Introduction
Malignant melanoma (MM) is the most fatal cutaneous
neoplasm, and usually arises as a result of uncontrolled growth of
pigment cells called melanocytes of the skin (1). MM most commonly presents as a primary
neoplasm of the skin, but it has also been identified in other
sites, including the respiratory tract, esophagus, liver,
gallbladder, ovaries, cervix, uterus, genitourinary tract and
leptomeninges. Almost every occurrence of MM of the lung is
metastatic in origin. Primary pulmonary MM accounts for just 0.01%
of all primary pulmonary tumors (2).
Approximately 35 cases have been described in the literature, and
these are mostly case reports of primary MM of the lung. In
particular, an extrapulmonary origin of the tumor should be
convincingly ruled out by detailed examination of the sites where
MM occurs frequently, including the skin or mucosa, before
considering this diagnosis. In this article we present a case of
primary MM of the lung in an elderly male, who was finally
diagnosed by pathological examination.
Case report
A 60-year-old healthy asymptomatic man with an
abnormal shadow on a chest X-ray was referred to Shandong
Provincial Hospital Affiliated to Shandong University, China, for
further investigation. The patient was an ex-smoker, having smoked
35 cigarettes per day between the age of 20 and 60. The patient had
no respiratory complaints or other physical symptoms and no
personal history of lung disease. The X-ray revealed an irregular
opacity in his left lower lobe (Fig.
1). Computed tomography (CT) revealed a tumor located in the
left lower lobe (Fig. 2).
Bronchoscopy revealed an endobronchial mass obstructing the left
lower lobe bronchus, and the results of the biopsy revealed
non-small-cell lung carcinoma. The patient underwent thoracotomy
and a semi-solid neoplasm was identified. A pneumonectomy with
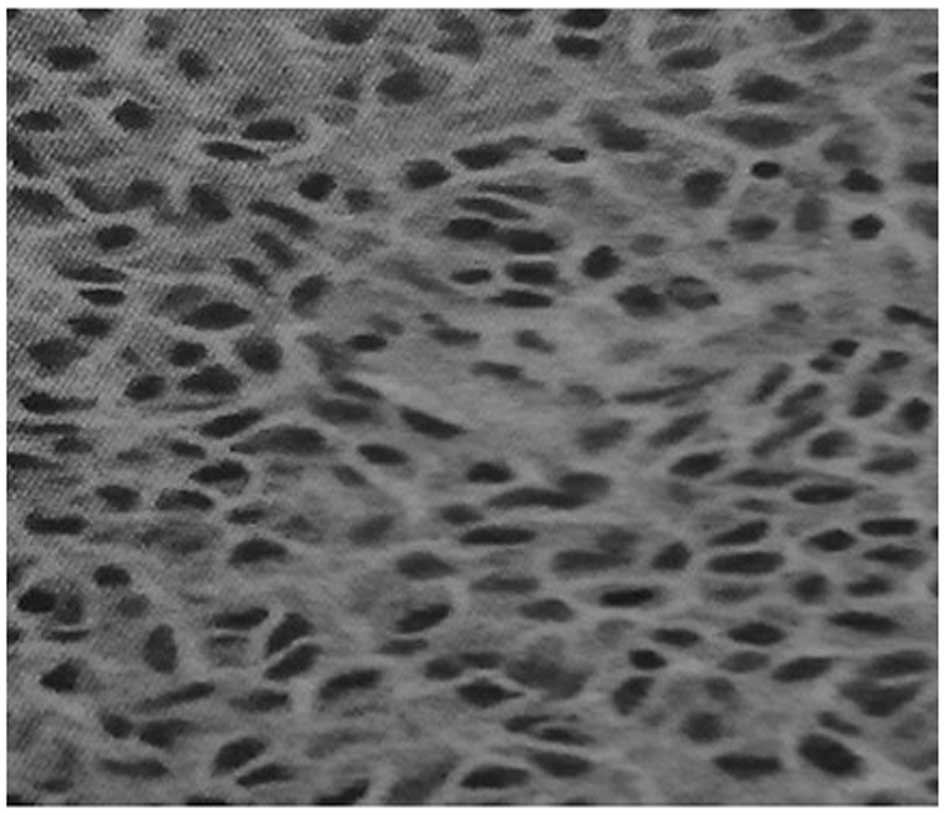
mediastinal lymph node dissection was carried out. Histologically
the tumor was composed predominantly of epithelioid tumor cells;
junctional change and mitotic activity with characteristic nesting
of malignant cells beneath the bronchial epithelium was also
observed, suggesting a diagnosis of MM. Immunohistochemical
reactions supported this diagnosis with a positive melanoma
cocktail of S-100 (Fig. 3),
melanoma-associated monoclonal antibody HMB45 and α-smooth muscle
actin, whereas cytokeratin, epithelial membrane antigen and
calponin were negative. Dissected hilar and mediastinal lymph nodes
were free of metastatic disease.
Considering the possibility of pulmonary metastasis
of MM, ophthalmic, skin, oral and rhinal examinations were carried
out by specialists to rule out extrapulmonary disease. No
additional abnormalities were observed on subsequent detailed
metastatic work-up including magnetic resonance imaging of the
brain, CT of the abdomen and whole-body bone scan and endoscopy
(upper gastrointestinal scope, colonoscope and cystoscope). The
patient received adjuvant chemotherapy postoperatively for 6
months, and is living disease-free 18 months after the surgery
without any major complaints. This study was approved by the Ethics
Committee of Shandong Provincial Hospital Affiliated to Shandong
University (Jinan, China). Written informed consent was obtained
from the patient's family.
Discussion
Primary MM of the lung is an extremely rare neoplasm
that accounts for just 0.01% of all primary lung tumors. There is
no precise etiology of primary MM of the lung. One possible
speculation is that the tumor occurs when a certain number of
epithelial cells have undergone differentiation towards melanocytes
in areas of squamous metaplasia (3).
No significant statistical difference in the incidence of primary
MM of the lung is observed between genders. However, cigarette
smoking may be a risk factor of primary MM of the lung, as
cigarette smoking may cause squamous metaplasia (4).
The symptoms of MM of the lung are similar to those
of bronchogenic carcinoma. It is frequently manifested with
symptoms of a cough, hemoptysis, postobstructive pneumonia, lobar
collapse or atelectasis. More rarely, it is identified in
asymptomatic healthy patients, as in the case of our patient. Its
radiological appearance is similar to that of lung cancer,
manifesting as an abnormal shadow or irregular mass (5). The final diagnosis of a primary MM of
the lung should be based on clinical, radiological and pathological
findings. The proposed criteria for its diagnosis may be split into
three groups (6–8). Clinical criteria: No previously resected
pigmented skin lesion, no demonstrable melanoma in any other organ
at time of surgery, solitary tumor in surgical specimen from the
lung, tumor morphology comparable with that of a primary tumor.
Radiological criteria: Abnormal shadow on chest X-ray, irregular
mass or node on computed tomography. Pathological criteria:
Invasion of the bronchial epithelium by melanoma cells, junctional
changes including ‘dropping off’ or ‘nesting’ just beneath the
bronchial epithelium, evident melanoma cells confirmed by
immuno-histochemical staining for S-100 and HMB-45.
The optimal treatment for patients with primary MM
of the lung remains to be determined. Surgical resection with an
oncologically adequate margin, such as lobectomy or pneumonectomy,
is usually the first choice of treatment in cases of primary MM of
the lung with no distant metastasis. The role of postoperative
adjuvant chemotherapy or radiotherapy is not fully known (3). Previously, various chemotherapeutic
agents have been used, including dacarbazine and immunotherapy with
interleukin-2 or interferon (2).
Radiation therapy is often used in patients with locally or
regionally advanced melanoma of the skin or for patients with
unresectable distant metastases. Although it may reduce the rate of
local recurrence, it does not prolong the survival rate.
The long-term survival rate of patients with primary
MM of the lung is usually poor, even for patients receiving
treatment of radical surgical excision. Long-term survival has been
achieved in two cases in the past (10 and 11 years following
lobectomy and pneumonectomy, respectively) (9,10). Further
evaluation and close follow-up of the patient is advised in order
to diagnose metastatic dissemination and to improve outcome.
In conclusion, primary MM of the lung represents a
rare pathological entity. Careful preoperative investigation and
postoperative confirmation of the diagnosis together with clinical
findings may establish the diagnosis. Surgical intervention and
resection of the involved lymph nodes is appropriate and offers the
possibility of long-time survival for certain patients.
References
|
1
|
Balch CM, Soong SJ, Gershenwald JE, et al:
Prognostic factors analysis of 17,600 melanoma patients: validation
of the American Joint Committee on Cancer melanoma staging system.
J Clin Oncol. 19:3622–3634. 2001.PubMed/NCBI
|
|
2
|
Bajetta E, Del Vecchio M, Bernard-Marty C,
et al: Metastatic melanoma: chemotherapy. Semin Oncol. 29:427–445.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wilson RW and Moran CA: Primary melanoma
of the lung: a clinicopathologic and immunohistochemical study of
eight cases. Am J Surg Pathol. 21:1196–1202. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Volpin E, Sauvanet A, Couvelard A and
Belghiti J: Primary malignant melanoma of the esophagus: a case
report and review of the literature. Dis Esophagus. 15:244–249.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Cagle P, Mace ML, Judge DM, Teague RB,
Wilson RK and Greenberg SD: Pulmonary melanoma. Primary vs
metastatic. Chest. 85:125–126. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Allen MS Jr and Drash EC: Primary melanoma
of the lung. Cancer. 21:154–159. 1968. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Bagwell SP, Flynn SD, Cox PM and Davison
JA: Primary malignant melanoma of the lung. Am Rev Respir Dis.
139:1543–1547. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Alghanem AA, Mehan J and Hassan AA:
Primary malignant melanoma of the lung. J Surg Oncol. 34:109–112.
1987. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Reed RJ 3rd and Kent EM: Solitary
pulmonary melanomas: Two case reports. J Thorac Cardiovasc Surg.
48:226–231. 1964.PubMed/NCBI
|
|
10
|
Reid JD and Mehta VT: Melanoma of the
lower respiratory tract. Cancer. 19:627–631. 1966. View Article : Google Scholar : PubMed/NCBI
|