workstation. LV systolic function parameters were assessed: LV
end-diastolic volume index (LVEDVI), LV end-systolic volume index
(LVESVI), LV stroke volume index (LVSVI), LVEF and cardiac output
(CO), using a semi-automatic software tool (Circulation II; Siemens
Medical Systems) and calculated by the standard cube formula and
indexed to body surface area. The end of the systolic and diastolic
phases was determined by previewing images at the level of the
mitral valve in 5% steps throughout the entire cardiac cycle (0–95%
of the R-R interval). The endocardial and epicardial border
contours were detected automatically and adjusted by manual tracing
when necessary (Fig. 1) in the two
phases. LVEF = (end diastolic − end systolic counts)/end diastolic
counts × 100%. LVSV was calculated as the end diastolic minus the
end systolic volume, and CO was the product of stroke volume and
heart rate.
Quantitative assessment of CTR with
CR
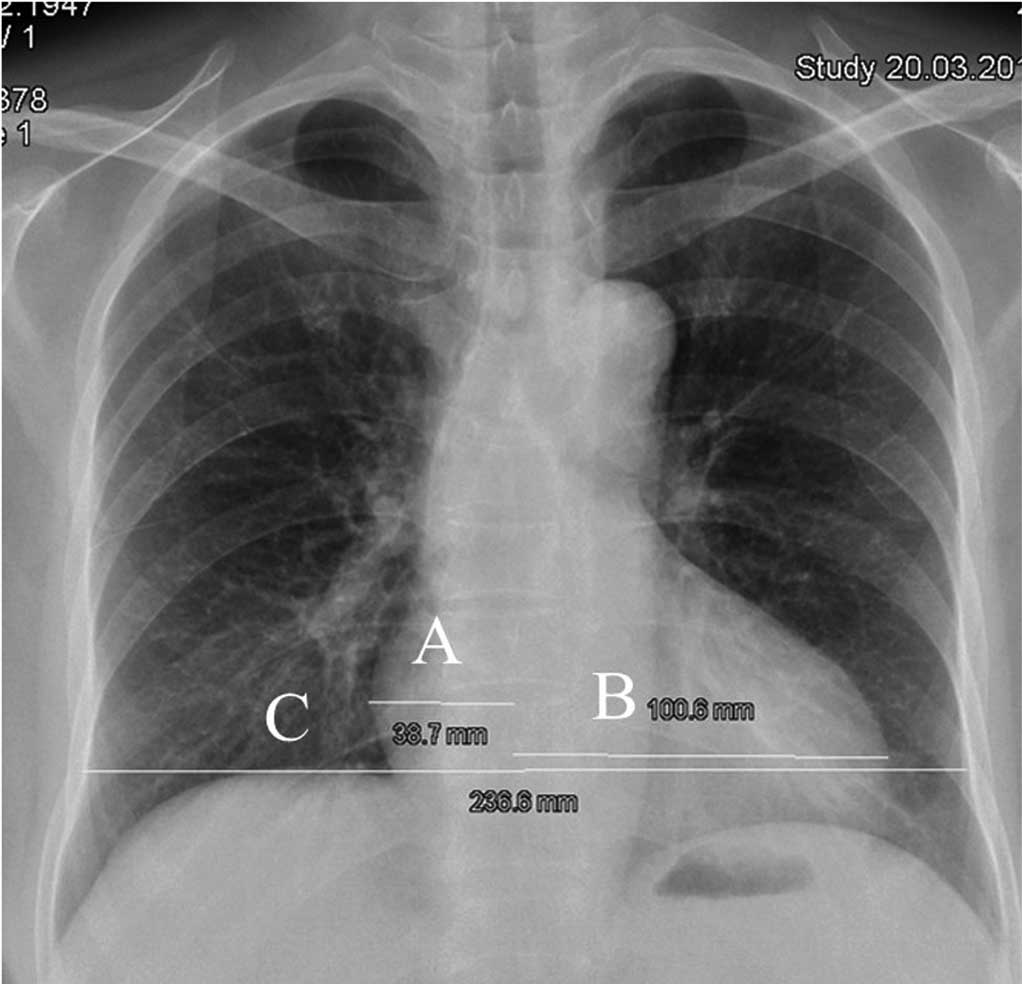
The CTR from the postero-anterior upright position
CR was performed using standard radiological techniques. The CTR
was calculated as the ratio of the maximal transverse diameter of
the cardiac silhouette to the distance between the internal margins
of the ribs at the level of the right hemidiaphragm (Fig. 2).
Determination of the CTR and LV systolic
function parameters
Two experienced observers blinded to the clinical
data of the patient and heart rate during the scan independently
measured the CTR and LV systolic function parameters of the
patients. All the results were estimated by the average of two
observers.
Statistical evaluation
Continuous data were described as the mean ±
standard deviation, and categorical data were described as the
percentage. The analysis was stratified according to the LVEF
(<55% vs. ≥55%) and CTR (<0.5 vs. ≥0.5) values. The CTR and
LV systolic function parameters were compared with the Student’s
t-test between subgroups. Pearson correlation and linear regression
were used to describe the correlation and linear association
between the CTR and LV systolic function parameters. Hypothesis
test values of P<0.05 were considered statistically significant.
Data management and statistical analyses were performed using SAS
V9.1.3 software (SAS Institute Inc., Cary, NC, USA). The
investigators had full access and responsibility for the integrity
of the data.
Results
Patient characteristics
All the examinations were performed without
technical problems, and the image quality was good for the data
analysis in all cases. The study cohort consisted of 203 subjects
that underwent DSCT-CA and CR, including 122 male and 81 female
subjects with an age range of 29–85 (Table I).
 | Table IDemographical and baseline clinical
characteristics of the study cohort. |
Table I
Demographical and baseline clinical
characteristics of the study cohort.
| Characteristics | Statistical
description |
|---|
| Age, years | 60.92±11.66 |
| Male, n | (%) 122 (60.10) |
| Diabetes, n (%) | 56 (27.59) |
| Hypertension, n
(%) | 119 (58.62) |
| Smoke, n (%) | 51 (25.12) |
| Drink, n (%) | 46 (22.66) |
| Heart rate (bpm) | 71.95±12.27 |
| Height, cm | 164.35±8.07 |
| Weight, kg | 66.91±11.12 |
| BMI,
kg/m2 | 24.68±3.21 |
| BSA,
m2 | 1.77±0,18 |
| CTR | 0.51±0.06 |
| LVEDVI,
ml/m2 | 72.78±27.89 |
| LVESVI,
ml/m2 | 25.85±20.93 |
| LVSVI,
ml/m2 | 46.87±12.60 |
| CO, L/min | 5.95±1.72 |
| LVEF, % | 66.72±11.77 |
Comparison of the CTR and LV systolic
function parameters according to the value of the LVEF and CTR
The CTR and LV systolic function parameters, such as
LVEDVI, LVESVI, LVSVI, LVEF and CO, were compared according to the
LVEF (<55% vs. ≥55%) and CTR (<0.5 vs. ≥0.5) values as shown
in Tables II and III. No significant difference was
identified for age, gender and body mass index (BMI) in all the
groups with the exception of male frequency, which was higher in
the normal range CTR group compared to the larger CTR group. The
mean values of the LVEDVI and LVESVI of the depressed LVEF group
were significantly higher than that of the preserved LVEF group
(108.56±57.15 vs. 67.52±14.56 ml/m2, P<0.001 and
64.07±37.81 vs. 20.23±7.23 ml/m2, P<0.001,
respectively). These two mean values in the normal range CTR group
were lower compared with the larger CTR group (67.10±15.00 vs.
77.30±34.32 ml/m2, P=0.009 and 21.94±8.96 vs.
28.97±26.54 ml/m2, P=0.017, respectively). In addition,
no significant difference of CTR and LVEF was identified between
the groups according to the values of LVEF and CTR.
 | Table IIComparison of the CTR and LV systolic
function parameters according to the value of the LVEF for the 203
subjects. |
Table II
Comparison of the CTR and LV systolic
function parameters according to the value of the LVEF for the 203
subjects.
| Characteristics | LVEF <55%
(n=36) | LVEF ≥55%
(n=167) | P-value |
|---|
| Age, years | 57.69±11.34 | 61.39±11.67 | 0.132 |
| Male, n (%) | 20 (76.92) | 102 (57.63) | 0.085 |
| BMI,
kg/m2 | 24.48±3.44 | 24.71±3.18 | 0.728 |
| CTR | 0.53±0.06 | 0.51±0.06 | 0.083 |
| LVEDVI,
ml/m2 | 108.56±57.15 | 67.52±14.56 | <0.001 |
| LVESVI,
ml/m2 | 64.07±37.81 | 20.23±7.23 | <0.001 |
| LVSVI,
ml/m2 | 44.07±22.89 | 47.28±10.32 | 0.226 |
| CO, L/min | 6.14±2.89 | 5.92±1.48 | 0.536 |
| LVEF, % | 42.92±8.78 | 70.22±7.21 | <0.001 |
 | Table IIIComparison of the CTR and LV function
parameters according to the value of the CTR for the 203
subjects. |
Table III
Comparison of the CTR and LV function
parameters according to the value of the CTR for the 203
subjects.
|
Characteristics | CTR <0.5
(n=90) | CTR ≥0.5
(n=113) | P-value |
|---|
| Age, years | 58.84±10.80 | 61.57±12.10 | 0.082 |
| Male, n (%) | 65 (72.22) | 57 (50.44) | 0.005 |
| BMI,
kg/m2 | 23.81±2.98 | 25.38±3.23 | 0.332 |
| CTR | 0.45±0.03 | 0.55±0.05 | <0.001 |
| LVEDVI,
ml/m2 | 67.10±15.00 | 77.30±34.32 | 0.009 |
| LVESVI,
ml/m2 | 21.94±8.96 | 28.97±26.54 | 0.017 |
| LVSVI,
ml/m2 | 45.15±10.80 | 48.24±13.77 | 0.083 |
| CO, L/min | 5.79±1.35 | 6.07±1.96 | 0.250 |
| LVEF, % | 67.61±9.30 | 66.02±13.41 | 0.339 |
Association between the CTR and LV
systolic function parameters
The correlation between the CTR and LV systolic
function parameters, including LVEDVI, LVESVI and LVEF, according
to the value of LVEF and CTR are provided in Tables IV and V. Significant correlations were found
between the CTR and LVEDVI, LVESVI and LVEF (r=0.66, P<0.001;
r=0.65, P<0.001; and r=−0.46, P=0.018, respectively) in the
depressed LVEF group. The CTR exhibited a weak correlation with
LVEDVI and LVESVI (r=0.25, P<0.001; and r=0.21, P=0.002,
respectively) in the overall groups. However, there was no
significant association determined between CTR and LV systolic
function parameters in the other subgroups.
 | Table IVCorrelation between the CTR and the
different measures of LV function for the 203 subjects, as
stratified by LVEF. |
Table IV
Correlation between the CTR and the
different measures of LV function for the 203 subjects, as
stratified by LVEF.
| LVEF <55%
(n=36) | LVEF ≥55%
(n=167) | Overall
(n=203) |
|---|
|
|
|
|
|---|
| CTR | LVEF (%) | CTR | LVEF (%) | CTR | LVEF (%) |
|---|
|
|
|
|
|
|
|
|---|
| Group variable | r | P-value | r | P-value | r | P-value | r | P-value | r | P-value | r | P-value |
|---|
| LVEDVI,
ml/m2 | 0.66 | <0.001 | −0.47 | 0.009 | 0.05 | 0.535 | −0.15 | 0.023 | 0.25 | <0.001 | −0.52 | <0.001 |
| LVESVI,
ml/m2 | 0.65 | <0.001 | −0.72 | <0.001 | 0.04 | 0.566 | −0.77 | <0.001 | 0.21 | 0.002 | −0.81 | <0.001 |
| LVEF, % | −0.46 | 0.018 | | | −0.10 | 0.175 | | | −0.08 | 0.244 | | |
 | Table VCorrelation between the CTR and the
different measures of LV function for the 203 subjects who
underwent CR and DSCT-CA, as stratified by CTR. |
Table V
Correlation between the CTR and the
different measures of LV function for the 203 subjects who
underwent CR and DSCT-CA, as stratified by CTR.
| CTR <0.5
(n=90) | CTR≥0.5
(n=113) |
|---|
|
|
|
|---|
| CTR | LVEF (%) | CTR | LVEF (%) |
|---|
|
|
|
|
|
|---|
| Group variable | r | P-value | r | P-value | r | P-value | r | P-value |
|---|
| LVEDVI,
ml/m2 | 0.20 | 0.053 | −0.15 | 0.151 | 0.16 | 0.086 | −0.62 | <0.001 |
| LVESVI,
ml/m2 | 0.11 | 0.299 | −0.79 | <0.001 | 0.15 | 0.125 | −0.85 | <0.001 |
| LVEF, % | −0.02 | 0.879 | | | −0.07 | 0.461 | | |
Association between the LV volume index
and LVEF
With regard to the association between LVEDVI and
LVESVI and LVEF, significant negative correlations were observed in
the overall group and nearly all the subgroups with the exception
of the normal range CTR group in which LVEDVI was not correlated
with LVEF (Tables IV and V). Notably, the correlation was stronger
between LVESVI and LVEF compared to that between LVEDVI and
LVEF.
Discussion
CR is commonly used as an initial test for the
diagnosis of heart size and systolic dysfunction, particularly in
general practice. The present study indicates that CTR derived from
CR directly was associated with LV volume index and LVEF in
patients suspected of having CAD with depressed LVEF as opposed to
with preserved LVEF. To the best of our knowledge, this is the
first demonstration regarding the correlation between CTR and LV
systolic function parameters measured in patients according to the
value of LVEF without congenital heart, pericardial, valvular heart
and pulmonary hypertension diseases.
The correlation between CTR and the LV volume or
diameter is known to be controversial in previous studies.
Hemingway et al (21) and
Clark et al (19) reported
a modest to high positive correlation in patients with various
heart diseases. An opposing conclusion has been reported in another
study, which was that CTR was not correlated with LV volume in
patients with acute chest pain (20). The present data indicated that
LVEDVI and LVESVI values were higher in the larger CTR group, and
showed an improved correlation between CTR and LV volume index in
the depressed compared with the preserved LVEF group. One possible
explanation is that the CTR measures depend on the transverse
dimension of the cardiac and thoracic silhouette. The cardiac
silhouette on a chest film encompasses all the contents of the
pericardium. As shown in Fig. 2,
the transverse dimension of the cardiac silhouette, which forms the
numerator of the CTR, is predominantly affected by the right atrium
size, the internal dimension of the left ventricle, the thickness
of the LV wall, pericardial thickness and the contents of the
pericardial space. The geometry of the thoracic shape is influenced
by factors, including pneumonectasis and thoracic collapse, which
are associated with pleurisy. Therefore, CTR should be regarded as
an unspecific marker for LV size enlargement with questionable
clinical value, particularly in congenital heart, pericardial,
valvular heart and pulmonary hypertension diseases. However,
patients with CAD or hypertrophic cardiomyopathy (HCM) and
depressed LVEF often present with LV myocardial infarction and LV
remodeling that cause dilatation of the left ventricle. When
depressed patients with LVEF were evaluated and other associated
diseases were excluded, the LV volume was shown to possibly be an
important factor of CTR value. Of note, several studies have
demonstrated a high correlation between LVEDV and LV size (20,22).
Thus, the CTR can be a marker of LV size enlargement in patients
with depressed LVEF rather than preserved LVEF or other associated
heart diseases.
Clinicians have extrapolated that the CTR can be
used to predict LV systolic function or predict the independent
mortality risk in patients with CHF or congenital heart disease
(2,17). The study by Cohn et al
(13) demonstrated a modest
negative correlation between CTR and EF among 584 male patients
with chronic CHF and low EF enrolled in V-HeFT (vasodilator-heart
failure trials) I (r=−0.27) and 758 male patients enrolled in
V-HeFT II (r=−0.28). Rose and Stolberg (23) reported a negative correlation
(r=−0.22) between CTR and angiographic EF among 256 subjects that
underwent cardiac catheterization. The present findings have shown
an improved correlation (r=−0.46) between CTR and LVEF compared to
the previous studies in the patients with depressed LVEF. However,
the correlation between CTR and LVEF was poor in the patients with
preserved LVEF regardless of whether the CTR was small or
large.
Certain clinical variables may interfere with the
association between CTR and LV systolic function. Patients with HF
and enlarged heart shadow, which includes cavity dimension and wall
thickness, may still have preserved LVEF (24,25).
For instance, an increased CTR due to hypertrophy may be associated
with low, normal or high EF in patients with HF caused by
hypertensive and HCM heart disease. In addition, patients with
valvular heart disease may have a varied and complex association
between CTR and LVEF. For example, there are distinct differences
between the classic patterns of chamber enlargement and LV
contractile function in patients with primary mitral stenosis and
regurgitation. Another possible explanation for the weak
association between CTR and EF lies with the variable distortion of
the right atrial and ventricular morphological characteristics and
function (26), which can occur in
any given LVEF among patients with CHF. Therefore, it can be argued
that LVEF can be normal in the presence of a grossly abnormal heart
size. Although patients with known valvular heart disease were not
included in the present study, the CTR demonstrated no significant
difference according to the LVEF value and compelling evidence was
obtained that CTR was not able to be reliably used to estimate LV
systolic function in individual patients with preserved LVEF.
However, for patients in the later stages of CAD,
dilated cardiomyopathy or HCM often present with LV myocardial
infarction and remodeling, which usually cause LV dilatation and
LVEF decrease. Any degree of cardiomegaly observed on the CTR is a
risk factor in these patients. Although CTR is not helpful in all
patients, it could play an important role in the assessment of LV
systolic dysfunction and the sequential follow-up of patients with
depressed LVEF.
By contrast, a strong association between LV volume
index and LVEF was observed in the patients in the present study.
In the majority of patients with chronic left-sided CHF, LV
systolic function decreases, filling pressure increases and the
chamber dilates (27). Dilation
and/or hypertrophy of other cardiac chambers may also occur. Thus,
patients with CHF generally have a larger LV size. A negative
correlation has been described between the three-dimensional
cardiac volume derived from CR and LVEF (12). Increased LV dimensions and systolic
dysfunction have been shown to be powerful predictors of mortality
in patients with cardiac diseases (8,28).
Previously, it has been well observed that LV dilatation occurs
when LV systolic function or contractile state (29) is compromised. In the present study,
although the LVEDVI or LVESVI was not able to represent LV size, a
negative correlation has been described between LV volume index,
particularly LVESVI and LVEF.
The present study had several limitations. Firstly,
this was a retrospective study and it was not possible to be
certain of the standardization for CR position. A poor inspiration
and the shape of the heart could make a falsely raised CTR.
However, the wide scatter of the points indicated that this was not
a systematic error. Secondly, in the present study, LVEDVI and
LVESVI were regarded as indexes to predict LV size without
considering LV wall thickness. Although there is a high correlation
between LVEDVI and LV size (20,22),
LV wall thickness occasionally plays an important role in LV size
enlargement. Thirdly, stratification for cardiac function was not
conducted in this study. Finally, the population of the depressed
LVEF was smaller than that of the preserved LVEF group.
In conclusion, the present data shows an improved
correlation between CTR and LV systolic function and volume index
in patients with depressed LVEF compared with preserved LVEF. LV
volume index is inversely correlated with LVEF in all the patients.
Thus, the CTR as measured on the CR is not able to distinguish
between patients with depressed or preserved LV function, but may
have a role in predicting the degree of LV dysfunction and
ventricular enlargement only once LV function has been reduced.
Acknowledgements
The present study was supported by a project funded
by the Priority Academic Program Development of Jiangsu Higher
Education Institutions (grant no. JX10231801), National Natural
Science Foundation of China (grant no. 81101104) and Natural
Science Foundation of Jiangsu Province (grant no. BK2012743).
References
|
1
|
No authors listed. Guidelines for the
evaluation and management of heart failure. Report of the American
College of Cardiology/American Heart Association Task Force on
Practice Guidelines (Committee on Evaluation and Management of
Heart Failure). Circulation. 92:2764–2784. 1995. View Article : Google Scholar
|
|
2
|
Goldsmith SR and Dick C: Differentiating
systolic from diastolic heart failure: pathophysiologic and
therapeutic considerations. Am J Med. 95:645–655. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Cohn JN and Rector TS: Prognosis of
congestive heart failure and predictors of mortality. Am J Cardiol.
62:25A–30A. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Keogh AM, Baron DW and Hickie JB:
Prognostic guides in patients with idiopathic or ischemic dilated
cardiomyopathy assessed for cardiac transplantation. Am J Cardiol.
65:903–908. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Cintron G, Johnson G, Francis G, Cobb F
and Cohn JN: Prognostic significance of serial changes in left
ventricular ejection fraction in patients with congestive heart
failure. The V-HeFT VA Cooperative Studies Group. Circulation.
87:VI17–VI23. 1993.PubMed/NCBI
|
|
6
|
Cohn JN, Archibald DG, Francis GS, et al:
Veterans Administration. Cooperative Study on Vasodilator Therapy
of Heart Failure: influence of prerandomization variables on the
reduction of mortality by treatment with hydralazine and isosorbide
dinitrate. Circulation. 75:IV49–IV54. 1987.
|
|
7
|
Kearney MT, Fox KA, Lee AJ, et al:
Predicting sudden death in patients with mild to moderate chronic
heart failure. Heart. 90:1137–1143. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lee TH, Hamilton MA, Stevenson LW, et al:
Impact of left ventricular cavity size on survival in advanced
heart failure. Am J Cardiol. 72:672–676. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
White HD, Norris RM, Brown MA, Brandt PW,
Whitlock RM and Wild CJ: Left ventricular end-systolic volume as
the major determinant of survival after recovery from myocardial
infarction. Circulation. 76:44–51. 1987.PubMed/NCBI
|
|
10
|
Woo P, Mao S, Wang S and Detrano RC: Left
ventricular size determined by electron beam computed tomography
predicts significant coronary artery disease and events. Am J
Cardiol. 79:1236–1238. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Laczkovics A, Grabenwöger F, Teufelsbauer
H, Dock W, Wollenek G and Wolner E: Noninvasive assessment of acute
rejection after orthotopic heart transplantation: value of changes
in cardiac volume and cardiothoracic ratio. J Cardiovasc Surg
(Torino). 29:582–586. 1988.
|
|
12
|
Hammermeister KE, Chikos PM, Fisher L and
Dodge HT: Relationship of cardiothoracic ratio and plain film heart
volume to late survival. Circulation. 59:89–95. 1979.PubMed/NCBI
|
|
13
|
Cohn JN, Johnson GR, Shabetai R, et al:
Ejection fraction, peak exercise oxygen consumption, cardiothoracic
ratio, ventricular arrhythmias, and plasma norepinephrine as
determinants of prognosis in heart failure. The V-HeFT VA
Cooperative Studies Group. Circulation. 87(6 Suppl): VI5–VI16.
1993.
|
|
14
|
Bertolet BD, Freund G, Martin CA,
Perchalski DL, Williams CM and Pepine CJ: Unrecognized left
ventricular dysfunction in an apparently healthy alcohol abuse
population. Drug Alcohol Depend. 28:113–119. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ernst ER, Shub C, Bailey KR, Brown LR and
Redfield MM: Radiographic measurements of cardiac size as
predictors of outcome in patients with dilated cardiomyopathy. J
Card Fail. 7:13–20. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Giamouzis G, Sui X, Love TE, Butler J,
Young JB and Ahmed A: A propensity-matched study of the association
of cardiothoracic ratio with morbidity and mortality in chronic
heart failure. Am J Cardiol. 101:343–347. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Dimopoulos K, Giannakoulas G, Bendayan I,
et al: Cardiothoracic ratio from postero-anterior chest
radiographs: a simple, reproducible and independent marker of
disease severity and outcome in adults with congenital heart
disease. Int J Cardiol. 166:453–457. 2013. View Article : Google Scholar
|
|
18
|
Chikos PM, Figley MM and Fisher L:
Correlation between chest film and angiographic assessment of left
ventricular size. AJR Am J Roentgenol. 128:367–373. 1977.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Clark AL and Coats AJ: Unreliability of
cardiothoracic ratio as a marker of left ventricular impairment:
comparison with radionuclide ventriculography and echocardiography.
Postgrad Med J. 76:289–291. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Schlett CL, Kwait DC, Mahabadi AA, et al:
Simple area-based measurement for multidetector computed tomography
to predict left ventricular size. Eur Radiol. 20:1590–1596. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hemingway H, Shipley M, Christie D and
Marmot M: Cardiothoracic ratio and relative heart volume as
predictors of coronary heart disease mortality. The Whitehall study
25 year follow-up. Eur Heart J. 19:859–869. 1998.PubMed/NCBI
|
|
22
|
Wiese TH, Rogalla P, Taupitz M, et al:
Assessment of left ventricular volumes and function:
intraindividual comparison of multi-slice spiral CT and electron
beam CT in an animal model. Acta Radiol. 45:819–827.
2004.PubMed/NCBI
|
|
23
|
Rose CP and Stolberg HO: The limited
utility of the plain chest film in the assessment of left
ventricular structure and function. Invest Radiol. 17:139–144.
1982. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Owan TE, Hodge DO, Herges RM, et al:
Trends in prevalence and outcome of heart failure with preserved
ejection fraction. N Engl J Med. 355:251–259. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Maeder MT and Kaye DM: Heart failure with
normal left ventricular ejection fraction. J Am Coll Cardiol.
53:905–918. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Jaffe CC and Weltin G: Echocardiography of
the right side of the heart. Cardiol Clin. 10:41–57.
1992.PubMed/NCBI
|
|
27
|
Parmley WW: Pathophysiology and current
therapy of congestive heart failure. J Am Coll Cardiol. 13:771–785.
1989. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Fleischmann KE, Goldman L, Robiolio PA, et
al: Echocardiographic correlates of survival in patients with chest
pain. J Am Coll Cardiol. 23:1390–1396. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Galderisi M, Lauer MS and Levy D:
Echocardiographic determinants of clinical outcome in subjects with
coronary artery disease (the Framingham Heart Study). Am J Cardiol.
70:971–976. 1992. View Article : Google Scholar : PubMed/NCBI
|