Introduction
Tuberous sclerosis complex (TSC) is a common genetic
disorder that results in aberrant cellular differentiation,
proliferation and migration early in life (1). TSC occurs in one out of 6,000
newborns and has affected an estimated 1 million individuals
globally (2). The condition is
characterized by the development of benign tumors in numerous
organs (1,3), including the skin (facial
angiofibromas), kidney (angiomyolipomas and cysts), lung
(lymphangioleiomyomatosis), brain (subependymal giant cell
astrocytomas and epileptogenic tuber), heart (rhabdomyomas) and
retina (optic nerve tumor) (4–7).
These tumors all have the potential to severely affect organ
function.
Recent research has revealed the pathogenic
mechanism underlying TSC. Mutations in either TSC1 or
TSC2, which encode hamartin and tuberin, respectively, cause
the abnormal activation of mammalian target of rapamycin (mTOR)
(8,9). Hyperactivation of the mTOR pathway,
leading to increased cell growth and proliferation, stimulates
tumor growth in the brain and other organs in patients with TSC.
There are increasing numbers of studies documenting the use of mTOR
inhibitors, such as rapamycin, for the treatment of patients with
TSC (10,11). These mTOR inhibitors are
potentially promising for the treatment of multiple TSC-related
tumor types, including renal angiomyolipomas, subependymal giant
cell astrocytomas and lymphangioleiomyomatosis (12–18).
The efficacy and safety of mTOR inhibitor therapy in
pediatric patients with TSC remain unclear, particularly as a
limited response to mTOR inhibitor therapy and drug-related adverse
reactions have been reported (19). Given the uncertainty over the
treatment effects of mTOR inhibitor and the difficulties in the
interpretation of the clinical studies, we therefore carried out a
systematic review to assess the efficacy and safety of mTOR
inhibitor in the treatment of children with TSC.
Materials and methods
Inclusion criteria
This review was reported according to the Preferred
Reporting Items for Systematic Reviews and Meta-Analysis statement
issued in 2009 (Checklist S1) (20). Quasi-randomized controlled trials
(RCTs), case series or case reports comparing any mTOR inhibitor
therapy versus placebo or any pretreatment status were included.
Studies that were not published as full reports, such as conference
abstracts and letters to editors, were excluded. Outcome measures
were evaluated by response rates and the incidence of adverse
events.
Search methods for study
identification
The PubMed, EmBase and Cochrane Library databases
were systematically searched from database inception to July 2013.
The search included the following terms: mTOR inhibitor OR
rapamycin OR everolimus OR sirolimus AND tuberous sclerosis. In
addition, the reference lists of the identified reports, reviews
and other relevant publications were manually searched to find
other pertinent studies. The medical subject heading, methods,
population, study design, intervention and outcome variables of
these articles were used to identify relevant studies.
Data collection and analysis
Two review authors independently examined the titles
and abstracts to select eligible studies, and the full texts of the
potentially relevant studies were retrieved. Two review authors
then independently extracted information from the eligible studies.
Data included the first author of the study, sample size, gender,
age, disease status, interventions, duration of the follow-up
periods, treatment outcomes and adverse reactions. Disagreements
concerning study inclusion were resolved through consensus and
group discussion.
Assessment of heterogeneity
Clinical heterogeneity between included studies was
assessed by comparing the distribution of important participant
factors (e.g. age and gender) between studies and study factors
(e.g. loss to follow-up and treatment regimens). Heterogeneity was
assessed using the χ2 test and I2 statistic
(21). The χ2 test
value was interpreted as significant when P<0.1. The
I2 statistic was interpreted as recommended by Higgins
and Green (22): 0–40%,
heterogeneity may not be important; 30–60%, heterogeneity may be
moderate; 50–90%, heterogeneity may be substantial; and 75–100%,
considerable heterogeneity (Higgins 2011). If substantial or
considerable heterogeneity was present i.e. P<0.1,
I2≥50%, the origin of the heterogeneity was
evaluated.
Statistical analysis
A sensitivity analysis was performed to explore the
impact of excluding outlying results. Treatment effects were
obtained from the number of events reported in each group. The
Mantel-Haenszel method was used to evaluate the treatment effect
(23,24). Dichotomous data were synthesized
using risk ratios. A P-value of 0.05 was used as the cut-off value
to determine statistical significance, and data are presented as
the estimated effect with 95% confidence intervals (CIs). All
statistical analyses were calculated using STATA software (version
12.0; Stata Corp. LP, College Station, TX, USA).
Results
Study characteristics
The characteristics of the included studies
(13–19,25–28)
are listed in Table I. The initial
search retrieved a total of 1,046 potentially relevant
publications. The titles and abstracts of the studies were screened
and 33 were found to be potentially eligible for inclusion. The
full text articles of these 33 studies were retrieved. Subsequent
to reading the full texts, 11 studies were found eligible for
inclusion according to the criteria for acceptable studies for this
review (Fig. 1). The eligible
studies reported outcomes on a total of 129 pediatric patients with
TSC (<18 years of age). The majority of cases (n=96, 74.4%)
received mTOR inhibitor therapy, while the remaining cases (n=33,
25.6%) were treated with non-mTOR inhibitor therapy (Table I). The follow-up for the patients
who received mTOR inhibitor ranged between 3.0 and 16.0 months. Ten
of the included studies (13–19,26–28)
were case series or case reports; the remaining study was an RCT
(24). Of the 33 clinical studies
that were relevant to mTOR inhibitor therapy in the patients with
TSC, 22 were excluded: 16 studies were excluded as they did not
include pediatric patients and six were excluded as they did not
include outcomes of interest.
 | Table ICharacteristics of the 11 studies
included in the meta-analysis. |
Table I
Characteristics of the 11 studies
included in the meta-analysis.
| First author, year
(ref.) | Sample size
(MC/NC) | Gender (M/F) | Age (years) | Inclusion
criteria | Interventiona | Follow-up
(months) |
|---|
| Franz, 2013 (24) | 68/33 | NR | 1.0–18.0 | Subependymal giant
cell astrocytomas associated with TSC | Everolimus | 9.7 |
| Foster, 2012
(25) | 4/0 | 2/2 | 5.0–17.0 | Facial
angiofibromas associated with TSC | Sirolimus | 6.0 |
| Salido, 2012
(26) | 7/0 | 4/3 | 6.0–14.0 | Facial
angiofibromas associated with TSC | Sirolimus | 9.0 |
| Sparagana, 2010
(19) | 1/0 | 0/1 | 12.0 | Optic nerve tumor
associated with TSC | Sirolimus | 16.0 |
| Pressey, 2010
(13) | 1/0 | 1/0 | 7.0 | Fibromatosis and
multifocal renal cell carcinoma associated with TSC | Sirolimus | 6.0 |
| Lam, 2010 (14) | 3/0 | 2/1 | 9.0–13.0 | Subependymal giant
cell astrocytomas associated with TSC | Sirolimus | 3.0 |
| Hofbauer, 2008
(15) | 1/0 | 0/1 | 15.0 | Facial
angiofibromas associated with TSC | Rapamycin | 9.0 |
| Franz, 2006
(16) | 4/0 | 2/2 | 3.0–15.0 | Subependymal giant
cell astrocytomas or a pilocytic astrocytoma associated with
TSC | Sirolimus | 3.0 |
| Birca, 2010
(17) | 1/0 | 0/1 | 8.0 | Subependymal giant
cell astrocytomas associated with TSC | Rapamycin | 3.0 |
| Staehler, 2012
(18) | 1/0 | 0/1 | 12.0 | Renal
angiomyolipoma associated with TSC | Sirolimus | 6.0 |
| Wataya-Kaneda, 2011
(27) | 5/0 | 2/3 | 9.0–17.0 | Facial
angiofibromas associated with TSC | Rapamycin | 3.0 |
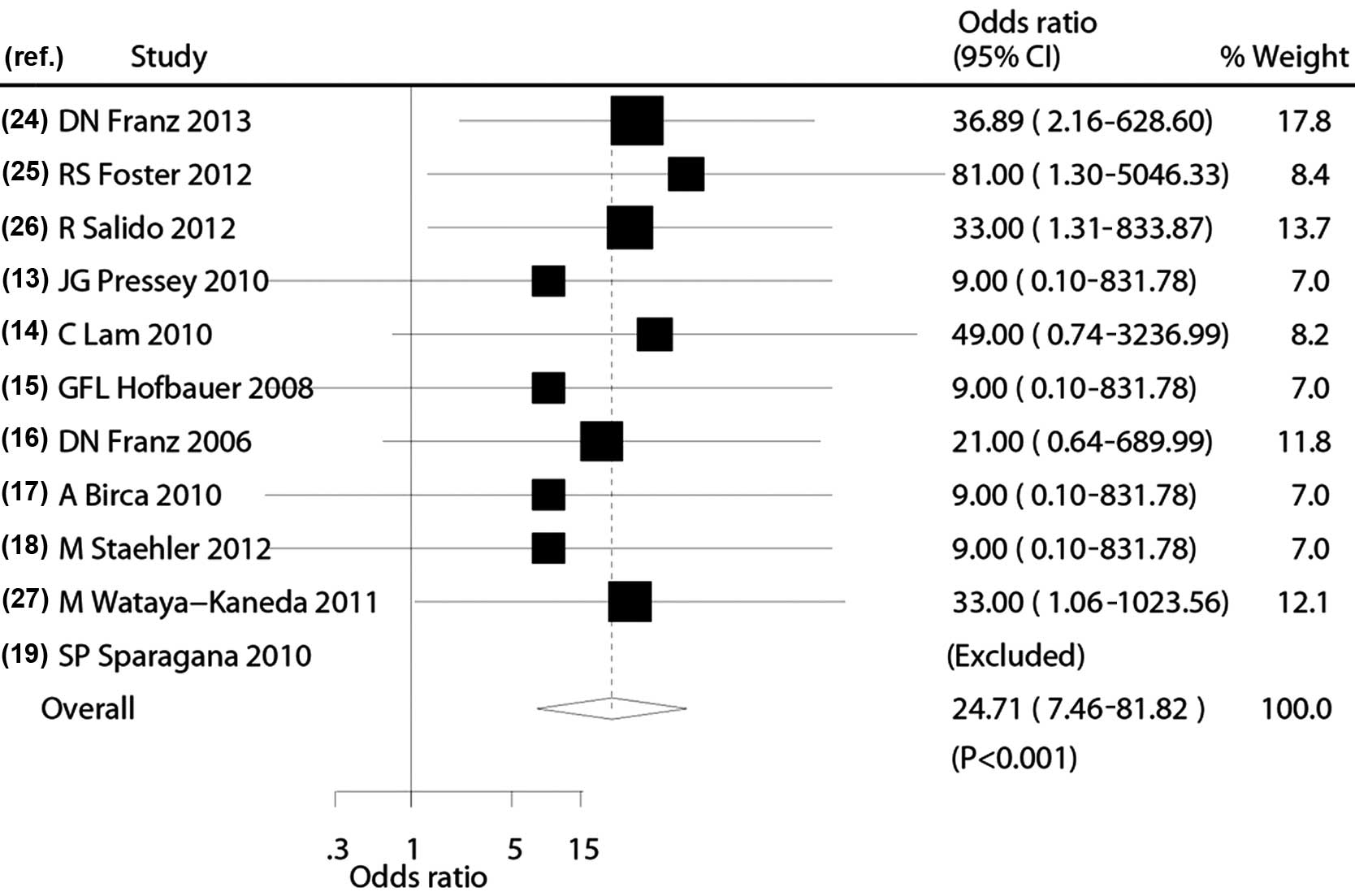
Efficacy of the mTOR inhibitor
Data reporting clinical response rates subsequent to
mTOR inhibitor therapy in pediatric patients with TSC were
available from 11 studies (n=129) (13–19,25–28).
The meta-analysis demonstrated a significantly increased response
rate in pediatric patients with TSC treated with mTOR inhibitor
therapy compared with those treated with non-mTOR inhibitor therapy
(odds ratio, 24.71; 95% CI, 7.46–81.72; P<0.001; Fig. 2). There was no evidence of
significant heterogeneity between trials (P=0.13,
I2=32%). Sensitivity analysis showed that the results
were not affected by the exclusion of any individual study.
Incidence of adverse events
Data reporting adverse effects associated with mTOR
inhibitor therapy and non-mTOR inhibitor therapy for the treatment
of pediatric patients with TSC were published in 11 studies (n=129)
(13–19,25–28).
Pediatric patients that received mTOR inhibitor therapy were more
likely to experience mouth ulceration, stomatitis, convulsion,
acneiform rash, arthralgias, diarrhea, thrombocytopenia,
hyperlipidemia and lipoproteinemia than those treated with non-mTOR
inhibitor therapy. The majority of the adverse events were grade 1
or 2 and self-limiting, but some required dose reduction or
temporary cessation. The grade 3 adverse events that occurred most
frequently were stomatitis, pyrexia and convulsion; grade 4 events
were rare (25–28). Non-specific adverse reactions were
reported in the treatment group in one study (25). Statistical analysis of the adverse
event data was not performed, as the majority of the studies
reported few adverse effects.
Discussion
TSC is a genetic disease affecting multiple systems
that causes non-malignant tumors in a number of vital organs, such
as the brain, kidneys, heart, eyes, lungs and skin. Numerous
symptoms are associated with the condition, including seizures,
developmental delay, behavioral problems, skin abnormalities and
lung and kidney disease (3). In
healthy individuals, TSC1 and TSC2 encode hamartin
and tuberin, and form the hamartin-tuberin tumor suppressor
complex. This inhibits the activation of the mTOR complex 1
(mTORC1), a kinase that modulates protein synthesis and cell growth
and proliferation (29,30). In most patients with TSC, a
mutation in either TSC1 or TSC2 results in an
aberrant activation of mTORC1, causing benign tumor growth
(31).
The benefit of mTOR inhibitor therapy for pediatric
patients with TSC has long been known. Previous studies have shown
that rapamycin plays a beneficial role in the treatment of TSC in a
mouse model (32,33). A case series demonstrated that
rapamycin therapy induced regression of TSC-related astrocytomas
and offered an alternative to surgical therapy for these lesions
(16). However, one case report
(19) indicated that a TSC-related
optic nerve tumor was not responsive to rapamycin.
Although nearly all studies conclude that mTOR
inhibitor therapy is an effective treatment for TSC, most
documented literature is in the form of case studies without any
statistical analysis. To summarize the literature and provide
preliminary evidence-based treatment guidelines for pediatricians
and neurologists, we performed a comprehensive literature search
and examined the efficacy of mTOR inhibitor therapy and the
possible adverse effects in 129 pediatric patients with TSC. The
results of the study suggest that mTOR inhibitor therapy can
increase clinical response rates compared with non-mTOR inhibitor
therapy. This is the first systematic review investigating the
efficacy and safety of mTOR therapy for the treatment of pediatric
patients with TSC. Our findings are in agreement with a recently
published RCT (25).
Several mechanisms for the antitumor effects of mTOR
inhibitors have been proposed. Firstly, mTOR inhibitors have been
suggested to inhibit mTOR-regulated processes by reducing the
phosphorylation of downstream mTOR effectors, including the
translational repressor eukaryotic elongation factor 4E binding
protein 1 and the S6 ribosomal protein kinase 1. This rehabilitates
the translation of pivotal proteins involved in cell cycle
regulation, glycolytic activity, angiogenesis, cell size control
and cellular growth (34,35). Secondly, mTOR inhibitors reduce the
expression of angiogenic factors, such as vascular endothelial
growth factor (VEGF). VEGF can promote neovascularization, which
plays a significant role in the development of solid tumors
(36,37).
The most common adverse events in pediatric patients
with TSC treated with mTOR inhibitor therapy were mouth ulceration,
stomatitis, convulsion and pyrexia (25). The majority of the adverse events
were grade 1 or 2 and self-limiting, but some required dose
reduction or temporary interruption of treatment. The most common
grade 3 adverse events were stomatitis, pyrexia and convulsion
(25–27). Infection in the upper respiratory
tract was also reported. It is noteworthy that a 17-year-old girl
experienced secondary amenorrhea, which may have been a consequence
of mTOR inhibitor therapy as previous data suggest that mTOR can
suppress puberty onset (38).
There were several limitations to this study.
Firstly, in accordance with the inherent assumptions made when
performing any meta-analysis, this study was based on pooled data,
which may not provide a detailed relevant analysis. Secondly,
different TSC disease status could have influenced our conclusions
about the response rates subsequent to mTOR inhibitor therapy.
Thirdly, data on any specific adverse event were unavailable in
these studies; therefore, the association between any specific type
of adverse event and mTOR inhibitor therapy was not identified. The
long-term assessment of the potential adverse effects of mTOR
inhibitor therapy on growth, development and sexual maturation in
the pediatric population remains to be resolved.
Future studies should focus on the efficacy and
safety of mTOR inhibitor therapy in combination with other drugs to
provide an optimal treatment strategy, as well as the efficacy and
safety of mTOR inhibitor therapy for the treatment of specific TSC
subtypes.
Acknowledgements
This study was supported by grants from the National
Natural Science Foundation of China (nos. 30770747, 30801249,
81071036 and 81211140048), the Beijing Municipal Natural Science
Foundation (nos. 7142150, 7081002 and 7042024) and the Capital
Characteristic Clinical Application Research Foundation (no.
Z121107001012056).
References
|
1
|
Borkowska J, Schwartz RA, Kotulska K and
Jozwiak S: Tuberous sclerosis complex: tumors and tumorigenesis.
Int J Dermatol. 50:13–20. 2011. View Article : Google Scholar
|
|
2
|
Osborne JP, Fryer A and Webb D:
Epidemiology of tuberous sclerosis. Ann NY Acad Sci. 615:125–127.
1991. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Crino PB, Nathanson KL and Henske EP: The
tuberous sclerosis complex. N Engl J Med. 355:1345–1356. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Benyounes N, Fohlen M, Devys JM, et al:
Cardiac rhabdomyomas in tuberous sclerosis patients: a case report
and review of the literature. Arch Cardiovasc Dis. 105:442–445.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hunter AG, Nezarati MM and Velsher L:
Absence of signs of systemic involvement in four patients with
bilateral multiple facial angiofibromas. Am J Med Genet A.
152A:657–664. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Sterman H, Furlan AB, Matushita H and
Teixeira MJ: Subependymal giant cell astrocytoma associated with
tuberous sclerosis presenting with intratumoral bleeding. Case
report and review of literature. Childs Nerv Syst. 29:335–339.
2013. View Article : Google Scholar
|
|
7
|
Meraj R, Wikenheiser-Brokamp KA, Young LR
and McCormack FX: Lymphangioleiomyomatosis: new concepts in
pathogenesis, diagnosis, and treatment. Semin Respir Crit Care Med.
33:486–497. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Crino PB: Evolving neurobiology of
tuberous sclerosis complex. Acta Neuropathol. 125:317–332. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Franz DN and Weiss BD: Molecular therapies
for tuberous sclerosis and neurofibromatosis. Curr Neurol Neurosci
Rep. 12:294–301. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Davies DM, Johnson SR, Tattersfield AE, et
al: Sirolimus therapy in tuberous sclerosis or sporadic
lymphangioleiomyomatosis. N Engl J Med. 358:200–203. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Curatolo P and Moavero R: mTOR inhibitors
in tuberous sclerosis complex. Curr Neuropharmacol. 10:404–415.
2012. View Article : Google Scholar :
|
|
12
|
Franz DN: Everolimus in the treatment of
subependymal giant cell astrocytomas, angiomyolipomas, and
pulmonary and skin lesions associated with tuberous sclerosis
complex. Biologics. 7:211–221. 2013.PubMed/NCBI
|
|
13
|
Pressey JG, Wright JM, Geller JI, et al:
Sirolimus therapy for fibromatosis and multifocal renal cell
carcinoma in a child with tuberous sclerosis complex. Pediatr Blood
Cancer. 54:1035–1037. 2010.PubMed/NCBI
|
|
14
|
Lam C, Bouffet E, Tabori U, et al:
Rapamycin (sirolimus) in tuberous sclerosis associated pediatric
central nervous system tumors. Pediatr Blood Cancer. 54:476–479.
2010. View Article : Google Scholar
|
|
15
|
Hofbauer GF, Marcollo-Pini A, Corsenca A,
et al: The mTOR inhibitor rapamycin significantly improves facial
angiofibroma lesions in a patient with tuberous sclerosis. Br J
Dermatol. 159:473–475. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Franz DN, Leonard J, Tudor C, et al:
Rapamycin causes regression of astrocytomas in tuberous sclerosis
complex. Ann Neurol. 59:490–498. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Birca A, Mercier C and Major P: Rapamycin
as an alternative to surgical treatment of subependymal giant cell
astrocytomas in a patient with tuberous sclerosis complex. J
Neurosurg Pediatr. 6:381–384. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Staehler M, Sauter M, Helck A, et al:
Nephron-sparing resection of angiomyolipoma after sirolimus
pretreatment in patients with tuberous sclerosis. Int Urol Nephrol.
44:1657–1661. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Sparagana SP, Wilkes DC, Thompson CE and
Bowers DC: Optic nerve tumor in tuberous sclerosis complex is not
responsive to sirolimus. Pediatr Neurol. 42:443–446. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Moher D, Liberati A, Tetzlaff J and Altman
DG; PRISMA Group. Preferred reporting items for systematic reviews
and meta-analyses: the PRISMA statement. PLoS Med. 6:e10000972009.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Higgins JP, Thompson SG, Deeks JJ and
Altman DG: Measuring inconsistency in meta-analyses. BMJ.
327:557–560. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Higgins JPT and Green S: Cochrane Handbook
for Systematic Reviews of Interventions Version 5.10. The Cochrane
Collaboration; Oxford: 2011
|
|
23
|
DerSimonian R and Laird N: Meta-analysis
in clinical trials. Control Clin Trials. 7:177–188. 1986.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ades AE, Lu G and Higgins JP: The
interpretation of random-effects meta-analysis in decision models.
Med Decis Making. 25:646–654. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Franz DN, Belousova E, Sparagana S, et al:
Efficacy and safety of everolimus for subependymal giant cell
astrocytomas associated with tuberous sclerosis complex (EXIST-1):
a multicentre, randomised, placebo-controlled phase 3 trial.
Lancet. 381:125–132. 2013. View Article : Google Scholar
|
|
26
|
Foster RS, Bint LJ and Halbert AR: Topical
0.1% rapamycin for angiofibromas in paediatric patients with
tuberous sclerosis: a pilot study of four patients. Australas J
Dermatol. 53:52–56. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Salido R, Garnacho-Saucedo G,
Cuevas-Asencio I, et al: Sustained clinical effectiveness and
favorable safety profile of topical sirolimus for tuberous
sclerosis - associated facial angiofibroma. J Eur Acad Dermatol
Venereol. 26:1315–1318. 2012. View Article : Google Scholar
|
|
28
|
Wataya-Kaneda M, Tanaka M, Nakamura A,
Matsumoto S and Katayama I: A topical combination of rapamycin and
tacrolimus for the treatment of angiofibroma due to tuberous
sclerosis complex (TSC): a pilot study of nine Japanese patients
with TSC of different disease severity. Br J Dermatol. 165:912–916.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Ehninger D: From genes to cognition in
tuberous sclerosis: implications for mTOR inhibitor-based treatment
approaches. Neuropharmacology. 68:97–105. 2013. View Article : Google Scholar
|
|
30
|
Han JM and Sahin M: TSC1/TSC2 signaling in
the CNS. FEBS Lett. 585:973–980. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Yang H, Wang X, Zhang Y, et al: Modulation
of TSC-mTOR signaling on immune cells in immunity and autoimmunity.
J Cell Physiol. 229:17–26. 2014.
|
|
32
|
Guo Y and Kwiatkowski DJ: Equivalent
benefit of rapamycin and a potent mTOR ATP-competitive inhibitor,
MLN0128 (INK128), in a mouse model of tuberous sclerosis. Mol
Cancer Res. 11:467–473. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Cambiaghi M, Cursi M, Magri L, et al:
Behavioural and EEG effects of chronic rapamycin treatment in a
mouse model of tuberous sclerosis complex. Neuropharmacology.
67:1–7. 2013. View Article : Google Scholar
|
|
34
|
Zhang Y and Zheng XF: mTOR-independent
4E-BP1 phosphorylation is associated with cancer resistance to mTOR
kinase inhibitors. Cell Cycle. 11:594–603. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Pópulo H, Lopes JM and Soares P: The mTOR
signalling pathway in human cancer. Int J Mol Sci. 13:1886–1918.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Guba M, Yezhelyev M, Eichhorn ME, et al:
Rapamycin induces tumor-specific thrombosis via tissue factor in
the presence of VEGF. Blood. 105:4463–4469. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Frost P, Berlanger E, Mysore V, et al:
Mammalian target of rapamycin inhibitors induce tumor cell
apoptosis in vivo primarily by inhibiting VEGF expression and
angiogenesis. J Oncol. 2013:8970252013. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Roa J, Garcia-Galiano D, Castellano JM, et
al: Metabolic control of puberty onset: new players, new
mechanisms. Mol Cell Endocrinol. 324:87–94. 2010. View Article : Google Scholar
|