Introduction
A number of studies have clarified that excessive
alcohol consumption is the primary etiological factor in the
induction of chronic pancreatitis (CP) or even pancreatic cancer
(1–3). Both in acute pancreatitis and CP, a
high intake of alcohol is an important causative factor; multiple
research studies have strived to elucidate the molecular mechanisms
responsible for alcohol-induced pancreatic injury (4). In acinar cells, alcohol has been
proven to elevate the activation of transcription factors, such as
nuclear factor-κB (NF-κB) and cytokine expression (5). Furthermore, alcohol exposure can
induce an increase in cytoplasmic calcium ions (Ca2+)
levels, which leads to mitochondrial depolarization and necrosis
(6).
The association between alcoholic pancreatitis and
susceptibility factors, including genetic polymorphisms (7), minor cystic fibrosis mutations
(8) and environmental factors,
such as bacterial endotoxins have been examined (9). Plasma endotoxin levels have been
shown to be higher in drinkers than in non-drinkers and are known
to correlate with the severity of alcoholic liver disease (10). Notably, an increase in gut
permeability may be induced by alcoholic intoxication, which allows
gut bacteria or bacterial products to enter the portal circulation
(11). Notably, a positive
correlation has been demonstrated between higher circulating
lipopolysaccharide (LPS) levels and an increased severity of acute
pancreatitis (12).
Alcohol consumption may lead to the enhanced
production of pro-inflammatory cytokines and chemokines. Alcoholic
hepatitis and pancreatitis, two major clinical complications of
chronic alcohol use, have been shown to be intimately associated
with increasing circulating levels of pro-inflammatory cytokines
that predict poor clinical outcomes (13,14). Previous studies have indicated
that acute alcohol can inhibit pro-inflammatory cell activation,
which is pivotal to innate immune activation (15). By contrast, chronic alcohol
exposure leads to the elevated activation of pro-inflammatory
cytokines in humans (16). Human
monocytes, following treatment with prolonged alcohol in
vitro, have been shown to produce increased levels of tumor
necrosis factor-α (TNF-α) and have shown elevated NF-κB activation
(17). Additionally, chronic
alcohol intake may persistently activate monocytes and macrophages,
resulting in a marked increase in the levels of in pro-inflammatory
cytokines, such as TNF-α, interleukin-1 (IL-1) and interleukin-1
(IL-6) and the chemokine interleukin-8 (IL-8) (18–20).
Chronic inflammation may cause cellular
transdifferentiation which can occur in a number of organs,
including the pancreas (21),
stomach (22), intestine
(23) and esophagus (24). Pancreatic acinar-to-ductal
metaplasia (ADM) has been identified as an initiating event that
can trigger the development of serious lesions, such as pancreatic
intraepithelial neoplasia (PanIN) or pancreatic ductal
adenocarcinoma (PDAC) (21,25). ADM, as a reversible process, can
be induced by activating K-ras mutations, epidermal growth factor
receptors or pancreatic inflammation (26–28). A previous study on patients with
duct-like metaplasia induced by CP demonstrated a 16-fold increase
in the relative risk for PDAC, increasing to 50-fold in patients
with familial CP (29).
In the pancreas, chronic alcohol exposure has been
reported to exacerbate the degree of fibrosis induced by LPS
through an augmented level of tumor growth factor-β (TGF-β)
(30). However, it remains
largely unknown whether the inflammation induced by chronic alcohol
and LPS may contribute to pancreatic ADM. In the present study, we
aimed to evaluate the role of inflammation induced by chronic
alcohol and LPS exposure in the progression of pancreatic ADM, as
well as to elucidaste the possible mechanisms involved. For this
purpose, cultured macrophages were exposed to varying doses of
alcohol for 1 week prior to LPS stimulation. TNF-α regulated upon
activation, normal T cell expression and secreted (RANTES)
expression was upregulated in the intoxicated macrophages with
activated NF-κB. Following treatment with the supernatant of
intoxicated macrophages, ADM of primary acinar cells was induced.
Furthermore, TNF-α and RANTES expression, as well as the
phosphatidylinositol-3-kinase (PI3K)/protein kinase B
(Akt)/inhibitory κB kinase(IKK) signaling pathway, have been shown
to be involved in the ADM of acinar cells. Moreover, Sprague-Dawley
(SD) rats were employed to explore the induction of pancreatic ADM
by chronic alcohol and LPS exposure. Some physiological parameters,
such as body weight, liver weight (LW) and pancreatic weight (PW)
were reduced in the exposed rats. Plasma alcohol concentrations and
oxidative stress levels in the serum along with TNF-α and RANTES
expression levels in monocytes were also induced following chronic
alcohol and LPS exposure. In addition, pancreatic ADM was induced
through the PI3K/Akt/IKK signaling pathway by augmented TNF-α and
RANTES levels in the exposed rats.
Materials and methods
Alcohol exposure and stimulation of
cells
A rat macrophage cell line obtained from ScienCell
Research Laboratories (Carlsbad, CA, USA) was cultured in
macrophage medium (MaM, Cat. no. 1921) according to the
manufacturer’s instructions. The macrophages were stimulated with
varying doses (0, 5, 10, 15, 20 and 25 mM) of alcohol [ethanol
(EtOH)] for 1 week prior to treatment with Escherichia
coli-derived LPS (100 ng/ml). The ethanol concentration was
selected according to a previous study (33). Ethanol (25 mM) in vitro is
approximately equal to a blood alcohol level of 0.1 g/dl, which is
achieved in vivo after a dose of moderate alcohol. Cell
viability was not affected by ethanol or LPS treatment (data not
shown).
Isolation of primary pancreatic acinar
cells
The isolation of primary pancreatic acinar cells was
as previously described (31).
Briefly, the pancreas was removed, washed twice with ice-cold PBS,
minced into 1–5-mm sections and digested with collagenase I (37°C
with a shaker). The collagen digestion was terminated by the
addition of an equal volume of ice-cold PBS. The digested
pancreatic sections were washed twice with PBS containing 5% FBS
and pipetted through a 500-μm mesh and then a 105-μm
mesh. The supernatant of this cell suspension containing acinar
cells was added dropwise to 20 ml PBS containing 30% FBS. The
acinar cells were then pelleted (1,000 rpm for 2 min at 4°C) and
resuspended in 10 ml Waymouth complete medium (1% FBS, 0.1 mg/ml
trypsin inhibitor and 1 μg/ml dexamethasone).
Animals and treatment
A total of 120 8-week old male SD rats were
purchased from Shanghai SLAC Laboratory Animal Co., Ltd. (Shanghai,
China). The animals were housed under standard conditions with a
12/12-h light/dark cycle at room temperature and fed a common diet
with free access to water. To establish chronic alcoholic and
LPS-stimulated rat models, the SD rats were randomly divided into 6
groups and intraperitoneally injected with 0, 5, 10, 15, 20 and 25
mmol/kg/day alcohol [ethanol (EtOH)] for 4 weeks. Following alcohol
exposure, a dose (1 mg/kg) of LPS was administered by intravenous
injection. For TNF-α and RANTES neutralization, the rats were
injected with anti-TNF-α (sc-8301; Santa Cruz Biotechnology, Santa
Cruz, CA, USA) or anti-RANTES (sc-514019; Santa Cruz Biotechnology)
antibodies. The doses of anti-TNF-α or anti-RANTES antibody w as
based on the results of preliminary experiments. To inhibit PI3K or
IKK activity in rats, LY294002 (a PI3K inhibitor; 100 mg/kg, 10 min
before the alcohol injection) was intravenously injected; 25%
dimethyl sulfoxide in PBS was used as the vehicle.
All animal experimental procedures were conducted
under the guidelines of the National Health and Medical Research
Council for the Care and Use of Animals for Experimental Purposes
in China. All efforts were made to minimize the suffering of the
animals.
siRNA transfection
Scrambled siRNA and small-interfering RNA (siRNA)
targeting NF-κB or the IL-1 receptor-associated kinase (IRAK)-M was
purchased from Santa Cruz Biotechnology. The cells were transfected
with scrambled or NF-κB/IRAK-M siRNA according to the
manufacturer’s instructions. Briefly, the NF-κB/IRAK-M and
scrambled siRNA (30 pmol) were diluted in 500 μl DMEM and
mixed with 5 μl Lipofectamine RNAiMAX (Invitrogen, Carlsbad,
CA, USA). Following 15 min of incubation at room temperature, the
complexes were added to the cells to a final volume of 3 ml medium.
The cells were then harvested at the indicated times for further
analysis. The efficiency of the NF-κB/RAK-M siRNA was confirmed by
western blot analysis of Flag expression.
Adenovirus construction
All recombinant adenoviruses were constructed
according to a previous report (32). Briefly, IκB or IRAK-M were
amplified and subcloned into pAdTrack-CMV, an adenoviral shuttle
plasmid, whereas GFP was used as a non-specific control.
Subsequently, the recombinant shuttle plasmids, pAdTrack-CMV and
pAdEasy-1, were homologously recombined in the Escherichia
coli strain BJ5183. The recombinant plasmids obtained were
transfected into HEK293 cells to generate recombinant adenovirus.
The virus was amplified and purified, and titers were determined
using the p24 ELISA kit (Cell Biolabs, Inc., San Diego, CA, USA),
before being stored at −80°C for subsequent use.
Reporter gene assays
The acinar cells were infected with
adenovirus-NF-κB-luciferase adenovirus (at 107 IFU/ml),
and immediately plated on a 24-well plate and cultured with 6
groups of macrophage supernatants. At 24 and 48 h after infection,
the cells were collected and washed with ice-cold PBS, lysed using
250 μl Passive Lysis Buffer (Promega, Madison, WI, USA) and
centrifuged (13,000 rpm for 10 min at 4°C). Assays for luciferase
activity were performed according to the luciferase assay protocol
(Promega) and measured using a luminometer (Veritas; Symantec) and
GloMax software (Promega).
Detection of plasma alcohol,
malondialdehyde (MDA)a nd glutathione peroxidase (GPx) levels, and
superoxide dismutase (SOD) activity
A Biochemical Analysis kit (Nanjing Jiancheng
Bioengineering Institute, Nanjing, China) was used to measure the
plasma alcohol concentration, MDA content, GPx and SOD activity
according to the manufacturer’s instructions. Each experiment was
performed no less than 3 times.
Enzyme-linked immunosorbent assay (ELISA)
for TNF-α and RANTES detection
The levels of TNF-α and RANTES in the serum were
analyzed using a commercially available ELISA kit (Yanjin
Biotechnology Co., Shanghai, China) according to the manufacturer’s
instructions. The absorbance was read at 450 nm using a 680XR
microplate reader (Bio-Rad Laboratories, Hercules, CA, USA). All
the samples were analyzed in duplicate. The standard curve for the
estimation of TNF-α and RANTES expression was created by linear
regression analysis.
RNA extraction and quantitative reverse
transcription-polymerase chain reaction (RT-qPCR)
RNA was extracted from the macrophages or acinar
cells using TRIzol RNA extraction reagent (Gibco, Rockville, MD,
USA) according to the manufacturer’s instructions. Approximately 5
μg total RNA for each sample were reverse transcribed into
first strand cDNA for RT-qPCR analysis. RT-qPCR was performed in a
final volume of 10 μl, which contained 5 μl of
SsoFast™ EvaGreen Supermix (Bio-Rad Laboratories), 1 μl of
cDNA (1:50 dilution) and 2 μl each of the forward and
reverse primers (1 mM). The steps used for RT-qPCR were as follows:
94°C for 2 min for initial denaturation; 94°C for 20 sec, 58°C for
15 sec, and 72°C for 15 sec; 2 sec for plate reading for 40 cycles;
and a melt curve from 65 to 95°C. β-actin was used as a
quantitative and qualitative control to normalize gene expression.
Data were analyzed using the formula: R = 2-(ΔCt sample − ΔCt
control). The sequences of all the primers used in this
experiment are presented in Table
I.
 | Table IList of primers used for RT-qPCR. |
Table I
List of primers used for RT-qPCR.
| Gene | Primer
sequence |
|---|
| TNF-α | F:
5′-ATGAGCACAGAAAGCATGATC-3′
R: 5′-TACAGGCTTGTCACTCGAATT-3′ |
| RANTES | F:
5′-TCCAATCTTGCAGTCGTGTTTG-3′
R: 5′-TCTGGGTTGGCACACACTTG-3′ |
| β-actin | F: 5′-GTG GGG CGC
CCC AGG CACCA-3′
R: 5′-CTC CTT AAT GTC ACG CAC GAT TTC-3′ |
Western blot analysis
The cells were homogenized and lysed with RIPA lysis
buffer (100 mM NaCl, 50 mM Tris-HCl pH 7.5, 1% Triton X-100, 1 mM
EDTA, 10 mM β-glycerophosphate, 2 mM sodium vanadate and protease
inhibitor). Protein concentration was assayed using a Micro BCA
Protein kit (Pierce, Rockford, IL, USA). Forty micrograms of
protein per lane were separated by 12% SDS-PAGE and electroblotted
onto nitrocellulose membranes (Amersham Pharmacia, Munich,
Germany). Subsequently, non-specific binding was blocked by
incubating with 5% non-fat milk in TBST buffer at room temperature
for 1 h. Immunodetection of target proteins [TNF-α, RANTES, IκB,
phosphorylated (p-)Akt, p-p38 mitogen-activated protein kinase
(MAPK), p-c-Jun amino-terminal kinase (JNK), amylase,
cytokeratin-19 (CK-19), total caspase-3, cleavage caspase-3 and
β-actin] was performed using mouse monoclonal antibody (1:1,000;
Santa Cruz Biotechnology) and anti-β-actin antibody (Sigma, St.
Louis, MO, USA), respectively. Goat anti-mouse IgG (1:5,000; Sigma)
followed by enhanced chemiluminescence (ECL, Amersham Pharmacia,
Piscataway, NJ, USA) was used for detection. BandScan 5.0 software
was used for the quantification of all the proteins after western
blot analysis.
Immunohistochemical analysis of amylase
and CK-19
A sequential method for amylase/CK-19 double
staining was used according to the immunohistochemistry enzyme
double staining protocol described in a previous study (34). Briefly, the sections were
incubated with goat polyclonal anti-CK19 antibody (dilution 1:100;
Santa Cruz Biotechnology) as the first primary antibody and
detected using the DAB substrate chromogen system (Sigma). The
sections were then blocked again with normal serum, and incubated
with the second primary antibody, mouse monoclonal anti-amylase
antibody (dilution 1:100; Santa Cruz Biotechnology), after
incubating with the anti-mouse secondary antibody and
avidin-biotin-peroxidase complex; 3-amino-9-ethylcarbazole (AEC)
peroxidase substrate with a characteristic red color was used to
detect positive staining and to distinguish from the brown color of
DAB. The negative control was established by replacement of the
primary antibody with normal serum. Specific antibody-labeled
signals were analyzed under a microscope (Nikon, Tokyo, Japan).
Statistical analysis
Data are expressed as the means ± SD. Statistical
significance was analyzed with the one-way factorial ANOVA or the
Student’s two-tailed t-test. A value of P<0.05 was considered to
indicate a statistically significant difference. All analyses were
conducted using SPSS software (SPSS, Inc., Chicago, IL, USA).
Results
TNF-α and RANTES expression induced by
LPS is enhanced by chronic alcohol exposure
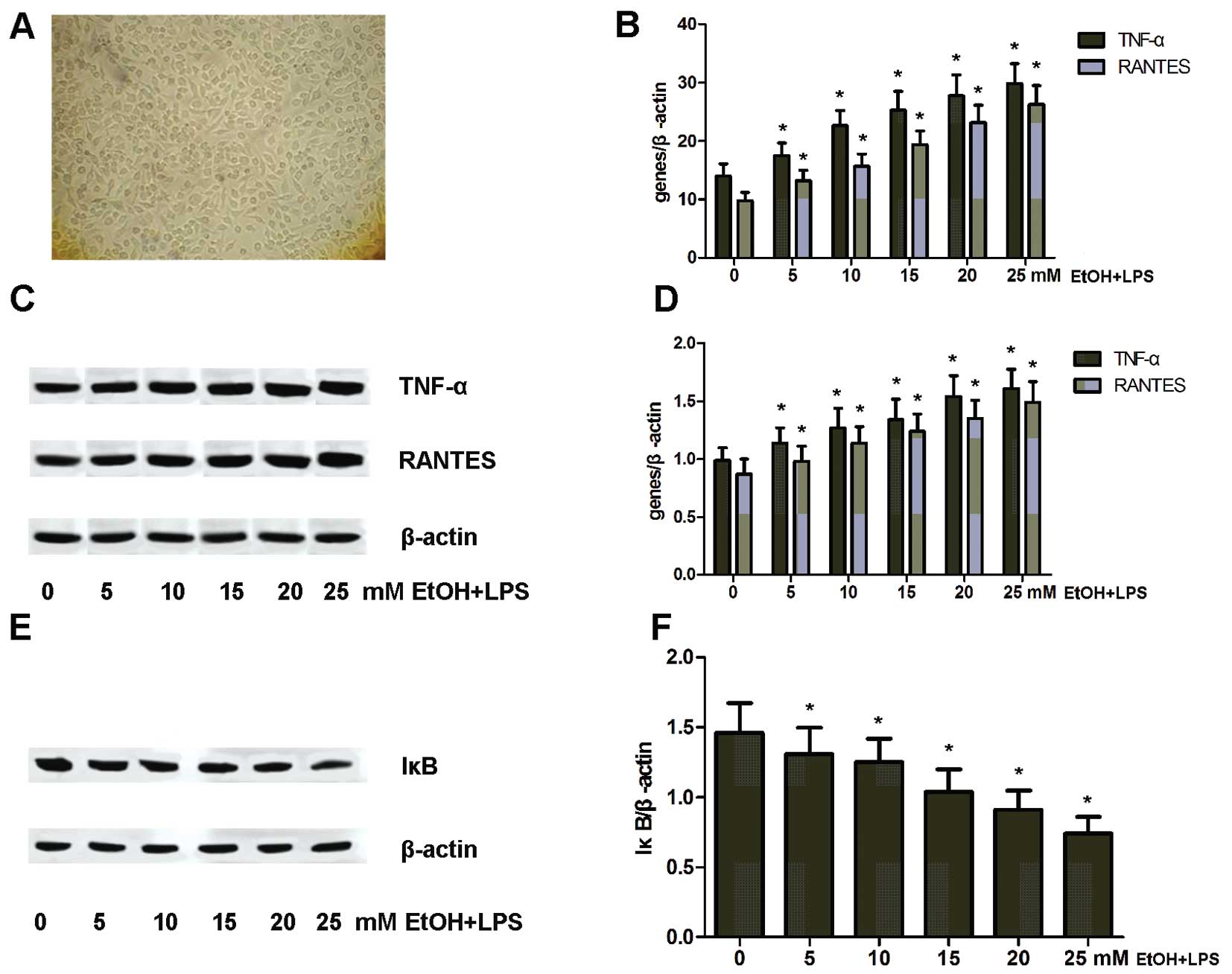
To explore the effects of chronic alcohol on TNF-α
and RANTES expression induced by LPS, we cultured rat macrophages
(Fig. 1A) with varying doses (0,
5, 10, 15, 20 and 25 mM) of alcohol for 1 week and then treated
them with LPS for 1 h. At the end of the treatment, the expression
levels of TNF-α and RANTES in these cells were detected by RT-qPCR.
The results revealed that the expression levels of TNF-α and RANTES
were continuously elevated by alcohol exposure in a dose-dependent
manner (Fig. 1B). This was
further confirmed by western blot analysis. NF-κB activity was
proven to be essential for TNF-α and RANTES expression (Fig. 1C and D). Therein, the expression
of IκB, as an inhibitory protein for NF-κB, was analyzed by western
blot analysis. Compared to the control group (0 mM alcohol),
chronic alcohol exposure clearly reduced the level of IκB
expression, implying NF-κB activation (Fig. 1E and F).
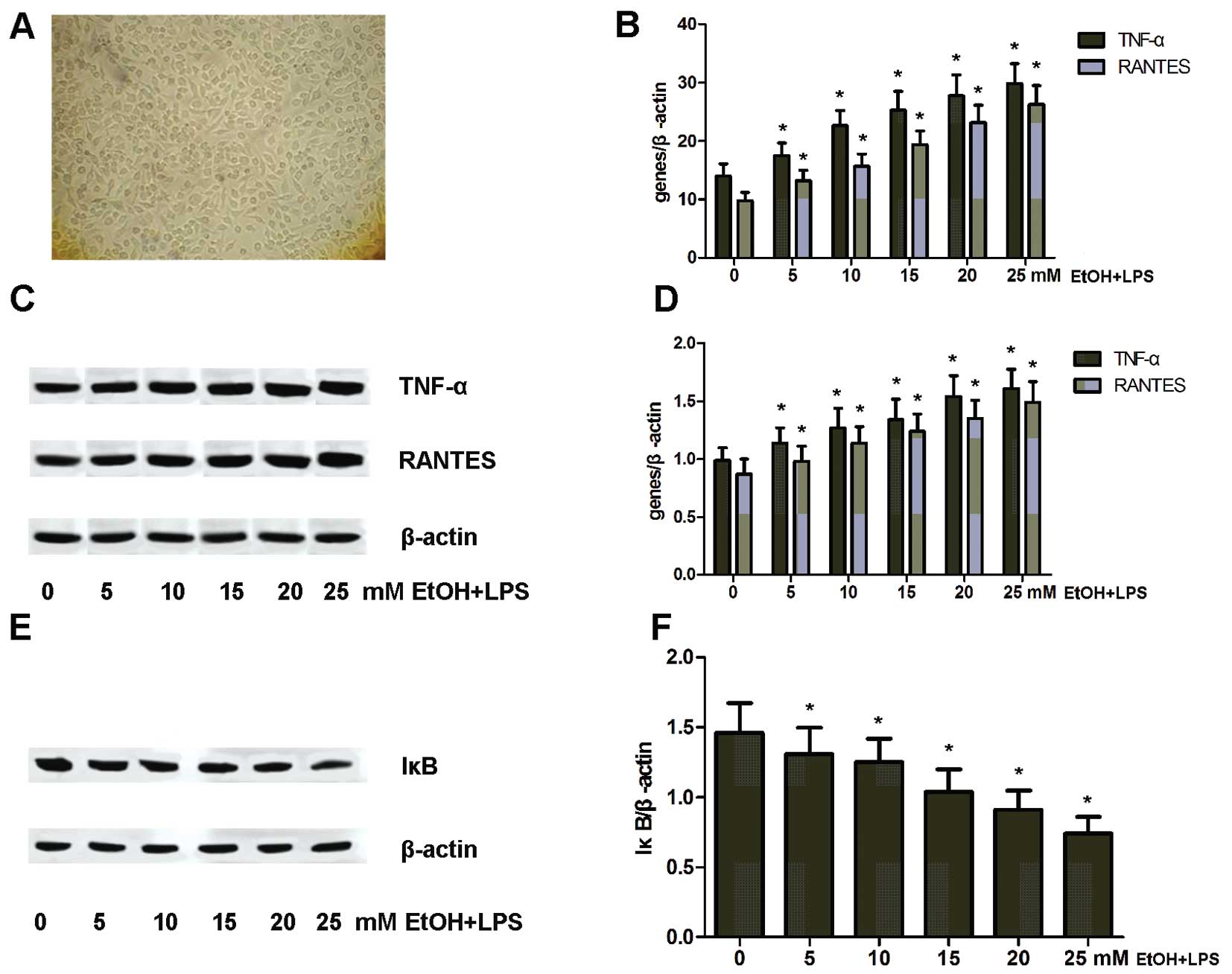 | Figure 1Chronic alcohol exposure upregulates
tumor necrosis factor (TNF)-α and regulated upon activation, normal
T cell expression and secreted (RANTES) expression in rat
macrophages. (A) Cultured rat macrophages (magnification, ×400,
F200). (B) mRNA expression of TNF-α and RANTES in rat macrophages
exposed to varying doses (0, 5, 10, 15, 20 and 25 mM) of alcohol
[ethanol (EtOH)] and lipopolysaccharide (LPS);
*P<0.05 vs. 0 mM EtOH + LPS group. (C) Protein
expression of TNF-α and RANTES in rat macrophages exposed to
varying doses (0, 5, 10, 15, 20 and 25 mM) of alcohol and LPS. (D)
Protein expression was analyzed using BandScan 5.0 software and
normalized to β-actin; *P<0.05 vs. 0 mM EtOH + LPS.
(E) Western blot analysis of IκB expression in rat macrophages
exposed to varying doses (0, 5, 10, 15, 20 and 25 mM) of alcohol
and LPS. (F) Protein expression was analyzed using BandScan 5.0
software and normalized to β-actin; *P<0.05 vs. 0 mM
EtOH + LPS. |
Knockdown of NF-κB/overexpression of IκB
lead to the reduction of TNF-α and RANTES expression induced by LPS
and chronic alcohol exposure
To further confirm the role of NF-κB and IκB in the
regulation of TNF-α and RANTES expression, cultured rat macrophages
were transfected with siRNA targeting NF-κB or adenovirus encoding
IκB. These cells were then exposed to alcohol (0 or 25 mM) and LPS
(100 ng/ml) as depicted above. The expression of TNF-α and RANTES
was analyzed by RT-qPCR. The knockdown of NF-κB or the
overexpression of IκB significantly decreased the expression of
TNF-α and RANTES (Fig. 2).
The IRAK-M/p38 MAPK/JNK signaling pathway
mediates the regulation of TNF-α and RANTES expression
It has been well established that IRAK-M plays a
vital role in activating NF-κB and in the regulation of
inflammation induced by alcohol and LPS (35,36). Rat macrophages were cultured in
the presence of varying doses (0, 5, 10, 15, 20 and 25 mM) of
alcohol for 1 week prior to LPS stimulation. IRAK-M expression was
analyzed in the exposed macrophages by western blot analysis. As
shown in Fig. 3, chronic alcohol
markedly impeded IRAK-M expression (Fig. 3A and B). Moreover, the expression
of p-p38 MAPK and p-JNK was also examined by western blot analysis.
The expression levels of p-p38 MAPK and p-JNK were upregulated by
chronic alcohol and LPS exposure (Fig. 3C and D). Furthermore, to explore
the role of IRAK-M in the regulation of TNF-α and RANTES
expression, we further transfected siRNA targeting IRAK-M into the
rat macrophages. The knockdown of IRAK-M induced an increase in
p-p38 MAPK and p-JNK expression, as well as TNF-α and RANTES
expression in these cells (Fig. 3E
and F).
 | Figure 3Interleukin-1 receptor-associated
kinase (IRAK)-M/p38 mitogen-activated protein kinase (MAPK)/c-Jun
amino-terminal kinase (JNK) plays a vital role in the regulation of
tumor necrosis factor (TNF)-α and regulated upon activation, normal
T cell expression and secreted (RANTES) expression in rat
macrophages. (A) Protein expression of IRAK-M in rat macrophages
exposed to varying doses (0, 5, 10, 15, 20 and 25 mM) of alcohol
[ethanol (EtOH)] and lipopolysaccharide (LPS). (B) Protein
expression was analyzed using BandScan 5.0 software and normalized
to β-actin; *P<0.05 vs. 0 mM EtOH + LPS. (C)
Expression of phosphorylated (p-)p38 MAPK and p-JNK was enhanced in
rat macrophages exposed to varying doses (0, 5, 10, 15, 20 and 25
mM) of alcohol and LPS. (D) Protein expression was analyzed using
BandScan 5.0 software and normalized to β-actin;
*P<0.05 vs. 0 mM EtOH + LPS group. (E) IRAK-M
expression was targeted by specific siRNA in macrophages prior to
exposure to 25 mM alcohol and LPS. Protein expression of p-p38
MAPK, p-JNK, TNF-α and RANTES was analyzed by western blot
analysis. (F) Protein expression was analyzed using BandScan 5.0
software and normalized to β-actin, *P<0.05 vs.
control; **P<0.05 vs. 25 mM EtOH + LPS group. |
ADM is induced by culture supernatants of
rat macrophages
Liou et al (31) proved that macrophages induce ADM
in a co-cultured context. In the present study, we hypothesized
that chronic alcohol promotes the activation of macrophages induced
by LPS and, thus, leads to ADM. To validate this hypothesis, rat
macrophages were cultured in the presence of varying doses (0, 5,
10, 15, 20 and 25 mM) of alcohol. Following culture for 1 week, 6
groups of cells were stimulated with LPS prior to collection of the
supernatant. Primary acinar cells were isolated from 30 rats and
then cultured with macrophage conditioned medium (collected
supernatant). In order to detect ADM, the expression of amylase for
acinar markers and CK-19 for ductal markers was analyzed by western
blot analysis. Compared to the controls (untreated cells), the
conditioned medium derived from alcohol- and LPS-treated
macrophages showed markedly decreased amylase expression and
increased CK-19 expression (Fig. 4A
and B).
The progression of ADM has been shown to be
implicated in a process of transdifferentiation and the induction
of anti-apoptosis (21,37). In the present study, sought to
analyze the expression of caspase-3 in acinar cells exposed to
macrophage-conditioned medium. As can be seen from the results of
western blot analysis, the cleavage of caspase-3 in the acinar
cells was evidently downregulated (Fig. 4C and D).
To further investigate the effects of TNF-α and
RANTES on ADM, we employed neutralizing antibodies (NABs) to
antagonize TNF-α and RANTES. As a result, neutralizing TNF-α and
RANTES markedly reversed the effects on amylase and CK-19
expression (Fig. 4E and F).
The PI3K/Akt/IKK signaling pathway plays
a vital role in NF-κB activation induced by rat macrophage
supernatants
NF-κB activation and translocation into the nucleus
has been proven to be an essential process for initiating ADM
(31). In this study, to examine
NF-κB activation, we introduced an NF-κB-luciferase reporter into
the acinar cells via an adenoviral transduction system. The results
revealed that treatment with macrophage supernatants markedly
promoted the activity of NF-κB (Fig.
5A). Importantly, compelling evidence has indicated that the
PI3K/Akt/IKK signaling pathway may be involved in the activation of
NF-κB (38,39). In the present study, PI3K
inhibitor LY294002 (25 mM) was added to the cultured primary acinar
cells prior to treatment with macrophage supernatants. The
expression of the phosphorylated form of Akt and IKK was then
analyzed by western blot analysis. Compared to the controls
(vehicle-treated group), the inhibition of PI3K led to a decrease
in phosphorylated Akt and IKK expression (Fig. 5B). Furthermore, NF-κB activity in
the acinar cells was also detected. The results revealed that PI3K
inhibition markedly abated NF-κB activity in the acinar cells
(Fig. 5C and D).
Physiological parameters of exposed
rats
To explore the effects of chronic alcohol and LPS on
the physiological parameters of rats, the animals were injected
with a series of doses (0, 5, 10, 15, 20 and 25 mmol/kg/day) of
alcohol for 4 weeks and then LPS (1 mg/kg). Following the
completion of treatment, all the animals were weighed and then
sacrificed by cervical dislocation, with their organs harvested for
the calculation of PW, LW, spleen weight (SW) and kidney weight
(KW). Compared to the control group (no treatment), increasing the
dose of alcohol significantly decreased BW, PW and LW in the rats
(Table II). However, no
difference was observed in the SW and KW of these rats among all
groups (Table II).
 | Table IIBody and organ weight of the animals
(n=60). |
Table II
Body and organ weight of the animals
(n=60).
| Groups | n | BW (g) | PW (g) | LW (g) | SW (g) | KW (g) |
|---|
| 0 | 10 | 455.9±29.7 | 1.89±0.27 | 6.19±0.95 | 0.93±0.27 | 3.43±0.91 |
| 5 | 10 | 437.6±29.4 | 1.61±0.25 | 5.91±0.62 | 1.15±0.33 | 3.37±0.79 |
| 10 | 10 | 422.7±28.7a | 1.43±0.25a | 5.34±0.81a | 1.26±0.32 | 3.44±0.89 |
| 15 | 10 | 401.3±27.5a | 1.31±0.26a | 4.68±0.64a | 1.17±0.29 | 3.35±0.88 |
| 20 | 10 | 392.5±22.8a | 1.20±0.18a | 4.15±0.73a | 1.32±0.41 | 3.47±1.15 |
| 25 | 10 | 387.8±26.5a | 1.07±0.19a | 3.73±0.71a | 1.24±0.56 | 3.51±1.21 |
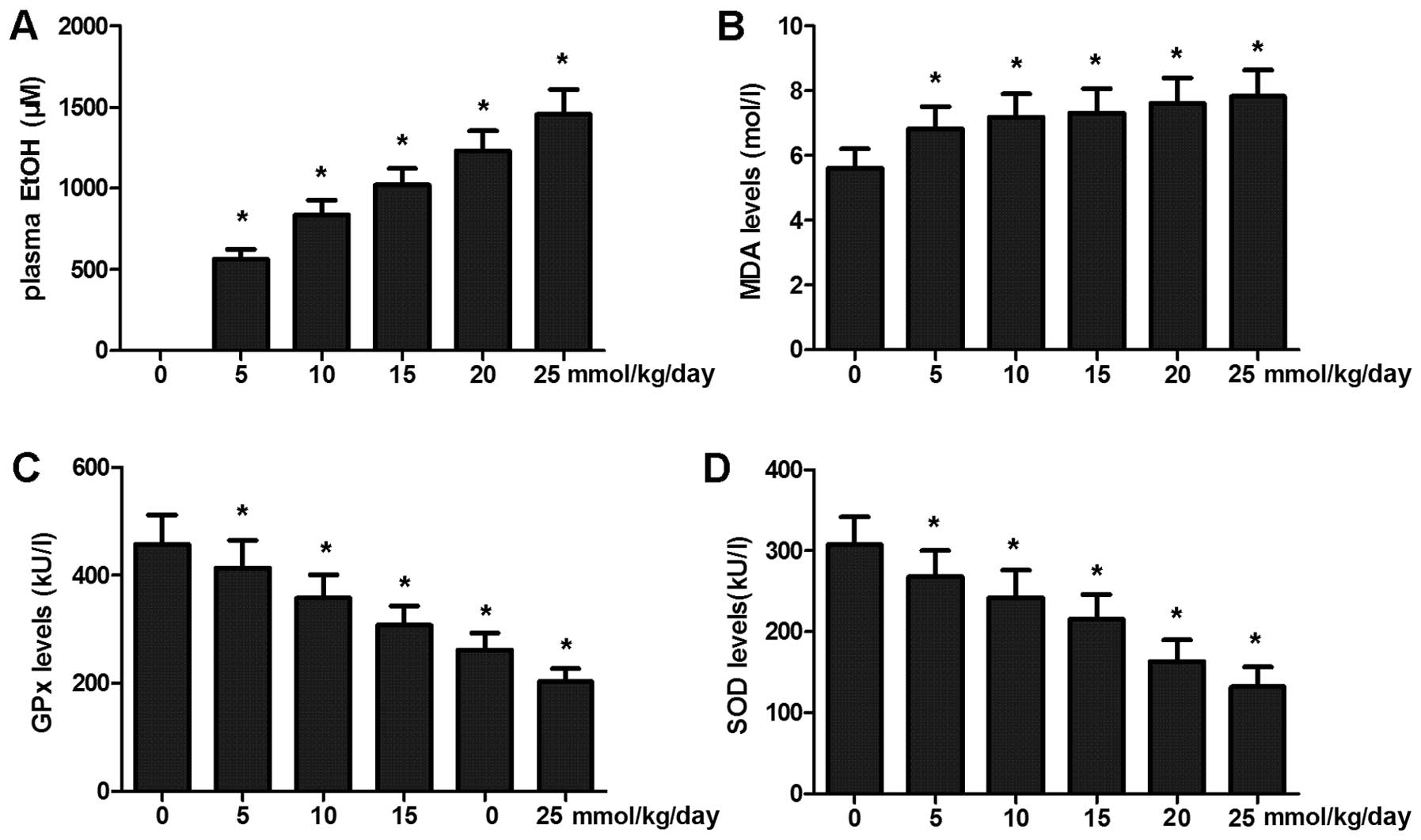
To determine the plasma alcohol concentration in the
rats, blood samples of these exposed rats were collected and
detected by enzyme-based assays. The plasma alcohol concentrations
of the exposed rats were much higher than those of the controls.
The results revealed that chronic alcohol exposure induced an
increase in the plasma alcohol concentration in the rats (Fig. 6A).
To determine oxidative stress caused by chronic
alcohol and LPS exposure, the MDA level, SOD activity and GPx
activity were calculated with the blood samples collected. Exposure
to chronic alcohol and LPS induced an increase in the MDA level in
serum with a concurrent decrease in SOD and GPx activity (Fig. 6B–D).
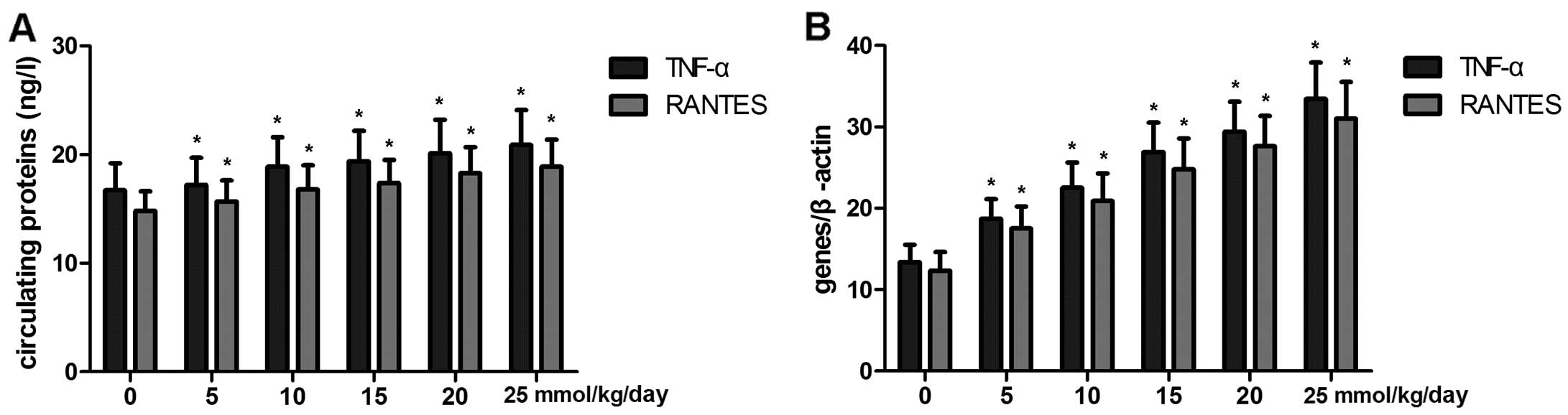
The levels of TNF-α and RANTES expression
in serum and monocytes are increased in rats
To investigate the effects of chronic alcohol and
LPS on circulating TNF-α and RANTES expression, TNF-α and RANTES
expression in serum was analyzed by ELISA. The results revealed
that the levels of TNF-α and RANTES in serum were evidently
increased by chronic alcohol and LPS exposure (Fig. 7A). Furthermore, monocytes in blood
samples were separated prior to TNF-α and RANTES expression in
these cells and were analyzed by RT-qPCR. Compared to the controls,
the expression levels of TNF-α and RANTES were distinctly
upregulated by chronic alcohol and LPS exposure (Fig. 7B).
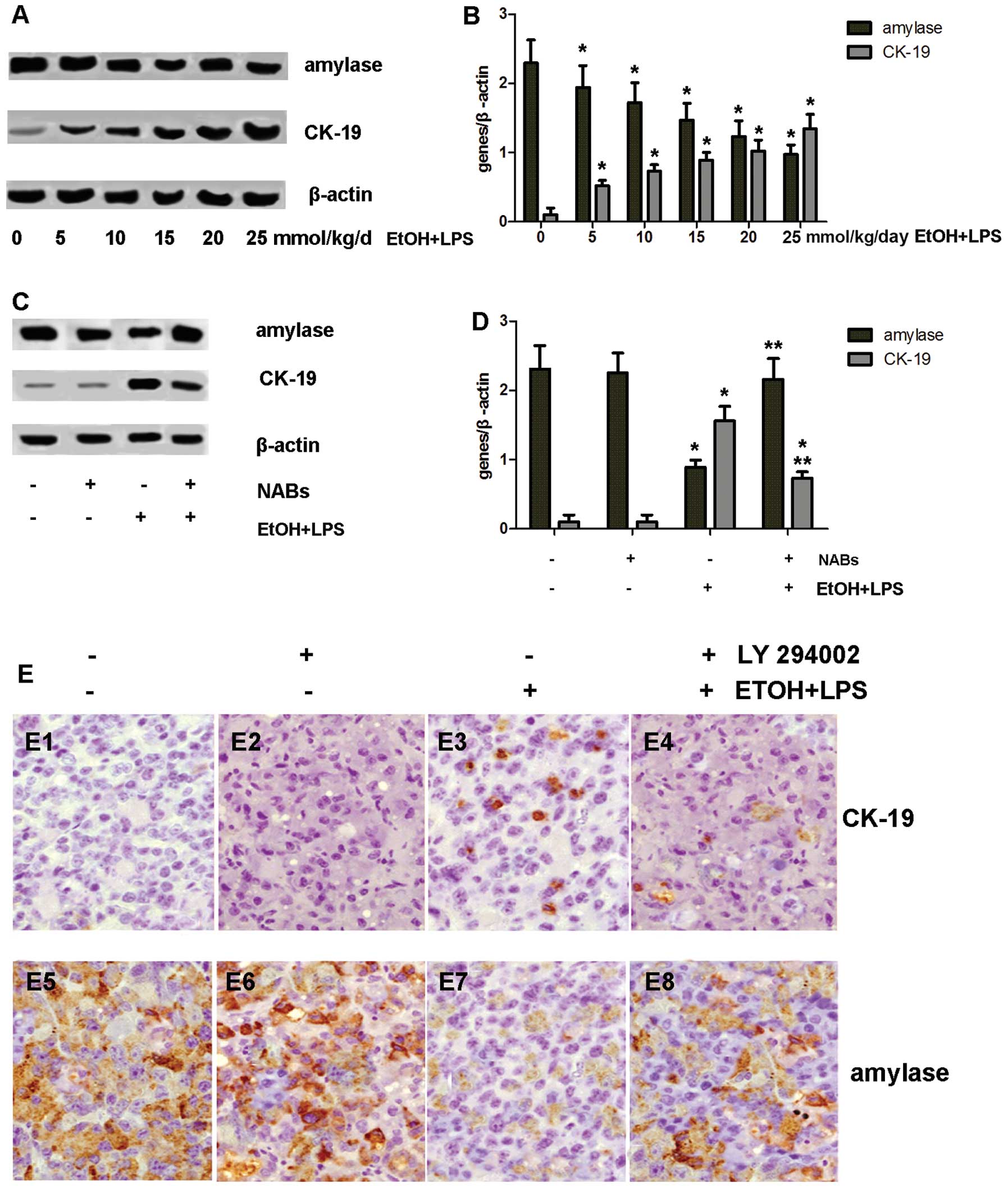
ADM is observed in pancreatic acinar
cells of rats
To further determine whether ADM occurs in
pancreatic acinar cells of rats exposed to chronic alcohol and LPS,
acinar cells derived from the exposed rats were isolated. Amylase
and CK-19 expression in these cells were analyzed by western blot
analysis. Chronic alcohol and LPS exposure significantly
downregulated amylase expression, but enhanced CK-19 expression in
the acinar cells compared with the controls (Fig. 8A and B).
We then explored whether ADM is inhibited as TNF-α
and RANTES is antagonized in vivo. Prior treatments with
NABs for neutralizing TNF-α and RANTES were carried out prior to
alcohol exposure (0, 25 mmol/kg/day)/LPS (1 mg/kg) in the rats. At
the end of treatment, these rats were then sacrificed and the
pancreases were harvested for the isolation of acinar cells.
Amylase and CK-19 expression in these cells was analyzed by western
blot analysis. Compared with the controls, neutralizing TNF-α and
RANTES induced an increase in amylase and a decrease in CK-19
expression in at the translational level (Fig. 8C and D).
The PI3K/Akt/IKK pathway plays an
essential role in the induction of pancreatic ADM in vivo
To further examine the role of the PI3K/Akt/IKK
pathway in the induction of pancreatic ADM in vivo, the
animals were administered PI3K inhibitor (LY294002, 100 mg/kg) 10
min piror to exposure to chronic alcohol (0 and 25 mmol/kg/day) and
LPS (1 mg/kg). As soon as the treatments were completed, these
animals were sacrificed and their pancreases were fixed in
formalin. Pancreatic sections were immunostained for amylase and
CK-19. As illustrated in the Fig.
8E, the inhibition of PI3K was sufficient to block pancreatic
ADM in the rats.
Discussion
Several studies have indicated that inflammation of
the pancreas may be an important source for the initiation of
pancreatic cancer (40–42). Reprogramming of pancreatic acini
has been shown to occur under many contexts and contributes to
acini transdifferentiation (43).
It has been demonstrated that chronic alcohol exposure elevates the
sensitivity of macrophages/monocytes and boosts the inflammatory
response to LPS stimulation (33). The role of alcohol and LPS
intoxication in the pancreas and the induction of pancreatic
lesions, and eventually, pancreatic cancer remains largely unknown.
In the present study, we provide evidence of the mechanisms through
which chronic alcohol modulates macrophage/monocyte responses and
causes acini transdifferentiation in the pancreas.
It is well established that acute alcoholic exposure
inactivates monocyte/macrophage responses to LPS stimulation, while
chronic exposure has the opposite effect (33,44). In this study, we found that
prolonged exposure to varying doses of alcohol resulted in an
increased expression of TNF-α and RANTES in rat macrophages
stimulated with LPS. The expression and secretion of
pro-inflammatory cytokines in macrophages have been proven to
correlate with the enhanced activity of NF-κB (45). In the present study, an increased
activity of NF-κB was observed in the macrophages treated with
alchohol and LPS with the upregulated expression of cytokines.
However, when NF-κB activity was hindered by the knockdown of NF-κB
expression or the overexpression of IκB, the expression of TNF-α
and RANTES in the macrophages was evidently downregulated.
IRAK-M is one of the primary targets in macrophages
exposed to alcohol (46). The
decreased expression of IRAK-M was induced in our study in
intoxicated macrophages. IRAK-M, as an upstream participant of
several pathways, regulates a cluster of factors which include
MAPKs and JNK and eventually activates NF-κB (47). In the present study, we found that
abated IRAK-M led to the increased expression of p38 MAPK and JNK,
as well as the secretion of TNF-α and RANTES. By contrast, the
increased IRAK-M expression evidently decreased TNF-κ and RANTES
secretion induced by prolonged exposure to alcohol and LPS
stimulation. These results indicate that IRAK-M, p38 MAPK and JNK
play an important role in the expression of pro-inflammatory
cytokines in macrophages exposed to chronic alcohol and LPS.
The transdifferentiation of acinar cells to
duct-like cells may lead to metaplastic duct lesions which are
commonly observed in pancreatitis (48). In the present study, culture
supernatants of intoxicated macrophages contributed to the process
of ADM in primary acinar cells. Furthermore, neutralizing TNF-α and
RANTES in the supernatant by NABs significantly abolished ADM in
the pancreatic acini. These results suggest the role of TNF-α and
RANTES in the induction of ADM, which is consistent with the
results of the study by Liou et al (31).
PI3K activation has been implicated in the
pathogenesis of various pancreatic lesions (49). The PI3K/Akt signaling pathway
mediates cell proliferation and invasiveness in pancreatic cancer
cells. The inhibition of PI3K signaling has been shown to lead to
abruption in G1-to-S phase progression and proliferation in
pancreatic cancer cells (50). In
this study, we found that the inhibition of PI3K resulted in a
decrease in pAkt/IKK expression and NF-κB activity induced by
macrophage culture supernatant. Given that NF-κB activity dominates
ADM in acinar cells, our data demonstrated that the PI3K/Akt/IKK
pathway was intimately associated with pancreatic ADM.
Evidence has indicated that a dedifferentiation
process may be a crucial part in ADM. Cultured pancreatic acini
will undergo apoptosis under normal conditions. However, once
pancreatic ADM has been induced, acinar cells can attain a longer
lifespan and proliferative properties (51). In the present study, treatment
with cultured supernatants of stimulated macrophages induced a
downregulation of the expression of cleaved caspase-3 in acinar
cells. Thus, an anti-apoptotic process may be induced in acinar
cells by the administration of macrophage culture supernatants.
Our results demonstrated that chronic alcohol
exposure and LPS stimulation may have an adverse effect on rats.
The body weight, PW and LW of the intoxicated rats were
significantly reduced at the end of treatment. Moreover, the
injection of alcohol and LPS enhanced the level of alcohol and
oxidative stress in the serum. Serum TNF-α and RANTES levels
examined by ELISA were distinctly augmented in the exposed rats
compared with the controls. Additionally, we found that TNF-α and
RANTES expression in monocytes in peripheral blood were evidently
upregulated by chronic alcohol exposure.
The monocyte secretion of cytokines, such as TNF-α
or RANTES plays a central role in the pathophysiology of
pancreatitis (52). In this
study, we detected the increased expression of CK-19 and decreased
amylase expression in acinar cells derived from alcoholic rats,
which indicated the occurrence of ADM induced by chronic alcohol
and LPS exposure. By contrast, neutralizing TNF-α and RANTES by
antibodies led to a decrease in pancreatic ADM. These data provide
evidence that TNF-α and RANTES play a major role in the induction
of ADM.
We observed that the PI3K/Akt/IKK pathway mediated
ADM induction by macrophage supernatants in cultured primary acini.
Accordingly, the inhibition of PI3K or IKK in the acini of rats
also significantly blocked ADM progression, which suggests the role
of PI3K/Akt/IKK in the induction of ADM in vivo.
Collectively, we found that chronic alcohol exposure
may promote cytokine secretion in macrophages/monocytes stimulated
by LPS both in vitro and in vivo. Under the
conditions of higher levels of pro-inflammatory cytokines,
pancreatic acini may undergo transdifferentiation which can be
blocked by PI3K or IKK inhibition. Since ADM is prevalent in
pancreatitis and can progress to advanced cancerous lesions,
targeting the PI3K/Akt/IKK pathway may be a promising approach for
the treatment of pancreatic ADM.
Acknowledgments
The present study was supported by grants from the
National Natural Science Foundation of China (NSFC) (no. 81172195,
81201824).
Abbreviations:
|
ADM
|
acinar-to-ductal metaplasia
|
|
Akt
|
protein kinase B
|
|
CK-19
|
cytokeratin-19
|
|
CP
|
chronic pancreatitis
|
|
ELISA
|
enzyme-linked immunosorbent assay
|
|
GPx
|
glutathione peroxidase
|
|
IKK
|
inhibitory κB kinase
|
|
IL-1
|
interleukin-1
|
|
IL-6
|
interleukin-6
|
|
IL-8
|
interleukin-8
|
|
IRAK
|
interleukin-1 receptor-associated
kinase
|
|
IκB
|
inhibitory κB
|
|
JNK
|
c-Jun amino-terminal kinase
|
|
KW
|
kidney weight
|
|
LPS
|
lipopolysaccharide
|
|
LW
|
liver weight
|
|
MAPK
|
mitogen-activated protein kinase
|
|
MDA
|
malondialdehyde
|
|
NF-κB
|
nuclear factor κB
|
|
PanIN
|
pancreatic intraepithelial
neoplasia
|
|
PDAC
|
pancreatic ductal adenocarcinoma
|
|
PI3K
|
phosphatidylinositol-3-kinase
|
|
PW
|
pancreatic weight
|
|
RT-qPCR
|
quantitative reverse
transcription-polymerase chain reaction
|
|
RANTES
|
regulated upon activation, normal T
cell expression and secreted
|
|
SD
|
Sprague-Dawley rat
|
|
siRNA
|
small-interfering RNA
|
|
SOD
|
superoxide dismutase
|
|
SW
|
spleen weight
|
|
TGF-β
|
tumor growth factor-β
|
|
TNF-α
|
tumor necrosis factor-α
|
References
|
1
|
Lang MB, Segersvard R, Grundsten M, et al:
Management of alcohol use disorders in patients with chronic
pancreatitis. JOP. 13:654–659. 2012.PubMed/NCBI
|
|
2
|
Lerch MM and Gorelick FS: Models of acute
and chronic pancreatitis. Gastroenterology. 144:1180–1193. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Duell EJ: Epidemiology and potential
mechanisms of tobacco smoking and heavy alcohol consumption in
pancreatic cancer. Mol Carcinog. 51:40–52. 2012. View Article : Google Scholar
|
|
4
|
Lucenteforte E, La Vecchia C, Silverman D,
et al: Alcohol consumption and pancreatic cancer: a pooled analysis
in the International Pancreatic Cancer Case-Control Consortium
(PanC4). Ann Oncol. 23:374–382. 2012. View Article : Google Scholar :
|
|
5
|
Gukovskaya AS, Mouria M, Gukovsky I, et
al: Ethanol metabolism and transcription factor activation in
pancreatic acinar cells in rats. Gastroenterology. 122:106–118.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ward JB, Petersen OH, Jenkins SA, et al:
Is an elevated concentration of acinar cytosolic free ionised
calcium the trigger for acute pancreatitis? Lancet. 346:1016–1019.
1995. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Whitcomb DC: Genetic polymorphisms in
alcoholic pancreatitis. Dig Dis. 23:247–254. 2005. View Article : Google Scholar
|
|
8
|
Truninger K, Malik N, Ammann RW, et al:
Mutations of the cystic fibrosis gene in patients with chronic
pancreatitis. Am J Gastroenterol. 96:2657–2661. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Vonlaufen A, Xu Z, Daniel B, et al:
Bacterial endotoxin: a trigger factor for alcoholic pancreatitis?
evidence from a novel, physiologically relevant animal model.
Gastroenterology. 133:1293–1303. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Fukui H, Brauner B, Bode JC, et al: Plasma
endotoxin concentrations in patients with alcoholic and
non-alcoholic liver disease: reevaluation with an improved
chromogenic assay. J Hepatol. 12:162–169. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Purohit V, Bode JC, Bode C, et al:
Alcohol, intestinal bacterial growth, intestinal permeability to
endotoxin, and medical consequences: summary of a symposium.
Alcohol. 42:349–361. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sharif R, Dawra R, Wasiluk K, et al:
Impact of toll-like receptor 4 on the severity of acute
pancreatitis and pancreatitis-associated lung injury in mice. Gut.
58:813–819. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Khan AQ, Nafees S and Sultana S: Perillyl
alcohol protects against ethanol induced acute liver injury in
Wistar rats by inhibiting oxidative stress, NFκ-B activation and
proinflammatory cytokine production. Toxicology. 279:108–114. 2011.
View Article : Google Scholar
|
|
14
|
Apte M, Pirola R and Wilson J: New
insights into alcoholic pancreatitis and pancreatic cancer. J
Gastroenterol Hepatol. 24(Suppl 3): S51–S56. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Mandrekar P and Szabo G: Signalling
pathways in alcohol-induced liver inflammation. J Hepatol.
50:1258–1266. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Boe DM, Richens TR, Horstmann SA, et al:
Acute and chronic alcohol exposure impair the phagocytosis of
apoptotic cells and enhance the pulmonary inflammatory response.
Alcohol Clin Exp Res. 34:1723–1732. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Zhang Z, Bagby GJ, Stoltz D, et al:
Prolonged ethanol treatment enhances lipopolysaccharide/phorbol
myristate acetate-induced tumor necrosis factor-α production in
human monocytic cells. Alcohol Clin Exp Res. 25:444–449.
2001.PubMed/NCBI
|
|
18
|
McClain CJ, Barve S, Deaciuc I, et al:
Cytokines in alcoholic liver disease. Semin Liver Dis. 19:205–219.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Zimmermann HW, Seidler S, Gassler N, et
al: Interleukin-8 is activated in patients with chronic liver
diseases and associated with hepatic macrophage accumulation in
human liver fibrosis. PLoS One. 6:e213812011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kiecolt-Glaser JK, Preacher KJ, MacCallum
RC, et al: Chronic stress and age-related increases in the
proinflammatory cytokine IL-6. Proc Natl Acad Sci USA.
100:9090–9095. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Strobel O, Dor Y, Alsina J, et al: In vivo
lineage tracing defines the role of acinar-to-ductal
transdifferentiation in inflammatory ductal metaplasia.
Gastroenterology. 133:1999–2009. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Uemura N, Okamoto S, Yamamoto S, et al:
Helicobacter pylori infection and the development of gastric
cancer. N Engl J Med. 345:784–789. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Eaden JA, Abrams KR and Mayberry JF: The
risk of colorectal cancer in ulcerative colitis: a meta-analysis.
Gut. 48:526–535. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Jankowski JA, Harrison RF, Perry I, et al:
Barrett’s metaplasia. Lancet. 356:2079–2085. 2000. View Article : Google Scholar
|
|
25
|
Bardeesy N and DePinho RA: Pancreatic
cancer biology and genetics. Nat Rev Cancer. 2:897–909. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Hingorani SR, Petricoin EF, Maitra A, et
al: Preinvasive and invasive ductal pancreatic cancer and its early
detection in the mouse. Cancer Cell. 4:437–450. 2003. View Article : Google Scholar
|
|
27
|
Means AL, Meszoely IM, Suzuki K, et al:
Pancreatic epithelial plasticity mediated by acinar cell
transdifferentiation and generation of nestin-positive
intermediates. Development. 132:3767–3776. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Carriere C, Seeley ES, Goetze T, et al:
The Nestin progenitor lineage is the compartment of origin for
pancreatic intraepithelial neoplasia. Proc Natl Acad Sci USA.
104:4437–4442. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Lowenfels AB, Maisonneuve P and Whitcomb
DC: Risk factors for cancer in hereditary pancreatitis.
International Hereditary Pancreatitis Study Group. Med Clin North
Am. 84:565–573. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Raynard B, Balian A, Fallik D, et al: Risk
factors of fibrosis in alcohol-induced liver disease. Hepatology.
35:635–638. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Liou GY, Doppler H, Necela B, et al:
Macrophage-secreted cytokines drive pancreatic acinar-to-ductal
metaplasia through NF-κB and MMPs. J Cell Biol. 202:563–577. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Liu L, Xu HM, Jiang H, Wang J, Song N and
Xie JX: Recombinant adenovirus-mediated expression of GHS-R1a in
HEK 293 cells. Neurosci Bull. 26:225–231. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Mandrekar P, Bala S, Catalano D, et al:
The opposite effects of acute and chronic alcohol on
lipopolysaccharide-induced inflammation are linked to IRAK-M in
human monocytes. J Immunol. 183:1320–1327. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Tandon RK and Garg PK: Oxidative stress in
chronic pancreatitis: pathophysiological relevance and management.
Antioxid Redox Signal. 15:2757–2766. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Sung NY, Yang MS, Song DS, et al:
Procyanidin dimer B2-mediated IRAK-M induction negatively regulates
TLR4 signaling in macrophages. Biochem Biophys Res Commun.
438:122–128. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Zhou H, Yu M, Fukuda K, et al: IRAK-M
mediates Toll-like receptor/IL-1R-induced NFκB activation and
cytokine production. EMBO J. 32:583–596. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Dey P, Rachagani S, Vaz AP, Ponnusamy MP
and Batra SK: PD2/Paf1 depletion in pancreatic acinar cells
promotes acinar-to-ductal metaplasia. Oncotarget. 5:4480–4491.
2014.PubMed/NCBI
|
|
38
|
Sun ZJ, Chen G, Hu X, et al: Activation of
PI3K/Akt/IKK-alpha/NF-kappaB signaling pathway is required for the
apoptosis-evasion in human salivary adenoid cystic carcinoma: its
inhibition by quercetin. Apoptosis. 15:850–863. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Venkatesan B, Valente AJ, Prabhu SD,
Shanmugam P, Delafontaine P and Chandrasekar B: EMMPRIN activates
multiple transcription factors in cardiomyocytes, and induces
interleukin-18 expression via Rac1-dependent PI3K/Akt/IKK/NF-kappaB
andMKK7/JNK/AP-1 signaling. J Mol Cell Cardiol. 49:655–663. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Bao Y, Giovannucci EL, Kraft P, et al:
Inflammatory plasma markers and pancreatic cancer risk: a
prospective study of five U.S. cohorts. Cancer Epidemiol Biomarkers
Prev. 22:855–861. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Basso D, Bozzato D, Padoan A, et al:
Inflammation and pancreatic cancer: molecular and functional
interactions between S100A8, S100A9, NT-S100A8 and TGFβ1. Cell
Commun Signal. 12(20): 2014
|
|
42
|
Grote VA, Kaaks R, Nieters A, et al:
Inflammation marker and risk of pancreatic cancer: a nested
case-control study within the EPIC cohort. Br J Cancer.
106:1866–1874. 2012.PubMed/NCBI
|
|
43
|
Morris JP IV, Wang SC and Hebrok M: KRAS,
Hedgehog, Wnt and the twisted developmental biology of pancreatic
ductal adenocarcinoma. Nat Rev Cancer. 10:683–695. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Szabo G, Chavan S, Mandrekar P, et al:
Acute alcohol consumption attenuates interleukin-8 (IL-8) and
monocyte chemoattractant peptide-1 (MCP-1) induction in response to
ex vivo stimulation. J Clin Immunol. 19:67–76. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Baker RG, Hayden MS and Ghosh S: NF-κB,
inflammation, and metabolic disease. Cell Metab. 13:11–22. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Tazi KA, Quioc JJ, Saada V, et al:
Upregulation of TNF-alpha production signaling pathways in
monocytes from patients with advanced cirrhosis: possible role of
Akt and IRAK-M. J Hepatol. 45:280–289. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Cuschieri J and Maier RV:
Mitogen-activated protein kinase (MAPK). Crit Care Med.
33:S417–S419. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Song SY, Gannon M, Washington MK, et al:
Expansion of Pdx1-expressing pancreatic epithelium and islet
neogenesis in transgenic mice overexpressing transforming growth
factor alpha. Gastroenterology. 117:1416–1426. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Arlt A, Gehrz A, Muerkoster S, et al: Role
of NF-κB and Akt/PI3K in the resistance of pancreatic carcinoma
cell lines against gemcitabine-induced cell death. Oncogene.
22:3243–3251. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Perugini RA, McDade TP, Vittimberga FJ Jr,
et al: Pancreatic cancer cell proliferation is phosphatidylinositol
3-kinase dependent. J Surg Res. 90:39–44. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Seeley ES, Carriere C, Goetze T, et al:
Pancreatic cancer and precursor pancreatic intraepithelial
neoplasia lesions are devoid of primary cilia. Cancer Res.
69:422–430. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Ramudo L, Manso MA, Sevillano S, et al:
Kinetic study of TNF-α production and its regulatory mechanisms in
acinar cells during acute pancreatitis induced by bile-pancreatic
duct obstruction. J Pathol. 206:9–16. 2005. View Article : Google Scholar : PubMed/NCBI
|