Introduction
Ovarian teratoma-associated encephalitis was first
reported in 1997 (1,2). In 2007, an association was identified
between this type of encephalitis and N-methyl-D-aspartate receptor
(NMDAR) antibodies (3). NMDAR is a
ligand-gated cation channel, comprising NR1 and NR2 subunits, that
serves crucial functions in synaptic transmission and plasticity
(4). Overactivation of NMDAR may
result in excitotoxicity, which contributes to the development of
epilepsy, dementia and stroke. Conversely, low NMDAR activity
results in symptoms that resemble schizophrenia (5). The autoantibodies produced in patients
with concurrent anti-NMDAR encephalitis and teratoma exhibit
cross-reactivity with the NMDAR in the teratoma, binding to the NR
subunits of NMDAR following entry into the cerebrospinal fluid.
Anti-NMDAR encephalitis is a severe condition that
is treatment-responsive. The disorder was initially identified in
young females with an ovarian teratoma. These patients developed
mood, behavior and personality abnormalities that resembled acute
psychosis. The symptoms of anti-NMDAR encephalitis include
neuropsychiatric symptoms, hyperkinesia, autonomic dysfunction,
hypoventilation and epilepsy. Anti-NMDAR encephalitis is generally
considered to be a paraneoplastic disease due to the rapid clinical
improvement typically observed in patients following an
ovariectomy. However, in certain patients, no teratoma or other
tumor types are detected; thus, the exact prevalence and incidence
of this disease remain unknown (2).
The present study reports a rare case involving a
patient with anti-NMDAR encephalitis and severe neurological
symptoms. Following a laparoscopic salpingo-oophorectomy, the
patient exhibited a rapid recovery.
Case report
Written informed consent was obtained from the
patient's family. A 39-year-old woman with no significant medical
history was admitted to the the Department of Obstetrics and
Gynecology, Osaka City University Graduate School of Medicine
(Osaka, Japan) with a 5-day history of fever and stomach ache. The
patients symptoms initially resembled those of the common cold.
However, one week later, the patient experienced hallucinations and
emotional lability. Blood testing and brain computed tomography
(CT) scans indicated no abnormalities. However, the condition
progressed, and the patient exhibited deteriorated emotional
lability, increased disorientation and progressive dyskinesia,
which was characterized by chorea of the body and limbs. An
examination of the cerebrospinal fluid detected a cell count of
77-mm3, with a high number of monocytes. However, the
head CT examination performed upon arrival revealed no notable
abnormalities. Initially, limbic-herpes encephalitis was considered
as a diagnosis; thus, the patient was administered acyclovir
(1,5000 mg-day, 7 days) and received steroid pulse therapy
(solu-medrol 1,000 mg-day, 3 days, 3 courses). However, the patient
subsequently developed apnea. Therefore, a tracheal intubation,
mechanical ventilation and plasmapheresis were performed. A lumbar
puncture, serum viral analysis, head CT and magnetic resonance
imaging (MRI) examinations were unable to clarify the etiology of
the patients symptoms. Therefore, anti-NMDAR encephalitis was
considered as a potential diagnosis, and mediastinal and pelvic CT
examinations were conducted to detect the presence of a teratoma.
An abdominal CT scan revealed a 24×24-mm cystic lesion in the
pelvis, which appeared to be an ovarian teratoma. Furthermore,
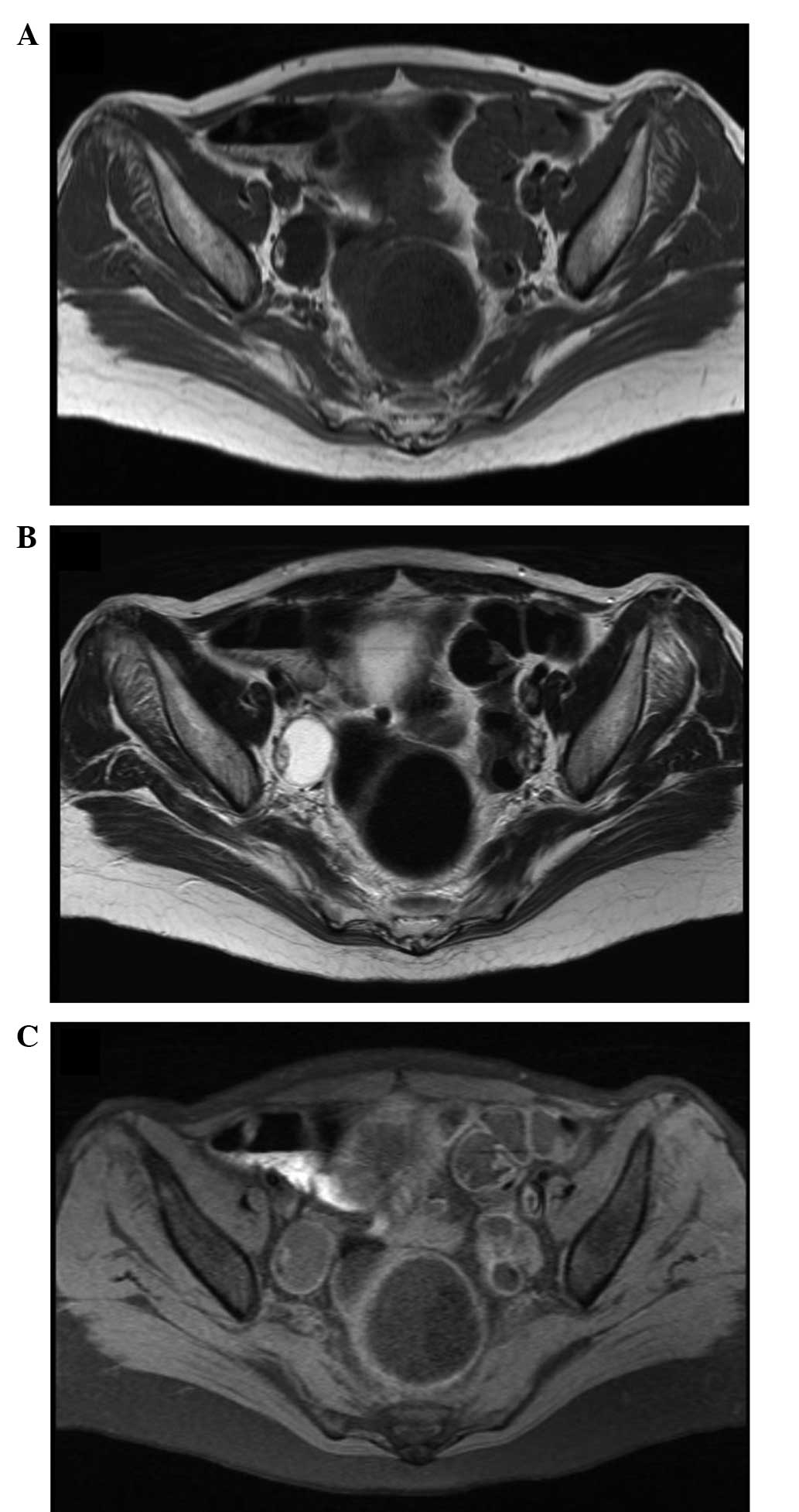
pelvic MRI revealed a right ovarian teratoma (Fig. 1). In addition, serum and
cerebrospinal fluid samples were collected, and were determined to
be positive for anti-NMDAR antibodies. A laparoscopic right
salpingo-oophorectomy was subsequently performed. Intraoperatively,
the right ovary was observed to be enlarged to 30 mm, while the
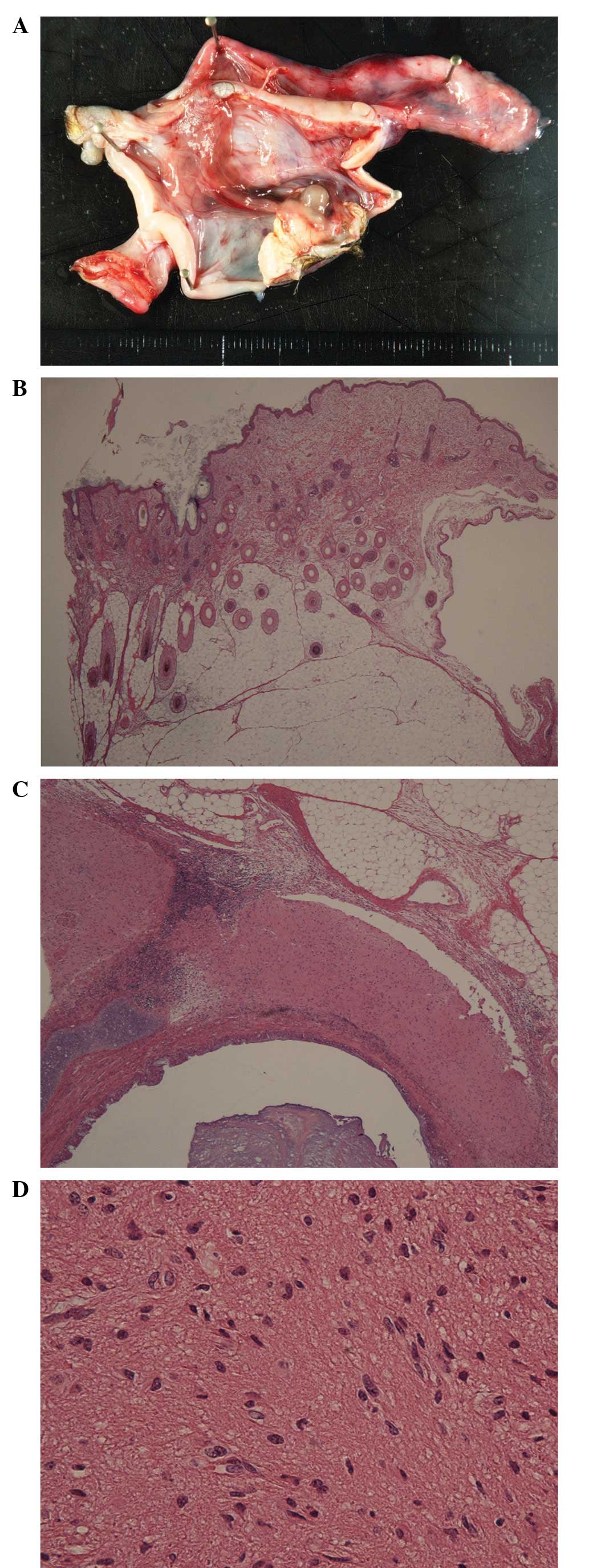
left ovary remained at a normal size (Fig. 2). Pathological examination confirmed
the diagnosis of a mature right ovarian cystic teratoma, containing
neural tissue (Fig. 3).
The patient underwent postoperative steroid therapy
(prednisolone 20 mg-day) until discharge, and the condition was
observed to improve gradually. Mechanical respiratory support was
no longer required by postoperative day 15, and the patient opened
her eyes and began speaking on postoperative day 20, until which
the patient had been comatose. Furthermore, the patients mental
symptoms exhibited notable improvement, and the patient achieved
complete recovery by postoperative day 53.
Discussion
Anti-NMDAR encephalitis is an autoimmune
antibody-mediated form of limbic encephalitis, that was initially
reported by Dalmau et al in 2007 (3). Anti-NMDAR encephalitis frequently
occurs in young women, at a median age of 23 years (5). Commonly observed symptoms include
psychiatric symptoms, involuntary movement of the face and limbs,
consciousness disturbances and central hypoventilation. The
clinical progression of anti-NMDAR encephalitis typically begins
with symptoms that resemble the common cold, which subsequently
progress to a period of psychiatric symptoms, followed by an
immobile period and a hyperactive period (6). This clinical course was observed in the
present case. A definitive diagnosis can be achieved following the
detection of anti-NMDAR antibodies in the cerebrospinal fluid and
serum.
A previous study reported that 40% of patients with
anti-NMDAR encephalitis are aged <18 years (median age, 14
years), while older female patients develop ovarian teratomas more
frequently compared with younger patients. Statistically, 31% of
female patients aged <18 years and 56% of female patients aged
>18 years exhibited teratomas (7). However, the incidence of paraneoplastic
anti-NMDAR encephalitis remains unknown.
A tumorectomy is an effective treatment method when
cases of teratoma are detected at an early stage (5). In addition, steroid pulse therapy,
gamma globulin therapy, plasmapheresis and immunosuppressant
therapy are effective treatment methods (8,9).
Although 75% of patients recover completely, severe and prolonged
disease is possible, and the mortality rate of anti-NMDAR
encephalitis is 7% (5).
The present study described a rare case involving a
patient with anti-NMDAR encephalitis who rapidly recovered from
severe neurological symptoms following a laparoscopic
salpingo-oophorectomy. The patient exhibited neuropsychiatric
symptoms, hyperkinesia, autonomic dysfunction, hypoventilation and
epilepsy; however, no signs of meningitis were observed. The
etiology of the patients symptoms was unable to be clarified by a
lumbar puncture, serum viral analysis, head CT or MRI examination.
Therefore, anti-NMDAR encephalitis was considered as a potential
diagnosis. Abdominal CT examination revealed a teratoma in the
patients right ovary. Furthermore, anti-NMDAR antibodies were
detected in the cerebrospinal fluid and serum of the patient. Thus,
the diagnosis of anti-NMDAR encephalitis was confirmed.
In conclusion, gynecologists should be aware that
small ovarian teratomas may induce anti-NMDAR encephalitis. Removal
of the NMDAR-expressing tumor reduces the serum and cerebrospinal
fluid levels of the pathological autoantibody (10). The present case report demonstrates
that complete recovery from the severe neurological symptoms of
anti-NMDAR encephalitis is possible following surgical
resection.
References
|
1
|
Nokura K, Yamamoto H, Okawara Y, Koga H,
Osawa H and Sakai K: Reversible limbic encephalitis caused by
ovarian teratoma. Acta Neurol Scand. 95:367–373. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Okamura H, Oomori N and Uchitomi Y: An
acutely confused 15-year-old girl. Lancet. 350:4881997. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Dalmau J, Tüzün E, Wu HY, Masjuan J, Rossi
JE, Voloschin A, Baehring JM, Shimazaki H, Koide R, King D, et al:
Paraneoplastic anti-N-methyl-d-aspartate receptor encephalitis
associated with ovarian teratoma. Ann Neurol. 61:25–36. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Lynch DR, Anegawa NJ, Verdoorn T and
Pritchett DB: N-methyl-D-aspartate receptors: different subunit
requirements for binding of glutamate antagonists, glycine
antagonists and channel-blocking agents. Mol Pharmacol. 45:540–545.
1994.PubMed/NCBI
|
|
5
|
Dalmau J, Gleichman AJ, Hughes EG, Rossi
JE, Peng X, Lai M, Dessain SK, Rosenfeld MR, Balice-Gordon R and
Lynch DR: Anti-NMDA-receptor encephalitis: Cases series and
analysis of the effect of antibodies. Lancet Neurol. 7:1091–1098.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Iizuka T, Sakai F, Ide T, Monzen T, Yoshii
S, Iigaya M, Suzuki K, Lynch DR, Suzuki N, Hata T and Dalmau J:
Anti-NMDA receptor encephalitis in Japan: Long-term outcome without
tumor removal. Neurology. 70:504–511. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Florance NR, Davis RL, Lam C, Szperka C,
Zhou L, Ahmad S, Campen CJ, Moss H, Peter N, Gleichman AJ, et al:
Anti-N-methyl-D-aspartate receptor (NMDAR) encephalitis in children
and adolescents. Ann Neurol. 66:11–18. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ishiura H, Matsuda S, Higashihara M,
Hasegawa M, Hida A, Hanajima R, Yamamoto T, Shimizu J, Dalmau J and
Tsuji S: Response of anti-NMDA receptor encephalitis without tumor
to immunotherapy including rituximab. Neurology. 71:1921–1923.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Sansing LH, Tüzün E, Ko MW, Baccon J,
Lynch DR and Dalmau J: A patient with encephalitis associated with
NMDA receptor antibodies. Nat Clin Pract Neurol. 3:291–296. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Seki M, Suzuki S, Iizuka T, Shimizu T,
Nihei Y, Suzuki N and Dalmau J: Neurological response to early
removal of ovarian teratoma in anti-NMDAR encephalitis. J Neurol
Neurosurg Psychiatry. 79:324–326. 2008. View Article : Google Scholar : PubMed/NCBI
|