Introduction
Acute mesenteric ischemia is a life-threatening
condition with a mortality rate of 40% (1). The condition is commonly caused by
acute thrombosis of a partially occluded atherosclerotic lesion.
The perioperative mortality rate of thrombosis in the superior
mesenteric artery (SMA) is relatively high due to the difficulty of
diagnosis, the extent of bowel ischemia infarction and the
complexity of surgical revascularization (2). Treatments for superior mesenteric
artery thrombosis include non-surgical treatment (anticoagulant
medicines) and surgical treatment, including endarterectomy, artery
bypass, artery segmental resection and anastomosis, and
intraarterial catheter-directed thrombolysis. During surgery,
bowels with necrosis require resection and follow-up surgery is
necessary to protect the remaining ischemic bowel tissues (3). Hybrid surgical techniques, a type of
surgical treatment combining the advantages of open surgical and
endovascular approaches, are widely used and include retrograde
open mesenteric stenting (ROMS), which is effective in treating
thrombosis in SMA (4). The present
study investigated a hybrid approach for treating patients
suffering from acute SMA thrombosis, which employed
fluoroscopically-assisted embolectomy and balloon angioplasty,
combined with catheter-directed thrombolysis during the laparotomy
(5).
Materials and methods
Patients
The hybrid technique was conducted on six patients
with acute SMA thrombosis, of which five were male and one was
female. Comorbid medical conditions, radiological findings,
perioperative data and follow-up information were obtained for all
patients (Table I). Three patients
presented with sudden and severe abdominal pain, out of proportion
with the physical findings, while the other three patients
exhibited diffuse, severe and constant pain, with signs of
peritoneal irritation. Atherosclerotic lesions were detected using
abdominal computed tomography (CT) scans, through which other
differential disease diagnoses were able to be excluded. Written
informed consent was obtained from the patients. The study was
approved by the ethics committee of Tianjin medical university
(Tianjin, China).
 | Table I.Medical data of six patients
undergoing the hybrid surgery. |
Table I.
Medical data of six patients
undergoing the hybrid surgery.
| Medical data | Pt 1 | Pt 2 | Pt 3 | Pt 4 | Pt 5 | Pt 6 |
|---|
| Gender | M | M | M | F | M | M |
| Age (years) | 59 | 70 | 73 | 72 | 73 | 69 |
| Time to surgery
(h) | 15 | 24 | 48 | 24 | 16 | 8 |
| Pain with signs of
peritoneal irritation | No | Yes | Yes | Yes | No | No |
| Pre-existing SMA
stenosis | Yes | Yes | Yes | Yes | Yes | Yes |
| Atrial
tachyarrhythmias | No | No | No | No | No | No |
| Coronary heart
disease | No | Yes | Yes | Yes | Yes | No |
| Cerebrovascular
disease | No | No | Yes | No | No | No |
| Hypertension | Yes | Yes | Yes | Yes | Yes | Yes |
| Chronic obstructive
pulmonary disease | No | No | Yes | Yes | Yes | No |
Surgical procedure
The right common femoral artery was entered
percutaneously using the Seldinger technique, and an introducer
sheath was inserted (6F; Cordis Corporation, Miami Lakes, FL, USA).
A pigtail catheter (5F; Cordis Corporation) was inserted into the
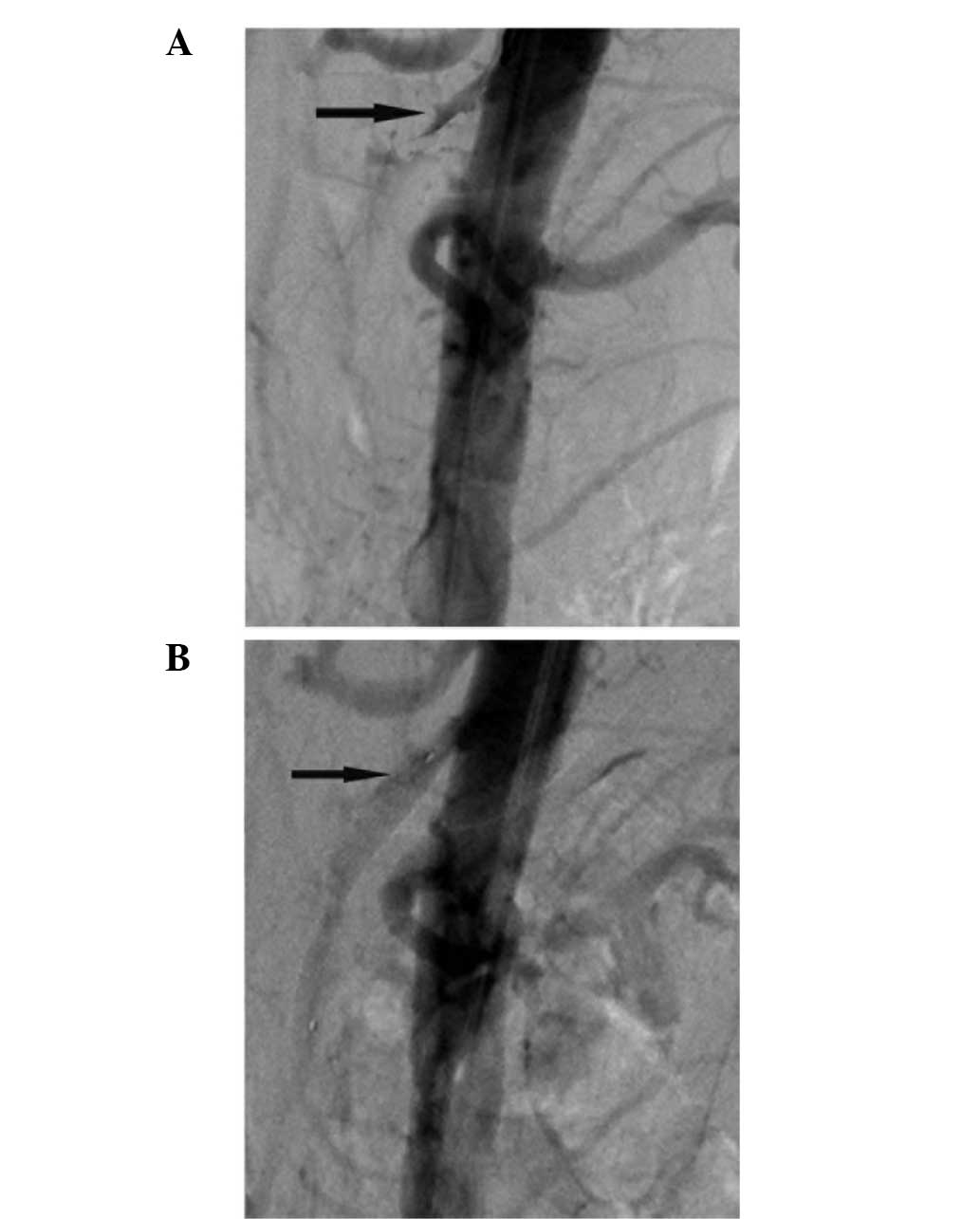
suprarenal abdominal aorta. An abdominal aorta angiography or
selective angiography was conducted for confirmation of thrombosis
in the occluded lesion of the SMA (Figs.
1A,1B and 2A). Subsequently, a midline laparotomy was
performed for assessment of the entire intestinal tract. Any
clearly necrotic bowel tissue was resected, while ischemic but
potentially recoverable tissue was left as much as possible. The
SMA was exposed at the root of the mesentery. A puncture (Merit
Medical Systems, Inc., South Jordan, UT, USA) was made in the SMA
at ∼6 cm distal to the origin, and a 6F sheath was inserted in a
retrograde fashion. A 0.035-in Glidewire (Terumo Corporation,
Tokyo, Japan) and an angled Glidecatheter (4F; Cordis Corporation)
were used to maneuver through the occlusive lesion into the aorta.
A 0.018-in control guide wire (Boston Scientific Corporation,
Natick, MA, USA) was introduced into the aorta to complete the
guide wire exchange. The vessel was clamped distally, a transverse
arteriotomy was made at the site of guide wire access and a
fluoroscopically-assisted embolectomy was performed using a
double-lumen balloon catheter (Edwards Lifesciences Corporation,
Irvine, CA, USA) over the wire. A local endarterectomy was
conducted if required. A retrograde injection reconfirmed the SMA
stenosis. Balloon angioplasty (diameter, 4–5 mm; Medtronic Invatec
S.p.A., Roncadelle, Italy) and/or stenting were completed to treat
the occlusive lesion. The stent measured 6 mm in diameter and 40 mm
in length (ev4; Endovasculat, Inc., Plymouth, MN, USA). Following
completion of the surgery, the SMA was opened to flush out the
emboli, the arteriotomy was closed and an angiogram was performed.
If blood flow was not restored to the ischemic bowels after 15 min,
a catheter (5F RH; Cordis Corporation) was inserted into the SMA
for thrombolysis, with urokinase (4×105 IU; Biochem
Pharmaceutical Corporation, Tianjin, China) administered over 20
min if necessary. Intra-arterial catheter-directed thrombolysis
with urokinase (8×105 IU/24 h) was performed
continuously for 48 h. In addition, doses of low molecular weight
heparin calcium (86 IU/kg, twice a day) were administered to ensure
adequate anticoagulation. The safety of the lytic treatment was
evaluated every 12 h by testing the fibrinogen levels (range,
1.80–4.00 g/l). A second-look laparotomy was performed after 48 h
to assess the health outcomes of the bowels, and anastomosis of the
bowel segments was performed to restore bowel continuity.
Acetylsalicylic acid or warfarin was subsequently administered long
term to stabilize the prothrombin time-international normalized
ratio (PT-INR) between 2–3 and fibrinogen between 2–4 g/L. The
coagulation function of the patients requires monitoring weekly for
at least 1 year and reduced to an appropriate frequency.
Clinical outcomes
Clinical success was defined as the recovery of the
ischemic bowels and the resolution of clinical symptoms within the
30-day perioperative period. Clinical examinations, ultrasonography
and/or CT-angiography of the SMA were performed to confirm the
patency during the follow-up period.
Results
Stenting
As shown in Fig. 2B,
two patients required a single stent, which measured 6 mm in
diameter and 40 mm in length (ev3 Endovascular, Inc.). These
patients experienced a full recovery of the ischemic bowels
following revascularization of the SMA during the laparotomy.
Intra-arterial catheter-directed
thrombolysis
Four patients required intra-arterial
catheter-directed thrombolysis following embolectomy and balloon
angioplasty of the SMA (Fig. 1C and
1D). However, one patient was found to have ∼100 cm ischemic
jejunum tissue following recanalization of the SMA during the first
laparotomy. The other three patients exhibited massive bowel
necrosis and underwent a necrotic bowel resection during the
initial surgery, after which two patients were found to have
necrotic small bowels from 80/70 cm proximal jejunum to 40/80 cm
terminal ileum, respectively. Although the remaining jejunum was
without evident necrosis, the viability of the tissue was poor. The
remaining patient exhibited substantial necrosis of the right colon
and massive small bowels, with only 90 cm ischemic proximal jejunum
tissue. These four patients underwent intra-arterial
catheter-directed thrombolysis for 48 h, and the ischemic bowels
were shown to have recovered by the second-look surgery.
Clinical outcomes
Early clinical success was achieved in all the
procedures. However, two patients developed acute renal failure
postoperatively; one patient recovered after 10 days of dialysis,
while the other individual succumbed to acute renal failure. In
addition, two patients developed a wound infection. The three
patients who underwent massive bowel resection did not develop
short bowel syndrome.
Long-term follow-up outcomes
The patency of the SMA was maintained in the five
surviving patients during the follow-up period. No patients have
experienced recurrence of acute or chronic mesenteric ischemia
since the surgical hybrid procedure (Table II).
 | Table II.Clinical outcomes of the six patients
following hybrid surgery on the SMA. |
Table II.
Clinical outcomes of the six patients
following hybrid surgery on the SMA.
| Patient | Procedure | Restoration of
ischemic bowels | Hospitalization
(days) | Postoperative
complications | Survival | Follow-up
(months) | Symptom
recurrence | Patency of SMA | Secondary
intervention |
|---|
| 1 | FATE+BA+UK | Yes | 12 | No | Yes | 19.5 | No | Yes | No |
| 2 | FATE+BA+UK | Yes | 18 | No | Yes | 12.6 | No | Yes | No |
| 3 | FATE+BA+UK | Yes | 21 | WI | Yes | 13.7 | No | Yes | No |
| 4 | FATE+BA+UK | Yes | 29 | ARF, WI | Yes | 4.6 | No | Yes | No |
| 5 | FATE+BA+stent | Yes | 30 | ARF, MSOF | No | N/A | N/A | N/A | N/A |
| 6 | FATE+BA+stent | Yes | 15 | No | Yes | 7.4 | No | Yes | No |
Discussion
Acute mesenteric ischemia secondary to a
pre-existing SMA atherosclerotic disease is a surgical emergency
associated with a poor prognosis. The condition requires prompt
diagnosis and early revascularization in order to avoid massive
bowel necrosis. Traditional approaches for achieving
revascularization involve an antegrade aortomesenteric bypass or
retrograde iliac artery to mesenteric artery bypass (3). However, the present study assessed the
viability of a combined surgical and endovascular approach, using
intraoperative retrograde balloon angioplasty or stenting during
the laparotomy, followed by intra-arterial catheter-directed
thrombolysis. The application of ROMS enabled the recanalization of
the SMA to be more simple and quick, subsequently improving the
mortality rate in patients with acute SMA thrombosis.
Milner et al (6) were the first to successfully perform
the hybrid ROMS technique on an elderly patient with acute SMA
thrombosis. Wyers et al (7)
reported a 100% technical success rate using ROMS on six patients,
with a mortality rate of 17%. The mortality rate of ROMS-treated
patients was lower when compared with that of conventional surgical
revascularization (80%) and a percutaneous stent (100%) for the
treatment of arterial occlusive mesenteric ischemia in 13 patients.
Stout et al (8)published a
case report that included three patients with acute occlusive
mesenteric ischemia who were treated with ROMS, which had a 100%
technical success rate. In the present study, two patients were
treated successfully with ROMS, with no technique-related
complications or morbidity, although one patient succumbed to acute
renal failure.
Previous studies have demonstrated the use of
thrombolytic therapy in the treatment of acute mesenteric ischemia
(9–11); however, to the best of our knowledge,
no studies have applied intra-arterial catheter-directed
thrombolysis following recanalization of the SMA. During the
laparotomy of the three patients who underwent a massive bowel
resection, only 20–30-cm sections of the proximal jejunums were
observed to be viable, whereas an ischemic change was evident in
the intestinal wall of the remaining proximal jejunum (50–60 cm).
Successful treatment of the 50–60-cm section of the jejunum was
necessary for the patients to survive surgery without developing
short bowel syndrome. Treating these ischemic bowels was a critical
health issue and the only viable treatment strategy was
intra-arterial catheter-directed thrombolysis. Although the main
trunk of the SMA was patent, a section of the distal vessel bed was
occluded with thrombi. Constant intra-arterial catheter-directed
thrombolysis may clear the microthrombus and reopen small branches
of the SMA to improve the perfusion of the ischemic bowels.
Although this thrombolytic therapy presents a risk of hemorrhage
for patients simultaneously undergoing an exploratory laparotomy
and bowel resection, intra-arterial catheter-directed thrombolysis
was an alternative approach for the prevention of necrosis in the
ischemic bowels. In the four patients that underwent this procedure
in the present study, no bleeding was evident at the time of the
thrombolytic therapy. Okamura et al have previously
demonstrated that urokinase has no effect during surgery since the
half-life in blood is only 16 min (11). However, in the present study,
adjusting the dose of urokinase according to the level of
fibrinogen was attempted in order to avoid hemorrhage. Whether
catheter-directed thrombolysis in the SMA hybrid surgery should be
attempted depends mainly on the viability of the bowels once the
SMA has been recanalized.
In conclusion, ROMS was demonstrated to be a viable
alternative procedure for emergent SMA revascularization. In
addition, intra-arterial catheter-directed thrombolysis following
recanalization of the SMA may be an alternative treatment for
preventing necrosis in the ischemic bowels of patients with acute
mesenteric ischemia. In the future, larger clinical trials are
required to investigate the clinical efficacy of the hybrid
techniques in the treatment of arterial occlusive mesenteric
ischemia.
References
|
1
|
Schoots IG, Koffeman GI, Legemate DA, Levi
M and van Gulik TM: Systematic review of survival after acute
mesenteric ischaemia according to disease aetiology. Br J Surg.
91:17–27. 2004. View
Article : Google Scholar : PubMed/NCBI
|
|
2
|
Bayrak S, Bektas H, Duzkoylu Y, Guneyi A
and Cakar E: Acute abdomen resulting from concurrent thrombosis of
celiac trunk and superior mesenteric artery. Case Rep Gastrointest
Med. 2014:1427012014.PubMed/NCBI
|
|
3
|
Matsubara K, Obara H and Kitagawa Y:
Diagnosis and treatment of embolism and thrombosis of abdominal
aorta and superior mesenteric artery. Nihon Rinsho. 72:1289–1293.
2014.PubMed/NCBI
|
|
4
|
Blauw JT, Meerwaldt R, Brusse-Keizer M,
Kolkman JJ, Gerrits D and Geelkerken RH: Retrograde open mesenteric
stenting for acute mesenteric ischemia. J Vasc Surg. 60:726–734.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Nomura Y, Yamaguchi M, Kitagawa A, Okada
T, Okita Y and Sugimoto K: Hybrid management of ruptured isolated
superior mesenteric artery dissecting aneurysm. J Vasc Surg.
54:1808–1811. 2014. View Article : Google Scholar
|
|
6
|
Milner R, Woo EY and Carpenter JP:
Superior mesenteric artery angioplasty and stenting via a
retrograde approach in a patient with bowel ischemia - a case
report. Vasc Endovascular Surg. 38:89–91. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wyers MC, Powell RJ, Nolan BW and
Cronenwett JL: Retrograde mesenteric stenting during laparotomy for
acute occlusive mesenteric ischemia. J Vasc Surg. 45:269–275. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Stout CL, Messerschmidt CA, Leake AE,
Veale WN, Stokes GK and Panneton JM: Retrograde open mesenteric
stenting for acute mesenteric ischemia is a viable alternative for
emergent revascularization. Vasc Endovascular Surg. 44:368–371.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Byun SJ and So BJ: Successful aspiration
and thrombolytic therapy for acute superior mesenteric artery
occlusion. J Korean Surg Soc. 83:115–118. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Malhotra AD, Chander RK and Kim HS:
Catheter-directed thrombolysis for acute superior mesentery artery
occlusion: a case report with long-term clinical follow-up. J Vasc
Interv Radiol. 21:158–160. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Okamura S, Fujiwara H, Sonoyama T, Ochiai
T, Ikoma H, Kubota T, et al: Management of acute superior
mesenteric artery occlusion by thrombolytic therapy. Case Rep
Gastroenterol. 3:300–305. 2009. View Article : Google Scholar : PubMed/NCBI
|