Introduction
Laser in situ keratomileusis (LASIK) is
currently the most common refractive surgical procedure used for
patients with myopia, astigmatism and hyperopia (1,2). In
the LASIK procedure, a microkeratome or femtosecond laser is used
to create a flap in the corneal epithelium to access the corneal
stroma, and the flap is raised to gain access to the underlying
stromal tissue. The curvature of the corneal stroma is reshaped by
subsequent excimer laser ablation of targeted stromal tissue and
the flap is repositioned (3–5).
These surgical procedures of LASIK result in faster visual
recovery, lower rates of regression and infection, less
postoperative pain and better refractive predictability compared
with photorefractive keratectomy with complete removal of the
central corneal epithelium (6–8).
Despite the advantages of LASIK and incremental
advances in the technique, LASIK has certain limitations with
regard to risk and visual outcomes, such as anatomic and refractive
complications (9). One of the most
common complications of LASIK is postoperative striae associated
with the creation of the corneal flap, which have a variety of
appearances (10). Flap striae are
classified into two types, namely macrostriae and microstriae
(11). Macrostriae appear as
parallel straight lines on retroillumination and are responsible
for the reduction of vision (12,13).
Visual acuity is usually reduced by two or three lines of
microstriae; however, this may be partially improved by a contact
lens or artificial tears (14,15).
Donnenfeld et al investigated the effects of hyperthermia
for the treatment of long-standing corneal flap striae following
LASIK and found that hyperthermic treatment is a safe, effective
treatment option for corneal striae after LASIK (16). Solomon et al found that
stretching the flap with a cotton-tip applicator is a simple, safe
and effective technique for reducing visually significant flap
striae (17). However, the
formation of striae can lead to a significant loss of corrected
visual acuity if the central pupil zone is affected and any later
intervention will decrease the probability of successful
elimination and visual outcomes (18). Therefore, the sooner that
symptomatic deep striae are diagnosed the more promptly effective
management procedures can be carried out.
Although there are many viewpoints concerning the
causes and pathogenesis of flap striae, such as misalignment or
displacement of the corneal flap following flap replacement,
movement of the corneal flap and a slippage effect of the corneal
flap over the ablated stromal bed following LASIK, the causes and
pathogenesis of flap striae have not been definitively confirmed
(19–21). In order to study the underlying
pathogenesis of flap striae, the present study investigated the
histopathological changes in adult New Zealand white rabbit corneas
following LASIK with the complication of flap macrostriae by
hematoxylin and eosin (H&E), periodic acid-Schiff (PAS) and
Masson’s trichrome staining on days 1, 3, 7 and 14, and at 1, 3 and
6 months postoperatively.
Materials and methods
Animals
Animal care and use was in accordance with the
guidelines established by the Animal Ethics Committee of Chongqing
Medical University (Chongqing, China). Fourteen healthy adult New
Zealand white rabbits weighing >2 kg were provided by the
Experimental Animal Center of Gulou Hospital Affiliated to Nanjing
University (Nanjing, China). Animals were housed singly and fed a
standard diet ad libitum. The right eyes of rabbits were
selected to receive conventional LASIK, followed by the creation of
flap striae (the macrostriae group) and the left eyes were
subjected to conventional LASIK only (the control group).
Preoperative preparation
During three preoperative days, conventional
antibiotic eye drops were applied to the eyes of the rabbits. Each
rabbit was generally anesthetized with an intramuscular injection
of droperidol (1 mg/kg) and ketamine hydrochloride (50 mg/kg), 15
min preoperatively. Then, 4% oxybuprocaine hydrochloride eye drops
were instilled into both eyes of each rabbit for surface
anesthesia.
Surgery
The two eyes of each rabbit were gently proptosed
and a hinged corneal flap was cut using a microkeratome (M2; Moria
SA, Antony, France), and a spherical ablation of −3.00 diopters (D)
was performed on the exposed stromal bed using an excimer laser
system (EC-5000 XII; Nidek, Gamagori, Japan) with an energy density
of 160–180 mJ/cm2 and a 40-Hz pulse rate. Following
careful repositioning of the flap, flap striae were generated in
the corneal flap in the right eye of each rabbit under a microscope
and the direction of the flap was perpendicular to the pedicle.
During the surgery, a bandage soft contact lens (radius of
curvature, 8.30 mm; diameter, 14 mm) was inserted to prevent flap
dislocation.
Postoperative treatment
During the first week after surgery, the animals
received an antibiotic ophthalmic solution for prophylaxis three
times daily to mitigate ocular inflammation. The flap margin and
adjacent regions were examined under a slit lamp and recorded
daily. In this study, the corneal flaps of two eyes in the
macrostriae group respectively fell off on the first and third
postoperative days. Therefore, these two cases were excluded from
the experiments and supplementary animal models were
established.
Histopathological examination
Two rabbits were randomly sacrificed with an
intravenous injection of an air overdose into the ear margin on 1,
3, 7 and 14 days and at 1, 3 and 6 months after the LASIK
procedure. Then, the eyeballs were removed immediately. The excised
corneal tissues were fixed in 10% formaldehyde and embedded in
paraffin wax. Serial 3-μm sections were cut and stained with
H&E, PAS, or Masson’s trichrome by standard procedures.
Results
Clinical observation
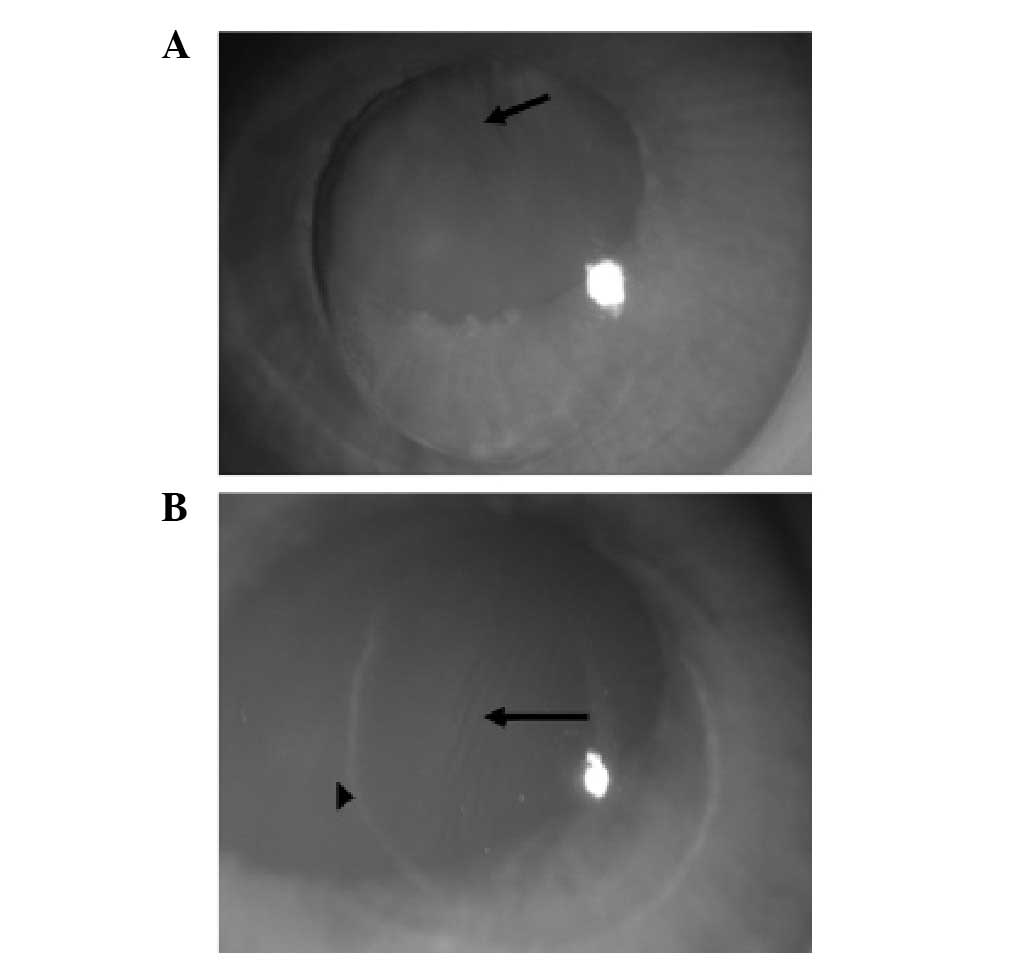
Eyes of the macrostriae group
On the first postoperative day, edema of the corneal
flap was evident and multiple striae were observed. In addition,
the corneal stromal bed at the margin of the flap was exposed
(Fig. 1A). One week
postoperatively, the flap margin was covered by epithelium;
multiple striae were present on the flap and a partial ring of
opacity was observed around the flap (Fig. 1B). One month after the surgery, the
striae on the flap were scarcely visible while the circinate
opacity was still present. The striae had largely disappeared three
months after surgery and the circinate opacity had almost
disappeared six months after the surgery.
Eyes of the control group
On the first postoperative day, a transparent
corneal flap, evident edema at the flap margin and marginal
furrowing of the flap were observed; the epithelium at the margin
had not completely grown into the edge of the incision. One week
postoperatively, the circinate opacity had recombined with the
incision and the corneal epithelium was completely healed with good
positioning of the corneal flap and slight edema. One month after
the surgery, the edema had completely disappeared and the surface
of the flap was smooth; the circinate opacity was fading gradually.
The cornea was fully healed and the circinate opacity had
disappeared entirely three months subsequent to the surgery. The
appearance of the cornea in the control group was similar to that
of the normal cornea.
Histopathological examination
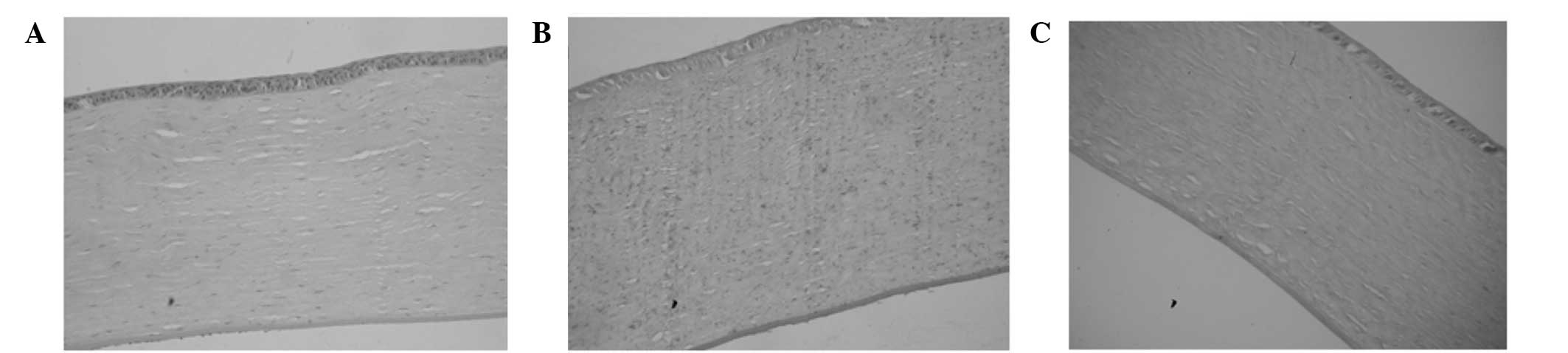
Normal corneas
A normal cornea stained with H&E is shown in
Fig. 2A. The corneal epithelium
was flat with uniform thickness. The morphologies of the flat and
columnar cells (~4–5 layers) could be observed clearly. The
epithelial basement membrane was continuous and flat. The
arrangement of stromal collagen fibers was regular and the nuclei
of corneal stroma cells exhibited a fusiform shape. In Fig. 2B, a section of normal cornea
stained with PAS is shown. Each layer of cells was stained evenly,
with the exception of the posterior elastic layer and the
endothelium of the cornea, which were stained deeply. A section of
normal cornea stained with Masson’s trichrome stain is shown in
Fig. 2C. The endothelium, nuclei
of corneal stromal cells and endothelial cells were stained red
while the remaining tissues were stained blue.
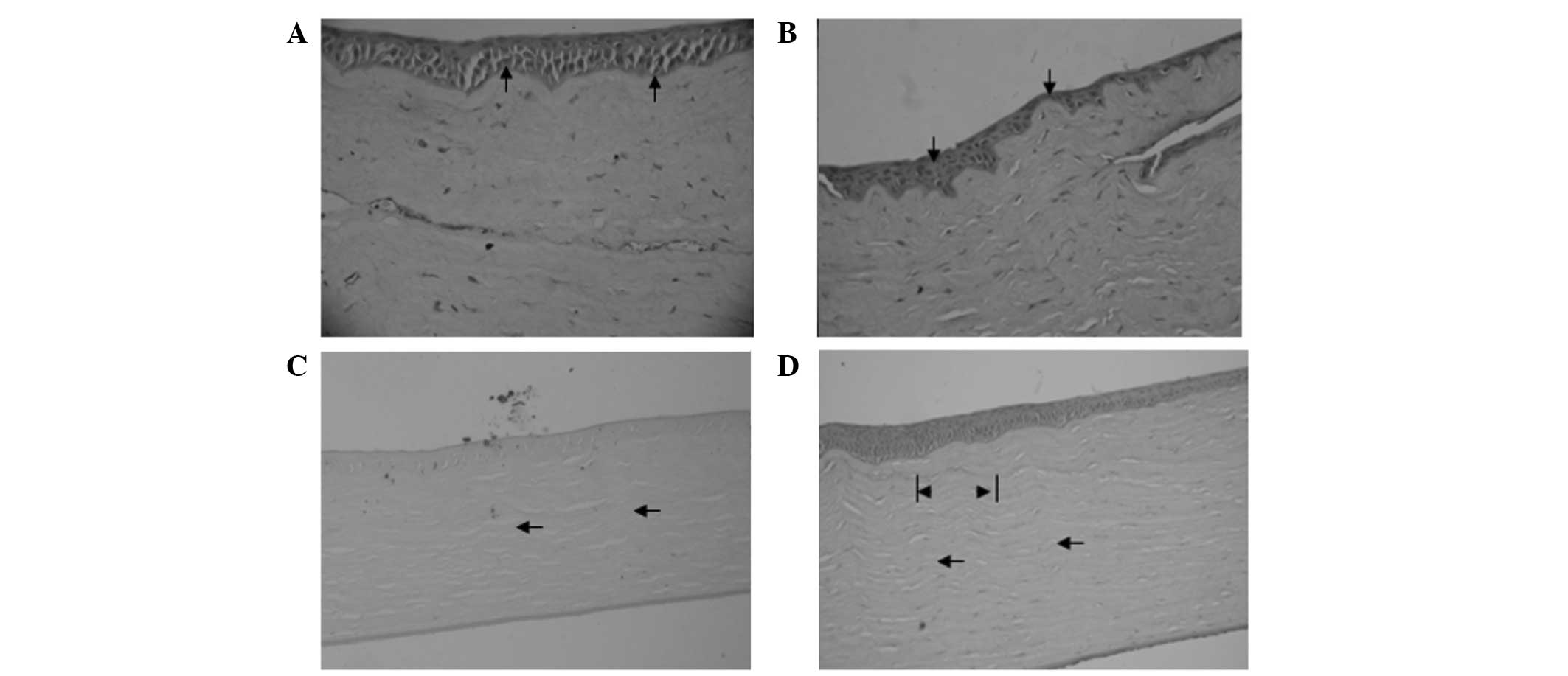
Corneas in the macrostriae group
Epithelial hyperplasia and ingrowth between the
corneal flap and stromal bed were observed on the first
postoperative day. The epithelial basement membrane and stromal
collagen fibers exhibited an irregularly undulating shape.
Infiltration of polymorphonuclear cells around the incision was
visible on the first postoperative day (Fig. 3A). On the third postoperative day,
the morphological characteristics of the corneas were almost the
same as those on the first postoperative day.
One week after surgery, a small number of
polymorphonuclear cells had infiltrated around the incision and an
epithelial plug was generated at the edge of the corneal flap. Two
weeks after surgery, the epithelium was thin (~2–3 layers) in the
strial troughs and thick (~7–10 layers) in the strial ridges
(Fig. 3B).
One month after surgery, there was no clear
difference in the number of epithelial layers between the strial
ridge and trough. The corneal stromal collagen fibers and striae
presented an irregularly undulating shape, in addition to
full-thickness striae of the flap, which affected two-thirds of the
entire level of the cornea (Fig.
3C). Three months after surgery, a regular undulating
arrangement of the stromal collagen fibers with a width of 60–80 μm
was observed (Fig. 3D). In the
sixth postoperative month, the morphological characteristics of the
corneas were comparable with those in the third postoperative
month.
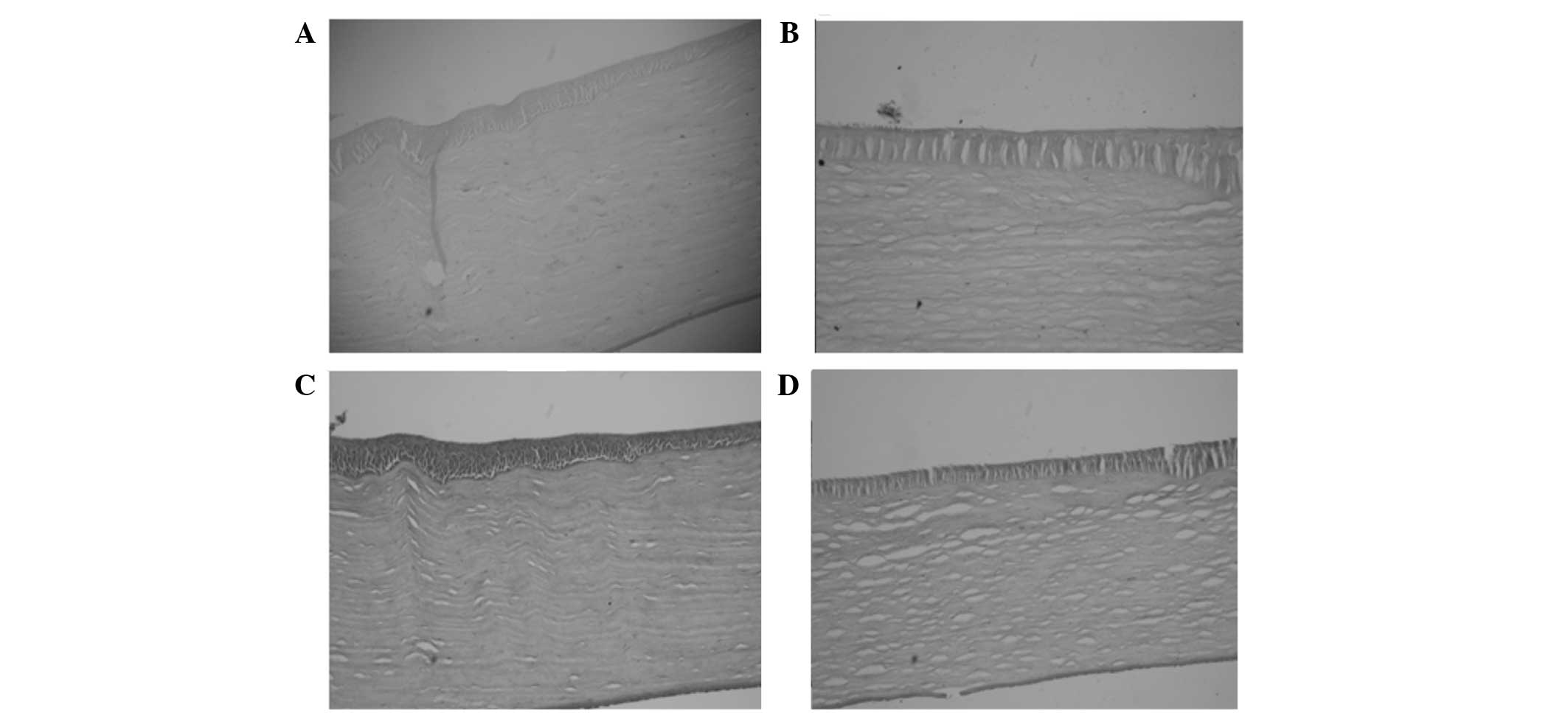
Corneas in the control group
The epithelium of the corneal flap was smooth and
the epithelial basement membrane showed microstriae of width 20–40
μm on the first postoperative day (Fig. 4A). There was no clear difference in
the morphological characteristics of the corneas between the third
and first postoperative days.
One week after surgery, the microstriae of the
epithelial basement membrane became less distinct (Fig. 4B). Two weeks after surgery, the
epithelium in the middle of the corneal flap became thinner and the
striae on the flap disappeared (Fig.
4C). One month after surgery, there was no evident change in
the morphological characteristics of the corneas. Three months
after surgery, the epithelium and stroma appeared normal (Fig. 4D).
PAS and Masson staining of corneas in the
control and macrostriae groups
There were no significant differences in the PAS and
Masson staining of corneas between the macrostriae and control
groups three months after the surgery. The flap margin and the
interlayer between the corneal flap and stromal bed were PAS
stained (Fig. 5A and B). PAS
staining is a staining method used to detect glycogen, which
indicates that glycogen was generated in the wound healing process
of the two groups. Masson staining is used to judge the degree of
the lesions and the repair condition of tissues in pathological
morphology. The Masson staining procedure stains collagen-rich
fibrotic regions blue and muscle red (22). The sections of the cornea were
noticeably stained (Fig. 5C and
D), which indicates that collagen fibers and muscle fibers were
generated in the wound healing process of the cornea.
Discussion
Although LASIK has become a popular technique for
refractive surgery, there are a number of complications that can
arise following such procedures, such as interface haze, flap edge
scarring, epithelial ingrowth and flap striae or folds (23). Since LASIK surgery and the
application of prevention methods for other kinds of complications
have become universal, the issues caused by flap striae have drawn
an increasing amount of attention from clinicians (18,24).
In the present study, the wound healing process and
histopathological changes were investigated in adult New Zealand
white rabbit corneas following LASIK surgery with the complication
of flap macrostriae. It was found that infiltration of
polymorphonuclear cells occurred around the incision in the cornea
in the macrostriae group on the first postoperative day. Parolini
et al examined four cases of corneal interface complications
that occurred following LASIK and found that severe central
inflammation following LASIK could be an extreme manifestation of
diffuse lamellar keratitis (25).
If foreign bodies are suspected to be the cause of inflammation,
early flap lifting with irrigation is imperative for successful
treatment (26). The inflammatory
reactions of corneas in the macrostriae group were more serious
than those in the control group and are likely to influence the
clinical outcome of the surgery.
In the control group, the epithelium of the corneal
flap was smooth and the epithelial basement membrane showed
microstriae 20–40 μm in width on the first postoperative day. Two
weeks after surgery, the epithelium in the middle of the corneal
flap became thinner and the striae on the flap disappeared.
However, in the macrostriae group, the corneal stromal collagen
fibers and striae exhibited an irregularly undulating appearance in
addition to full-thickness striae of flap, which affected
two-thirds of the entire level of the cornea one month
postoperatively. Early recognition of the serious postoperative
complications of LASIK in order for prompt surgical management to
be undertaken is crucial for achieving a successful surgical and
visual outcome (27). It has been
reported that striae are challenging to eliminate as time goes by
since the corneal flap gradually develops fibrosis and lose its
original elasticity, which leads to increased resistance to
flattening (17,28). Therefore, it is recommended that
striae are treated early since delay is likely to cause
considerable difficulty (29).
Furthermore, the altered arrangement of the corneal stromal
collagen fibers and striae in the macrostriae group is likely to
increase the adverse effects on visual acuity. Six months after
surgery, a regular undulating arrangement of stromal collagen
fibers with a width of 60–80 μm remained visible. That is, the
clinical impact of the flap macrostriae was prolonged. However, the
present study only investigated the time points of 1, 3, 7 and 14
days, and 1, 3 and 6 months postoperatively.
In conclusion, the present study identified that the
inflammatory reactions and clinical impact of LASIK were more
serious than those in the control group when flap macrostriae were
present. The flap microstriae in the control group disappeared two
weeks postoperatively. However, macrostriae with a width of 80–120
μm affecting two-thirds of the entire cornea remained present six
months postoperatively. Therefore, in order to reduce and prevent
the occurrence of flap striae, longer-term studies are required to
further elucidate the causes and pathogenesis of flap striae.
Acknowledgements
The authors wish to express warm thanks to Fenghe
(Shanghai) Information Technology Co., Ltd., whose ideas and help
gave a valuable added dimension to the present study.
References
|
1
|
Aslanides IM and Mukherjee AN: Adjuvant
corneal crosslinking to prevent hyperopic LASIK regression. Clin
Ophthalmol. 7:637–641. 2013.PubMed/NCBI
|
|
2
|
Duffey RJ and Leaming D: US trends in
refractive surgery: 2004 ISRS/AAO Survey. J Refract Surg.
21:742–748. 2005.PubMed/NCBI
|
|
3
|
Shortt AJ and Allan BD: Photorefractive
keratectomy (PRK) versus laser-assisted in-situ keratomileusis
(LASIK) for myopia. Cochrane Database Syst Rev.
CD0051352006.PubMed/NCBI
|
|
4
|
Settas G, Settas C, Minos E and Yeung IY:
Photorefractive keratectomy (PRK) versus laser assisted in situ
keratomileusis (LASIK) for hyperopia correction. Cochrane Database
Syst Rev. 6:CD0071122012.PubMed/NCBI
|
|
5
|
Shortt AJ, Bunce C and Allan BD: Evidence
for superior efficacy and safety of LASIK over photorefractive
keratectomy for correction of myopia. Ophthalmology. 113:1897–1908.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Sutton GL and Kim P: Laser in situ
keratomileusis in 2010 - a review. Clin Experiment Ophthalmol.
38:192–210. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ambrosio R Jr and Wilson S: LASIK vs LASEK
vs PRK: advantages and indications. Semin Ophthalmol. 18:2–10.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Moisseiev E, Sela T, Minkev L and Varssano
D: Increased preference of surface ablation over laser in situ
keratomileusis between 2008–2011 is correlated to risk of ectasia.
Clin Ophthalmol. 7:93–98. 2013. View Article : Google Scholar
|
|
9
|
Melki SA and Azar DT: LASIK complications:
etiology, management, and prevention. Surv Ophthalmol. 46:95–116.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Solomon KD, Holzer MP, Sandoval HP, et al:
Refractive Surgery Survey 2001. J Cataract Refract Surg.
28:346–355. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Pannu JS: Incidence and treatment of
wrinkled corneal flap following LASIK. J Cataract Refract Surg.
23:695–696. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Gimbel HV, Penno EE, van Westenbrugge JA,
Ferensowicz M and Furlong MT: Incidence and management of
intraoperative and early postoperative complications in 1000
consecutive laser in situ keratomileusis cases. Ophthalmology.
105:1839–1848. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Tham VM and Maloney RK: Microkeratome
complications of laser in situ keratomileusis. Ophthalmology.
107:920–924. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
von Kulajta P, Stark WJ and O’Brien TP:
Management of flap striae. Int Ophthalmol Clin. 40:87–92. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Gimbel HV, Basti S, Kaye GB and
Ferensowicz M: Experience during the learning curve of laser in
situ keratomileusis. J Cataract Refract Surg. 22:542–550. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Donnenfeld ED, Perry HD, Doshi SJ, Biser
SA and Solomon R: Hyperthermic treatment of post-LASIK corneal
striae. J Cataract Refract Surg. 30:620–625. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Solomon R, Donnenfeld ED, Perry HD, Doshi
S and Biser S: Slitlamp stretching of the corneal flap after laser
in situ keratomileusis to reduce corneal striae. J Cataract Refract
Surg. 29:1292–1296. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Tehrani M and Dick HB: Striae in the flap
after laser in situ keratomileusis. Etiology, diagnosis and
treatment. Ophthalmologe. 99:645–650. 2002.(In German). View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Probst LE and Machat J: Removal of flap
striae following laser in situ keratomileusis. J Cataract Refract
Surg. 24:153–155. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Muñoz G, Alió JL, Pérez-Santonja JJ and
Attia WH: Successful treatment of severe wrinkled corneal flap
after laser in situ keratomileusis with deionized water. Am J
Ophthalmol. 129:91–92. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Charman WN: Mismatch between flap and
stromal areas after laser in situ keratomileusis as source of flap
striae. J Cataract Refract Surg. 28:2146–2152. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Dobrin PB, Baker WH and Gley WC:
Elastolytic and collagenolytic studies of arteries. Implications
for the mechanical properties of aneurysms. Arch Surg. 119:405–409.
1984. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Naripthaphan P and Vongthongsri A:
Evaluation of the reliability of the Nidek MK-2000 microkeratome
for laser in situ keratomileusis. J Refract Surg. 17(2 Suppl):
S255–S258. 2001.PubMed/NCBI
|
|
24
|
Touboul D, Salin F, Mortemousque B, et al:
Advantages and disadvantages of the femtosecond laser
microkeratome. J Fr Ophtalmol. 28:535–546. 2005.(In French).
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Parolini B, Marcon G and Panozzo GA:
Central necrotic lamellar inflammation after laser in situ
keratomileusis. J Refract Surg. 17:110–112. 2001.PubMed/NCBI
|
|
26
|
Choi JA and Kim MS: LASIK
interface-captured foreign bodies after mild traumatic corneal
scratch without flap displacement. Korean J Ophthalmol. 26:222–225.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Lam DS, Leung AT, Wu JT, et al: Management
of severe flap wrinkling or dislodgment after laser in situ
keratomileusis. J Cataract Refract Surg. 25:1441–1447. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Rabinowitz YS and Rasheed K: Fluorescein
test for the detection of striae in the corneal flap after laser in
situ keratomileusis. Am J Ophthalmol. 127:717–718. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Sridhar MS, Rao SK, Vajpayee RB, et al:
Complications of laser-in-situ-keratomileusis. Indian J Ophthalmol.
50:265–282. 2002.
|